Abstract
The changes of tibiofemoral articular cartilage contact locations during knee activities represents a physiological functional characteristics of the knee. However, most studies reported relative motions of the tibia and femur using morphological flexion axes. Few data have been reported on comparisons of morphological femoral condyle motions and physiological tibiofemoral cartilage contact location changes. This study compared the morphological and physiological kinematic measures of 20 knees during an in vivo weightbearing single leg lunge from full extension to 120° of flexion using a combined MRI and dual fluoroscopic imaging system (DFIS) technique. The morphological femoral condyle motion was measured using three flexion axes: trans-epicondylar axis (TEA), geometric center axis (GCA) and iso-height axis (IHA). At low flexion angles, the medial femoral condyle moved anteriorly, opposite to that of the contact points, and was accompanied with a sharp increase in external femoral condyle rotation. At 120° of flexion, the morphological measures of the lateral femoral condyle were more posteriorly positioned than those of the contact locations. The data showed that the morphological measures of femoral condyle translations and axial rotations varied with different flexion axes and did not represent the physiological articular contact kinematics. Biomechanical evaluations of the knee joint motion should include both morphological and physiological kinematics data to accurately demonstrate the functionality of the knee.
Keywords: Knee, Singe leg lunge, In vivo, Cartilage contact kinematics, Flexion axes, Posterior femoral translation
1. Introduction
Accurate knowledge of the knee kinematics is critical for understanding of the joint functionality and for development of surgical techniques such as total knee arthroplasty and ligament reconstruction that are aimed to restore normal knee joint functions (Eckhoff et al., 2007; Most et al., 2004). Various knee kinematics data during knee flexion have been reported using different measurement methods (Churchill et al., 1998; Colle et al., 2012; Dennis et al., 2005; Mochizuki et al., 2014; Mu et al., 2011). For example, the morphological trans-epicondylar axis (TEA) and the geometrical center axis (GCA) have been traditionally used to measure the medial and lateral femoral condyle translations and axial rotations (Li et al., 2013; Oussedik et al., 2012; Victor, 2009; Walker et al., 2011). A new flexion axis termed iso-height axis (IHA) was recently proposed that measured minimum variations in femoral condyle heights with knee flexion (Rao et al., 2020). Several studies have shown that different flexion axes could provide different kinematics data of the same knee motion (Gromov et al., 2014; Hull, 2020; Tanifuji et al., 2013; Victor, 2009; Walker et al., 2011). However, the tibiofemoral articulation of the knee, that is an articular joint, is an integral part of the knee joint motion. It represents a physiological motion characteristic of the knee, as articular contact locations directly affect the moment arms of the knee muscles and joint reaction forces (Lerner et al., 2015). A few studies have investigated the association of the morphological kinematics and the physiological tibiofemoral articulation under various loading conditions (Asano et al., 2001; Pinskerova et al., 2004; Qi et al., 2013; Walker et al., 2011). This information is instrumental for investigation of the knee kinematics and for improvement of surgical methods to restore normal knee functions.
In this paper, we measured in vivo tibiofemoral articular cartilage contact point changes during a weightbearing, single leg lunge of the knee as well as the corresponding translations and axial rotations of the femoral condyles using different morphological flexion axes. Moreover, the contact point motions were compared with the femoral condyle translation data. It was hypothesized that the femoral condyle motions measured using the morphological flexion axes did not represent the physiological articular contact motion of the knee during the full range of in vivo weightbearing, single leg lunge.
2. Methods
2.1. Subjects
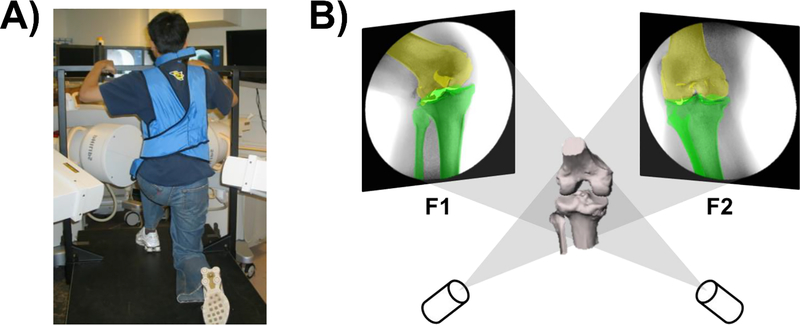
Twenty healthy knees of 20 subjects (14 men and 6 women; age 33±13 years; body mass index: 25.5±3.5 kg/m2; 9 left and 11 right) were recruited and written consent was signed by all subjects prior to participation in this study. A combined MRI and dual fluoroscopic imaging system (DFIS) technique was used to measure knee kinematics (Li et al., 2004). The DFIS that was composed of two orthogonally positioned fluoroscopes (BV Pulsera; Philips, Bothell, WA) (Fig. 1A). Each knee was imaged using a 3T MRI scanner (Siemens, Erlangen, Germany) in sagittal plane. The images were used to construct a three-dimensional (3D) surface model of the knee, including the femur, tibia, and their cartilage surfaces, in a solid modeling software (Rhinoceros, Seattle, WA). Each subject performed a quasi-static single-legged lunge with a 15° increment from full extension to maximal flexion. During experiment, the knee kept stable at each target flexion angle for 1–3 seconds while imaged using the DFIS. The 3D knee model and the fluoroscopic images were imported into the software to create a virtual DFIS in computer (Fig. 1B). The projections of the 3D femur and tibia models were matched to their corresponding fluoroscopic images to reproduce the knee positions in space. It was reported that this technique has errors less than 0.1 mm and 0.3° in measuring tibiofemoral translations and rotations, respectively (Li et al., 2008).
Fig. 1.
(A) The dual fluoroscopic imaging system (DFIS) set up for measurements of knee joint motion during a quasi-static single leg lunge. (B) Illustration of the 3D-2D registration that reproduce the kinematics of the knee in a virtual DFIS by matching the projections of the 3D knee model to the two fluoroscopic images captured along flexion path.
2.2. Knee Kinematics Analysis
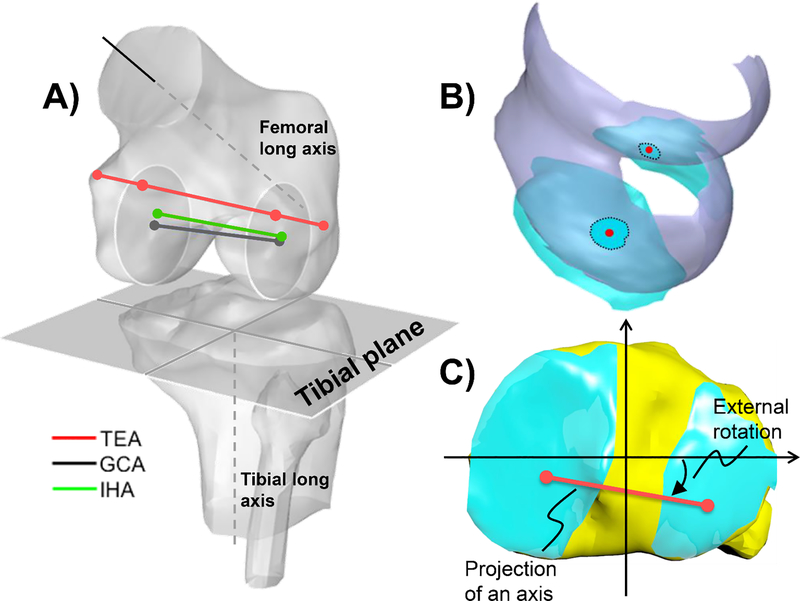
To determine the contact point and femoral condyle motions, a knee joint coordinate system was established (Qi et al., 2013) (Fig. 2A). The tibial long axis was parallel to the posterior wall of the proximal tibial shaft constructed from MRI images. The tibial plane was defined as vertical to the long axis. The medial-lateral axis was defined as a line connecting the centroids of two circles fitting to the medial and lateral tibial plateau surfaces. The anterior-posterior axis was perpendicular to the two axes in the tibial plane. The femoral long axis was defined along the centroid of the distal femoral shaft constructed from MRI images (Fig. 2A). The knee flexion was measured between the tibia and femur long axes in sagittal plane. The GCA axis was defined as a line connecting the centroids of two circular planes (GCA planes) fitting to the maximal cross-sections of the posterior portions of the medial and lateral condyles in the sagittal plane (Rao et al., 2020). The TEA axis was defined by connecting the medial and lateral epicondyles (Most et al., 2004; Walker et al., 2011), and the two intersection points between the TEA and two GCA planes were used to determine the condylar motions. The IHA was determined as the line connecting the two points in the medial and lateral GCA planes, respectively that measured the least vertical shifts of the respective condyles along the knee flexion path (Rao et al., 2020). The articular contact point was defined as the centroid of the overlapping area of the femoral and tibial cartilage surfaces at each knee flexion position (DeFrate et al., 2004; Qi et al., 2013; Yin et al., 2017) (Fig. 2B).
Fig. 2.
(A) Definition of the tibial coordinate system and femoral flexion axes for measurements of femoral condyle translations. (B) Determination of tibiofemoral articular cartilage contact points by the centroid of the overlapping areas of the tibiofemoral cartilage surfaces. (C) Measurements of femoral condyle translations and axial rotations on the tibial coordinate plane using the projections of the femoral condyle axes.
The contact points and the flexion axes were all projected onto the tibial plane for measurements of the anteroposterior translations of the contact points and flexion axes as well as the axial rotations of the femoral condyles (Fig. 2C) (Dimitriou et al., 2016). The articular contact point location path was used to represent the physiological motion and the femoral condyle motion to represent the morphological motion of the knee.
2.3. Data Analysis
A repeated measure ANOVA and post-hoc Tukey analysis were used to compare the physiological and morphological joint kinematics data. Paired t tests were used to analyze the differences between the medial and lateral compartments. Independent variable was the knee flexion angles and motion measurement methods. The dependent variables were defined as femoral condylar motions and rotations. A statistically significant difference was determined when p<0.05.
3. Results
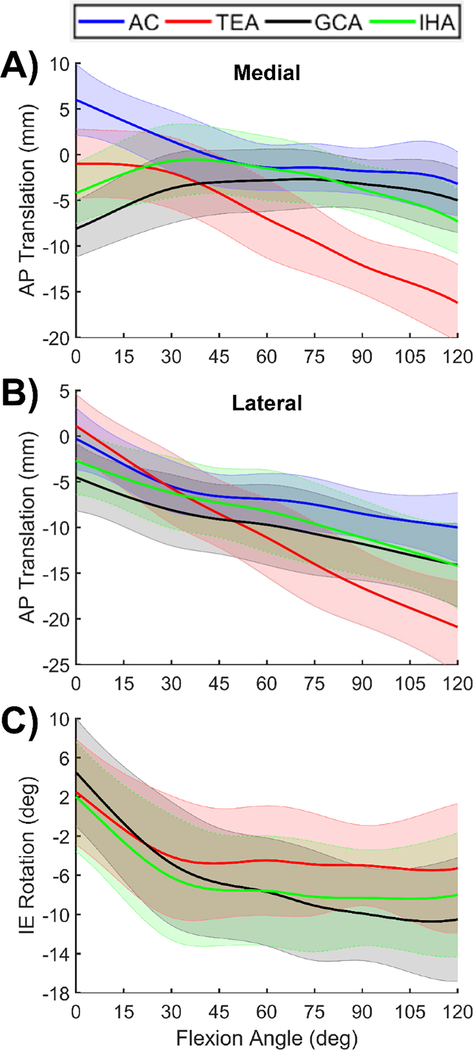
In the medial compartment (Fig. 3A), the contact point was positioned at 6.0±3.9 mm anteriorly at full extension and moved posteriorly until 60° knee flexion (-1.4±2.5 mm). Thereafter, the contact point had minimal motion with flexion. All flexion axes measured condyle positions posterior to the contact point at full extension (p<0.05). The TEA condyle moved slightly posteriorly until 30° of flexion and moved posteriorly thereafter. The GCA condyle moved anteriorly with knee flexion until 60° (p<0.05) and kept almost constant with further flexion. The IHA condyle moved anteriorly with knee flexion until around 30° and reached similar positions with the contact points. Beyond 45°, the condyle moved posteriorly consistently with flexion angles. Overall (from 0° to 120° flexion, Table 1), the contact point excursion (10.7±4.6 mm) was smaller than the TEA condyle excursion (16.0±5.2 mm) (p<0.05), but significantly larger than those of the GCA (7.3±2.1 mm) and IHA (7.9±3.5 mm) (p<0.05).
Fig. 3.
Anteroposterior translations (+: anterior / -: posterior) of the (A) medial and (B) lateral femoral condyles compared with articular contact (AC) motions, and (C) axial rotations (+: internal / -: external) of the femoral condyles during knee flexion. Shaded bands represent ± one standard deviation.
Table 1.
Anteroposterior translations of the articular contact (AC) points and femoral condyles at different ranges of knee flexion (“+” = anterior; “−” = posterior)
| 0 – 30° | 30 – 60° | 60 – 90° | 90 – 120° | Overall (Max - Min) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| M | L | M | L | M | L | M | L | M | L | |
| AC | −4.6±4.7a | −5.1±4.1ab | −2.8±2.4b | −1.5±2.1b | −0.4±1.7c | −1.5±1.3b | −1.4±2.3b | −1.5±3.1a | 10.7±4.6b | 10.5±4.0a |
| TEA | −1.0±2.1b | −6.8±3.6a | −5.0±1.8a | −5.4±2.2a | −5.1±2.7a | −5.5±2.0a | −4.1±3.3a | −4.3±3.7a | 16.0±5.2c | 22.4±4.4c |
| GCA | 4.5±2.5c | −3.6±3.7b | 0.8±1.9c | −1.6±2.3b | −0.3±1.6c | −2.1±2.1b | −1.8±2.2b | −2.3±3.3a | 7.3±2.1a | 10.8±3.3a |
| IHA | 3.6±2.5c | −3.5±3.7b | −0.8±1.9c | −2.0±2.4b | −2.4±1.7b | −2.8±2.1b | −3.5±2.4ab | −3.2±3.4a | 7.9±3.5a | 12.4±3.2a |
Note:
Multiple comparisons (i.e., ANOVA + Tukey post hoc tests): for each column, each letter subscript represents a group within which there are no significant differences (p > 0.05); the subscripts in an alphabetical order were assigned to the groups with the means in an increasing order. Different subscripts mean significant differences between groups (p < 0.05).
Student t-tests: the significant differences in the ROMs between the medial and lateral sides were indicated by bold.
In the lateral compartment (Fig. 3B), the contact point was positioned at −0.3±3.4 mm posteriorly at full extension and moved posteriorly to −5.5±2.8 mm with knee flexion until 30°. Thereafter, the contact point continued posterior motion at a slower rate to −10±3.8 mm at 120° flexion. The TEA condyle motion was similar to the contact point from full extension to 30° of flexion, but moved posteriorly more quickly than the contact points thereafter. The GCA condyle positions were about 5 mm posterior to the contact points along the flexion path (p<0.05). The IHA condyle positions were slightly posterior to the contact points until 75° of flexion. Thereafter, the condyle position moved posteriorly. Overall (Table 1), the contact point excursion was 10.5±4.0 mm, significantly smaller than that (22.4±4.4 mm) of the TEA (p<0.05), but similar to those of the GAC (10.8±3.3 mm) and IHA (12.4±3.2 mm) (p>0.05).
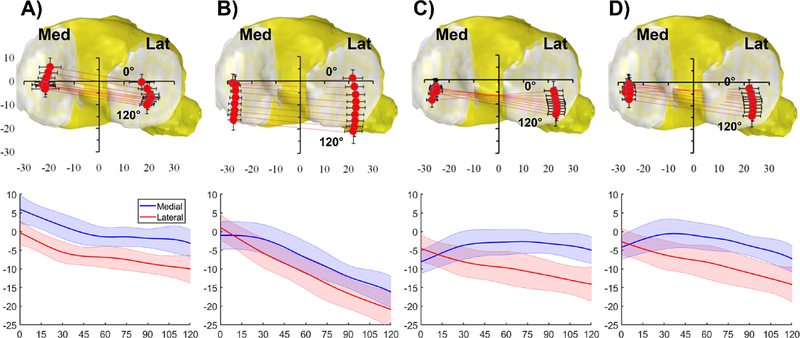
The medial contact points were about 5 mm more anterior than lateral points along the flexion path (p<0.05), but with similar translational excursions (p>0.05) (Table 1 and Fig. 4A). For all flexion axes, the lateral condyle is more anterior than the medial side at full extension, and beyond 15° flexion, becomes more posterior than the medial side until maximal flexion (Table 1 and Figs. 4B, C, D). The axial rotations of the femur were similar in trends when measured using the three flexion axes (Fig. 3C). A sharp increase in external condyle (internal tibial) rotation was measured from full extension to 30° of flexion. Thereafter, the axial rotation continuously increased with flexion by using the GCA, but with slower increasing rates using the TEA and IHA. Overall (Table 2), the largest range of the femoral condyle axial rotations was measured by the GCA (17.5±4.7°), significantly greater than those measured by the TEA (12.2±4.8°) and by the IHA (13.4±4.5°) (p>0.05).
Fig. 4.
Comparison of the motions of the medial and lateral femoral condyles using (A) articular contact points, (B) TEA, (C) GCA, and (D) IHA axes during the knee flexion. For each motion description, the upper plots graphically present the medial and lateral femoral condyle motions projected onto the tibial plane. The contact points / axis end points of the medial and lateral condyles at each flexion angle are connected by straight lines. The vertical and horizontal bars represent ± one standard deviations of the anteroposterior and mediolateral location measurements. The lower plots quantitatively describe the anteroposterior locations of the medial and lateral femoral condyles from 0° to 120° of flexion using different motion descriptions. The shaded bands represent ± one standard deviation.
Table 2.
Axial rotation ranges of the femoral condyles during knee flexion (“+” = internal rotation and “−” = external rotation of the femur relative to the tibia)
| 0 – 30° | 30 – 60° | 60 – 90° | 90 – 120° | Overall (Max - Min) | |
|---|---|---|---|---|---|
| TEA | −6.6±4.8a | −0.4±2.6b | −0.5±4.4a | −0.3±4.5a | 12.2±4.8a |
| GCA | −9.3±4.9a | −2.9±3.0a | −2.2±3.5a | −0.7±4.0a | 17.5±4.7b |
| IHA | −8.1±5.0a | −1.4±3.1ab | −0.7±3.5a | 0.3±3.9a | 13.4±4.5a |
Note:
Multiple comparisons (i.e., ANOVA + Tukey post hoc tests): for each column, each letter subscri represents a group within which there are no significant differences (p > 0.05); the subscripts in alphabetical order were assigned to the groups with the means in an increasing order.
4. Discussion
This study compared the motions of the physiological articular contact points and morphological femoral condyles of the same knee during a weightbearing knee flexion. The morphological condyle positions were more posterior than those of the contact points. The medial femoral condyle was shown to move in opposite direction with the contact points at low flexion angles, corresponding to a sharp increase in external femoral condyle rotation. These data indicated that the morphological femoral condyle motions varied with different flexion axes and did not accurately represent the physiological articular contact kinematics during the single leg lung of the knee.
Many studies have reported the knee motion using different coordinate systems (Dabirrahmani and Hogg, 2017; Mannel et al., 2004; Miranda et al., 2010; Renault et al., 2018). Oussedik et al. (2012) used a functional flexion axis and Kozanek et al. (2009) used TEA and GCA to analyze femoral condyle translations during gait. Eckhoff et al. (2007) indicated that a GCA can closely simulate the flexion axis of the knee compared to a TEA. Most et al. (2004) and Walker et al. (2011) revealed that the TEA and GCA measured different femoral condyle motions and axial rotations using cadaveric knees. For comparison of the articular contact kinematics and the femoral condyle motion, Pinskerova et al. (2004) showed more anterior positions at low flexion and similar positions at high flexion angles of the contact points when compared to the femoral condyle positions during a squat on both legs measured using sagittal plane MR images of the knee. Similar observations in the medial side of knee were reported by Walker et al. (2011) using cadaveric knees.
The femoral condyle motions and the cartilage contact kinematics in this paper were generally consistent in trend with previous data during knee flexion (Dimitriou et al., 2016; Feng et al., 2016; Most et al., 2004; Pinskerova et al., 2004; Walker et al., 2011). The differences in motion magnitudes could be due to variations in testing conditions among different studies, such as in vivo single leg lunge versus squat on both legs (Pinskerova et al., 2004) or simulated loads on cadaveric knees (Walker et al., 2011). Furthermore, our data showed that the medial and lateral contact points consistently moved posteriorly and the lateral contact points were consistently more posterior than the medial side (Fig. 4A). This physiological contact kinematics patterns could be due to the complicated articular surface geometry and in vivo loading conditions of the knee. The morphological flexion axes measured more posteriorly positioned femoral condyles than the articular contact points. The TEA had largest ranges of femoral condyle translations that almost doubled the articular contact excursions since its location is more anterior and proximal than other flexion axes on the femoral condyles. All flexion axes measured paradoxical anterior translations of the medial condyle at low flexion angles (Fig. 4). The sharp increases in external femoral rotations at low flexion angles correspond to the condyle motion patterns measured using these flexion axes. The TEA only showed axial rotation center at medial side at low flexion angles due to the minimal translation of the medial condyle (Fig. 4B). Both GCA and IHA axes showed rotation centers at approximate tibial center due to similar magnitudes of anterior translations of the medial femoral condyle and posterior translations of the lateral femoral condyle at low flexion angles (Figs. 4C, D).
These data confirmed that selections of flexion axes could affect the measurements of the condyle translations and rotations. The morphological femoral condyle motions could not represent those of the articular contact points along the flexion path. In knee joint kinematics studies, TEA has been widely used since it can be conveniently identified using morphological landmarks on skin surfaces or X-ray images of the knee (Berger et al., 1993; Griffin et al., 2000; Victor, 2009; Yoshino et al., 2001). The GCA is determined using the posterior femoral condyle geometries. The IHA axis is established by minimizing the proximal-distal variations of the femoral condyles during knee flexion using accurate 3D imaging technique (Rao et al., 2020). It is critically important to clearly describe the reference coordinates when reporting knee kinematics. Surgical treatment of the knee may need to be evaluated on restoration of both morphological and physiological knee joint kinematics (Nakamura et al., 2015; Nicolet-Petersen et al., 2020).
There are several limitations in current study that should be noted. We only investigated a quasi-static single leg lunge. Future studies should measure in vivo knee joint motions under various dynamic loading conditions such as walking, stair-ascending and -descending. Morphometry of the knee was not measured and therefore, it is difficult to provide a geometric explanation of the measured knee kinematics. Future investigation should pursue a correlation between the geometric characteristics and kinematics patterns of the knee. Furthermore, the articular contact kinematics was measured using the centroids of the tibiofemoral cartilage overlapping areas along the flexion path. Accurate definition of articular contact kinematics is difficult due to the complicated cartilage structure including inhomogeneous thickness distribution and surface shape. Future investigation should develop knee computational models to consistently determine accurate articular contact kinematics. Despite these limitations, this study presented quantitative data of morphological and physiological kinematics of the knee during an in vivo weightbearing single leg lunge.
In summary, our data indicated that both medial and lateral contact points translate posteriorly with flexion and the medial side is more anterior than the lateral side. The data of femoral condyle translations and rotations are sensitive to the selection of morphological flexion axes. The morphological condyle motion did not accurately represent the physiological articular contact point motion. Biomechanical descriptions of the knee joint motion should include both physiological and morphological kinematics data to accurately demonstrate the functionality of the knee.
Acknowledgement
This work was partially supported by the NIH (R01 AR052408) and the Department of Orthopaedic Surgery at Newton-Wellesley Hospital.
Footnotes
Conflict of Interest
The authors declare that there is no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Asano T, Akagi M, Tanaka K, Tamura J, Nakamura T, 2001. In vivo three-dimensional knee kinematics using a biplanar image-matching technique. Clin Orthop Relat Res(388), 157–166. [DOI] [PubMed] [Google Scholar]
- Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS, 1993. Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res(286), 40–47. [PubMed] [Google Scholar]
- Churchill DL, Incavo SJ, Johnson CC, Beynnon BD, 1998. The transepicondylar axis approximates the optimal flexion axis of the knee. Clin Orthop Relat Res(356), 111–118. [DOI] [PubMed] [Google Scholar]
- Colle F, Bignozzi S, Lopomo N, Zaffagnini S, Sun L, Marcacci M, 2012. Knee functional flexion axis in osteoarthritic patients: comparison in vivo with transepicondylar axis using a navigation system. Knee Surg Sports Traumatol Arthrosc 20(3), 552–558. [DOI] [PubMed] [Google Scholar]
- Dabirrahmani D, Hogg M, 2017. Modification of the Grood and Suntay Joint Coordinate System equations for knee joint flexion. Med Eng Phys 39, 113–116. [DOI] [PubMed] [Google Scholar]
- DeFrate LE, Sun H, Gill TJ, Rubash HE, Li G, 2004. In vivo tibiofemoral contact analysis using 3D MRI-based knee models. J Biomech 37(10), 1499–1504. [DOI] [PubMed] [Google Scholar]
- Dennis DA, Mahfouz MR, Komistek RD, Hoff W, 2005. In vivo determination of normal and anterior cruciate ligament-deficient knee kinematics. J Biomech 38(2), 241–253. [DOI] [PubMed] [Google Scholar]
- Dimitriou D, Tsai TY, Park KK, Hosseini A, Kwon YM, Rubash HE, Li G, 2016. Weightbearing condyle motion of the knee before and after cruciate-retaining TKA: In-vivo surgical transepicondylar axis and geometric center axis analyses. J Biomech 49(9), 1891–1898. [DOI] [PubMed] [Google Scholar]
- Eckhoff D, Hogan C, DiMatteo L, Robinson M, Bach J, 2007. Difference between the epicondylar and cylindrical axis of the knee. Clin Orthop Relat Res 461, 238–244. [DOI] [PubMed] [Google Scholar]
- Feng Y, Tsai TY, Li JS, Rubash HE, Li G, Freiberg A, 2016. In-vivo analysis of flexion axes of the knee: Femoral condylar motion during dynamic knee flexion. Clin Biomech (Bristol, Avon) 32, 102–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin FM, Math K, Scuderi GR, Insall JN, Poilvache PL, 2000. Anatomy of the epicondyles of the distal femur: MRI analysis of normal knees. J Arthroplasty 15(3), 354–359. [DOI] [PubMed] [Google Scholar]
- Gromov K, Korchi M, Thomsen MG, Husted H, Troelsen A, 2014. What is the optimal alignment of the tibial and femoral components in knee arthroplasty? Acta Orthop 85(5), 480–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hull ML, 2020. Coordinate system requirements to determine motions of the tibiofemoral joint free from kinematic crosstalk errors. J Biomech 109, 109928. [DOI] [PubMed] [Google Scholar]
- Kozanek M, Hosseini A, Liu F, Van de Velde SK, Gill TJ, Rubash HE, Li G, 2009. Tibiofemoral kinematics and condylar motion during the stance phase of gait. J Biomech 42(12), 1877–1884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lerner ZF, DeMers MS, Delp SL, Browning RC, 2015. How tibiofemoral alignment and contact locations affect predictions of medial and lateral tibiofemoral contact forces. J Biomech 48(4), 644–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li G, Van de Velde SK, Bingham JT, 2008. Validation of a non-invasive fluoroscopic imaging technique for the measurement of dynamic knee joint motion. J Biomech 41(7), 1616–1622. [DOI] [PubMed] [Google Scholar]
- Li G, Wuerz TH, DeFrate LE, 2004. Feasibility of using orthogonal fluoroscopic images to measure in vivo joint kinematics. J Biomech Eng 126(2), 314–318. [DOI] [PubMed] [Google Scholar]
- Li JS, Hosseini A, Cancre L, Ryan N, Rubash HE, Li G, 2013. Kinematic characteristics of the tibiofemoral joint during a step-up activity. Gait Posture 38(4), 712–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannel H, Marin F, Claes L, Durselen L, 2004. Establishment of a knee-joint coordinate system from helical axes analysis--a kinematic approach without anatomical referencing. IEEE Trans Biomed Eng 51(8), 1341–1347. [DOI] [PubMed] [Google Scholar]
- Miranda DL, Rainbow MJ, Leventhal EL, Crisco JJ, Fleming BC, 2010. Automatic determination of anatomical coordinate systems for three-dimensional bone models of the isolated human knee. J Biomech 43(8), 1623–1626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mochizuki T, Sato T, Blaha JD, Tanifuji O, Kobayashi K, Yamagiwa H, Watanabe S, Koga Y, Omori G, Endo N, 2014. The clinical epicondylar axis is not the functional flexion axis of the human knee. J Orthop Sci 19(3), 451–456. [DOI] [PubMed] [Google Scholar]
- Most E, Axe J, Rubash H, Li G, 2004. Sensitivity of the knee joint kinematics calculation to selection of flexion axes. J Biomech 37(11), 1743–1748. [DOI] [PubMed] [Google Scholar]
- Mu S, Moro-Oka T, Johal P, Hamai S, Freeman MA, Banks SA, 2011. Comparison of static and dynamic knee kinematics during squatting. Clin Biomech (Bristol, Avon) 26(1), 106–108. [DOI] [PubMed] [Google Scholar]
- Nakamura S, Ito H, Yoshitomi H, Kuriyama S, Komistek RD, Matsuda S, 2015. Analysis of the Flexion Gap on In Vivo Knee Kinematics Using Fluoroscopy. J Arthroplasty 30(7), 1237–1242. [DOI] [PubMed] [Google Scholar]
- Nicolet-Petersen S, Saiz A, Shelton T, Howell SM, Hull ML, 2020. Small differences in tibial contact locations following kinematically aligned TKA from the native contralateral knee. Knee Surg Sports Traumatol Arthrosc 28(9), 2893–2904. [DOI] [PubMed] [Google Scholar]
- Oussedik S, Scholes C, Ferguson D, Roe J, Parker D, 2012. Is femoral component rotation in a TKA reliably guided by the functional flexion axis? Clin Orthop Relat Res 470(11), 3227–3232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinskerova V, Johal P, Nakagawa S, Sosna A, Williams A, Gedroyc W, Freeman MA, 2004. Does the femur roll-back with flexion? J Bone Joint Surg Br 86(6), 925–931. [DOI] [PubMed] [Google Scholar]
- Qi W, Hosseini A, Tsai TY, Li JS, Rubash HE, Li G, 2013. In vivo kinematics of the knee during weight bearing high flexion. J Biomech 46(9), 1576–1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao Z, Zhou C, Zhang Q, Kernkamp WA, Wang J, Cheng L, Foster TE, Bedair HS, Li G, 2020. There are isoheight points that measure constant femoral condyle heights along the knee flexion path. Knee Surg Sports Traumatol Arthrosc. [DOI] [PMC free article] [PubMed]
- Renault JB, Aullo-Rasser G, Donnez M, Parratte S, Chabrand P, 2018. Articular-surface-based automatic anatomical coordinate systems for the knee bones. J Biomech 80, 171–178. [DOI] [PubMed] [Google Scholar]
- Tanifuji O, Sato T, Kobayashi K, Mochizuki T, Koga Y, Yamagiwa H, Omori G, Endo N, 2013. Three-dimensional in vivo motion analysis of normal knees employing transepicondylar axis as an evaluation parameter. Knee Surg Sports Traumatol Arthrosc 21(10), 2301–2308. [DOI] [PubMed] [Google Scholar]
- Victor J, 2009. Rotational alignment of the distal femur: a literature review. Orthop Traumatol Surg Res 95(5), 365–372. [DOI] [PubMed] [Google Scholar]
- Walker PS, Heller Y, Yildirim G, Immerman I, 2011. Reference axes for comparing the motion of knee replacements with the anatomic knee. Knee 18(5), 312–316. [DOI] [PubMed] [Google Scholar]
- Yin P, Li JS, Kernkamp WA, Tsai TY, Baek SH, Hosseini A, Lin L, Tang P, Li G, 2017. Analysis of in-vivo articular cartilage contact surface of the knee during a step-up motion. Clin Biomech (Bristol, Avon) 49, 101–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshino N, Takai S, Ohtsuki Y, Hirasawa Y, 2001. Computed tomography measurement of the surgical and clinical transepicondylar axis of the distal femur in osteoarthritic knees. J Arthroplasty 16(4), 493–497. [DOI] [PubMed] [Google Scholar]