Abstract
Background
Warm acupuncture, a combination of the mechanical stimulation of acupuncture and thermal stimulation of moxibustion, is commonly used in treating acute low back pain (LBP). This trial aimed to compare the efficacy of stronger (above 43°C) and weaker (above 40°C) heat stimulation in warm acupuncture on the function and pain in patients with acute LBP due to lumbosacral disc degeneration (LDD).
Methods
One hundred and fifty-nine adults were randomly assigned to receive warm acupuncture treatment with silver needle (SvN) or with stainless steel needle (SSN) (1:1). Both groups received a 3-week therapy with 3 sessions per week. The primary outcome was the modified Oswestry Disability Index at week 4. The secondary outcomes included average pain, three physical sign tests and adverse events. Participants were followed up at week 16 and week 28 after randomization.
Results
The LBP related disability and pain intensity significantly relieved more in the SvN warm acupuncture group than in the SSN group, in both the short and long term (p<0.001). The between-groups difference in physical signs showed statistical significance only in the short term (p = 0.024), but not in long term (p = 0.081; p = 0.069).
Conclusion
Compared with warm acupuncture with stainless-steel needle at above 40°C, warm acupuncture with silver needle at above 43°C relieved more disability and pain in patients with acute LBP due to LDD.
Study registration
Chinese Clinical Trial Registry (ChiCTR1800019051)
Keywords: Low back pain, Lumbosacral disc degeneration, Acupuncture therapy, Nociception, Heat stimulation
1. Introduction
Acute Low Back Pain (LBP) is mostly caused by lumbosacral disc degeneration (LDD) when the structural correlate is confirmed (80~89%)1,2. It causes variable clinical duration and is prone to develop chronic syndrome3, 4, 5, 6 in up to 10% of the affected population7,8. The one-year recurrence rate in cases with sciatica is up to 25%9. The Chinese Consensus on Rehabilitation of Lumbar Disc Herniation (version 2017)10 suggests non-surgical interventions as the first-line therapy for about 80–90% of LBP onsets.
Acupuncture and moxibustion are among the non-surgical therapy for acute LBP. The 2017 Clinical Practice Guideline from the American College of Physicians recommended to use acupuncture and superficial heat in the management of acute LBP with low and moderate quality evidence11. Warm acupuncture in traditional Chinese medicine (TCM) is a combination of acupuncture and moxibustion. It combines both the mechanical stimulation from needle and the thermal stimulation from moxibustion, and is considered to be a good choice in treating musculoskeletal disorders according to the documentation in Yellow Emperor's Canon of Internal Medicine-Miraculous Pivot (Huang Di Nei Jing-Ling Shu), one of the most important TCM classics. It's also considered a promising therapy for LBP due to LDD in TCM12. Temperature is considered as an essential factor in warm acupuncture13. However, due to the poor thermal conductivity of commonly used stainless-steel needle (SSN), the heat stimulation is usually low with the temperature of about 41.7 °C at the skin13 and lower in the intramuscular part. Our previous study showed that silver needle acupuncture was superior than stainless-steel needle acupuncture when both combined with traditional moxibustion in treating LBP due to lumbar disc herniation14, which indicated higher heat stimulation may cause more benefit. Our other study also found that silver needle (SvN) produced stronger thermal stimulation compared to needles made of other metallic material13, and the initial heat pain threshold of 43°C to 47°C is a safe and suitable range in warm acupuncture for people. The aim for this trial was to investigate whether warm acupuncture with silver needle at above 43°C is effective and safe in reducing disability and pain in patients with acute LBP due to LDD compared with warm acupuncture with usual stainless-steel needle at lower temperature.
2. Methods
2.1. Trial design
This was a randomized, patient- and assessor-blinded trial with two parallel arms (1:1), conducted in three independent centers (Outpatient Clinic of Acupuncture and Moxibustion in Longhua Hospital, Baoshan Hospital of Integrated Traditional Chinese and Western Medicine, and Shanghai Pudong Hospital of TCM) from December 2018 to January 2020. The trial consisted of a 3-week intervention and an additional 25-week follow-up. This trial was approved by the Ethics Committee of Shanghai Pudong Hospital of TCM and was registered on the Chinese Clinical Trial Registry (ChiCTR) (Registration number: ChiCTR1800019051).
2.2. Sample size
The sample size was calculated based on a previous RCT with the same comparison15. According to the result that the post-treatment mODI score (x ± S) decreased to 26.29 ± 18.02 in the silver needle group, and 34.58 ± 15.10 in the stainless-steel needle group, a sample size of 128 participants (64 for each group) would be acceptable to detect a similar difference between the two groups to achieve a 2-sided 5% significance level with at least 80% power. Considering possible attrition (i.e., 20% dropout) during the trial, a total of 160 patients were needed.
2.3. Randomization and blinding
We used a central randomization system by which the allocation was dynamically balanced by study sites. Randomization sequence was generated using SPSS Statistics (version 22.0). When a candidate was enrolled, the allocation assistant in each center called the central coordinator who ran the central randomization system for the participant's ID number and group allocation. Only acupuncturists were informed of the participant's group allocation via email. Outcome assessors and statisticians were not informed of the group allocation of the participants. Participants were informed different types of warm acupuncture were studied, but were not told the differences of the two treatments.
2.4. Participants
One hundred and eighty patients aged from 20 ~ 70 years were recruited from December 2018 to November 2019, through the official homepage of involved hospitals, bulletin boards, and fliers in nearby community.
Participants were included if they (1) presented all the following symptoms and signs confirmed by orthopedists in each center: a) LBP with or without lower extremity pain for no more than 12 weeks; b) the presence of nerve root entrapment, including Paresthesia, Dysreflexia, low Myodynamia, or muscle atrophy in the affected lower extremity; c) paravertebral tenderness, limited range of forward bending and a positive Lasegue' s sign or Mackiewicz' s sign; (2) had computed tomography or magnetic resonance imaging scan evidence supporting a confirmed LDD which resulted in all the symptoms and signs presented; (3) reported Visual Analogue Scale (VAS) pain score ≥ 5 at the visit; (4) met the criteria for Cold-Dampness-Bi syndrome according to the TCM diagnosis16. The exclusion criteria were (1) LDD with comorbidities including spinal tumor, Cauda Equina nerve damage, lumbar spinal stenosis, lumbar Spondylolisthesis, Ankylosing spondylitis, sciatica of the nerve trunk lesion, Piriformis syndrome, spinal infection or any other situation that might cause peripheral neuropathy; (2) life-threatening complication or contraindication to acupuncture therapy; (3) experience of other conservative and surgical therapy for LDD in the past two months; (4) pregnancy or lactation.
All participants were informed of the purpose, study procedure, and any potential risks during the trial before signing the informed consent forms. To improve patient's adherence, the participants who finished the whole treatment were subsidized (200 RMB / person).
2.5. Study interventions
The warm acupuncture was performed with moxibustion devices and acupuncture needles. The acupuncture needles used in the SvN group were strictly sterilized reusable silver needles (0.40 mm*75 mm, 70% pure silver, Hwato Medical Material Co., Ltd., Suzhou, China), and in the SSN group were disposable stainless steel filiform needles (0.40 mm*75 mm, Jiajian Medical Material Co., Ltd., Wuxi, China). The specially designed moxibustion device (DAJ-23, XiangHe Chinese Traditional Medicine Instruments Co., Ltd., Heilongjiang, China) consisted of a ceramic heating part at the top and a cork layer at the bottom as an insulation preventing the heat transfer from the upper heating part to the skin. In the middle of the cork layer, there is a thin copper tube that can be inserted in the upper heating part. After the acupuncture needle was inserted in the body, the moxibustion device was put through the needle on the skin, with the needle in the copper tube. When the device was turned on, the heat from the upper heating part transferred to the copper tube then to the needle. We applied eight moxibustion devices on the main points at the lumbar region during treatment. (Supplement 1).
Needles were inserted vertically to a depth of 30~50 mm, and manipulated manually until "Deqi" sensation was obtained. The device's output temperature was set and kept stable at about 50°C. The temperature at the skin surface at the site of needle was detected as about 43°C in the SvN group and about 40°C in the SSN group after immediate removal of the moxibustion device with a thermal camera (FLIR ONE pro, version 3.0, FLIR Systems, Inc.) (Supplement 2). Thus the actual temperature during warm acupuncture with the heating device on should be higher than that detected after immediate removal of the heating device (i.e., above 43°C in the SvN group and above 40°C in the SSN group at the acupuncture site).
Each treatment session was about 25 min with the heating up procedure at the first 5 min. The treatments were performed 3 times a week for 3 weeks with a total of 9 sessions. The room temperature was kept at 25 ± 0.8 °C during treatment.
Points of bilateral BL23, BL25, and BL54 and unilateral EX-B2 15/16 of the affected side were chosen (Supplement 3) in the treatment for LDD with cold-dampness syndrome based on TCM theory and literature review17. A pair of additional acupoints might be added according to patients’ individual symptoms or signs.
Four qualified acupuncturists, each with the acupuncture practice of at least ten years, did the treatment. They were trained by the chief coordinator in the treatment regimen as well as in the management and reporting of the adverse events during treatment.
During the trial, patients were required to not to take analgesia or alcohol in the past 24 h before treatment, or the appointment would be canceled and postponed. Patients were also recommended to avoid lumbar exertion in daily life and have more rest.
2.6. Outcome measurements
The patients were assessed at baseline and at week 4 (one week after the end of treatment), 16 and 24.
2.6.1. Primary outcome
The primary outcome was the self-assessed modified Oswestry Disability Index (mODI) in Chinese version18, which was responsive in evaluating LBP related disability, including symptom severity, functional activity, and behavioral performance. The score of mODI was in form of percentage ranging from 0 (no disability) to 100 (most crippled).
2.6.2. Secondary outcomes
The average pain intensity of the low back in the past 7 days was measured by VAS (from 0 to 10; 0: no pain, 1~3: mild pain, 4~6: moderate pain, 7~10 severe pain; >3 indicates medical management is needed)19.
Physical signs, including straight leg raising test or femoral nerve stretch test, radiation pain sensory disturbance and muscle weakness, were evaluated with three physician-assessed items in Japanese Orthopedic Association Back Pain Evaluation Questionnaire (JOABPEQ)20. The higher score indicates the less severe physical signs. The other items in JOABPEQ overlapping with mODI were not measured to avoid repetition.
Participants' expectancy and rationale credibility for the treatment was evaluated by a specific credibility/expectancy questionnaire21 immediately after the first treatment.
Incidence of adverse effects, whether related to treatment or not, were documented at each visit and during follow up.
2.7. Statistical methods
All data were double-entered into a password-protected database. The data and safety monitoring board (DSMB) had free access to audit and investigate the individual participant data (IPD).
The primary analysis compared the 4-week mODI score between the two groups in all patients whose 4-week data were available. To compare the two groups on the demographic and baseline characteristics, we used chi square test for categorical data, and 2-sample t-test or Mann-Whitney U test for continuous data, depending on whether the data are normally distributed. To compare the primary (mODI) and secondary endpoints (mODI score at other time points, average VAS pain, physical signs score and participants’ credibility and expectancy) at each time point, two-sample t-test or Mann-Whitney U test was performed. All statistical analyses were performed using SPSS (version 22.0, IBM Corp., Armonk, NY). All reported p values were two sided and a significance level of 0.05 was used.
3. Results
3.1. Demographic characteristics
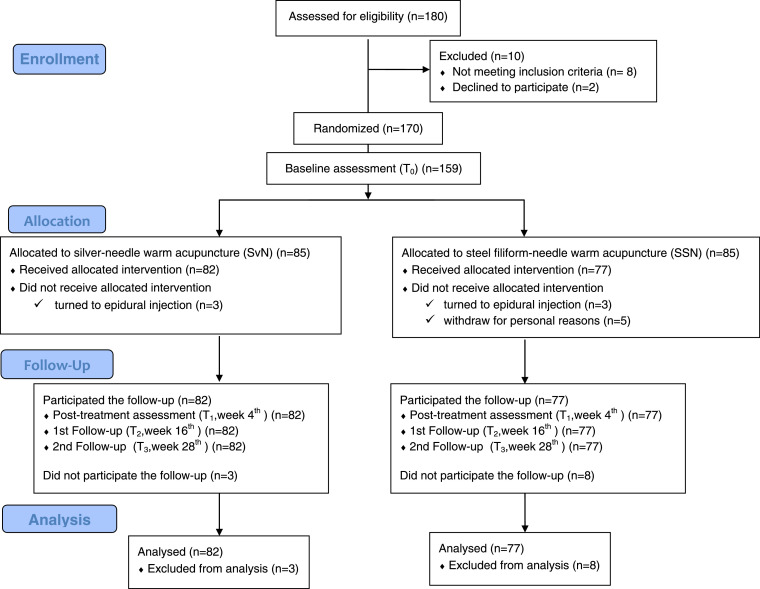
One hundred and seventy out of 180 candidates were enrolled in this trial and randomly assigned to SvN (n = 85) or SSN group (n = 85). Eleven dropouts failed to finish the treatment (6 shifted to epidural injection before the first visit, and other 5 ceased after the first treatment for personal reasons), and 159 patients (93.5%) completed the trial (Fig. 1).
Fig. 1.
Flow chart of the study process (adapted from the CONSORT flow chart).
The baseline characteristics were comparable between the groups (Table 1). No statistically significant between-group difference was found in age, sex, BMI, disease duration, occurrence of leg pain, affected level, mODI, average VAS pain, 3 physical signs in JOABPEQ as well as patients’ expectancy and rationale credibility
Table 1.
Demographic and Baseline Characteristics of the participants
| Characteristics | SvN group (N = 82) | SSN group (N = 77) | p value |
|---|---|---|---|
| Age (yrs, ± SD) | 47.01 ± 11.57 | 46.39 ± 12.34 | 0.743 |
| Sex (N) | 0.875 | ||
| male | 32 | 31 | |
| female | 50 | 46 | |
| BMI (kg/m2, ± SD) | 23.93 ± 3.157 | 24.04 ± 2.92 | 0.817 |
| Duration (wks, median, interquartile range) | 3 (2–6) | 4 (2–6) | 0.417 |
| Occurrence of leg pain (N, %) | 79 (96.3) | 69 (87.3) | 0.095 |
| Affected levels (N, %) | |||
| L2–L3 | 1 (1.2) | 0 (0) | |
| L3–L4 | 40 (48.8) | 32 (41.5) | |
| L4–L5 | 72 (88.8) | 61 (79.2) | |
| L5–S1 | 76 (92.7) | 72 (93.5) | |
| Participants’ expectancy and rationale credibility | |||
| (median, interquartile range) | 21 (8.4–29.6) | 20 (10.4–27.2) | 0.062 |
| mODI (%) | 50 (40–64) | 56 (42–62) | 0.329 |
| Average VAS pain | 7 (7–8) | 7 (6–8) | 0.087 |
| 3 physical signs in JOABPEQ | 4 (3–4) | 4 (3–4) | 0.123 |
BMI, body mass index; JOABPEQ, Japanese Orthopedic Association Back Pain Evaluation Questionnaire; mODI, modified Oswestry Disability Index; N, number; SD, standard deviation; SvN, silver needle; SSN, stainless-steel filiform needle; VAS, Visual Analogue Scale; wks, weeks; yrs, years.
3.2. Outcomes
3.2.1. Primary outcomes
At week 4, less disability in mODI of 8% (2%–18%) was reported in patients receiving SvN group compared with that of 30% (20%–42%) in SSN group, and the difference between the two groups was significantly different (18%; 95% confidence interval [CI], 14% to 23%; p < 0.001) (Table 2).
Table 2.
The mODI, VAS pain, and Physical examination score in JOABPEQ of the participants
| Week | SvN group (n = 82) | SSN group (n = 77) | Difference (95% CI) | p value | |
|---|---|---|---|---|---|
| mODI (%) | 4 | 8 (2–18) | 30 (20–42) | 18 (14, 23) | <0.001 |
| 16 | 7 (2–18) | 26 (18–42) | 17 (12, 22) | <0.001 | |
| 28 | 10 (2–20) | 26 (18–42) | 16 (11, 20) | <0.001 | |
| Average VAS pain | 4 | 1 (0–2) | 4 (2–5) | 3 (1.6, 2.7) | <0.001 |
| 16 | 1 (0–2) | 4 (2–5) | 2 (1.4, 2.4) | <0.001 | |
| 28 | 1 (0–3) | 4 (2–5) | 3 (1.1, 2.1) | <0.001 | |
| 3 physical signs in JOABPEQ | 4 | 5.5 (5–6) | 5 (5–6) | 0 (0, 1) | 0.024 |
| 16 | 6 (5–6) | 5 (5–6) | 0 (-0.59, 0.02) | 0.081 | |
| 28 | 6 (5–6) | 5 (5–6) | 0 (-0.55, 0.08) | 0.069 |
IQR, interquartile range; JOABPEQ, Japanese Orthopedic Association Back Pain Evaluation Questionnaire; ODI, Oswestry Disability Index; SvN, silver needle; SSN, stainless-steel needle; VAS, Visual Analogue Scale.
3.2.2. Secondary outcomes
MODI at the follow-ups (week 16 and 28) were also significantly better in patient treating with SvN warm acupuncture than those with SSN warm acupuncture (p < 0.001) (Table 2). The patients in the SvN group reported less average VAS pain than those in the SSN group at all time points (p < 0.001) (Table 2). The patients receiving SvN warm acupuncture were evaluated to have less severe physical signs in JOABPEQ at only week 4 (p = 0.024), and the superiority did not seem to continue at the follow-up week 16 and 28 (p = 0.081 and p = 0.069) (Table 2).
3.2.3. Adverse events
No serious adverse events were reported in both groups during the study. The common minor adverse events included mild bruise, pain, soreness, or numbness at the acupuncture site in both groups.
4. Discussion
Our study found that a total of 3 weeks with thrice weekly treatments of silver needle warm acupuncture at 43°C showed better effect in relieving LBP related disability and pain compared with stainless steel needle warm acupuncture at 40°C. The effect remained up to 25 weeks after the end of treatment, while the effect of warm acupuncture with silver needle over stainless steel needle in improving LBP physical signs did not prolong after treatment. The findings are similar to those of other previous studies15,22,23. However, in these studies, the temperature of the warm acupuncture were not measured, and they also had methodological flaws such as small sample size and inadequate follow-up time15,22,23. The strength of our treatment was that we used a modern moxibustion device rather than the traditional ignited moxa to warm the needle. The moxibustion device is more convenient to operate, and can provide safer, steadier and controllable heat stimulation. The temperature was set steady to produce enough heat stimulation (above 43°C in silver needle warm acupuncture, and above 40°C in stainless steel needle warm acupuncture) while not cause burn at skin.
We speculated that the temperature of about 43°C and over at the skin surface could be an important peripheral mechanism involved in the better pain relief effect in the SvN group. The temperature over 43 °C is the main activators of TRPV1 (transient receptor potential cation channel subfamily V member 1, expressed on the free nerve endings of both C-fiber and Aδ-fiber24,25) and the response threshold of afferent Aδ-fiber and C-fiber nociceptors26, 27, 28. TRPV1 and C-fiber play the essential role in the peripheral afferent mechanism in the analgesia of thermal stimulation. Research noticed that the thermal stimulation of 38°C at acupoint only produced local analgesia, while thermal stimulation of 43°C and 46°C produced systematic and stronger analgesia. Such systematic analgesia effect disappeared and the local analgesia effect significantly weakened in TRPV1 knockout mice29. These findings all suggested the involvement of TRPV1 and C-fiber in the peripheral afferent mechanism in the analgesia of thermal stimulation.
In addition, there was another central mechanism of heat stimulation at 43 °C in the endogenous descending modulation of nociception. In LDD induced LBP, the mechanical impingement of lumbosacral nerve root fibers and subsequent inflammatory mediator release heightened the peripheral nociceptive activity. The further sensitization (i.e., the secondary hyperalgesia) in the area surrounding the primary injury site arose, followed by the enhanced central nociceptive responses (i.e., the generalized hyperalgesia) particularly within supraspinal regions30, 31, 32. Heat stimulation at 43 °C occurred in the area involving the secondary hyperalgesia might effectively control the pain by eliciting the descending inhibition pathway alone33. This supraspinal discriminator-mediated descending system is physiologically inactive, but it can have a robust control of pain once triggered by the sufficient C-afferent inputs34. Heat stimuli preferentially activate the C- nociceptors29, and the acupoint area may contain the denser distribution of C- fibers35,36. In the light of these researches, warm acupuncture at 43 °C by SvN on responsive acupoints might gain its edge in triggering descending inhibitory modulation alone to bring about antinociception.
Our study indicated that stronger heat stimulation (above 43°C) in warm acupuncture resulted in better effect for acute LBP, which is more easily to achieve by using silver needle. Although silver needle is not commonly used in modern acupuncture practice, due to its higher cost and the need in sterilization, its better thermal conductivity makes it superior in combining the effects of acupuncture and moxibustion, especially in treating musculoskeletal disorders. In the practice of the silver needle warm acupuncture, the practitioners should be careful in controlling the temperature above the heat pain threshold of 43°C but not cause burn, as well as in sterilization to avoid infection. To make warm acupuncture more applicable in the clinic, new types of sterilized needle with lower cost and similar thermal conductivity is warranted.
Our study has some limitations. First, the number of participants recruited from each of the three clinical sites varied, which might introduce selection bias. Second, the actual temperature of the needle in the body were not measured due to the defect of the measurement tool. Third, the sample size is not large enough to do subgroup analysis. The last, we haven't evaluated the change of other radicular symptom specific to LDD other than pain.
In conclusion, SvN warm acupuncture produced more heat stimulation and resulted in better clinical effects in reducing disability and relieving pain in patients with LBP due to LDD, compared with SSN warm acupuncture. The heat stimulation above 43°C in SvN warm acupuncture may contribute to the superiority.
Acknowledgments
Acknowledgments
We would like to thank Dr. Yanwen Song, Dr. Kangze Cao, Dr. Huimin Sheng, Dr. Liping Cheng, and Dr. Shu Wang for their dedication to this study.
Author contributions
The trial was designed by TL and ZQH, and improved by KC. LS, DPJ took charge of data analysis. KC and TL drafted the manuscript, which was carefully discussed and revised by SYW, ZY and SZ. All authors had read and approved the final manuscript.
Conflict of interest
The authors declare no conflict of interests.
Funding
This research was funded by the Pudong New Area Health Commission, Shanghai, China (PDZY-2018-0610, PWRd2018-03); Three-Year Development Plan Project for Traditional Chinese Medicine of Shanghai Municipal Health Commission (ZY (2018-2020)-CCCX-2001-05).
Ethical statement
This RCT was approved by the Ethics Committee of Shanghai Pudong Hospital of TCM and registered on the Chinese Clinical Trial Registry. Informed consent was obtained from all participants.
Data availability
The data that support the findings of this study will be upload to ResMan Research Manager of the Clinical Trial Management Public Platform for public share as long as the fund board check and accept our program completion (anticipated on March 2021).
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.imr.2021.100748.
Contributor Information
Ke Cheng, Email: cheng_ker@hotmail.com.
Zouqin Huang, Email: pzyzjk@163.com.
Appendix. Supplementary materials
Reference
- 1.Ostenfeld T, Krishen A, Lai RY. A randomized, placebo-controlled trial of the analgesic efficacy and safety of the p38 MAP kinase inhibitor, losmapimod, in patients with neuropathic pain from lumbosacral radiculopathy. Clin J Pain. 2015;31(4):283–293. doi: 10.1097/AJP.0000000000000122. [DOI] [PubMed] [Google Scholar]
- 2.Suri P, Rainville J, Katz JN. The accuracy of the physical examination for the diagnosis of midlumbar and low lumbar nerve root impingement. Spine (Phila Pa 1976) 2011;36(1):63–73. doi: 10.1097/BRS.0b013e3181c953cc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frymoyer JW, Pope MH, Clements JH. Risk factors in low-back pain. An epidemiological survey. J Bone Joint Surg Am. 1983;65(2):213–218. doi: 10.2106/00004623-198365020-00010. [DOI] [PubMed] [Google Scholar]
- 4.Hicks GE, Gaines JM, Shardell M. Associations of back and leg pain with health status and functional capacity of older adults: findings from the retirement community back pain study. Arthritis Rheum. 2008;59(9):1306–1313. doi: 10.1002/art.24006. [DOI] [PubMed] [Google Scholar]
- 5.Konstantinou K, Dunn KM. Sciatica: review of epidemiological studies and prevalence estimates. Spine (Phila Pa 1976) 2008;33(22):2464–2472. doi: 10.1097/BRS.0b013e318183a4a2. [DOI] [PubMed] [Google Scholar]
- 6.Valat JP, Genevay S, Marty M. Sciatica. Best Pract Res Clin Rheumatol. 2010;24(2):241–252. doi: 10.1016/j.berh.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 7.Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet. 2017;389(10070):736–747. doi: 10.1016/S0140-6736(16)30970-9. [DOI] [PubMed] [Google Scholar]
- 8.Majid K, Truumees E. Epidemiology and natural history of low back pain. Semin Spine Surg. 2008;20(2):87–92. [Google Scholar]
- 9.Suri P, Rainville J, Hunter DJ. Recurrence of radicular pain or back pain after nonsurgical treatment of symptomatic lumbar disk herniation. Arch Phys Med Rehabil. 2012;93(4):690–695. doi: 10.1016/j.apmr.2011.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhou M, YS He C. Chinese consensus on rehabilitation of lumbar disc herniation. Chinese Rehabil Med. 2017;32(2):129–135. [Google Scholar]
- 11.Whyman J D, Leipzig R M. Noninvasive treatments for acute, subacute, and chronic low back pain. Ann Intern Med. 2017;167(11):834. doi: 10.7326/L17-0473. [DOI] [PubMed] [Google Scholar]
- 12.Zhu YM, ZT Tian QH. The recent progress of TCM in treating lumbar disc herniation. J Emerg Traditional Chin Med. 2018;27(1):175–177. [Google Scholar]
- 13.Lin L, Cheng K, Shen XY. Analysis on the temperature-time curve in warm needling manipulation with acupuncture needles of different materials. Chin Acupunc Moxib. 2019;39(12):1301–1307. doi: 10.13703/j.0255-2930.2019.12.012. [DOI] [PubMed] [Google Scholar]
- 14.Huang ZQ, Zhang S, Wang WM. Observations on the Efficacy of Silver Needle Acupuncture plus Instrumental Ginger Moxibustion in treating lumbar intervertebral disc herniation. Shanghai J Acu-mox. 2017;36(002):193–197. [Google Scholar]
- 15.Li W, XH Wang H, Huang J. Clinical analysis of a composite treatment with silver needles for lumbar intervertebral disc herniation. Shanghai J Acupunct Moxibustion. 2014;33(4):356–359. [Google Scholar]
- 16.Vol. 2. Nan Jing. Nanjing University Press; 1995. Chinese state administration of taditional Chinese Medicine; p. 199. (Criteria of diagnosis and therapeutic effect of disease and syndromes in TCM). [Google Scholar]
- 17.Yanan Bai DZ. Preliminary study on ancient and modern regularity of acupuncture treatment in lumbar disc herniation. Liaoning J Tradit Chinese Med. 2016;43(2):373–376. [Google Scholar]
- 18.Cheng JW, Wang ZL, Liu W. Improvement of Oswestry disability index and its test of reliability and validity. Chinese J Spine Spinal Cord. 2017;27(3):235–241. [Google Scholar]
- 19.Sun B, Che X. Visual Analogue Scale (VAS) Chinese Journal of Neurosurgery. 2012;28(6):645. [Google Scholar]
- 20.Tominaga R, Sekiguchi M, Yonemoto K. Establishment of reference scores and interquartile ranges for the Japanese Orthopaedic Association Back Pain Evaluation Questionnaire (JOABPEQ) in patients with low back pain. J Orthop Sci. 2018;23(4):643–648. doi: 10.1016/j.jos.2018.03.010. [DOI] [PubMed] [Google Scholar]
- 21.Devilly GJ, Borkovec TD. Psychometric properties of the Credibility/Expectancy Questionnaire. J Behav Ther Exp Psychiatry. 2000;31(2):73–86. doi: 10.1016/s0005-7916(00)00012-4. [DOI] [PubMed] [Google Scholar]
- 22.Zhang JJ, Liu XX, Zhang LH. Clinical observation of silver needle in the treatment of lumbar disc herniation of blood stasis type. Chin Manip Rehabil Med. 2020;11(18):17–19. [Google Scholar]
- 23.Zhou XJ. Clinical observation of thick silver needle in the treatment of lumbar disc herniation. Chin Commun Doctors. 2011;13(24):193–194. [Google Scholar]
- 24.Bevan S, Quallo T, Trpv1 Andersson DA. Handb Exp Pharmacol. 2014;222:207–245. doi: 10.1007/978-3-642-54215-2_9. pmid:24756708. [DOI] [PubMed] [Google Scholar]
- 25.Purves Dale. 5. ed. Sinauer; Sunderland, Mass: 2011. Neuroscience. pp. 211–21s2. ISBN 978-0-87893-695-3. [Google Scholar]
- 26.Andrew D, Greenspan JD. Mechanical and heat sensitization of cutaneous nociceptors after peripheral inflammation in the rat [J] J Neurophysiol. 1999;82(5):2649–2656. doi: 10.1152/jn.1999.82.5.2649. [DOI] [PubMed] [Google Scholar]
- 27.McMullan S, Lumb BM. Spinal dorsal horn neuronal responses to myelinated versus unmyelinated heat nociceptors and their modulation by activation of the periaqueductal grey in the rat[J] J Physiol. 2006;576(2):547–556. doi: 10.1113/jphysiol.2006.117754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cain DM, Khasabov SG, Simone DA. Response properties of mechanoreceptors and nociceptors in mouse glabrous skin: an in vivo study[J] J Neurophysiol. 2001;85(4):1561–1574. doi: 10.1152/jn.2001.85.4.1561. [DOI] [PubMed] [Google Scholar]
- 29.Xin JJ, Su YS, Yang ZK. Effects of electroacupuncture and regional thermal stimulation at "Zusanli" (ST 36) on pain thresholds of TRPV 1 knock-out mice. Zhen Ci Yan Jiu. 2012 Dec;37(6):431–439. [PubMed] [Google Scholar]
- 30.Campbell CM, Edwards RR. Mind-body interactions in pain: the neurophysiology of anxious and catastrophic pain-related thoughts. Transl Res. 2009;153(3):97–101. doi: 10.1016/j.trsl.2008.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Giesecke T, Gracely RH, Grant MA. Evidence of augmented central pain processing in idiopathic chronic low back pain. Arthritis Rheum. 2004;50(2):613–623. doi: 10.1002/art.20063. [DOI] [PubMed] [Google Scholar]
- 32.Nijs Jo, Torres-Cueco Rafael, Paul van Wilgen C. Applying modern pain neuroscience in clinical practice: criteria for the classification of central sensitization pain. Pain Physician. 2014;17(5):447–457. [PubMed] [Google Scholar]
- 33.Lei J, Ye G, Wu JT, Pertovaara A, You HJ. Role of capsaicin- and heat-sensitive afferents in stimulation of acupoint-induced pain and analgesia in humans. Neuroscience. 2017;358:325–335. doi: 10.1016/j.neuroscience.2017.06.051. [DOI] [PubMed] [Google Scholar]
- 34.You HJ, Lei J, Sui MY. Endogenous descending modulation: spatiotemporal effect of dynamic imbalance between descending facilitation and inhibition of nociception. J Physiol. 2010;588(Pt 21):4177–4188. doi: 10.1113/jphysiol.2010.196923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Freynhagen R, Rolke R, Baron R. Pseudoradicular and radicular low-back pain–a disease continuum rather than different entities? answers from quantitative sensory testing. Pain. 2008;135(1–2):65–74. doi: 10.1016/j.pain.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 36.Markman JD, Czerniecka-Foxx K, Khalsa PS. AAPT Diagnostic Criteria for Chronic Low Back Pain [published online ahead of print, 2020 Feb 6] J Pain. 2020 doi: 10.1016/j.jpain.2020.01.008. S1526-5900(20)30009-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study will be upload to ResMan Research Manager of the Clinical Trial Management Public Platform for public share as long as the fund board check and accept our program completion (anticipated on March 2021).