Summary
Background
Patient-facing (frontline) health-care workers (HCWs) are at high risk of repeated exposure to SARS-CoV-2.
Aim
We sought to determine the association between levels of frontline exposure and likelihood of SARS-CoV-2 seropositivity amongst HCW.
Methods
A cross-sectional study was undertaken using purposefully collected data from HCWs at two hospitals in London, United Kingdom (UK) over eight weeks in May–June 2020. Information on sociodemographic, clinical and occupational characteristics was collected using an anonymised questionnaire. Serology was performed using split SARS-CoV-2 IgM/IgG lateral flow immunoassays. Exposure risk was categorised into five pre-defined ordered grades. Multivariable logistic regression was used to examine the association between being frontline and SARS-CoV-2 seropositivity after controlling for other risks of infection.
Findings
615 HCWs participated in the study. 250/615 (40.7%) were SARS-CoV-2 IgM and/or IgG positive. After controlling for other exposures, there was non-significant evidence of a modest association between being a frontline HCW (any level) and SARS-CoV-2 seropositivity compared to non-frontline status (OR 1.39, 95% CI 0.84–2.30, P=0.200). There was 15% increase in the odds of SARS-CoV-2 seropositivity for each step along the frontline exposure gradient (OR 1.15, 95% CI 1.00–1.32, P=0.043).
Conclusion
We found a high SARS-CoV-2 IgM/IgG seropositivity with modest evidence for a dose-response association between increasing levels of frontline exposure risk and seropositivity. Even in well-resourced hospital settings, appropriate use of personal protective equipment, in addition to other transmission-based precautions for inpatient care of SARS-CoV-2 patients could reduce the risk of hospital-acquired SARS-CoV-2 infection among frontline HCW.
Keywords: Serology, Sars-cov-2, Covid-19, Coronavirus, Health-care workers, Risk
Background
The Coronavirus Disease 2019 (COVID-19) pandemic caused by Severe Acute Respiratory Syndrome-Coronavirus-2 (SARS-CoV-2) has escalated rapidly [1]. As of 10 February 2021, there were 106 million confirmed COVID-19 cases with 2.3 million deaths globally. The United Kingdom (UK) had endured a considerable burden of the European COVID-19 outbreak, with the highest number of cumulative confirmed cases in Europe at 4 million and the highest number of deaths at 114,000. [2] Among all the cities in the UK, London recorded the highest cumulative COVID-19 cases and deaths. [3] Based on data mainly drawn from the Americas and Europe, healthcare workers (HCWs) have been estimated to account for 8% of all reported COVID-19 cases, though with highly variable between-country results. [4].
HCWs are occupationally at high-risk of SARS-CoV-2 infection. [5] Their unique exposure comes from repeated close contact with COVID-19 inpatients. Additionally, some HCWs perform Aerosol Generating Procedures (AGP) on COVID-19 patients, which are believed to be associated with a very high risk of transmission. SARS-CoV-2 infection among HCWs results in illness and/or the need to self-isolate. [6] The absence of HCWs from work results in an additional strain on the remaining HCWs who may become less likely to comply with IPC precautions. [7] These substantial consequences of SARS-CoV-2 among HCWs call for clear understanding of the extent and mechanisms of transmission of disease in this group.
Serology provides the potential for additional case identification, in support of polymerase chain reaction (PCR) testing of acute cases of infection, as it allows recognition of prior SARS-CoV-2 infection. This can be particularly useful given the frequent occurrence of asymptomatic infection among HCW. [8] Despite generally having lower sensitivity, lateral flow immunoassays (LFA) are faster, cheaper and easier to perform than other laboratory-based serological tests making them potentially useful for large sero-epidemiologic studies. [[9], [10], [11]] Analyses of possible risk factors for serologically-detected SARS-CoV-2 infection among HCWs reported so far have shown divergent results on whether being a COVID-19 frontline HCW (working in COVID-19 units) is associated with SARS-CoV-2 infection. [12] Our study at two hospitals in London sought to determine the seroprevalence of SARS-CoV-2 in HCWs, and whether being a frontline HCW is associated with a higher risk of SARS-CoV-2 seropositivity.
Methods
Study design and participants
This cross-sectional study was conducted within an ongoing prospective SARS-CoV-2 serological testing programme for two hospitals in London. [13] Approximately 4,000 HCWs were employed in these hospitals and potentially eligible for voluntary LFA testing. Any HCW who fitted the inclusion criteria given below, and verbally consented to complete an anonymous questionnaire during an eight-week period between 4 May 2020 and 30 June 2020. The inclusion criteria were as follows:
-
1)
having worked at either (or both) of Chelsea and Westminster Hospital and West Middlesex Hospital between 1 March 2020 and 30 June 2020
-
2)
in line with Public Health England (PHE) guidance, during the first three weeks of the study, only HCWs who had symptoms matching the PHE case definition for SARS-CoV-2 infection (onset at least 14 days earlier) were eligible for testing. [14].
-
3)
for the remaining five weeks of the study, testing became open to all HCW in the two hospitals.
To note, both participating hospitals were able to provide access to both appropriate Personal Protective Equipment (PPE) and relevant Infection Prevention and Control (IPC) training activities throughout the study period. However, we accept that individual staff may have experienced exposures without such protective measures; an anonymous unlinked questionnaire design was used to maximize accurate self-reporting of nosocomial exposure.
Sample size calculation: assuming a seroprevalence of 30%; single cluster population of 4,000 HCWs; alpha error of 5% and design effect of 1.0, a minimum sample size of 300 was calculated using OpenEpi.
Procedures
Specialised staff seconded from a sexual health multidisciplinary team with extensive experience in oropharyngeal swab testing, serology and point-of-care testing attended to the participants. They screened participants for clinical symptoms, performed a point-of-care LFA, checked eligibility for the study, took verbal consent and gave them an anonymised study questionnaire. Participants self-administered the questionnaire while waiting for their LFA result. The questionnaire (supplementary data) took approximately four minutes to complete and collected data on various exposures at home, during travel and while at work. The serology test result was filled by the attending clinical staff member upon return of the questionnaire. Participation was voluntary and serological testing was also provided to those HCWs who did not wish to participate in the study. Validated combined IgM- and IgG-based SARS-CoV-2 LFAs were used to ascertain seropositivity status of HCWs. [9] Due to external supply limitations, different LFAs were used in the course of the study. These included Encode SARS-CoV-2 split IgM/IgG One Step Rapid Test Device (Zhuhai Encode Medical Engineering, Zhuhai, China); Onsite Biotech COVID-19 split IgG/IgM Rapid Test (CTK Biotech, Poway, CA, USA); Orient Gene Biotech COVID-19 IgM/IgG Rapid Test Cassette (Zhejiang Orient Gene Biotech, Zhejiang, China) and VivaDiag™ SARS-CoV-2 IgM/IgG Rapid Test (VivaChek Biotech, Hangzhou, China). Hereafter, the test kits will be referred to as Encode, Onsite, Orient Gene and VivaDiag. Their sensitivities and specificities, based on our local evaluation with reference to the Abbott chemiluminescence microparticle immunoassay as a gold-standard were respectively: Encode (93.4%, 99.0%); Onsite (88.2%, 94.0%); Orient Gene (87.0%, 96.0%); Viva Diag (71.0%, 93.0%). A single drop of blood was added to each of the IgM and IgG test chambers, followed by two drops of buffer. To reduce the risk of user variability, LFAs were read at 15 minutes by two clinical staff experienced in the use of point-of-care analysis. The seropositivity status was categorised into either positive (with a positive control test line with either positive IgM or IgG, or both test lines) or negative. The study data were entered using EpiData entry software.
Statistical analysis
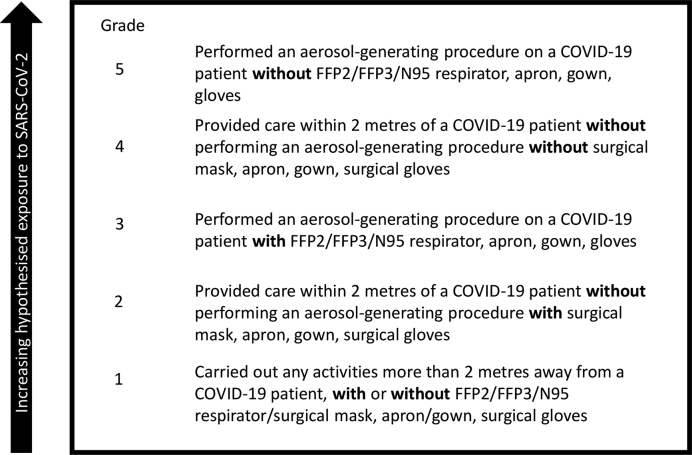
Data analysis was performed using STATA (v16 STATA Corp, USA). The primary exposure was having been a frontline HCW, defined as having worked in any COVID-19 dedicated hospital zone (denoted as red or green zones). Red zones were defined as locations where AGPs were conducted; green zones were all other COVID-19 patient-care areas. A non-frontline HCW was defined as one who did not work in either red or green zones (i.e., administrative staff, laboratory staff, SARS-CoV-2 negative wards). Frontline exposure status was further categorised into five pre-defined grades based on hypothesised procedural risk of acquisition of SARS-CoV-2, according to the maximum level of risk that individual reported experiencing since the onset of widespread local transmission of SARS-CoV-2 in the UK (March 2020) (Fig. 1).
Figure 1.
Grading of the variable ‘frontline’ among healthcare workers. COVID-19 – Coronavirus Disease-2019, FFP2 – Filtering Face Piece-2, FFP3-Filtering Face Piece-3, N95–respirator with 95% filtration efficiency.
The various sociodemographic, occupational and clinical characteristics of the study participants and the seroprevalence were summarized using proportions (%). The association between each possible risk factor and SARS-CoV-2 seropositivity was examined by logistic regression models. Odds ratios (ORs) with 95% confidence intervals (CIs) were calculated to measure the effect size. Strength of evidence, in addition to CIs, was assessed using P-values with a significance threshold set at 0.05. To adjust for confounding, a multivariable logistic regression model was fitted. It was initiated by adding frontline status (main exposure) followed by forced variables namely age, sex and ethnicity. Variables which were deemed to be confounders were associated to frontline status, possible risk factors of SARS-CoV-2 seropositivity and not on the causal pathway between frontline status and SARS-CoV-2 seropositivity. These variables were added to the model if they showed an association with the outcome (in univariable analysis), affected the association between the main exposure and outcome by >5% and there was no evidence of multicollinearity (defined as > 50% change in the standard error of the odds ratio coefficient for frontline status). We did not include variables relating to the “downstream” effects of SARS-CoV-2 infection (such as clinical symptoms) in our models as these could not plausibly affect risk of acquisition. Effect estimates were presented as ORs with confidence intervals and P-value for showing the strength of association. Likelihood ratio tests were conducted to determine if the effect of being frontline on SARS-CoV-2 seropositivity was modified by age, sex and ethnicity.
Ethics approval
Administrative approval was given by Chelsea and Westminster Hospital NHS Foundation Trust. Ethical approval was given by the London School of Hygiene and Tropical Medicine Research Ethics Committee in London, UK. Participants gave verbal informed consent before completing the questionnaire.
Results
Baseline characteristics
Between 4 May 2020 and 30 June 2020, approximately 2100 HCWs at the two hospitals attended the SARS-CoV-2 serology testing programme. Of these, 615 (approximately 25%) completed the questionnaire and were included in the study. The majority of participants identified as female (71.0%) and white ethnicity was the commonest (64.2%), followed by Asian (19.0%), Black (8.9%), mixed (4.6%) and other ethnicities (3.1%); see Table 1. Younger (<40 years) participants were more frequently represented (n=363; 59.0%) and the most represented profession was nursing (35.1%), followed by doctors (24.4%), and allied health sciences (15.8%). There was a far greater number of frontline HCWs (n=446; 72.5%) than non-frontline HCWs, (n=168; 27.3%). Most of the HCWs (n=546; 88.8%) reported a history of a suspected or confirmed COVID-19 staff contact in their working unit. The majority of the study participants (n=515, 83.7%) reported “always” using appropriate PPE with only 12.4% (n=76) reporting that appropriate PPE was “not always” used.
Table 1.
Sociodemographic and occupational characteristics of the study participants and unadjusted odds ratios for their association with SARS-CoV-2 seropositivity
| Variable | Number | (%) | Odds ratio (95%CI) | P-valued |
|---|---|---|---|---|
| Total | 615 | (100) | ||
| Age in years | ||||
| <40 | 363 | (59.0) | 1.00 (Reference) | |
| ≥40 | 249 | (40.5) | 0.89 (0.63–1.27) | 0.531 |
| Missing | 3 | (0.5) | ||
| Sex | ||||
| Female | 437 | (71.0) | 1.00 (Reference) | |
| Male | 156 | (25.4) | 1.24 (0.84–1.82) | 0.279 |
| Missing | 22 | (3.6) | ||
| Ethnicity | ||||
| White | 395 | (64.2) | 1.00 (Reference) | |
| Asian | 117 | (19.0) | 1.01 (0.65–1.58) | 0.961 |
| Black | 55 | (8.9) | 0.78 (0.42–1.46) | 0.437 |
| Mixed | 28 | (4.6) | 0.57 (0.23–1.40) | 0.222 |
| Other | 19 | (3.1) | 1.31 (0.49–3.46) | 0.592 |
| Missing | 1 | (0.2) | ||
| Household size, people | ||||
| ≤2 | 346 | (55.3) | 1.00 (Reference) | |
| >2 | 256 | (41.6) | 1.12 (0.79–1.59) | 0.527 |
| Missing | 13 | (2.1) | ||
| Pre-illness household contact with suspected/confirmed COVID-19 casea | ||||
| No | 505 | (84.9) | 1.00 (Reference) | |
| Yes | 90 | (15.1) | 1.19 (0.76–1.87) | 0.451 |
| Hospital | ||||
| Chelsea and Westminster | 469 | 76.3 | 1.00 (Reference) | |
| West Middlesex | 119 | 19.3 | 1.30 (0.85–1.99) | 0.224 |
| Both | 27 | 4.4 | 1.25 (0.52–2.91) | 0.611 |
| Profession | ||||
| Nurse | 216 | (35.1) | 1.00 (Reference) | |
| Doctor | 150 | (24.4) | 1.44 (0.92–2.24) | 0.109 |
| Allied and health science | 97 | (15.8) | 1.02 (0.60–1.71) | 0.954 |
| Other | 152 | (24.7) | 1.51 (0.95–2.40) | 0.080 |
| Type of transport to work | ||||
| Public | 171 | (27.8) | 1.00 (Reference) | |
| Private | 287 | (46.7) | 1.30 (0.86–1.97) | 0.214 |
| Both | 147 | (23.9) | 1.33 (0.82–2.16) | 0.242 |
| Missing | 10 | (1.6) | ||
| Total travel duration to work, minutes (singe way) | ||||
| ≤15 | 289 | (47.0) | 1.00 (Reference) | |
| >15 | 315 | (51.2) | 1.00 (0.71–1.42) | 0.988 |
| Missing | 11 | (1.8) | ||
| Frontline exposure grade (main exposure) | ||||
| Non-frontline | 168 | (27.3) | 1.00 (Ref) | |
| Frontline (all Grades) | 446 | (72.5) | 0.99 (0.66–1.48) | 0.961 |
| Grade 1 | 51 | 1.17 (0.60–2.29) | 0.638 | |
| Grade 2 | 105 | 0.84 (0.49–1.46) | 0.546 | |
| Grade 3 | 158 | 0.73 (0.45–1.19) | 0.211 | |
| Grade 4 | 105 | 1.34 (0.79–2.26) | 0.276 | |
| Grade 5 | 27 | 1.89 (0.82–4.35) | 0.136 | |
| Missing | 1 | (0.2) | ||
| Had suspected/confirmed unit staff COVID-19 contact | ||||
| Yes | 546 | (88.8) | 1.00 (Reference) | |
| No | 43 | (7.0) | 1.67 (0.82–3.38) | 0.155 |
| Missing | 26 | (4.2) | ||
| Had COVID-19 focussed IPC trainingb | ||||
| Yes | 411 | (66.8) | 1.00 (Reference) | |
| No | 179 | (29.1) | 1.24 (0.85–1.81) | 0.255 |
| Missing | 25 | (4.1) | ||
| Frequency of use of appropriate PPEc | ||||
| Always | 515 | (83.7) | 1.00 | |
| Not always | 76 | (12.4) | 1.73 (1.04–2.84) | 0.028 |
| Missing | 24 | (3.9) | ||
^ is for confidence interval.
COVID-19 – Coronavirus Disease-2019
IPC– Infection Prevention & Control.
PPE-Personal Protective Equipment.
From Wald's Test.
Clinical and laboratory characteristics
The majority of the participants (81.6%) reported prior symptoms suggestive of COVID-19 with almost all of these (476/502) indicating that symptoms had started more than 14 days previously. However, during the study period, only 369 (60.0%) of the participants indicated that they had self-isolated for an appropriate indication (after COVID-19 symptoms or contact), indicating a substantial proportion appeared not to have self-isolated following symptoms. Twenty-four participants (3.9%) reported having previously had a positive laboratory SARS-CoV-2 PCR test. Based on combined results from all different LFAs, the seroprevalences were IgM 34.1%, IgG 37.4% and overall (either/or IgM/IgG positive) 40.7%. (Table 2). The seroprevalence in the initial 3-week period (testing limited to previously symptomatic HCW) and the final 5-week period (testing open to all HCW) were 37.5% and 43.3%, respectively and the difference was not statistically significant (P=0.092).
Table 2.
Clinical and laboratory characteristics of the study participants
| Variable | Number | (%) |
|---|---|---|
| Total | 615 | (100) |
| Had history of COVID-19a symptoms | ||
| Yes | 502 | (81.6) |
| No | 72 | (11.7) |
| Unsure | 41 | (6.7) |
| When symptoms began, days | ||
| <7 | 8 | (1.3) |
| 7–14 | 13 | (2.1) |
| 15–21 | 40 | (6.5) |
| >21 | 476 | (77.4) |
| Not applicable | 78 | (12.7) |
| History of self-isolation | ||
| Yes | 369 | (60.0) |
| No | 224 | (36.4) |
| Missing | 22 | (3.6) |
| Had a positive SARS-CoV-2b PCR testc | ||
| Yes | 24 | (3.9) |
| No | 591 | (96.1) |
| Type of SARS-CoV-2 LFAd test | ||
| Encode | 333 | (54.1) |
| Onsite | 239 | (38.9) |
| Viva Diag | 24 | (3.9) |
| Orient Gene | 19 | (3.1) |
| SARS-CoV-2 IgM | ||
| Positive | 210 | (34.1) |
| Negative | 402 | (65.4) |
| Missing | 3 | (0.5) |
| SARS-CoV-2 IgG | ||
| Positive | 230 | (37.4) |
| Negative | 381 | (62.0) |
| Missing | 4 | (0.6) |
| Overall SARS-CoV-2 IgM/IgG result (either positive; main outcome variable) | ||
| Positive | 250 | (40.7) |
| Negative | 365 | (59.3) |
COVID-19 – Coronavirus Disease-2019.
SARS-CoV-2 – Severe Acute Respiratory Syndrome Coronavirus 2.
PCR – Polymerase Chain Reaction.
LFA – Lateral Flow immunoassay.
Factors associated with seropositivity
In a crude analysis, there was no evidence of an association between frontline status and SARS-CoV-2 seropositivity (OR 0.99, 95%CI 0.66–1.48). For other univariable associations, only “frequency of use of appropriate PPE” had evidence of an association with seropositivity (OR 1.73, 95% CI 1.04–2.84). There was no evidence that any particular ethnic groups or professions or a history of a prior suspected/confirmed COVID-19 contact either at home or among unit staff were associated with risk of SARS-CoV-2 seropositivity (Table 1).
In an adjusted analysis, there was a non-significant evidence of a modest association between being a frontline HCW and SARS-CoV-2 seropositivity OR 1.39 (95% CI 0.84–2.30) (see Table 3). This model included adjustment for age, sex, ethnicity, profession, history of unit staff suspected/confirmed COVID-19 contact, history of attending a COVID-19 focussed IPC training and frequency of PPE use. Additionally, there was an association between the higher grades (4 and 5) of frontline exposure and SARS-CoV-2 seropositivity. Being frontline with Grade 4 exposure was associated with 82% higher odds of seropositivity compared with being non-frontline (OR 1.82, CI 0.72–3.02) and being frontline with Grade 5 exposure was associated with more than double the odds of seropositivity compared to being non-frontline (OR 2.49, 95%CI 1.00–6.12). A test for trend showed that the odds of seropositivity followed the exposure gradient with a 15% increase in odds of seropositivity from each frontline grade to the next (OR 1.15, 95% CI 1.00–1.32). Likelihood ratio tests showed that there was no evidence of an interaction of the association between frontline status and seropositivity by age (P=0.913), sex (P=0.791) or ethnicity (P=0.254).
Table 3.
Adjusted odds ratios for the association between being a frontline healthcare worker and SARS-CoV-2 seropositivity, grossly, and by frontline exposure grade.
| Odds ratio (95%CIa) |
P-valueb |
Odds ratio (95%CI) |
P-valuec |
|
|---|---|---|---|---|
| Unadjusted (n=615) | Fully adjustedd(n=547) | |||
| Frontline | ||||
| No | 1.00 (reference) | 1.00 (reference) | ||
| Yes | 0.99 (0.66–1.48) | 0.961 | 1.39 (0.84–2.30) | 0.200 |
| Frontline grade | ||||
| Non-frontline | 1.00 (reference) | 1.00 (reference) | ||
| Grade 1 | 1.17 (0.60–2.29) | 0.638 | 1.48 (0.72–3.02) | 0.283 |
| Grade 2 | 0.84 (0.49–1.46) | 0.546 | 1.15 (0.61–2.17) | 0.661 |
| Grade 3 | 0.73 (0.45–1.19) | 0.211 | 1.06 (0.57–1.96) | 0.854 |
| Grade 4 | 1.34 (0.79–2.26) | 0.276 | 1.82 (0.96–3.44) | 0.065 |
| Grade 5 | 1.89 (0.82–4.35) | 0.136 | 2.49 (1.00–6.18) | 0.049 |
| Test for trend | ||||
| Frontline grade | 1.15 (1.00–1.32) | 0.043 | ||
CI – Confidence Interval.
From Wald Test.
From Likelihood Ratio Test.
This model included adjustment for age, sex, ethnicity, profession, history of unit staff suspected/confirmed COVID-19 contact, history of attending a COVID-19 focussed IPC training and frequency of PPE use.
Discussion
Among HCW across two hospitals in London after the UK COVID-19 first wave, SARS-CoV-2 IgM/IgG seropositivity was 40.7%. After adjustment for relevant confounding variables, being a frontline HCW was associated with 39% higher odds of seropositivity than equivalent non-frontline HCWs, though this finding was not statistically significant. On a test for trend, there was an increase in the risk of seropositivity along a pre-defined frontline exposure gradient.
Interpretation of key findings
Seroprevalence
The seroprevalence of 40.7% from our study is similar to other studies of HCWs who were working with substantial numbers of COVID-19 patients at around the same time as our study. These studies showed seroprevalence of 45.3% in London, UK and 37.5% in New York, United States of America (USA). [15,16] This level is much higher than a seroprevalence of 14.5% found in tertiary-level maternity-care HCWs in London and the community in London (13.0%) and England (6.0%) at around the same time. [17,18] However, the seroprevalence from our study differed markedly from other sero-epidemiologic studies among HCWs from countries in mainly the Americas and Europe which were carried out during or just after their first COVID-19 wave peak (April–June 2020). [[19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33]] These studies showed an estimated overall seroprevalence of 8.7% (95% CI 6.7–10.9%) but had varying study designs, serology tests and HCW populations which may also account for the divergent findings. [12].
The high seroprevalence of SARS-CoV-2 in our study could be explained firstly, by our focus on hospital-based HCWs, most (72.5%) of whom had contact with confirmed COVID-19 patients (frontline). These staff have been reported to have higher risk of SARS-CoV-2 infection than non-hospital HCWs [23,34]. Secondly, the screening criteria at the start of our study included HCW having had symptoms at least 14 days prior to testing, though this requirement was later removed. This criterion was met by over 80% of our overall study population. Indeed, in a bigger prospective SARS-CoV-2 serological testing study, within which this study was conducted, the seroprevalence among symptomatic HCWs was four times that in those who were asymptomatic. [13] We therefore may have recruited participants with a higher pre-test probability of actually having had COVID-19 hence a high seropositivity. This means we may have over-estimated the seropositivity in the entire HCW population of these hospitals. However, we found no statistically significant difference in HCW seropositivity between the initial 3-week and the final 5-week period, so we believe any degree of over-estimation to be modest. Such a lack of difference may also have been because of seroprevalence gradually rising between these two periods, following the peak of the first COVID-19 wave in the UK. Thirdly, the London catchment area had the highest community SARS-CoV-2 seropositivity, COVID-19 cases, hospital admissions, and deaths in the UK during the study period, therefore it is likely that HCWs in our study had a substantial exposure to both community and healthcare-associated SARS-CoV-2 transmission. [[35], [36], [37]].
Seropositivity association
Our study found frontline HCWs to have higher odds of seropositivity than non-frontline staff, but the probability that this result could have occurred by chance is high. A similar study using comparable LFAs in Denmark reported that HCWs in COVID-19 dedicated wards had a 63% higher risk of seropositivity than their counterparts in non-COVID-19 workspaces (RR 1.63, 95%CI 1.34–2.03). [23] Likewise, a study in Sweden reported more than three-times higher odds in HCWs who had COVID-19 patient contact than those who did not (OR 3.3, 95% CI 2.2–5.3) [30]. A lack or lapse in the use of appropriate PPE may be the possible explanation to the association between being frontline and seropositivity.
Conversely, seroprevalence surveys among HCWs in Belgium, Italy, Spain and USA found no relationship between exposure to COVID-19 patients and SARS-CoV-2 IgG and/or IgM seropositivity. [25,29,31,32] These studies suggested that there was greater community-associated rather than healthcare-associated SARS-CoV-2 transmission among HCWs. The differences between our study results and these findings could also have occurred as a result of different study designs, timings of testing, response rates, HCW populations, PPE protocols or a combination of these.
Seropositivity trend
Our study revealed a dose-response trend of seropositivity with the grade of being exposed to COVID-19 as a frontline HCW, according to a pre-defined gradient of exposure. We are not aware of prior studies considering HCW exposure status along an ordered gradient of exposure risk and considering confounding effects of other exposures. However, some corroborative evidence for our findings comes from other studies, including a study in the USA which showed an increased risk of SARS-CoV-2 seropositivity when HCWs carry out tasks without adequate PPE. [19] A study with participants from both the UK and the US, also showed that among HCWs who had direct contact with patients, HCWs who reported using inadequate PPE, or PPE reuse had an increased risk of a positive COVID-19 PCR test than those who had adequate PPE. [34].
Study strengths
In this study, seropositive cases originated from the same population that generated seronegative cases, thereby increasing internal validity and comparability. As recruitment and documentation of exposures was done before the LFA test result, outcome status did not determine inclusion in the study nor influence responses to the questionnaire. We believe that the use of an anonymous questionnaire will have promoted accurate self-reporting of in-hospital exposure risks. The LFAs used in the study were internally validated and had a fair diagnostic performance with sensitivities of 72–94% and specificities of 93–99%. These LFAs could detect either IgM or IgG thereby increasing sensitivity as compared to single IgM or IgG test. [38] We believe our study was unique in use of an exposure gradient from low to high exposure risk for SARS-CoV-2, thereby making it a highly sophisticated evaluation of this exposure.
Limitations
This study's cross-sectional design makes it difficult to prove that exposure came before infection, hence reverse causality of some associations is a possibility if individuals' risk-adjusted after infection. Our study could have underestimated prior SARS-CoV-2 infection in some participants due to (i) them not having developed detectable anti-SARS-CoV-2 antibodies and may have used cell-mediated immune response for their prior SARS-CoV-2 infection, (ii) having been tested before antibodies had developed as a result of delayed development of detectable antibodies (iii) having developed antibodies but missed by the LFA test. Four different LFAs with different diagnostic performances were used in the course of the study, due to external supply issues. Though the majority (93%) of participants had either Encode or Onsite LFA which both had excellent sensitivity, we acknowledge that use of the single best LFA would have given the most reliable results. [13]. There is a possibility that SARS-CoV-2 seroprevalence may have been overestimated as some IgM-only bands may have been false positives – this is a recognized limitation of these assays. Very few patients were IgM+/IgG-, hence any such overestimation is likely to be minimal. Furthermore, our questionnaire did not ask about use of eye protection which may provide protection against SARS-CoV-2 containing droplets or droplet nuclei. Out of the total population of HCW in these two hospitals, only a relatively small proportion (approximately 15%) took part in this study, so if there were non-representative participation this could produce biased results. We believe that the profile of participants was broadly reflective of the staff working in the Trust.
Conclusions
We demonstrated a high SARS-CoV-2 IgM/IgG seropositivity with an association between increasing frontline exposure and SARS-CoV-2 seropositivity among hospital HCWs at well-resourced hospitals in the UK. Use of the recommended and appropriately donned PPE and compliance with other IPC transmission-based precautions in inpatient care of COVID-19 patients among HCW in the highest exposure risk groups could further reduce risk of healthcare-associated SARS-CoV-2 transmission.
Consent for publication
No patient identifiable data necessitating consent was used in this study.
Availability of data and materials
The datasets analysed in this study are available from Dr Luke Moore (luke.moore@nhs.net) on reasonable request. The questionnaire used is included as a study Appendix.
Authors' contributions
Admire Simbarashe Murongazvombo: Conceptualisation, Methodology, Investigation, Formal analysis, Visualisation, Writing - Original draft preparation, Writing – Review and Editing. Rachael Sarah Jones: Resources, Conceptualisation, Methodology, Investigation, Writing - Original draft preparation, Writing – Review and Editing, Project administration. Michael Rayment: Resources, Conceptualisation, Methodology, Investigation, Writing - Original draft preparation, Writing – Review and Editing, Project Administration. Scott John Charles Pallett: Resources, Conceptualisation, Methodology, Writing – Review and Editing. Nabeela Mughal: Resources, Conceptualisation, Methodology, Writing – Review and Editing. Berge Azadian: Resources, Conceptualisation, Methodology, Writing – Review and Editing. Hugo Donaldson: Resources, Conceptualisation, Methodology, Writing – Review and Editing. Gary William Davies: Resources, Writing – Review and Editing, Supervision. Luke Stephen Prockter Moore: Resources, Conceptualisation, Methodology, Writing – Review and Editing, Data curation, Supervision. Alexander Michael Aiken: Conceptualisation, Methodology, Investigation, Formal analysis, Writing - Original draft preparation, Writing – Review and Editing, Data curation, Supervision.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest statement
LSPM has consulted for/received speak fees from bioMerieux (2013–21), DNAelectronics (2015), Dairy Crest (2017–18), Pfizer (2018–21), Eumedica (2016–21), Profile Pharma (2018), and Umovis Lab (2020–21), and received research grants from the UK National Institute for Health Research (NIHR; 2013–2019), and CW+ Charity (2018–2021).
RSJ has acted as a speaker or adviser to, has been an investigator for, or received support to attend conferences or educational grants to her institution from Gilead, ViiV, Janssen and MSD. NM has consulted for/received speak fees from), Pfizer (2019–21), Eumedica (2016).
Acknowledgements
We would also like to acknowledge the staff at Chelsea and Westminster Hospital NHS Foundation Trust's 10 Hammersmith Broadway Clinic for administering the study questionnaire and conducting the point-of-care serology test as well as the study participants for consenting to take part in the study. ASM acknowledges the Chevening Scholarships, the UK government's global scholarship programme, funded by the Foreign, Commonwealth and Development Office (FCDO) and partner organisation for funding MSc studies at the London School of Hygiene and Tropical Medicine during which this study was conducted. LSPM acknowledges support from the National Institute of Health Research (NIHR) Imperial Biomedical Research Centre (BRC) and the National Institute for Health Research Health Protection Research Unit (HPRU) in Healthcare Associated Infection and Antimicrobial Resistance at Imperial College London in partnership with Public Health England. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research, or the UK Department of Health.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.infpip.2021.100157.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.World Health Organization (WHO) 2021. Timeline of WHO’s response to COVID-19.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline [Google Scholar]
- 2.World Health Organization (WHO) 2021. WHO Coronavirus disease (COVID-19) dashboard.https://covid19.who.int/ [Google Scholar]
- 3.Daily summary | Coronavirus in the UK n.d. https://coronavirus.data.gov.uk/(accessed February 10, 2021).
- 4.World Health Organization (WHO). Weekly epidemiological update - 2 February 2021 2021. https://www.who.int/publications/m/item/weekly-epidemiological-update---2-february-2021 (accessed March 3, 2021).
- 5.David K. Occupational risks for COVID-19 infection. Occup Med (Chic Ill) 2020;70:3–5. doi: 10.1093/occmed/kqaa036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.COVID-19: management of exposed healthcare workers and patients in hospital settings - GOV.UK n.d. https://www.gov.uk/government/publications/covid-19-management-of-exposed-healthcare-workers-and-patients-in-hospital-settings/covid-19-management-of-exposed-healthcare-workers-and-patients-in-hospital-settings (accessed April 12, 2020).
- 7.Lai X., Wang X., Yang Q., Xu X., Tang Y., Liu C. Will healthcare workers improve infection prevention and control behaviors as COVID-19 risk emerges and increases, in China? Antimicrob Resist Infect Control. 2020;9:83. doi: 10.1186/s13756-020-00746-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhao D., Wang M., Wang M., Zhao Y., Zheng Z., Li X. Asymptomatic infection by SARS-CoV-2 in healthcare workers: A study in a large teaching hospital in Wuhan, China. Int J Infect Dis. 2020;99:219–225. doi: 10.1016/j.ijid.2020.07.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pallett S, Denny S, Patel A, Charani E, Mughal N, Stebbing J, et al. Point-of-care serological assays for SARS-CoV-2 in a UK hospital population: potential for enhanced case finding Res Sq 2020. 10.21203/rs.3.rs-28006/v1. [DOI] [PMC free article] [PubMed]
- 10.Feng W., Newbigging A.M., Le C., Pang B., Peng H., Cao Y. Molecular Diagnosis of COVID-19: Challenges and Research Needs. Anal Chem. 2020;92:10196–10209. doi: 10.1021/acs.analchem.0c02060. [DOI] [PubMed] [Google Scholar]
- 11.Moura D.T.H., McCarty T.R., Ribeiro I.B., Funari M.P., Oliveira P.V.A.G., Miranda Neto A.A. Diagnostic Characteristics of Serological-Based COVID-19 Testing: A Systematic Review and Meta-Analysis. Clinics (Sao Paulo) 2020;75 doi: 10.6061/clinics/2020/e2212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Galanis P., Vraka I., Fragkou D., Bilali A., Kaitelidou D. Seroprevalence of SARS-CoV-2 antibodies and associated factors in healthcare workers: a systematic review and meta-analysis. J Hosp Infect. 2021;108:120–134. doi: 10.1016/j.jhin.2020.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pallett S.J.C., Rayment M., Patel A., Fitzgerald-Smith S.A.M., Denny S.J., Charani E. Point-of-care serological assays for delayed SARS-CoV-2 case identification among health-care workers in the UK: A prospective multicentre cohort study. Lancet Respir Med. 2020;8:885–894. doi: 10.1016/s2213-2600(20)30315-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.COVID-19: investigation and initial clinical management of possible cases - GOV.UK n.d. https://www.gov.uk/government/publications/wuhan-novel-coronavirus-initial-investigation-of-possible-cases (accessed January 20, 2021).
- 15.Houlihan C.F., Vora N., Byrne T., Lewer D., Kelly G., Heaney J. Pandemic peak SARS-CoV-2 infection and seroconversion rates in London frontline health-care workers. Lancet. 2020;396:e6. doi: 10.1016/S0140-6736(20)31484-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mansour M., Leven E., Muellers K., Stone K., Mendu D.R., Wajnberg A. Prevalence of SARS-CoV-2 Antibodies Among Healthcare Workers at a Tertiary Academic Hospital in New York City. J Gen Intern Med. 2020;35:2485–2486. doi: 10.1007/s11606-020-05926-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bampoe S., Lucas D.N., Neall G., Sceales P., Aggarwal R., Caulfield K. A cross-sectional study of immune seroconversion to SARS-CoV-2 in frontline maternity health professionals. Anaesthesia. 2020;75:1614–1619. doi: 10.1111/anae.15229. [DOI] [PubMed] [Google Scholar]
- 18.Ward H., Atchison C., Whitaker M., Ainslie K.E.C., Elliott J., Okell L. SARS-CoV-2 antibody prevalence in England following the first peak of the pandemic. Nat Commun. 2021;12:1–8. doi: 10.1038/s41467-021-21237-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Self W.H., Tenforde M.W., Stubblefield W.B., Feldstein L.R., Steingrub J.S., Shapiro N.I. Seroprevalence of SARS-CoV-2 Among Frontline Health Care Personnel in a Multistate Hospital Network — 13 Academic Medical Centers, April–June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1221–1226. doi: 10.15585/mmwr.mm6935e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Martin C, Montesinos I, Dauby N, Gilles C, Dahma H, Van Den Wijngaert S, et al. Dynamics of SARS-CoV-2 RT-PCR positivity and seroprevalence among high-risk healthcare workers and hospital staff 2020. 10.1016/j.jhin.2020.06.028. [DOI] [PMC free article] [PubMed]
- 21.Behrens G.M.N., Cossmann A., Stankov M.V., Witte T., Ernst D., Happle C. Perceived versus proven SARS-CoV-2-specific immune responses in health-care professionals. Infection. 2020;48:631–634. doi: 10.1007/s15010-020-01461-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xu X., Sun J., Nie S., Li H., Kong Y., Liang M. Seroprevalence of immunoglobulin M and G antibodies against SARS-CoV-2 in China. Nat Med. 2020;26:1193–1195. doi: 10.1038/s41591-020-0949-6. [DOI] [PubMed] [Google Scholar]
- 23.Iversen K., Bundgaard H., Hasselbalch R.B., Kristensen J.H., Nielsen P.B., Pries-Heje M. Risk of COVID-19 in health-care workers in Denmark: an observational cohort study. Lancet Infect Dis. 2020 doi: 10.1016/s1473-3099(20)30589-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Garcia-Basteiro A.L., Moncunill G., Tortajada M., Vidal M., Guinovart C., Jiménez A. Seroprevalence of antibodies against SARS-CoV-2 among health care workers in a large Spanish reference hospital. Nat Commun. 2020;11:1–9. doi: 10.1038/s41467-020-17318-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sotgiu G., Barassi A., Miozzo M., Saderi L., Piana A., Orfeo N. SARS-CoV-2 specific serological pattern in healthcare workers of an Italian COVID-19 forefront hospital. BMC Pulm Med. 2020;20:203. doi: 10.1186/s12890-020-01237-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vilibic-Cavlek T., Stevanovic V., Tabain I., Betica-Radic L., Sabadi D., Peric L. Severe acute respiratory syndrome coronavirus 2 seroprevalence among personnel in the healthcare facilities of Croatia, 2020. Rev Soc Bras Med Trop. 2020;53:1–3. doi: 10.1590/0037-8682-0458-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gómez-Ochoa S.A., Franco O.H., Rojas L.Z., Raguindin P.F., Roa-Díaz Z.M., Wyssmann B.M. COVID-19 in Healthcare Workers: A Living Systematic Review and Meta-analysis of Prevalence, Risk Factors, Clinical Characteristics, and Outcomes. Am J Epidemiol. 2020 doi: 10.1093/aje/kwaa191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shields A., Faustini S.E., Perez-Toledo M., Jossi S., Aldera E., Allen J.D. SARS-CoV-2 seroprevalence and asymptomatic viral carriage in healthcare workers: A cross-sectional study. Thorax. 2020 doi: 10.1136/thoraxjnl-2020-215414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dimcheff D.E., Schildhouse R.J., Hausman M.S., Vincent M.S.B.M., Markovitz E., Chensue S.W. Seroprevalence of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection among Veterans Affairs healthcare system employees suggests higher risk of infection when exposed to SARS-CoV-2 outside the work environment. Infect Control Hosp Epidemiol. 2020;12:1–7. doi: 10.1017/ice.2020.1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rudberg A.S., Havervall S., Månberg A., Jernbom Falk A., Aguilera K., Ng H. SARS-CoV-2 exposure, symptoms and seroprevalence in healthcare workers in Sweden. Nat Commun. 2020;11:1–8. doi: 10.1038/s41467-020-18848-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Steensels D., Oris E., Coninx L., Nuyens D., Delforge M.L., Vermeersch P. Hospital-Wide SARS-CoV-2 Antibody Screening in 3056 Staff in a Tertiary Center in Belgium. JAMA - J Am Med Assoc. 2020;324:195–197. doi: 10.1001/jama.2020.11160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moscola J., Sembajwe G., Jarrett M., Farber B., Chang T., McGinn T. Prevalence of SARS-CoV-2 Antibodies in Health Care Personnel in the New York City Area. JAMA. 2020;324:893. doi: 10.1001/jama.2020.14765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Korth J., Wilde B., Dolff S., Anastasiou O.E., Krawczyk A., Jahn M. SARS-CoV-2-specific antibody detection in healthcare workers in Germany with direct contact to COVID-19 patients. J Clin Virol. 2020;128:104437. doi: 10.1016/j.jcv.2020.104437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nguyen L.H., Drew D.A., Graham M.S., Joshi A.D., Guo C.-G., Ma W. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Heal. 2020 doi: 10.1016/s2468-2667(20)30164-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Office for National Satistics. Coronavirus (COVID-19) Infection Survey pilot 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/coronaviruscovid19infectionsurveypilot/englandandwales4september2020 (accessed September 11, 2020).
- 36.Coronavirus (COVID-19) in the UK: Cases n.d. https://coronavirus.data.gov.uk/cases (accessed September 7, 2020).
- 37.Sero-surveillance of COVID-19 - GOV.UK 2020. https://www.gov.uk/government/publications/national-covid-19-surveillance-reports/sero-surveillance-of-covid-19 (accessed September 6, 2020).
- 38.Li Z., Yi Y., Luo X., Xiong N., Liu Y., Li S. Development and clinical application of a rapid IgM-IgG combined antibody test for SARS-CoV-2 infection diagnosis. J Med Virol. 2020;92:1518–1524. doi: 10.1002/jmv.25727. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets analysed in this study are available from Dr Luke Moore (luke.moore@nhs.net) on reasonable request. The questionnaire used is included as a study Appendix.