Abstract
Mucormycosis is a life-threatening infection with most commonly rhino-orbital-cerebral and pulmonary syndromes that mostly occurs in immunocompromised patients. FDG-PET/CT emerged as a sensitive non-invasive tool to identify systemic mucormycosis. We present a 59-year-old woman for whom a PET/CT with 18F-FDG was performed in search of a primary location of mucormycosis with non-contributive conventional workup. A large left abdominal mass was seen, compatible with a fungus ball, with intense parietal uptake and without any central uptake. The localization of the infection provided a target for surgery and permitted to adapt the therapeutic strategy. After resection, the final diagnosis was consistent with mucormycosis. To our knowledge, this is the first report of a PET/CT image with FDG showing an intestinal fungus ball. PET/CT with 18F-FDG may contribute to the management of patients with fungal infections of unknown origin.
Keywords: Intestinal mucormycosis, PET/CT, FDG, Fungal infection
Background
Mucormycosis, previously called zygomycosis, is a life-threatening infection that mostly occurs in immunocompromised patients. It is a rare human infection reflecting the effectiveness of the immune system as all humans have ample exposure to the fungi during day-to-day activities and because infections occur almost always in the presence of an underlying compromising condition (diabetes, hematologic malignancy). The infection involves most commonly the facial sinuses, with possible extension into the brain, and the lungs presumably because of the inhalation of the spores into the paranasal sinuses. Other rarer deep localizations have been described (Barnes et al. 2017; Chinen et al. 2009; Marutsuka et al. 2013; Rashid et al. 2019; Ahmad et al. 2019; Forrester et al. 2015). The gastrointestinal tract is an unusual location, and infection probably occurs because of the ingestion of spores. The most common site seems to be the stomach followed by the colon (Agha et al. 1985). Treatment involves a combination of surgical debridement of the involved tissues and antifungal treatment. The diagnosis is difficult to establish as it depends on the identification of organisms in the tissue by histopathology with culture confirmation. However, culture often yields no growth. This explains why rates of delayed diagnosis and mortality are still high (Farmakiotis and Kontoyiannis 2016). Thus, in an appropriate clinical setting, the clinician often starts an empirical treatment for mucormycosis because early initiation of therapy is crucial. However, to maximize the outcome, surgery is essential which requires the localization of the primary infection. 18F-FDG can be used for its nonspecific uptake in infectious, inflammatory, and neoplastic processes. FDG-PET/CT emerged as a sensitive non-invasive tool to identify systemic mucormycosis (Dang et al. 2012; Liu et al. 2013; Altini et al. 2015; Song 2019), which can serve as a new diagnostic modality and have a significant impact on the therapeutic management.
Case presentation
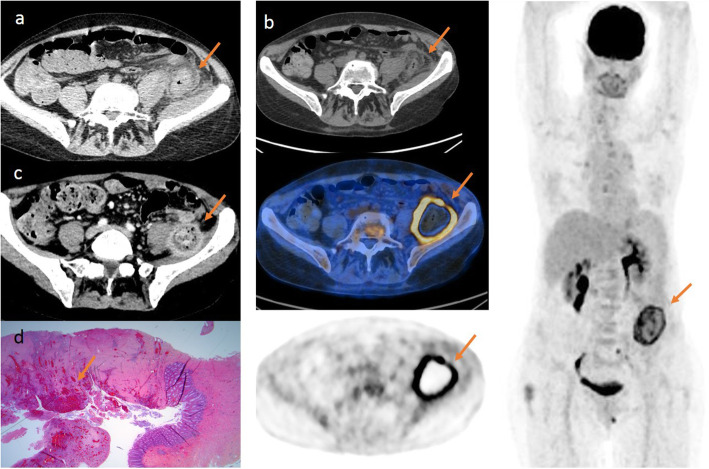
We present herein a case of a 59-year-old woman initially diagnosed with acute myeloid leukemia. Post induction chemotherapy, this pancytopenic patient developed a persisting fever despite broad-spectrum antibiotics. A thoracoabdominal CT (a, arrow) was performed, without IV contrast because of renal failure, and showed features of aspecific colitis with wall thickening, thickening of the fascial planes, and infiltration of the pericolic fat and the iliopsoas muscle (Fig. 1). PCR blood analysis for mucor demonstrated positivity, and an isavuconazole treatment was started. Subsequent thorax and sinus CT was negative. Ten days after the first CT (a), a PET/CT with 18F-FDG (b, arrow) was performed in search of a primary location for eventual resection. Images were acquired on a GE Discovery IQ PET/CT (GE Healthcare, Milwaukee) 65 min after injection of 138 MBq of FDG. A large left abdominal mass was seen, compatible with a fungus ball, with intense parietal uptake (SUV max bw 8.81) and without any central uptake and in which the colon descendens seems to enter and exit without deformation. A month later, a second pre-operative CT with IV contrast (c, arrow) was performed and showed a fibrotic inflammatory mass with necrotic center adhering to the iliopsoas muscle and encompassing the descending colon. The final histological diagnosis after resection was a chronic ischemic ulcerated enterocolitis with fistulation and associated abscess, consistent with mucormycosis as it typically invades blood vessels with ischemia and loss of blood supply (d, arrow) (Fig. 1). No hyphae were seen, and culture for mucormycosis remained negative. The patient recovered well from the surgery. On a hematological plan, the patient is actually considered in complete remission. An allogenic stem cell transplantation was performed after the digestive surgery.
Fig. 1.
Intestinal mucormycosis “fungus ball” located with [18F]-FDG-PET/CT. a CT image on 3 November 2018 without contrast injection of aspecific colitis as shown by the orange arrow. b PET/CT image on 15 November 2018 of the intestinal fungus ball: left column: top panel: CT axial view without contrast; middle panel: fused PET/CT image; bottom panel: PET axial view; the right column shows a whole body volume–rendered image. The orange arrows show the intestinal fungus ball. c CT with the injection of contrast on 19 December 2018 showing a fibrotic inflammatory mass with necrotic center adhering to the iliopsoas muscle and encompassing the descending colon as shown with an orange arrow. d 03 January 2019: histological exam of intestinal resection. Coloration used: hematoxylin-eosin; magnitude: X1.25
Discussion
Along with clinical, laboratory, and histopathological data, imaging plays an important role in the diagnosis and management of mucormycosis. Even though the most common primary locations are usually well located with a standard thorax and sinus CT, other deep locations may present a problem. This is particularly important in this setting as resection of the fungus ball is necessary to complete the treatment. 18F-FDG-PET/CT has proven to be valuable in providing complementary information concerning the primary location and the extent of the fungal disease.
Conclusion
To our knowledge, this is the first report of a PET/CT image with FDG of an intestinal fungus ball which permitted to localize the disease, which provided a target for surgery, and to adapt the therapeutic strategy. PET/CT with 18F-FDG may contribute in the management of patients with fungal infections of unknown origin.
Acknowledgements
Not applicable.
Abbreviations
- 18F-FDG-PET/CT
18fluorine fluoro deoxyglucose positron emission tomography/computed tomography
Authors’ contributions
LOD and ST conceived and designed the study. LOD, LV, FG, FC, KM, NM, ST, LS, and EG performed acquisition, analysis, and interpretation of data. LOD, ST, LV, and FG drafted the article and performed the final approval. All authors read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
The images and biopsy samples remain available in our database.
Ethics approval and consent to participate
For this case report, informed and written consent for publication was obtained from the patient. As the FDG-PET/CT was part of the clinical examination, no ethical approval was needed.
Consent for publication
We hereby consent for publication.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Franklin Gallo, Email: Gallo.franklin@iuct-oncopole.fr.
Lavinia Vija, Email: Vija_lm@yahoo.com.
Sophie Le Grand, Email: LeGrand.sophie@iuct-oncopole.fr.
Nada Moukarbel, Email: Moukarbel.nada@iuct-oncopole.fr.
Koen Mortele, Email: kmortele@bidmc.harvard.edu.
Erwan Gabiache, Email: Gabiache.erwan@iuct-oncopole.fr.
Frédéric Courbon, Email: Courbon.frederic@iuct-oncopole.fr.
Suzanne Tavitian, Email: tavitian.suzanne@iuct-oncopole.fr.
Lawrence O. Dierickx, Email: dierickxlawrence@hotmail.com
References
- Agha FP, Lee HH, Boland CR, Bradley SF. Mucormycoma of the colon: early diagnosis and successful management. American Journal of Roentgenology. 1985;145(4):739–741. doi: 10.2214/ajr.145.4.739. [DOI] [PubMed] [Google Scholar]
- Ahmad Z, Arshad S, Idrees R, Abdul-Ghafar J, Din NU. Fatal invasive gastrointestinal fungal infection in three non-immunocompromised patients. J Coll Physicians Surg Pak. 2019;29(2):181–184. doi: 10.29271/jcpsp.2019.02.181. [DOI] [PubMed] [Google Scholar]
- Altini C, Niccoli Asabella A, Ferrari C, Rubini D, Dicuonzo F, Rubini G. (18)F-FDG PET/CT contribution to diagnosis and treatment response of rhino-orbital-cerebral mucormycosis. Hell J Nucl Med. 2015;18(1):68–70. doi: 10.1967/s002449910167. [DOI] [PubMed] [Google Scholar]
- Barnes AMT, Crespo-Diaz RJ, Cohenour J, Kirsch JD, Arbefeville S, Ferrieri P. A noninvasive rhizopus infection with a bladder fungal ball in a patient with poorly controlled diabetes mellitus. Lab Med. 2017;49(1):75–79. doi: 10.1093/labmed/lmx060. [DOI] [PubMed] [Google Scholar]
- Chinen K, Matsumoto H, Fujioka Y. Cardiac mucormycosis presenting as a “fungus ball” in the left atrium. Intern Med. 2009;48(19):1781–1782. doi: 10.2169/internalmedicine.48.2611. [DOI] [PubMed] [Google Scholar]
- Dang Chun-Jiang, Li Ya-Jun, Zhan Feng-Hua, Shang Xiao-Ming. The Appearance of Pulmonary Mucormycosis on FDG PET/CT. Clinical Nuclear Medicine. 2012;37(8):801–803. doi: 10.1097/RLU.0b013e31825ae470. [DOI] [PubMed] [Google Scholar]
- Farmakiotis D, Kontoyiannis DP. Mucormycoses. SO Infect Dis Clin North Am. 2016;30(1):143–163. doi: 10.1016/j.idc.2015.10.011. [DOI] [PubMed] [Google Scholar]
- Forrester JD, Chandra V, Shelton AA, Weisser TG. Gastrointestinal mucormycosis requiring surgery in adults with hematological malignant tumors: literature review. Surg Infect. 2015;16(2):194–202. doi: 10.1089/sur.2013.232. [DOI] [PubMed] [Google Scholar]
- Liu Y, Wu H, Huang F, Fan Z, Xu B. Utility of 18F-FDG PET/CT in diagnosis and management of mucormycosis. Clin Nucl Med. 2013;38(9):e370–e371. doi: 10.1097/RLU.0b013e3182867d13. [DOI] [PubMed] [Google Scholar]
- Marutsuka T, Masuda Y, Saishoji T. Resected case of pulmonary mucormycosis. Kyobu Geka. 2013;66(3):223–226. [PubMed] [Google Scholar]
- Rashid S, Ben Abid F, Babu S, et al. Fatal renal mucormycosis with Apophysomyces elegans in an apparently healthy male. Aging Male. 2019;16:1–4. doi: 10.1080/13685538.2019.1586871. [DOI] [PubMed] [Google Scholar]
- Song B-I. F-18 fluorodeoxyglucose positron emission tomography/computed tomography image of gastric mucormycosis mimicking advanced gastric cancer: a case report. World J Clin Cases. 2019;7(10):1155–1160. doi: 10.12998/wjcc.v7.i10.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The images and biopsy samples remain available in our database.