Abstract
Objective
Contemporary management of patients with neuro-oncologic disease requires an understanding of approvals by the US Food and Drug Administration (FDA) related to nervous system tumors. To summarize FDA updates applicable to neuro-oncology practitioners, we sought to review oncology product approvals and Guidances that were pertinent to the field in the past year.
Methods
Oncology product approvals between January 1, 2020, and December 31, 2020, were reviewed for clinical trial outcomes involving tumors of the nervous system. FDA Guidances relevant to neuro-oncology were also reviewed.
Results
Five oncology product approvals described outcomes for nervous system tumors in the year 2020. These included the first regulatory approval for neurofibromatosis type 1: selumetinib for children with symptomatic, inoperable plexiform neurofibromas. Additionally, there were 4 regulatory approvals for non-central nervous system (CNS) cancers that described clinical outcomes for patients with brain metastases. These included the approval of tucatinib for metastatic human epidermal growth factor receptor 2 (HER2)-positive breast cancer including patients with brain metastases, brigatinib for anaplastic lymphoma kinase (ALK)-positive non-small cell lung cancer (NSCLC), and pralsetinib and selpercatinib for RET fusion-positive NSCLC. Finally, two FDA Guidances for Industry, “Cancer Clinical Trial Eligibility Criteria: Brain Metastases” and “Evaluating Cancer Drugs in Patients with Central Nervous System Metastases” were published to facilitate drug development for and inclusion of patients with CNS metastases in clinical trials.
Conclusions
Despite the challenges of the past year brought on by the COVID-19 pandemic, progress continues to be made in neuro-oncology. These include first-of-their-kind FDA approvals and Guidances that are relevant to the management of patients with nervous system tumors.
Keywords: Brain metastasis, Clinical trial, Neuro-oncology, Regulatory
Introduction
Contemporary neuro-oncology encompasses a broad range of pathologies and requires an up-to-date understanding of recent advances in care. These advances include US Food and Drug Administration (FDA) regulatory approvals and Guidance documents relevant to the field. Among oncology drug approvals, neuro-oncology-specific approvals typically account for only a small fraction [1]. However, advances related to non-central nervous system (CNS) cancers may also apply to neuro-oncology, particularly in regards to CNS metastases. These require a broad understanding of the cancer treatment landscape by neuro-oncologists, radiation oncologists, and neurosurgeons.
Over the past year, significant progress has been made in oncology, including efforts overseen by the FDA and its Oncology Center of Excellence (OCE) [2]. In this report we review approvals that are relevant to neuro-oncologists and neurosurgeons and FDA Guidance documents relevant to clinical investigators studying neuro-oncologic disorders.
Marketing approvals relevant to neuro-oncology in 2020
US FDA oncology marketing approvals between January 1, 2020, and December 31, 2020, were reviewed for neuro-oncology relevance. Sixty-one approvals for new molecular entities and supplements were identified during this time period [2, 3]. Oncology products whose prescription drug labels described clinical trial data (Sect. 14) related to tumors involving the nervous system were included. A total of 5 approvals described nervous system efficacy data (Table 1), including 1 indication for patients with neurofibromatosis type 1 (NF1) and 4 indications for patients with non-CNS primary cancers.
Table 1.
Oncology product approvals reporting neuro-oncology outcomes in product labeling between January 1, 2020 and December 31, 2020
| Oncology product | Approval date | Approval type | Indication | Neuro-oncology relevance |
|---|---|---|---|---|
| Selumetinib | 4/10/2020 | Regular | Neurofibromatosis Type 1 | Plexiform neurofibromas |
| Tucatinib | 4/17/2020 | Regular | HER2 + breast cancer | Brain metastases |
| Selpercatinib | 5/8/2020 | Accelerated | RET fusion + NSCLC | Brain metastases |
| Brigatinib | 5/22/2020 | Regular | ALK + NSCLC | Brain metastases |
| Pralsetinib | 9/4/2020 | Accelerated | RET fusion + NSCLC | Brain metastases |
HER2 + human epidermal growth factor receptor 2-positive, RET rearranged during transfection, NSCLC non-small cell lung cancer, ALK anaplastic lymphoma kinase
Selumetinib for NF1
On April 10, 2020, selumetinib was approved for pediatric patients (≥ 2 years old) with NF1-associated symptomatic, inoperable plexiform neurofibromas. NF1 is a tumor predisposition syndrome with a prevalence of approximately 1 in every 3000 individuals and results in the development of peripheral and plexiform neurofibromas [4, 5]. Plexiform neurofibromas are large tumors that grow from peripheral nerves throughout the body and can be a significant cause of morbidity depending on location. Although typically benign, plexiform neurofibromas can transform into malignant peripheral nerve sheath tumors (MPNSTs). Selumetinib is an oral inhibitor of mitogen-activated protein kinase (MAPK) kinase (MEK) that is affected by loss of the tumor suppressor Neurofibromin 1. This approval was significant in that it marked the first FDA-approved therapy for children with NF1.
Approval was based on a National Cancer Institute (NCI)-sponsored study (SPRINT, NCT01362803) that evaluated the efficacy of selumetinib (25 mg/m2 orally, twice a day) in 50 pediatric patients with NF1 [6, 7]. This multi-center, open-label, single-arm trial included pediatric patients with NF1 (ages 3–18 years) with a measurable plexiform neurofibroma. All patients had defined morbidity caused by their target lesion and were treated until disease progression or unacceptable toxicity. The primary endpoint was investigator-assessed overall response rate (ORR), defined as a > 20% reduction in tumor volume per Response Evaluation in Neurofibromatosis and Schwannomatosis (REiNS) criteria and confirmed by consecutive magnetic resonance imaging (MRI), 3–6 months apart [8].
Objective responses, all partial, were observed in 33 patients (ORR 66%; 95% CI 51–79%) by investigator assessment. The median time to onset of response was 7.2 months (range: 3.3 months to 1.6 years). Duration of response was greater than 12 months in 82% of patients. Independent centralized review demonstrated responses in 22 patients (ORR 44%; 95% CI 30–59%). Outcomes from this single-arm trial were referenced against natural history data provided by the NCI, which confirmed that spontaneous regression of neurofibromas in NF1 was uncommon, however a formal statistical analysis was not performed [9]. Clinical outcome assessments that evaluated plexiform neurofibroma-related symptoms, functional impairment, and disfigurement were used to support the clinical relevance of treatment with selumetinib [7, 9].
Safety was assessed in a larger pooled population of 74 children with NF1 who received selumetinib. The safety profile was found to be consistent with the drug class of MEK inhibitors [9]. The most common adverse reactions (occurring in ≥ 40%) were: vomiting, rash, abdominal pain, diarrhea, nausea, dry skin, fatigue, musculoskeletal pain, pyrexia, stomatitis, headache, paronychia, and pruritis [9].
Tucatinib for HER2+ metastatic breast cancer
On April 17th, 2020 tucatinib was approved, in combination trastuzumab and capecitabine, for adult patients with advanced unresectable or metastatic human epidermal growth factor receptor 2 (HER2)-positive breast cancer, including patients with brain metastases, who have received one or more prior anti-HER2-based regimens for metastatic disease. This was the first FDA approval that specified patients with brain metastases in the indication statement, which was significant to this population as approximately 30–50% of patients with HER2-positive breast cancer will develop CNS metastases [10–12]. This was also the first application for a new molecular entity to utilize Project Orbis, an international collaboration led by the FDA Oncology Center of Excellence that allows concurrent review among international regulatory agencies (Box). For tucatinib, collaborative review included the Australian Therapeutic Goods Administration, Health Canada, Singapore’s Health Sciences Authority, and Switzerland’s Swissmedic.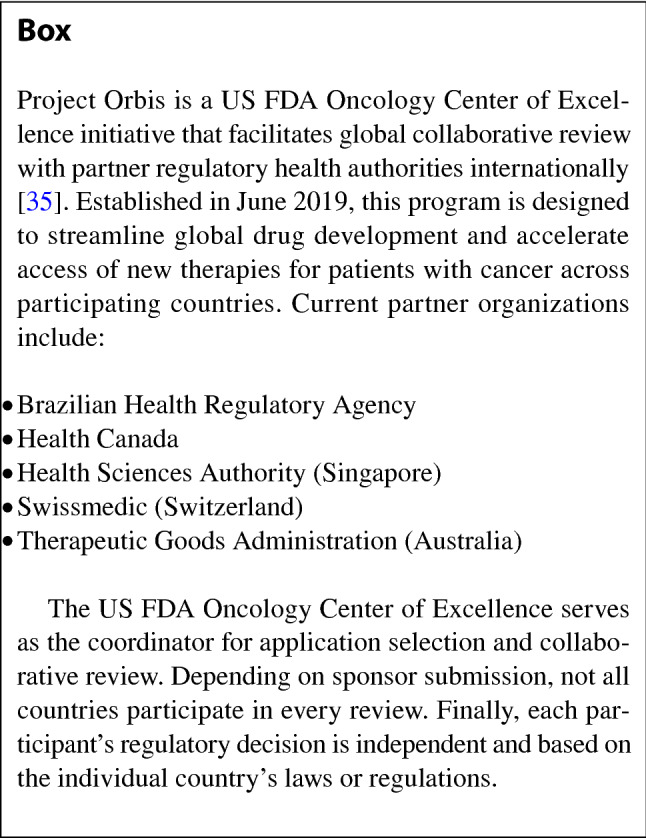
Approval of tucatinib was based on results of a randomized (2:1), double-blind, placebo-controlled trial (HER2CLIMB, NCT02614794), which included 612 patients with HER2-positive metastatic breast cancer who had previously received trastuzumab, pertuzumab, and ado-trastuzumab emtansine (T-DM1) [13, 14]. Patients were randomized to receive either tucatinib (300 mg twice daily) plus trastuzumab and capecitabine (n = 410) or placebo plus trastuzumab and capecitabine (n = 202). Use of capecitabine, with known activity for breast cancer brain metastases, in both arms of the study, allowed for inclusion of patients with active brain metastases [15]. Initially, 480 patients were randomized; subsequently a protocol amendment increased the sample size to 600 to include additional patients with brain metastases. The primary endpoint was progression-free survival (PFS), however PFS in the sub-population of patients with history or presence of brain metastases (PFSbrainmets) was a key secondary endpoint with alpha allocation and a pre-specified analysis plan [16].
Forty-eight percent of patients had a history of or present brain metastases at treatment. Brain metastases were considered active (either untreated or treated and progressive) in 28% of patients. Median PFSbrainmets was 7.6 months in the tucatinib arm (n = 198; 95% CI 6.2–9.5 months) and 5.4 months in the placebo arm (n = 93; 95% CI 4.1–5.7 months), which represented a significant difference (Hazard Radio [HR] 0.48; 95% CI 0.34–0.69; P < 0.00001).[14, 16, 17]. Although exploratory, in the subset of patients with active brain metastases, median PFS was also greater in the tucatinib arm compared to the control arm (9.5 vs. 4.1 months; HR, 0.36; 95% CI 0.22–0.57; P < 0.00010). Grade 3 or worse adverse reactions that occurred in ≥ 5% of patients on the tucatinib arm included diarrhea, palmar-plantar erythrodysesthesia (hand-foot syndrome), and hepatotoxicity [14].
This study and the subsequent regulatory approval demonstrate the feasibility of designing and implementing a clinical trial to specifically evaluate a therapy in patients with brain metastases that meets regulatory standards. This was supported by the study’s inclusion of a broad group of patients with brain metastases including those with active brain metastases, use of a drug in both arms with known CNS activity, identification of patients with brain metastases as a key subpopulation in the pre-specified statistical analysis plan, and evaluation of both CNS and systemic outcomes together in this subpopulation (PFSbrainmets).
Other oncology approvals with relevant neuro-oncology efficacy results
Three additional oncology approvals included efficacy data relevant to neuro-oncology (Table 1). All three approvals specified indications for non-small cell lung cancer (NSCLC), reporting outcome data for brain metastases. Unlike the clinical trial used to support approval for tucatinib, these studies were not designed to support an indication specifically for the sub-population of patients with brain metastases.
On May 8, 2020 selpercatinib was granted accelerated approval for adult patients with metastatic RET fusion-positive NSCLC. RET fusions have been identified in 1–2% of NSCLCs and have been suggested to be associated with a relatively high frequency of brain metastases [18, 19]. Selpercatinib was studied in a multi-center, open-label trial (LIBRETTO-001) that included patients with RET fusion-positive NSCLC and thyroid cancer, as well as RET-mutant medullary thyroid cancer [20, 21]. One hundred five patients with metastatic NSCLC who were previously treated with platinum chemotherapy were included. Among this cohort, patients with previously treated or untreated brain metastases were included if either asymptomatic or neurologically stable for at least 2 weeks prior to the study [20]. In total, 11 patients with measurable brain metastases by RECIST criteria (version 1.1) were treated; no patient received CNS radiation therapy within 2 months of study entry. Objective responses in intracranial lesions were observed in 10 patients as assessed by independent centralized review, with 3 complete responses and 7 partial responses; all responders had duration of response of ≥ 6 months [21].
On September 4, 2020, pralsetinib was granted accelerated approval for the treatment of adult patients with metastatic RET fusion-positive NSCLC [22]. Pralsetinib was studied in a multi-center, open-label trial (ARROW) that enrolled patients with tumors harboring RET alterations, including 87 patients with metastatic RET fusion-positive NSCLC who were previously treated with platinum chemotherapy. Patients with CNS metastases were included if they were asymptomatic and had stable or decreasing steroid requirements within 2 weeks of enrollment. Eight patients had measurable brain metastases at baseline and no patient received radiation therapy to the brain within 2 months prior to study entry. Objective responses in intracranial lesions were observed in 4 patients as assessed by independent centralized review, including 2 complete responses; 75% of responders had a duration of response ≥ 6 months.
On May 22, 2020, brigatinib was approved for adult patients with anaplastic lymphoma kinase (ALK)-positive metastatic NSCLC, regardless of prior therapy [23]. Brigatinib was studied in a randomized, multi-center, open-label trial (ALTA 1L) that included patients with advanced ALK-positive NSCLC who had not previously received another ALK-targeted therapy [24]. Patients with CNS metastases were included if they were asymptomatic and had stable or decreasing steroid requirements within 7 days of enrollment. Patients were randomized to receive either brigatinib (n = 137) or crizotinib (n = 138) and the presence of CNS metastases was among the stratification factors. Eighteen patients in the brigatinib arm had measurable CNS disease by RECIST criteria (version 1.1). By blinded independent review, the intracranial overall response rate was 78% (95% CI 52–94%) with complete responses in 28%. Intracranial duration of response was based on the time from first measured response to intracranial progression of any kind (new lesions, target lesion growth by RECIST criteria, or unequivocal growth of a non-target lesion) or death. Among the 14 patients with intracranial response in the brigatinib arm, 64% had a duration of response ≥ 24 months by Kaplan–Meier analysis [23].
Mortality rates for NSCLC continue to improve, following the approval of several immunotherapies and targeted therapies for this indication [25]. As brain metastases are among the most common cause of death in NSCLC, results such as those listed above suggest that this improvement in mortality may extend to patients with brain metastases in the future [26, 27]. While these results presented above are descriptive and considered exploratory, future analyses may be strengthened by trials specifically designed to study outcomes in patients with NSCLC brain metastases, just as HER2CLIMB did by using the PFSbrainmets endpoint for patients with breast cancer brain metastases.
US FDA guidance documents relevant to neuro-oncology
FDA Guidance documents represent an opportunity for the Agency to publish its interpretation of regulatory issues and provide guidance to industry. Unlike the Code of Federal Regulation, Guidance documents do not generate legally binding requirements. Guidance documents are drafted by FDA staff and undergo a period in which they are open to public comment (Level 1 Guidances) before being finalized. In 2020, FDA released two Guidance documents specific to neuro-oncology that are discussed herein: Cancer Clinical Trial Eligibility: Brain Metastases (Finalized) and Evaluating Cancer Drugs in Patients with Central Nervous System Metastases: Guidance for Industry (Draft) [28, 29].
Cancer clinical trial eligibility: brain metastases
CNS metastases are an increasingly common manifestation of certain cancers but remain a frequent exclusion criterion for cancer clinical trials. An analysis of 297 oncology IND applications submitted in 2015 to the FDA found that presence of known, active or symptomatic CNS metastases were a common exclusion criteria (77.4%) [30]. Among these protocols, 140 (47.1%) allowed enrollment of patients with treated or stable brain metastases. Similarly, a review of enrollment criteria among 413 NSCLC clinical trial registrations on ClinicalTrials.gov revealed that 14% of trials excluded patients with any history of CNS metastases and 19% strictly excluded patients with leptomeningeal disease [31]. An additional 41% of studies only allowed patients with CNS disease who had received prior local therapy. Expanding inclusion criteria to allow for more patients with CNS metastases could better represent the populations of patients with cancer, but must be balanced against concerns of patient protection [32]. The American Society of Clinical Oncology (ASCO) and Friends of Cancer Research (FOCR) working groups initially addressed these concerns in 2017 [33]. Building on this work and as part of a series of Guidance documents on broadening eligibility criteria for clinical trials, the FDA published the Guidance document entitled “Cancer clinical trial eligibility: Brain Metastases” in July 2020 [28].
The Guidance document recommends distinction between patients with (1) treated/stable brain metastases, (2) active brain metastases, and (3) leptomeningeal metastases. Recommendations for clinical trial inclusion are specific to each of these categories and are summarized in Table 2. Recommendations for exclusion criteria relevant to patients with brain metastases also described. These include considerations for drugs with potential to increase bleeding risk or patients with increased risk of hemorrhage, drugs with the potential to lower seizure threshold or patients with increased seizure risk, drugs with cytochrome P450 (CYP) interactions in patients on CYP inducing antiepileptics, and drugs that may be affected by concomitant corticosteroid use in patients who are corticosteroid-dependent.
Table 2.
Recommendations for clinical trial inclusion among patients with CNS metastases
| CNS disease type | Recommendations |
|---|---|
| Treated/stable brain metastases |
(1) Patients with treated/stable brain metastases should be included in trials unless there is a strong rationale to exclude such patients (2) Inclusion of patients with treated/stable brain metastases should not be dependent on whether the drug’s pharmacological properties predict penetration of the blood–brain barrier (3) Patients should be neurologically stable prior to study entry to mitigate the uncertainty of attributing CNS toxicity to the investigational drug or underlying disease. To achieve this, consider limiting enrollment to patients receiving a stable or decreasing corticosteroid dose at the time of study entry |
| Active brain metastases |
(1) Patients with active brain metastases should not be automatically excluded from trials and should be included if the treating physician determines that immediate CNS specific treatment is unlikely to be required and: (a) there is a strong rationale for likelihood of CNS activity, or (b) CNS metastases are common in the target population (2) For drugs with known CNS toxicities, exclusion of patients with active brain metastases may be justified, especially early in drug development |
| Leptomeningeal metastases |
(1) Patients with LMD should not be automatically excluded from trials and should be included if:—the treating physician determines that immediate CNS specific treatment is unlikely to be required, (a) the drug is anticipated to have CNS activity and is relevant for the primary tumor, and (b) there is strong scientific rationale to support the likelihood of benefit, based on pre-existing data |
CNS central nervous system, LMD leptomeningeal disease
Adapted from: US Food and Drug Administration (2019) Cancer Clinical Trial Eligibility Criteria: Brain Metastases Guidance for Industry [28]
A final concern addressed by this Guidance is the reluctance of providers to perform baseline CNS imaging prior to study enrollment. Baseline screening MRI may be avoided out of concern that asymptomatic lesions identified at screening may trigger clinical trial exclusion [33]. Regardless, baseline CNS screening provides critical information on the CNS efficacy and safety of oncology drug products. The Guidance recommends baseline CNS imaging for (1) patients with a history of brain metastases, (2) populations at increased risk of brain metastasis, (3) trials with specific concerns related to the inclusion of patients with brain metastases, and (4) if study aims to demonstrate CNS efficacy.
Evaluating cancer drugs in patients with central nervous system metastases: draft guidance for industry
As clinical trial eligibility expands for patients with CNS metastases, consistent recommendations for evaluation of CNS efficacy in oncology products will become increasingly necessary. To address these concerns, a Guidance document addressing clinical trial design considerations for patients with CNS metastases was drafted for public comment [29]. The draft Guidance document addresses clinical trial design, in particular the challenges related to prior CNS-directed therapies, imaging assessment of CNS metastases, study endpoints, and leptomeningeal disease [34]. Finally, the document addresses the concern that CNS disease should not be evaluated in isolation and recommends systemic imaging assessment be performed in tandem with CNS disease assessment.
Conclusions
Despite the challenges related to the COVID-19 pandemic, significant progress continues to be made in neuro-oncology, including regulatory efforts at the FDA. Several marketing approvals reported effects in brain metastases, which are relevant to multi-disciplinary care by neuro-oncologists and neurosurgeons caring for patients who meet these indications. This year also saw the first marketing approval for an oncology drug product for NF1. Additionally, Guidance documents regarding clinical trials including patients with CNS metastases were published to provide recommendations that represent the FDA’s current thinking on this subject and carry relevance for investigators studying cancers with risk of nervous system metastasis.
Acknowledgements
We acknowledge the contributions of our colleagues at the US Food and Drug Administration (FDA) who contributed to this work, specifically Kirsten Goldberg. The views expressed in this article are those of the authors and do not necessarily reflect the official views or policies of the US FDA.
Author contributions
GUM: Conception and design, Wrote the manuscript. AKB: Conception and design, Critical review of the manuscript. DB: Critical review of the manuscript. EL: Critical review of the manuscript. JK: Critical review of the manuscript. LPS: Critical review of the manuscript. AJ: Critical review of the manuscript. MS: Critical review of the manuscript. SW: Critical review of the manuscript. LAK: Critical review of the manuscript. MRT: Critical review of the manuscript. RP: Critical review of the manuscript. JAB: Critical review of the manuscript, Supervision. HS: Critical review of the manuscript, Supervision.
Declarations
Conflict of interest
All Authors declare that they have no competing interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zhou J, Vallejo J, Kluetz P, Pazdur R, Kim T, Keegan P, Farrell A, Beaver JA, Sridhara R. Overview of oncology and hematology drug approvals at US Food and Drug Administration between 2008 and 2016. J Natl Cancer Inst. 2019;111:449–458. doi: 10.1093/jnci/djy130. [DOI] [PubMed] [Google Scholar]
- 2.US Food and Drug Administration (2020) Oncology center of excellence 2020 annual report.
- 3.Amiri-Kordestani L, Pazdur R. Oncology approvals in 2020: a year of firsts in the midst of a pandemic. Nat Rev Clin Oncol. 2021;18:2020–2021. doi: 10.1038/s41571-021-00477-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huson SM, Compston DA, Harper PS. A genetic study of von Recklinghausen neurofibromatosis in south east Wales. II. Guidelines for genetic counselling. J Med Genet. 1989;26:712–721. doi: 10.1136/jmg.26.11.712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Friedman JM. Epidemiology of neurofibromatosis type 1. Am J Med Genet - Semin Med Genet. 1999;89:1–6. doi: 10.1002/(SICI)1096-8628(19990326)89:1<1::AID-AJMG3>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- 6.Dombi E, Baldwin A, Marcus LJ, et al. Activity of selumetinib in neurofibromatosis type 1–related plexiform neurofibromas. N Engl J Med. 2016;375:2550–2560. doi: 10.1056/NEJMoa1605943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gross AM, Wolters PL, Dombi E, et al. Selumetinib in children with inoperable plexiform neurofibromas. N Engl J Med. 2020;382:1430–1442. doi: 10.1056/NEJMoa1912735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dombi E, Ardern-Holmes SL, Babovic-Vuksanovic D, et al. Recommendations for imaging tumor response in neurofibromatosis clinical trials. Neurology. 2013 doi: 10.1212/01.wnl.0000435744.57038.af. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.US Food and Drug Administration (2020) Drug Approval Package: Koselugo (selumetinib). In: Drugs@FDA. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2020/213756Orig1s000MultidisciplineR.pdf.
- 10.Leyland-Jones B. Human epidermal growth factor receptor 2-positive breast cancer and central nervous system metastases. J Clin Oncol. 2009;27:5278–5286. doi: 10.1200/JCO.2008.19.8481. [DOI] [PubMed] [Google Scholar]
- 11.Pestalozzi BC, Holmes E, de Azambuja E, et al. CNS relapses in patients with HER2-positive early breast cancer who have and have not received adjuvant trastuzumab: a retrospective substudy of the HERA trial (BIG 1–01) Lancet Oncol. 2013;14:244–248. doi: 10.1016/S1470-2045(13)70017-2. [DOI] [PubMed] [Google Scholar]
- 12.Brufsky AM, Mayer M, Rugo HS, et al. Central nervous system metastases in patients with HER2-positive metastatic breast cancer: Incidence, treatment, and survival in patients from registHER. Clin Cancer Res. 2011;17:4834–4843. doi: 10.1158/1078-0432.CCR-10-2962. [DOI] [PubMed] [Google Scholar]
- 13.Murthy RK, Loi S, Okines A, et al. Tucatinib, trastuzumab, and capecitabine for HER2-positive metastatic breast cancer. N Engl J Med. 2020;382:597–609. doi: 10.1056/NEJMoa1914609. [DOI] [PubMed] [Google Scholar]
- 14.Shah M, Wedam S, Cheng J, et al. FDA approval summary: tucatinib for the treatment of patients with advanced or metastatic HER2-positive breast cancer. Clin Cancer Res. 2021;27(5):1220–1226. doi: 10.1158/1078-0432.CCR-20-2701. [DOI] [PubMed] [Google Scholar]
- 15.Ekenel M, Hormigo AM, Peak S, DeAngelis LM, Abrey LE. Capecitabine therapy of central nervous system metastases from breast cancer. J Neurooncol. 2007;85:223–227. doi: 10.1007/s11060-007-9409-0. [DOI] [PubMed] [Google Scholar]
- 16.Lin NU, Borges V, Anders C, et al. Intracranial efficacy and survival with tucatinib plus trastuzumab and capecitabine for previously treated HER2-positive breast cancer with brain metastases in the HER2CLIMB trial. J Clin Oncol. 2020;38:2610–2619. doi: 10.1200/JCO.20.00775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.US Food and Drug Administration (2020) Drug approval package: Tukysa (tucatinib). In: Drugs@FDA. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2020/213411Orig1s000MultidisciplineR.pdf.
- 18.Drilon A, Lin JJ, Filleron T, et al. Frequency of brain metastases and multikinase inhibitor outcomes in patients with RET–rearranged lung cancers. J Thorac Oncol. 2018;13:1595–1601. doi: 10.1016/j.jtho.2018.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang R, Hu H, Pan Y, et al. RET fusions define a unique molecular and clinicopathologic subtype of non-small-cell lung cancer. J Clin Oncol. 2012;30:4352–4359. doi: 10.1200/JCO.2012.44.1477. [DOI] [PubMed] [Google Scholar]
- 20.Drilon A, Oxnard GR, Tan DSW, et al. Efficacy of selpercatinib in RET fusion-positive non–small-cell lung cancer. N Engl J Med. 2020;383:813–824. doi: 10.1056/NEJMoa2005653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bradford D, Larkins E, Mushti SL, et al. FDA approval summary: selpercatinib for the treatment of lung and thyroid cancers with RET gene mutations or fusions. Clin Cancer Res. 2020;27:2130–2135. doi: 10.1158/1078-0432.CCR-20-3558. [DOI] [PubMed] [Google Scholar]
- 22.US Food and Drug Administration (2020) Drug approval package: Gavreto (pralsetinib). In: Drugs@FDA. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2021/214701Orig1s000TOC.cfm.
- 23.ARIAD Pharmaceuticals (2020) Alunbrig® (brigatinib) [package insert]. In: Drugs@FDA. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/208772s008lbl.pdf.
- 24.Camidge DR, Kim HR, Ahn MJ, et al. Brigatinib versus crizotinib in advanced ALK inhibitor-naive ALK-positive non-small cell lung cancer: second interim analysis of the phase III ALTA-1L trial. J Clin Oncol. 2020;38:3592–3603. doi: 10.1200/JCO.20.00505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Singh H, Pazdur R (2021) Contribution of early clinical benefit end points to decreased lung cancer mortality rates. JAMA Oncol 10.1001/jamaoncol.2020.8090 [DOI] [PubMed]
- 26.Rotolo F, Dunant A, Le Chevalier T, Pignon JP, Arriagada R. Adjuvant cisplatin-based chemotherapy in nonsmall-cell lung cancer: new insights into the effect on failure type via a multistate approach. Ann Oncol. 2014;25:2162–2166. doi: 10.1093/annonc/mdu442. [DOI] [PubMed] [Google Scholar]
- 27.Robinson AG, Young K, Balchin K, Ashworth A, Owen T. Causes of death and subsequent treatment after initial radical or palliative therapy of stage III non-small-cell lung cancer. Curr Oncol. 2015;22:333–340. doi: 10.3747/co.22.2432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.US Food and Drug Administration (2019) Cancer clinical trial eligibility criteria: brain metastases guidance for industry. https://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM633132.pdf.
- 29.US Food and Drug Administration (2020) Evaluating cancer drugs in patients with central nervous system metastases guidance for industry DRAFT GUIDANCE. https://www.fda.gov/vaccines-blood-biologics/guidance-compliance-regulatory-information-biologics/biologics-guidances.
- 30.Jin S, Pazdur R, Sridhara R. Re-evaluating eligibility criteria for oncology clinical trials: analysis of investigational new drug applications in 2015. J Clin Oncol. 2017;35:3745–3752. doi: 10.1200/JCO.2017.73.4186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McCoach CE, Berge EM, Lu X, Barón AE, Ross Camidge D. A brief report of the status of central nervous system metastasis enrollment criteria for advanced non-small cell lung cancer clinical trials: a review of the clinicaltrials.gov trial registry. J Thorac Oncol. 2016;11:407–413. doi: 10.1016/j.jtho.2015.10.024. [DOI] [PubMed] [Google Scholar]
- 32.Beaver JA, Ison G, Pazdur R. Reevaluating eligibility criteria—balancing patient protection and participation in oncology trials. N Engl J Med. 2017;376:1504–1505. doi: 10.1056/NEJMp1615879. [DOI] [PubMed] [Google Scholar]
- 33.Lin NU, Prowell T, Tan AR, et al. Modernizing clinical trial eligibility criteria: recommendations of the American society of clinical oncology-friends of cancer research brain metastases working group. J Clin Oncol. 2017;35:3760–3773. doi: 10.1200/JCO.2017.74.0761. [DOI] [PubMed] [Google Scholar]
- 34.Marur S, Beaver JA, Pazdur R (2021) Evaluating cancer drugs in patients with central nervous system metastases. JAMA Oncol [DOI] [PubMed]
- 35.de Claro RA, Spillman D, Hotaki LT, et al. Project orbis: global collaborative review program. Clin Cancer Res. 2020;26:6412–6416. doi: 10.1158/1078-0432.CCR-20-3292. [DOI] [PubMed] [Google Scholar]


