Abstract
COVID‐19 cases are increasing daily worldwide. With such emerging disease, the medical community should be aware of atypical clinical presentations in order to help with correct diagnosis, and to take the proper measures to isolate and treat patients to avoid healthcare professionals being infected and to limit its spread (SARS‐CoV‐2). Thrombogenesis in COVID‐19 has been described in few cases, but a thrombosis of a large digestive vessel has not been documented so far. Mesenteric ischemia due to an obstruction of a large vessel may be a new presentation of COVID‐19 infection.
Keywords: COVID‐19 infection, gastrointestinal symptoms, ischemia, surgery, vessel obstruction
Atypical clinical presentation of COVID‐19 infection is rare. It represents 10%‐15%. In front of abdominal pain, it is appropriate to think about Thrombogenesis disorders related to COVID infection in parallel with gastrointestinal and surgical causes.

1. INTRODUCTION
COVID‐19 cases are increasing daily worldwide. With such emerging disease, the medical community should be aware of atypical clinical presentations in order to help with correct diagnosis, and to take the proper measures to isolate and treat patients to avoid healthcare professionals being infected and to limit its spread.
COVID‐19 Infection may be asymptomatic or cause an acute respiratory disease. The typical clinical manifestations are general and respiratory symptoms: fever, shortness of breath, and cough. Bilateral pneumonia, acute respiratory distress syndrome, or death can occur. Less common symptoms included headache, diarrhea, nausea, and vomiting. However, diarrhea and abdominal pain as the first symptom is rarely reported.
The pathophysiology of these two symptoms likely relies on an inflammatory process such as gastroenteritis among other reasons. 1
COVID‐19‐associated coagulopathy is recognized to be one of the key drivers of mesenteric vascular thrombosis; however, there is a lack of both radiologic and histologic evidence for large arterial and venous mesenteric vessel thrombosis. 2
We report a case of COVID‐19 infection causing mesenteric ischemia diagnosed early and has been treated with Heparin.
2. CASE REPORT
A 68‐year‐old no smoking male patient with no past medical history, presented with epigastric pain and diarrhea since 4 days. In the physical examination, he was febrile at 38.5°C and he had hypogastric tenderness. Blood test showed WBC at 17 660/mL, C‐reactive protein at 125 mg/L, and D‐Dimers were elevated at 6876 ng/mL. An abdominal CT scan showed a thickening of the right colon wall and the last 30 cm of the small bowl associated (Figure 1) with an obstruction of the terminal segment of the ileo colic artery (Figure 2). There were no other signs of ischemia. We decided to put the patient under medical treatment with unfractionated heparine. On the second day of his stay, he developed a dry cough and the abdominal pain decreased. We performed a laparoscopy on the third day that showed a normal condition of the colon and the small bowl. With the appearance of respiratory signs and the pandemic context, we decided to perform a COVID‐19 RT‐PCR test to the patient. He tested positive. Fortunately, the use of protective clothing was mandatory to take any sample, and wearing a mask is compulsory among staff members and patients in our department. That prevented the spread of the infection during this patient stay. He was transferred to a COVID department established during the epidemic. After 1 week of treatment, the patient is asymptomatic with soft abdomen and normal rate of WBC and C‐reactive protein.
FIGURE 1.
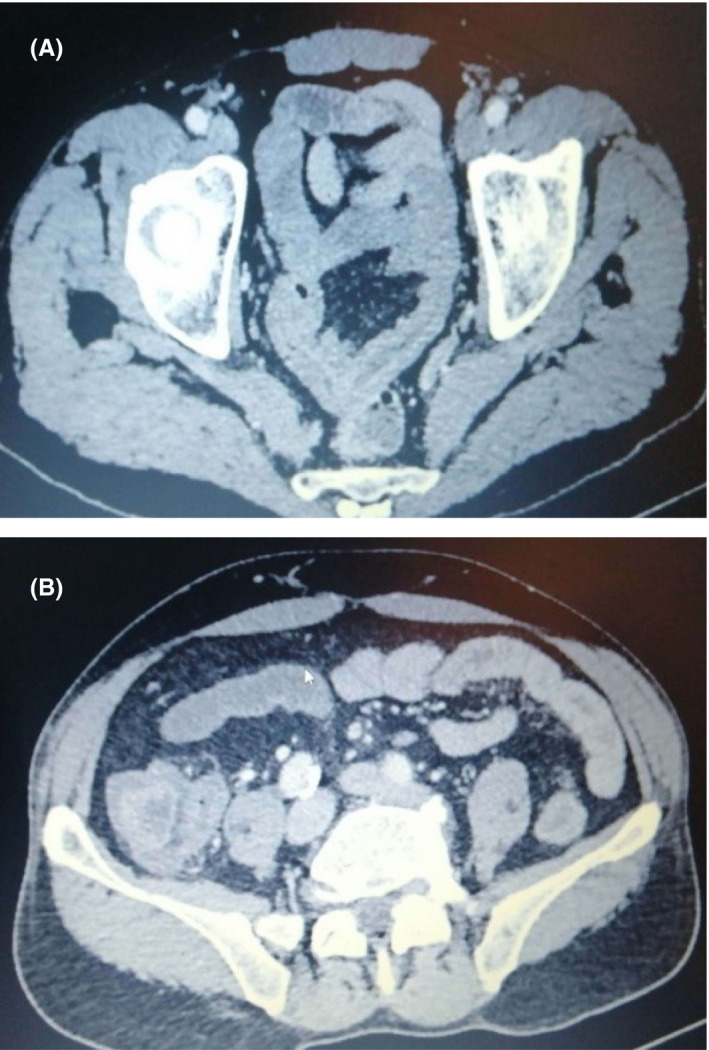
Small intestine (A) and colon (B) wall thickening
FIGURE 2.

CT scan image showing obstruction of the ileo colic artery
3. DISCUSSION
This case of mesenteric ischemia in a patient with COVID 19, with no risk of thrombogenesis highlights the variability of symptoms of this disease.
To our knowledge, we are among the first who described a case of mesenteric large vessel obstruction associated to the COVID 19 virus worldwide.
CT scan is known to be one of diagnostic means of COVID‐19. Besides bilateral multiple ground glass opacities at lung bases in chest CT scan, abdominal imaging findings such as small and large bowel wall thickening, fluid‐filled colon, pneumatosis intestinalis, pneumoperitoneum, intussusception, and ascites have also been reported. 3
Thrombogenesis in COVID‐19 has also been described in few cases and it can be attributed to the direct and indirect cytotoxic effects of the SARS‐CoV‐2 virus on vascular endothelium, due to the corona virus's affinity to the ACE‐2 receptor on endothelial surfaces. In fact, endothelial dysfunction is a principal determinant of micro vascular dysfunction by shifting the vascular equilibrium towards more vasoconstriction with subsequent organ ischemia, inflammation with associated tissue edema, and a pro coagulant state. 4 Endothelial injury is also evident from the direct invasion of endothelial cells by SARS‐CoV‐2 through angiotensin‐converting enzyme 2 (ACE‐2) receptors. Viral elements were found inside the endothelial cells. 5 Increased cytokines are released, such as interleukin (IL)‐6, activation of the complement pathways leading all to endothelial cells injuries. 5
This can explain vascular and neurological symptoms such as hypotension and altered mental status described in some patient, and the systematic use of prophylactic anticoagulation. 5 , 6
In our case, this phenomenon touched a large vessel rather than capillaries, which is why it was treatable by heparine.
To reduce the contamination rate properly, it is imperative to recognize SARS‐CoV‐2‐positive patients rapidly in order to deliver adapted care and to isolate them from the rest of the patients until their recovery. Early suspicion is also necessary to protect healthcare workers, who should use personal protective equipment in such cases.
It implies that, as long as the COVID‐19 pandemic is ongoing, patients presenting with nonexplained gastrointestinal symptoms should be managed as potentially infected and COVID‐19 diagnostic tests should be performed in time such is our case.
4. CONCLUSION
Life threatening manifestations of the corona virus disease are related mostly to the respiratory system, but due to thrombogenesis, other manifestations in gastrointestinal tract should be taken into account such as acute mesenteric ischemia.
CONFLICT OF INTEREST
The authors whose names are listed certify that they have conflict of interests.
AUTHOR CONTRIBUTIONS
Souhir Nasseh: involved in study conception and design. Trabelsi Med Mehdi and Haloui Nabil: acquired the data. Souhir Nasseh and Trabelsi Med Mehdi: analyzed and interpreted the data. Souhir Nasseh and Trabelsi Med Mehdi: drafted the manuscript. Oueslati Anouer, Jerraya Hichem, and Nouira Ramzi: involved in critical revision.
ETHICAL STATEMENT
This material is the authors' own original work, which has not been previously published elsewhere. All authors have been personally and actively involved in substantial work leading to the paper, and will take public responsibility for its content. Patient privacy has been respected.
ACKNOWLEDGMENTS
Published with written consent of the patient.
Nasseh S, Trabelsi MM, Oueslati A, Haloui N, Jerraya H, Nouira R. COVID‐19 and gastrointestinal symptoms: A case report of a Mesenteric Large vessel obstruction. Clin Case Rep. 2021;9:e04235. 10.1002/ccr3.4235
DATA AVAILABILITY STATEMENT
Data sharing not applicable.
REFERENCES
- 1. Gahide G, Frandon J, Vendrell J‐F. COVID‐19 patients presenting with afebrile acute abdominal pain. Clin Med. 2020;20(3):e4‐e6. 10.7861/clinmed.2020-0150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Parry AH, Wani AH, Yaseen M. Acute mesenteric ischemia in severe coronavirus‐19 (COVID‐19): possible mechanisms and diagnostic pathway. Academic Radiology. 2020;27(8):1190. 10.1016/j.acra.2020.05.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abdominal Radiology. doi: 10.1007/s00261-020-02739-5. [DOI]
- 4. Bonetti PO, Lerman LO, Lerman A. Endothelial Dysfunction. Arterioscler Thromb Vasc Biol. 2003;23(2):168‐175. 10.1161/01.ATV.0000051384.43104.FC [DOI] [PubMed] [Google Scholar]
- 5. Singhania N, Bansal S, Nimmatoori DP, Ejaz AA, McCullough PA, Singhania G. Current overview on hypercoagulability in COVID‐19. Am J Cardiovasc Drugs. 2020;20(5):393‐403. 10.1007/s40256-020-00431-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Singhania N, Bansal S, Singhania G. An atypical presentation of novel coronavirus disease 2019 (COVID‐19). Am J Med. 2020;133(7):e365‐e366. 10.1016/j.amjmed.2020.03.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable.


