Abstract
When temporal bone fractures are associated with facial palsy (FP) evolution the medical team have no much time to make a decision: to do or not to do a surgical approach? How to evaluate the necessity? When to do it and when is the correct time?
Keywords: facial nerve decompression, facial palsy, temporal bone fracture, Wallerian degeneration
When temporal bone fractures are associated with facial palsy (FP) evolution the medical team have no much time to make a decision: to do or not to do a surgical approach? How to evaluate the necessity? When to do it and when is the correct time?
1. CASE REPORT
A 23‐year‐old male involved in a high‐intensity automobile accident presented at the trauma scene traumatic brain injury (TBI) evolving to right‐sided subdural hematoma and immediate bilateral facial paralysis (FP). Patient was admitted to Intensive Care Unit and Neurosurgery team opted for a nonsurgical approach. Patient was discharged on the 12th day and referred to Ear, Nose, and Throat team only on the 16th day of FP, reporting bilateral hypoacusis and persistent bilateral facial palsy. Patient denied dizziness, tinnitus, otorrhagia, otorrhea, and rhinorrhea.
The otoscopy examination showed absence of external auditory meatus injuries and intact tympanic membrane associated with bilateral hemotympanum. The VII cranial nerve examination revealed complete bilateral postnuclear facial paralysis (House & Brackman Grade VI). All other cranial nerves evaluation was normal. Audiometry demonstrated mild conductive hearing loss in the right side and moderate conductive hearing loss in the left, with pure tone average (PTA, calculated at 0.5, 1, 2, 4 kHz) of 35 dB HL in the right ear and 55 dB HL in the left. Speech audiometry confirmed left hearing loss.
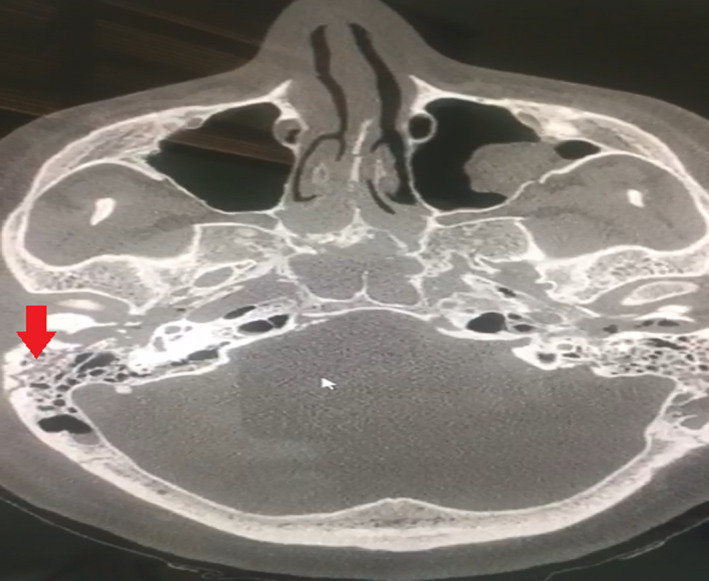
Maxillofacial computed tomography scan (CT scan) showed multiple nondisplaced fractures lines on the both sides of zygomatic and sphenoid bone and on the posterior wall of left maxillary bone. Temporal CT scan evidenced a longitudinal fracture on the right temporal bone and a transverse fracture on the left side, both sparing the otic capsule (Figures 1 and 2).
FIGURE 1.
CT‐Scan on the right side: Longitudinal fracture limited to the mastoid bony sparing the Otic Capsule
FIGURE 2.
CT‐Scan on the left side: Transversal fracture going from the mastoid bony toward the middle ear (closer to the ossicular chain). Even though the transversal direction of fracture line, it is sparing the Otic Capsule
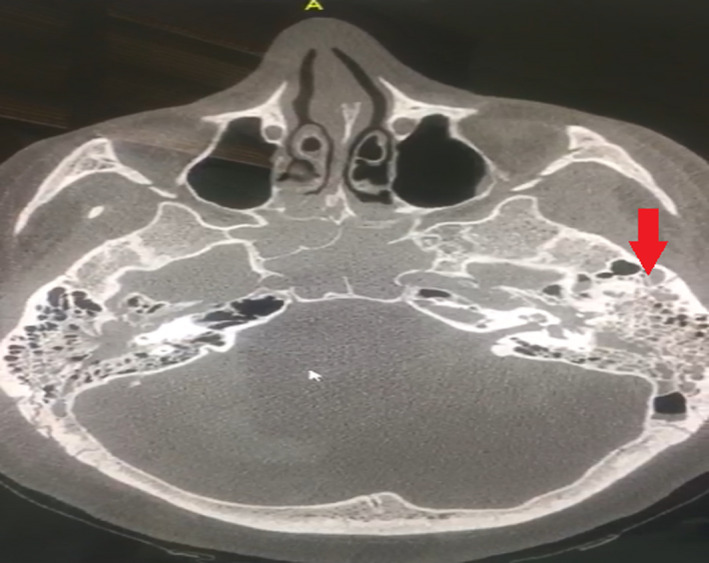
On the 18th day after trauma, it was performed an electroneuromyography revealing bilateral absence of muscular response to stimulus. Then, a facial nerve decompression on both sides was executed at the same surgical session. The right ear was the first approached where a fracture going toward the external auditory canal causing nerve dehiscence. During the posterior tympanotomy, it was possible to observe at the level of tympanic portion just below the incudostapedial joint, a compression of the facial nerve by a bone spike that was removed. There were the same patterns at the left side, but additionally, the incudostapedial joint was disarticulated and the stapes suprastructure was destroyed. The facial nerve decompression was executed followed the same techniques on both sides and extended from the geniculated ganglion to the stylomastoid foramen (Figures 3 and 4). The patient started physical therapy afterward and in one‐year follow‐up, he presented a House & Brackman facial palsy grade II bilaterally.
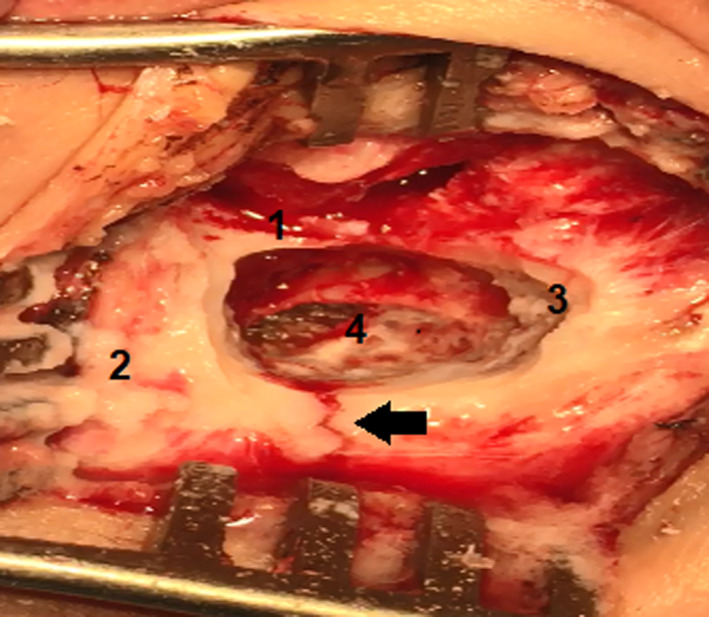
FIGURE 3.
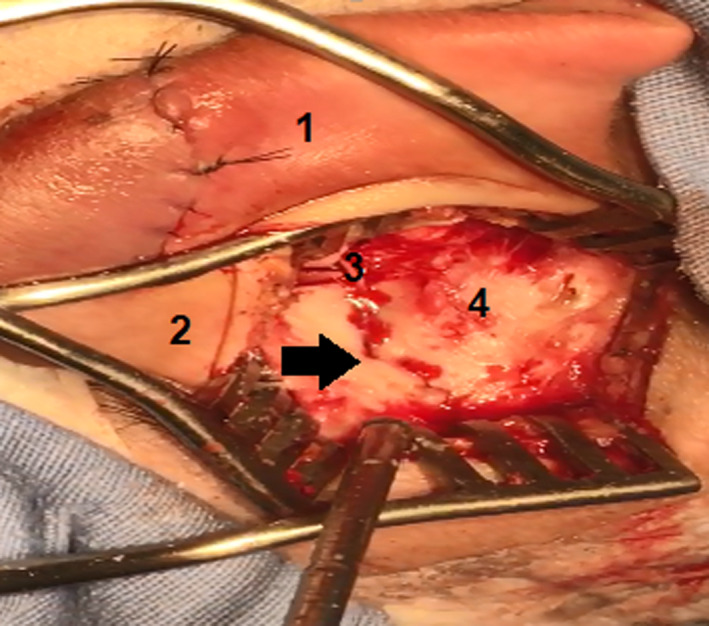
Transoperative View of the left side: 1‐Posterior part of pinna. 2‐Mastoid tip. 3‐Posterior bony of external ear canal. 4‐Tegmen tympani. Black Arrow‐Fracture line. The fracture line going toward the external ear canal, near to the region of mastoid portion of facial nerve
FIGURE 4.
Transoperative View of the right side: 1‐Posterior bony of external ear canal. 2‐mastoid tip. 3‐Tegmen tympani. 4‐Mastoid cavity after drilling had been done by a surgeon. Black Arrow‐Fracture line
2. DISCUSSION
Bilateral facial nerve paralysis is a rare entity, corresponding to less than 2% of all facial palsy cases. 1 The most important causes are trauma, infectious diseases (eg, mononucleosis, syphilis, Lyme disease, bilateral otitis media, and bilateral Herpes‐Zoster), neurological diseases (eg, multiple sclerosis, stroke, and neoplasms), and diseases which remain with uncertain etiologies, such Guillain‐Barre syndrome, Melkersson‐Rosenthal syndrome, sarcoidosis, and leukemia. 2
Cranial trauma associated with temporal bone fractures is responsible for 3% of all facial palsy (FP) cases, which can be traditional divided into longitudinal, transverse, and mixed fractures. 2 Recently, a new classification was proposed based on the otic capsule, dividing the fractures into otic capsule sparing and otic capsule disrupting. 3 The importance to classify the fracture type relies on its prediction of the severity of the signs and symptoms the patient can develop. Longitudinal fractures, usually sparing the otic capsule, correspond to the majority of all temporal bone fractures and are often associated with mild cases and absence of FP. Transverse fractures are less frequent, but more often associated with otic capsule disruption. Due to the fracture line path going toward the otic capsule, patients usually present some complications as cerebrospinal fluid fistulae (CSF), otic capsule damage, or facial nerve injury. 3 The current patient's CT scan evidenced a longitudinal fracture on the right temporal bone and a transverse fracture on the left side, both sparing the otic capsule. As already mentioned, longitudinal fracture predicts lower risk of facial nerve injury, however, our patient presented bilateral facial nerve lesion.
The risk of FP is 6 to 7% overall the temporal bone fractures, when 25% of them are acute, complete, and presenting at outset. The remaining 75% have partial facial nerve palsy at the first evaluation and subsequently worsens within one to 16 days 3 , 4 , 5 The management of facial paralysis due to temporal bone trauma is a challenging. It is not a simple decision select whether a patient should go under facial decompression surgery or not and might undergo to isolated medical treatment. 3
After any injury to the peripheral nerve, the process known as Wallerian degeneration occurs. It is an innate immune response, culminating in recruitment of macrophages (that will make the phagocytosis of degenerated myelin anterogradely to the lesion), and in activation of Schwan cells within the first 24 hours. These cells play an important role in this phenomenon dividing themselves rapidly into two daughter cells and upregulating the gene expression for proteins to assist the degeneration and reparation process. 6 The success of the regeneration depends on the degree of nerve injury. In 1943, Seddon described three basic types of injury: neuropraxia, axonotmesis, and neurotmesis. In 1951, Sunderland (SD) amplified it classifying injuries into five degrees as is described on Table 1. Highers degrees of SD are associated with higher facial palsy presentations. 3 , 6
TABLE 1.
Sunderland amplified classification
| Sunderland amplified classification | |
|---|---|
| Grade | Findings |
| Type I | Conduction block‐Neuropraxia |
| Type II | Axonal Injury‐Axonotmesis |
| Type III | Type II + Endoneurium Injury |
| Type IV | Type III + Perineurium Injury |
| Type V | Type IV + Epineurium Injury‐Neurotmesis |
The correct therapeutic decision relies on, through clinical evaluation, separating patients in two groups. First group includes patients who have acute, complete facial paralysis at onset, usually at the trauma scene. Normally, this group has a higher degree of SD and a potentially fully unrecoverable injury. 3 Second group includes patients who have a delayed facial paralysis onset, commonly associated with a less severe degree of dysfunction and greater capacity to recover. Steroid therapy should be given within the first 2 weeks regardless of the grade of the severity of the injury. A weekly follow‐up and diagnostics by EnoG on the 3th day will provide prognostic informations where the first group is associated with poor recovery in nerve function. 3 , 6
ENoG measures the evoked compound muscle action potential of the stimulated facial nerve, being the most useful electrodiagnostic test for prognostic information. It should be done after 3 days of injury as this is the time to the Wallerian degeneration takes to reach the stylomastoid foramen. 6 When there is more than 90% of degeneration within 6 days or a degeneration higher than 95% within 14 days, a potentially unrecoverable SD V degree injury may have set, with a poor long‐term prognosis. Facial nerve exploration and decompression are usually recommended in this group of patients. 3 The timing for facial nerve decompression after the onset still controversial, varying from the first 3 days to after 3 weeks of palsy. 3 Delayed surgical decompression was generally considered ineffective as a treatment for VII paralysis due to course of Wallerian Degeneration total reach. 7 However, some authors like Jim Kim et al 8 demonstrated that patients previously treated with steroids since VII paralysis has set out and undergone surgery after 3 weeks have improved outcomes. 8 , 9 The majority of temporal bone trauma cases have other life‐threatening injuries that may delay early surgical decompression but when it is possible is preferable perform it within 2 weeks although the improved outcomes of delayed intervention. 8 , 9 The current patient had not been treated with corticosteroids, and on the 18th day, an ENoG was performed revealing bilateral absence of muscular response to stimulus undergoing bilateral surgery decompression at the same day. Then, he started a physical therapy in order to improve facial movements functions as it is described by LM Pereira et al 10 After one‐year follow‐up, patient presented a House & Brackman facial palsy grade II bilaterally. The House & Brackmann classification is an useful grade system (varying from I to IV degrees) to describe facial function objectively, conveniently, and quantitatively. It is useful in measuring recovery from facial nerve insults as a trauma and other conditions as Bell's palsy and Ramsay Hunt syndrome. The scale evaluates the symmetry and tone of face in the rest, the motion of muscle of forehead, nose, and mouth, the closure of eye and how much effort is required to do it, the presence of synkinesis, spasm, and contracture. It is described better in Table 2. 11
TABLE 2.
The House & Brackmann facial paralysis scale
| The house & Brackmann facial paralysis scale |
|---|
| I‐Normal |
| Normal facial functions in all areas |
| II‐Mild Dysfunction |
| At rest: Normal symmetry and tone. Motion: Normal movement of forehead. Preserved ability to close eye with minimal efforts and slight asymmetry. Ability to move the corners of mouth with efforts with slight asymmetry. No synkinesis, spasm, or facial contracture |
| III‐Moderate dysfunction |
| At rest: Normal symmetry and tone at rest. Motion: Slight to no movement of forehead. Ability to close eye with maximal effort with obvious asymmetry. Ability to move the corners of mouth with efforts with obvious asymmetry. Presence of synkinesis, spasm, and facial contracture |
| IV‐Moderately severe dysfunction |
| At rest: Normal symmetry and tone at rest. Motion: No movement of forehead, inability to close eye completely with maximal effort. Asymmetrical movements of corner of mouth with maximal effort. Presence of no important synkinesis, facial spasm, and contracture |
| V‐Severe dysfunction |
| At rest: Asymmetry of droop of corner of mouth and decrease or absent of nasal labial fold. Motion: no movement of forehead; incomplete closure of eyes and only slight movement with maximal effort. Slight movement of corner of mouth. Synkinesis, spasm, and facial contracture usually absent. |
| VI‐Total paralysis |
| Loss of tone; asymmetry; no motion; no synkinesis, contracture, or facial spasm |
When otic capsule damage occurs severe to profound sensorineural hearing loss (SNHL) install immediately. 3 Conductive hearing losses (CHL) are caused by hemotympanum, efusion in the middle ear, or disruption of the ossicular chain and are most common in otic capsule disruption. 3 The current patient developed hemotympanum as a cause of CHL and did not develop other causes of CHL and SNHL or CSF leak.
The current patient presented with bilateral conductive hearing loss worse on the left side. The great challenges one those facial nerve decompression surgery are the risk to cause sensorineural hearing loss and dizziness regarding the proximity of the nerve to the lateral canal. The surgery was done with no of those complications. On the left side was tried an ossicular chain reconstruction but the result was not satisfactory than it was performed a hearing aid with patient agreement. In one‐year follow‐up, after he had done physical therapy, he presented a House & Brackman facial palsy grade II bilaterally (Figures 5, 6, 7, and 8).
FIGURE 5.
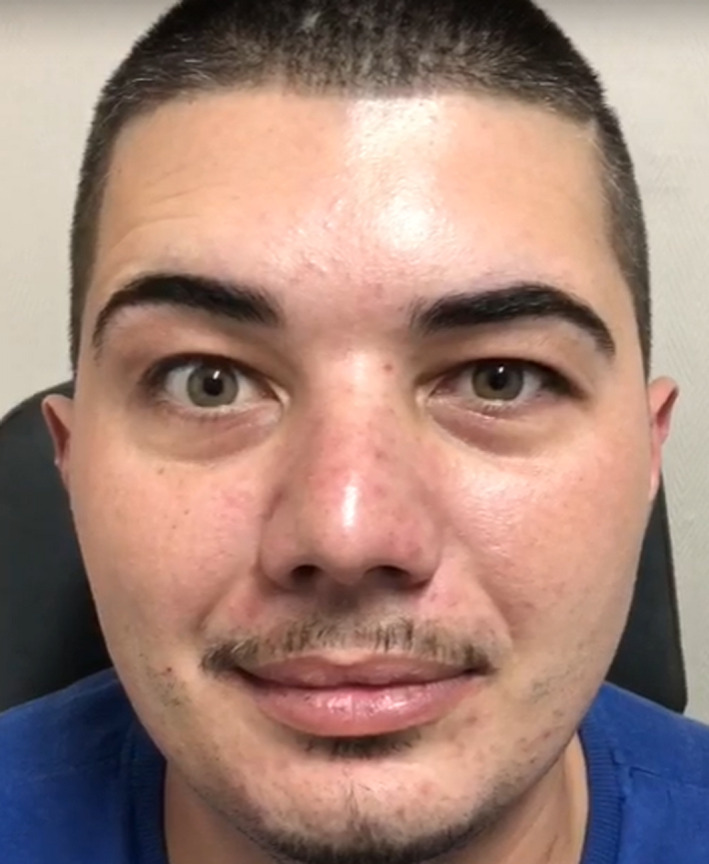
Two months postoperatively: Slight asymmetry of the forehead during movement. Normal symmetry and tone in the corners of mouth at rest
FIGURE 6.
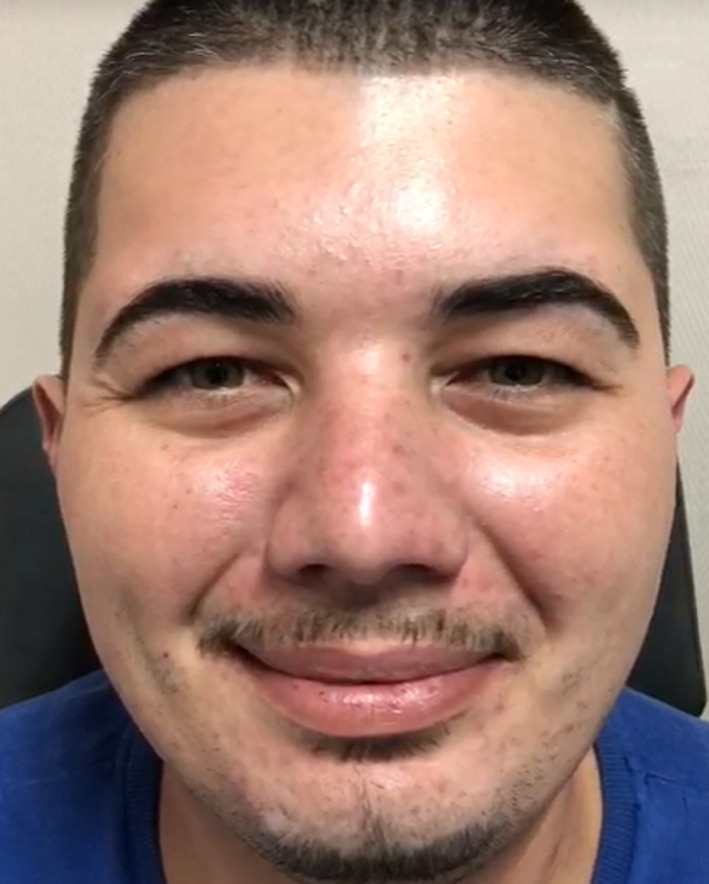
Two months postoperatively: Normal symmetry and tone at rest in the forehead. Slight asymmetry in the corners of mouth during movement
FIGURE 7.
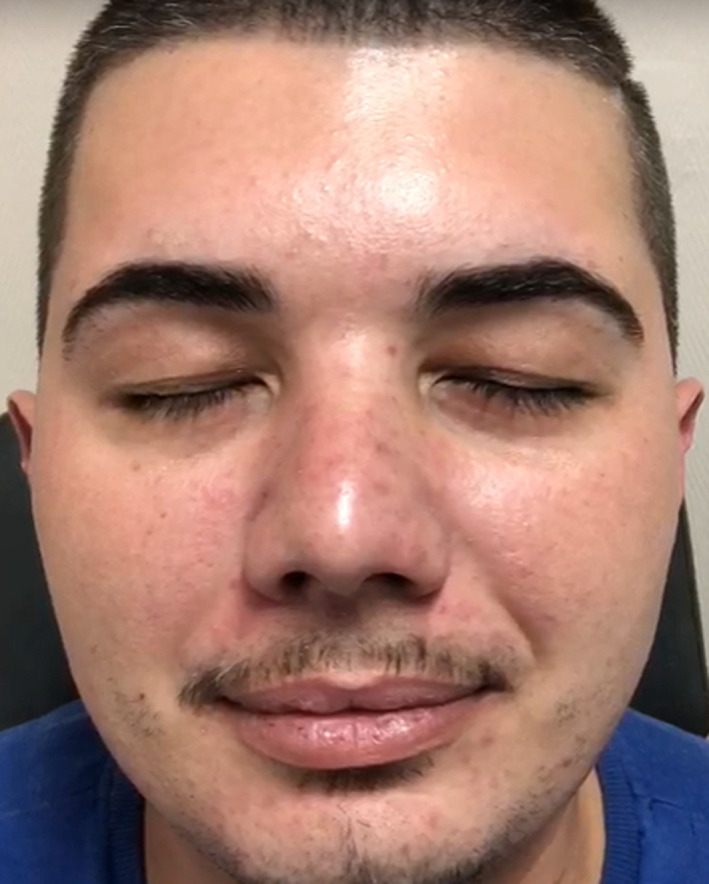
Two months postoperatively: Preserved ability to close both eyes with minimal effort
FIGURE 8.
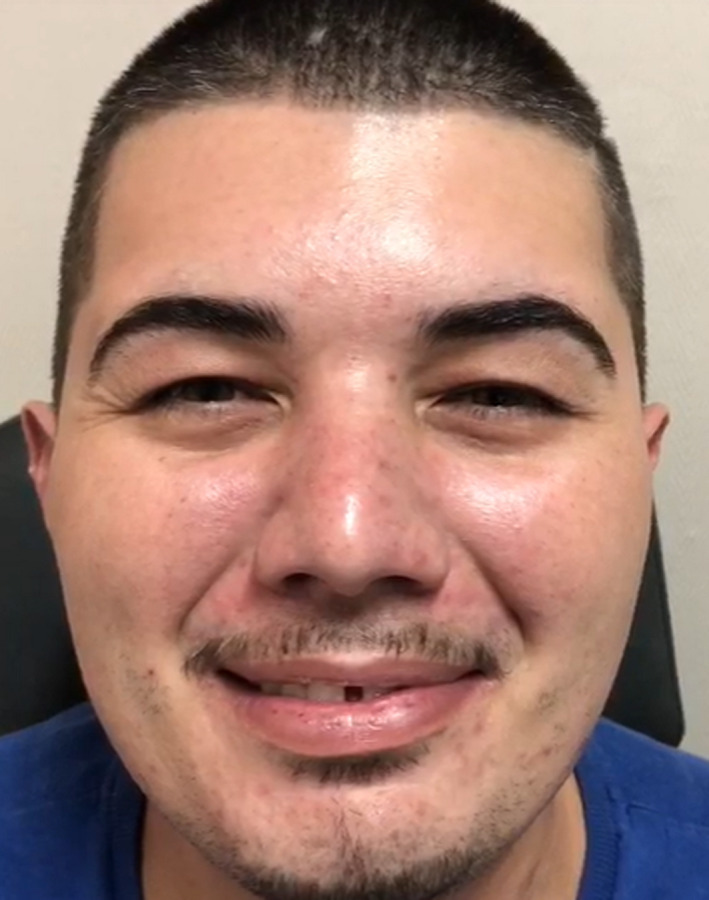
Two months postoperatively: Slight asymmetry in the corners of mouth with maximal effort
3. CONCLUSION
Peripheral facial palsy is more associated with transverse temporal bone fracture or, according to the most recent classification, fractures with otic capsule disruption. Medical management begins usually with corticosteroid to prevent inflammatory local reaction and reduce the Wallerian degeneration degree. There is no consensus regarding surgical treatment; however, the authors opinion is to evaluate the necessity of facial nerve decompression guided by the clinical characteristics and ENoG result. ENoG should be done after the third day (the authors suggest after the seventh day). If the degree of facial nerve degeneration is more than 90% within 6 days or a degeneration higher than 95% within 14 days facial nerve exploration and decompression are usually recommended.
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTIONS
NMA: involved in conception, organization, and manuscript writing. GCG: involved in manuscript writing. AMC: involved in manuscript review. VARdS: involved in surgical planning and in‐room surgeon, conception, organization, and review.
ETHICAL STATEMENT
The patient has signed an informed consent, and all data used were anonymized.
ACKNOWLEDGMENTS
No other person has contributed to the current manuscript. There are no financial or material supports.
Abrahão NM, Guimarães GC, Castilho AM, Silva VARD. Bilateral facial paralysis secondary to temporal bone trauma: A case report and literature review. Clin Case Rep. 2021;9:e04272. 10.1002/ccr3.4272
DATA AVAILABILITY STATEMENT
Research data are not shared (due to privacy and ethical restrictions).
REFERENCES
- 1. Pothiawala S, Lateef F. Bilateral facial nerve palsy: a diagnostic dilemma. Case Rep Emerg Med. 2012;2012:1‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Eliçora SŞ, Dinç AE, Bişkin S, Damar M, Bilgin E. Bilateral facial paralysis caused by bilateral temporal bone fracture: a case report and a literature review. Case Rep Otolaryngol. 2015;2015:1‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Diaz R, Cervenka B, Brodie H. Treatment of temporal bone fractures. J Neurol Surg Part B Skull Base. 2016;77(05):419‐429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Brodie HA, Thompson TC. Management of complications from 820 temporal bone fractures. Am J Otol. 1997;18(2):188‐197. [PubMed] [Google Scholar]
- 5. Exadaktylos AK, Sclabas GM, Nuyens M, et al. The clinical correlation of temporal bone fractures and spiral computed tomographic scan: a prospective and consecutive study at a level i trauma center. J Trauma Inj Infect Crit Care. 2003;55(4):704‐706. [DOI] [PubMed] [Google Scholar]
- 6. Lee D‐H. Clinical efficacy of electroneurography in acute facial paralysis. J Audiol Otol. 2016;20(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fisch U, Esslen E. Total intratemporal exposure of the facial nerve pathologic findings in Bell's palsy. Arch Otolaryngol. 1972;95:335‐341. [DOI] [PubMed] [Google Scholar]
- 8. Kim J, Moon IS, Lee W‐S. Effect of delayed decompression after early steroid treatment on facial function of patients with facial paralysis. Acta Otolaryngol (Stockh). 2010;130(1):179‐184. [DOI] [PubMed] [Google Scholar]
- 9. Siang PG, Ying XT, Dayang Suhana AM, Ing PT. Surgical outcomes of transmastoid facial nerve decompression: preliminary data from a Malaysian tertiary hospital from 2013–2018. Med J Malaysia. 2020;75(3):281‐285. [PubMed] [Google Scholar]
- 10. Pereira L, Obara K, Dias J, Menacho M, Lavado E, Cardoso J. Facial exercise therapy for facial palsy: systematic review and meta‐analysis. Clin Rehabil. 2011;25(7):649‐658. [DOI] [PubMed] [Google Scholar]
- 11. House JW. Facial nerve grading systems. Laryngoscope. 1983;93(8):1057‐1069. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Research data are not shared (due to privacy and ethical restrictions).


