Abstract
Background
Fiji, a Pacific Island nation of 884,887 (2017 census), has experienced a prolonged epidemiological transition. This study examines trends in mortality and life expectancy (LE) in Fiji by sex and ethnicity over 1996–2017, with comparisons to published estimates.
Methods
Trends in infant mortality rates (IMR), under-5 mortality (U5M), adult mortality (probability of dying), LE (at birth) and directly age-standardised death rates (DASRs) by sex and ethnicity, are calculated (with 95% confidence limits) using unit death records from the Fiji Ministry of Health and Medical Services. The LE gap between populations, or within populations over time, is examined using decomposition by age. Period trends are assessed for statistical significance using linear regression.
Results
Over 1996–98 to 2014–17: IMR and U5M for i-Taukei and Fijians of Indian descent declined; U5M decline for i-Taukei (24.6 to 20.1/1000 live births) was significant (p = 0.016). Mortality (15–59 years) for i-Taukei males was unchanged at 27% but declined for Indians 33 to 30% (p = 0.101). Mortality for i-Taukei females increased 22 to 24% (p = 0.011) but declined for Indians 20 to 18% (p = 0.240). DASRs 1996–2017 were lower for i-Taukei (9.3 to 8.2/1000 population) than Indian males (10.6 to 9.8/1000). DASRs declined for i-Taukei (both sexes, p < 0.05), and for Indians (both sexes, p > 0.05). Over 22 years, LE at birth increased by 1 year or less (p = 0.030 in male i-Taukei). In 2014–17, LE (years) for males was: i-Taukei 64.9, Indians 63.5; and females: i-Taukei 67.0 and Indians 68.2. Mortality changes in most 5-year age groups increased or decreased the LE gap less than 10 weeks over 22 years. Compared to international agency reports, 2014–17 empirical LE estimates (males 64.7, females 67.8) were lower, as was IMR.
Conclusions
Based on empirical data, LE in Fiji has minimally improved over 1996–2017, and is lower than some international agencies report. Adult mortality was higher in Indian than i-Taukei men, and higher in i-Taukei than Indian women. Exclusion of stillbirths resulted in IMRs lower than previously reported. Differing mortality trends in subgroups highlight the need to collect census and health data by ethnicity and sex, to monitor health outcomes and inform resource allocation.
Keywords: Infant mortality, Under-5 mortality, Life expectancy, Fiji, Trend analysis, Decomposition
Background
Comprehensive, timely measures of mortality and accurate assignment of causes of death are fundamental in understanding the health of a population and effectively allocating health resources [1]. Measures of mortality may be calculated directly from data collected and collated locally, with corrections for biases, or from modelling techniques [2]. Results are most accurate if based on complete local deaths and denominators from recently measured populations.
Fiji has experienced demographic and epidemiological transitions since the mid-twentieth century, with reductions in infectious diseases leading to mortality decline, increased life expectancy (LE) and population growth, followed by fertility reduction. Increased proportional mortality from cardiovascular and other non-communicable diseases (NCDs) in adults is considered to have contributed to the plateau in LE in Fiji since the mid-1980s [3, 4].
Fiji is the second most populous of the Pacific Island countries (PICs) in Oceania, with a population of 884,887 at the 2017 census, of which 81% resides on Viti Levu and 15% on Vanua Levu [5]. The proportion of the population aged > 65-years grew from 3 to 6% over 1996–2017 [5, 6]. The predominant ethnic groups in Fiji are: 62% i-Taukei (Melanesian) Fijians; and 31% Fijians of Indian descent (referred hereinafter as ‘Indians’); with 7% other Pacific Islanders, Asians, Europeans, and others [7].
Free, or low cost, public health care, funded through taxation, is provided by: three divisional (tertiary care), two specialist and 17 sub-divisional hospitals; 84 health centres (with a medical officer or nurse practitioner); and 98 nursing stations [8]. Government funding of health services in Fiji (2011) was amongst the lowest of PICs at 2.9–3.5% of gross domestic product [9]. Compared to the minimum World Health Organisation (WHO) standard (228 health workers/100,000 people), 9 of 15 provinces in Fiji were below target for nurses and none met the target for doctors in 2007 [10].
Cross-sectional studies have shown that Indians have a higher prevalence of hypertension [11] and type 2 diabetes mellitus (T2DM) at a lower body mass index (BMI) than i-Taukei [12]. Prevalence of obesity, and incidence and prevalence of T2DM [12, 13] increased over 1980–2011 in both sexes and major ethnicities (p < 0.05), with likely impact on premature mortality and LE [12]. Public health initiatives targeting NCDs have been implemented, following development of a National NCD Strategic Plan 2015–19 [14]. Accurate and timely mortality measures based on local empirical data are required to monitor the success of these initiatives.
The Fiji Births, Deaths and Marriages (BDM) Registration Act 1975 requires registration of every birth, and the completion of a Medical Certificate of Cause of Death (MCCD) by a medical or nurse practitioner or midwife, in accordance with the International Classification of Diseases (ICD) [15]. Every Notification of Birth (NoB) and MCCD is forwarded to the Data Analysis Management Unit (DAMU) of the MoHMS for collation. No fee is levied for timely registration of births or deaths, however the requirement for in-person attendance by a family member at the BDM office to complete the legal registration process may create a barrier to completion. DAMU birth and death records have been assessed as more complete than the civil register [16, 17].
Infant mortality rates (IMR), under-5 mortality (U5M) and adult mortality (15–59 years), as well as LE at birth, are widely reported epidemiological measures of population health. LE is included in the United Nations (UN) Human Development Index, [14] and is normally derived from age-specific death rates. Adult mortality is defined by the UN as the probability of dying between ages 15–60 years, [18] often considered as working ages, where mortality contributes to lost productivity. The causes of death are quite different between the two halves of the adult age range, and consequently examination of mortality in 15–34- and 35–59-year age ranges will better inform targeting of preventative health interventions. The gap, or lack thereof, in LE between populations, or over time within a population, is the sum of positive and negative contributions of age-specific mortality [19]. Decomposition of the LE gap can identify specific age groups or segments of the population as targets for mortality reduction interventions.
LE at birth, U5M and adult mortality from NCD’s at ages 30–69 years are included in the Healthy Island indicators adopted in The Pacific Island Countries and Areas - WHO Cooperation Strategy 2018–2022 [8]. When accurately measured, these indicators facilitate monitoring of progress towards Sustainable Development Goal (SDG) three: ensuring healthy lives and well-being at all ages. By 2030, SDG 3.2. is to reduce newborn mortality to ≤12/1000 live births and to reduce U5M to ≤25/1000 live births; and SDG 3.4 is to reduce by one third premature mortality from NCDs [20].
This study estimates age-specific all-cause mortality and LE trends by ethnicity and sex in Fiji over 1996–2017 to assess the extent to which the previously reported plateaux in LEs during 1985–2007 [3] has persisted, and compares these estimates with published data from other sources. Age-specific mortality rate contributions to LE are also assessed.
Methods
Study design
In this population-based study, mortality rates by age group, sex and ethnicity are calculated to estimate adult mortality and LE using the hypothetical cohort method [21]. Infant and < 5 years deaths, and births in the same period, are used for IMR and U5M [22].
Deaths
All deaths occurring in Fiji between January 1996 and December 2017 and reported to the Fiji MoHMS were analysed according to date of death (DoD) (including deaths recorded in 2018 occurring in 2017). De-identified unit records were extracted from the electronic recording systems maintained by the DAMU of MoHMS (Table 1), each record containing age at death or date of birth (DoB), DoD, cause of death, national health number (NHN), sex and ethnicity of the decedent. Whilst the tools used for recording details of deaths changed during 1996–2017, the process for reporting deaths did not. Electronic mortality records were maintained in a Microsoft Access database from 1996 to 2010, and in the mortality module of the Patient Information System (PATIS Plus) from 2012 onwards. The NHN is a unique identification number used to track and record any interaction of a person with the health system in Fiji, and can be used for confirmation of demographic information, such as age, sex and ethnicity during data entry from the MCCD into electronic systems.
Table 1.
Number of deaths by sex, summarised by age groups, per trienniab, i-Taukei and Indian, Fiji 1996–2017
| Age | Deaths Male Totala | Deaths Female Totala | ||||||||||||
| Period | 96–98 | 99–01 | 02–04 | 05–07 | 08–10 | 11–13 | 14–17b | 96–98 | 99–01 | 02–04 | 05–07 | 08–10 | 11–13 | 14–17b |
| < 1 | 509 | 436 | 500 | 591 | 471 | 501 | 734 | 438 | 369 | 425 | 502 | 352 | 434 | 498 |
| 1–4 | 171 | 201 | 154 | 160 | 246 | 172 | 189 | 140 | 173 | 119 | 124 | 202 | 120 | 153 |
| 5–14 | 207 | 238 | 188 | 178 | 150 | 139 | 175 | 136 | 187 | 162 | 118 | 105 | 99 | 142 |
| 15–34 | 747 | 819 | 788 | 787 | 681 | 778 | 967 | 494 | 577 | 601 | 518 | 528 | 498 | 707 |
| 35–59 | 2924 | 3359 | 3263 | 3581 | 3561 | 3788 | 5300 | 1920 | 1988 | 2182 | 2373 | 2572 | 2621 | 3800 |
| 60–74 | 2496 | 2948 | 3166 | 3309 | 3399 | 3813 | 5668 | 1848 | 2242 | 2479 | 2539 | 2957 | 3057 | 4463 |
| ≥75 | 1644 | 1891 | 1873 | 1795 | 1772 | 2011 | 2857 | 1588 | 1731 | 1834 | 1792 | 2037 | 2160 | 3372 |
| Unkc | 79 | 221 | 153 | 27 | 1 | 31 | 0 | 82 | 170 | 133 | 12 | 1 | 32 | 0 |
| Total | 8777 | 10,113 | 10,085 | 10,428 | 10,281 | 11,233 | 15,890 | 6646 | 7437 | 7935 | 7978 | 8754 | 9021 | 13,135 |
| Deaths i-Taukei Male | Deaths i-Taukei Female | |||||||||||||
| < 1 | 322 | 287 | 339 | 407 | 336 | 371 | 567 | 268 | 256 | 303 | 345 | 244 | 335 | 378 |
| 1–4 | 128 | 155 | 120 | 119 | 191 | 135 | 161 | 113 | 142 | 89 | 102 | 163 | 95 | 122 |
| 5–14 | 115 | 143 | 116 | 124 | 90 | 106 | 129 | 82 | 95 | 106 | 77 | 74 | 64 | 100 |
| 15–34 | 375 | 390 | 382 | 423 | 380 | 435 | 520 | 261 | 305 | 333 | 314 | 323 | 294 | 449 |
| 35–59 | 1258 | 1401 | 1465 | 1741 | 1737 | 1941 | 2863 | 998 | 1122 | 1233 | 1431 | 1539 | 1641 | 2444 |
| 60–74 | 1325 | 1600 | 1762 | 1818 | 1873 | 2089 | 3175 | 1029 | 1316 | 1467 | 1508 | 1680 | 1666 | 2529 |
| ≥75 | 887 | 1019 | 1056 | 1014 | 1030 | 1148 | 1691 | 920 | 1031 | 1126 | 1091 | 1223 | 1249 | 1933 |
| Unkc | 41 | 100 | 81 | 12 | 1 | 17 | 0 | 49 | 99 | 84 | 7 | 1 | 21 | 0 |
| Total | 4451 | 5095 | 5321 | 5658 | 5638 | 6242 | 9106 | 3720 | 4366 | 4741 | 4875 | 5247 | 5365 | 7955 |
| Deaths Indian Male | Deaths Indian Female | |||||||||||||
| < 1 | 167 | 130 | 142 | 165 | 119 | 105 | 136 | 156 | 102 | 109 | 139 | 95 | 88 | 104 |
| 1–4 | 30 | 41 | 28 | 34 | 37 | 28 | 21 | 26 | 23 | 23 | 18 | 33 | 21 | 24 |
| 5–14 | 83 | 80 | 58 | 51 | 56 | 25 | 41 | 48 | 79 | 47 | 37 | 29 | 28 | 35 |
| 15–34 | 332 | 379 | 366 | 320 | 246 | 294 | 378 | 215 | 253 | 246 | 176 | 179 | 175 | 233 |
| 35–59 | 1528 | 1830 | 1637 | 1681 | 1643 | 1676 | 2205 | 855 | 790 | 855 | 845 | 932 | 891 | 1191 |
| 60–74 | 1050 | 1226 | 1246 | 1346 | 1367 | 1550 | 2251 | 752 | 856 | 930 | 934 | 1185 | 1285 | 1769 |
| ≥75 | 656 | 762 | 716 | 680 | 638 | 738 | 989 | 592 | 608 | 612 | 621 | 708 | 824 | 1285 |
| Unkc | 33 | 105 | 63 | 15 | 0 | 12 | 0 | 28 | 62 | 48 | 3 | 0 | 9 | 0 |
| Total | 3879 | 4553 | 4256 | 4292 | 4106 | 4428 | 6021 | 2672 | 2773 | 2870 | 2773 | 3161 | 3321 | 4641 |
a Total includes i-Taukei, Indians, others. b2014–17 4-year data. c Unk: deaths with unknown age proportionately redistributed prior to analysis
During the 1990s a separate form was used for recording stillbirths, but its use was discontinued in 2000. A new MCCD format from 2009 introduced recording of DoB and added a checkbox to identify stillbirths. Up to 172 foetal deaths (ICD-10 P95) per year (0–2.5% of total deaths) were identified in the unit death records for 2000–17, with higher numbers found in the data extracted from PATIS Plus from 2012 to 17 (160–172 per year). These deaths, clearly identified as stillbirths (P95, DoB and DoD identical), were removed prior to all analyses.
Deaths with unknown age were proportionately redistributed. These comprised 2.2% of total deaths in 1999–2001 and 0.3–1.6% in other periods. Annual numbers of deaths in the MoHMS data compared with those published by Fiji Bureau of Statistics (FBoS) for 1996–2008, [17] and WHO for 1996–2012, [23] matched exactly for most years. MoHMS data differed for 4 years by 8–51 deaths/year, representing < 1% of deaths, but were higher than WHO data by 3.5% (203) in 2001 and 10% (601) in 2003. Differences are likely a result of supply of mortality data to agencies prior to complete enumeration by Fiji MoHMS, and/or inclusion of stillbirths in counts of infant deaths. During June–December 2018 an additional 348 deaths were recorded in the MoHMS database with a DoD between January–December 2017; mortality data from earlier years were essentially complete at the time of extraction in June 2018.
Deduplication
Records with the same death certificate number, DoD, DoB, cause of death, sex and ethnicity were considered duplicates and were removed. The highest number of duplicated records occurred in 2017; de-duplication reduced the deaths by 0.3%. Previous reviews of Fiji mortality concluded MoHMS death data as the most reliable source for mortality analysis from 1996, [14] and death registration, by sex and ethnicity, for 1996–2004 was assessed as essentially complete (≥95% excepting females 2002–04 at 85%), [3, 4, 17] using the Brass growth-balance method [24].
Populations and births
Population denominators are from Fiji Censuses. Populations by ethnicity (by 5-year age group and sex) were published by the FBoS following the 1996 [6] and 2007 Fiji Censuses [25]. The 2017 census population (884,887 compared to 837,271 at the 2007 census) was lower than projections from 2007 for 2017 (~ 910,000) [26]. Ethnicity data were not released following the 2017 census because of reservations concerning data quality [27]. Ethnicity projections published by FBoS in 2017 [7] were used to estimate the ethnic composition of the 2017 population; this projected an increase in i-Taukei, as a proportion of the total population, from 56.8 to 62.1%, and a decrease in Indians from 37.5 to 30.7% [7]. The proportion of each ethnic group in 2007 in each 5-year age group, by sex, was multiplied by the ratio of FBoS projected population proportions (%) (62.1/56.8 for i-Taukei and 30.7/37.5 for Indian) to estimate the populations by ethnicity for 2017. Annual populations for intercensal years, by sex and five-year age group, from 0 to 4 years to ≥75 years, were estimated by linear interpolation of Fiji populations from the 1996, [6] 2007 [25] and 2017 censuses [5].
Data on live births per year were available from the MoHMS for 1996–2017 by ethnicity, but not by sex. In 2012–17, 99.5% of births are reported to have occurred within health facilities, [16] supporting the reliability of birth statistics.
Analysis
To reduce variation from small event numbers and enumeration biases, live births, deaths, and populations over 1996–2013 were grouped by triennia, with the most recent period containing four-years (2014–17) to avoid the potential of stochastic variation from analysis of single-year data.
All-cause mortality was estimated as IMR and U5M; adult mortality, expressed as the probability (%) of dying over 15–34 years (young adult, 20q15), 35–59 years (mid-age adult, 25q35), 15–59 years (adult, 45q15) and 30–69 years (40q30), [8]; and LE at birth. There is some overlap of mortality measures, consistent with overlaps in the currently monitored parameters by international agencies, such as Global Burden of Disease (GBD), WHO and UN. Comparisons involving LE (hypothetical cohort method) are not affected by differing age structures of populations. All-age directly age-standardised mortality rates (DASRs) were calculated using the 2007 Fiji census population as the standard, in 5-year age groups (< 5 to ≥75 years).
IMR was calculated using deaths < 1-year divided by live births in the same period (1q0), and U5M (5q0) calculated from deaths < 5-years divided by live births in the same period [22]. For sex specific lifetables, mortality < 5 years was estimated using population denominators. Adult mortality was calculated from the sum of mortality rates (mx) in each 5-year age group (nx) over the broader age interval (cumulative rate), with the probability of dying in the specified age interval (cumulative risk) derived as:
Cumulative risk = 1 − e(cumulative rate) [28].
All mortality estimates, 95% confidence intervals (CIs) (normal approximation of the binomial) and CIs for LE (derived from the Chiang II method for estimating variance of the probability of dying) [21] were calculated using Microsoft Excel; the calculation tools, with explanatory notes, are publicly available [29].
LE differences between 1996 and 98 and 2014–17, and between ethnic groups by sex, were decomposed to examine the contribution of mortality by 5-year age groups to LE gaps, following Arriaga’s method, [20] using Excel spreadsheets adapted from those developed by Auger et al. [30]
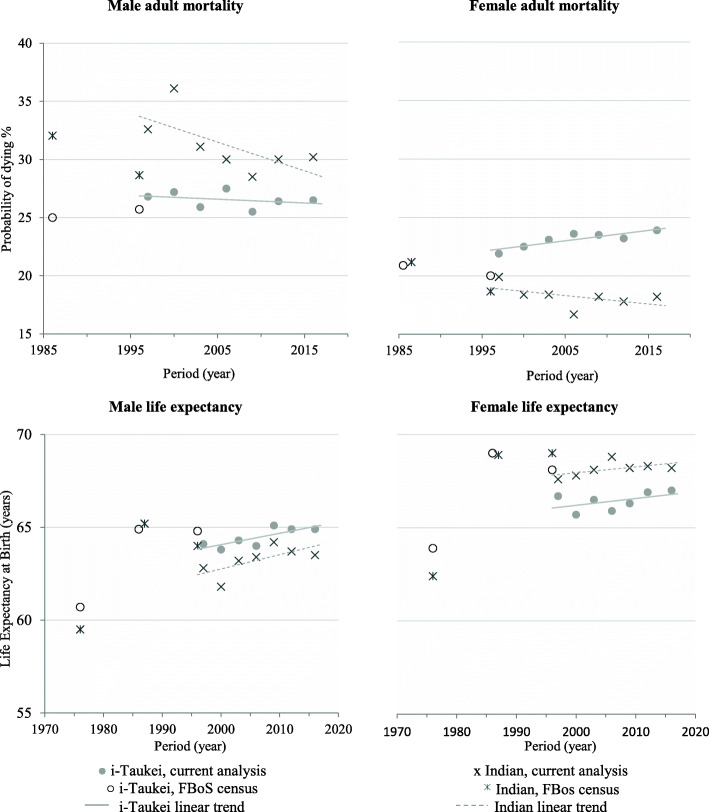
Linear regression was used to assess the statistical significance of period trends, by determining a p-value for trend for U5M, adult mortality, LE and DASR, using Proc Reg is SAS, Version9.4. Earlier estimates of adult mortality (probability of dying 15–59 years) and LE at birth, for both sexes and ethnicities, from indirect demographic methods from Fiji Censuses of 1976, 1986 and 1996, are displayed (Fig. 1) to show longer term trends.
Fig. 1.
Adult (15–59 years) risk of mortality and life expectancy, by ethnicity, Fiji 1975–2017. 1976, Census survivorship data used to impute model life tables [31]. 1986, Child and adult survival data used to impute logit model life tables [32]. 1996, Vital registration and census data used to impute model life tables (UN Far Eastern 2 parameter model) [6]. All other data from present analysis. FBoS: Fiji Bureau of Statistics
Comparisons
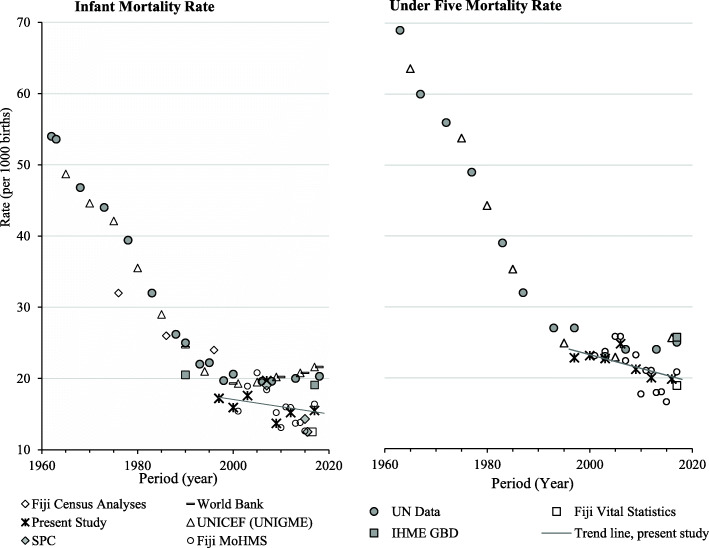
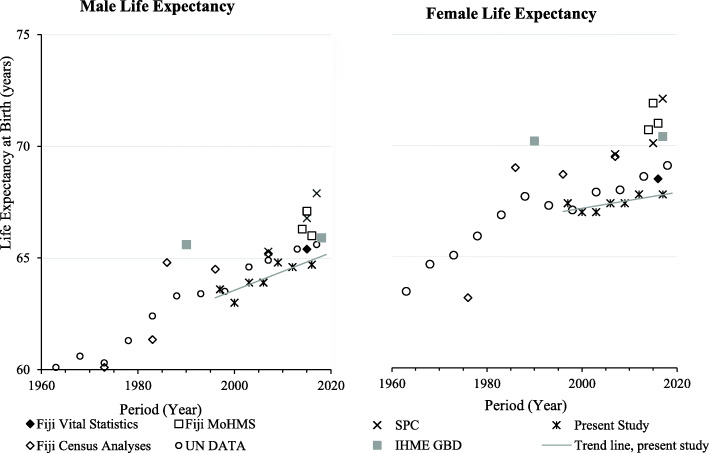
Published Fiji mortality estimates from diverse sources from 1963 to 2018 for IMR and U5M (Fig. 3), and LE by sex from 1960 to 2018 (Fig. 4) are displayed.
Fig. 3.
Published Infant Mortality Rates and Under 5 Mortality Rates for Fiji 1960–2018. Fiji Census Analysis [6, 31, 32]; World Bank [33]; UN Data [34]; Fiji Vital Statistics [16]; UNICEF (UNIGME) [35]; IHME GBD (Institute for Health Metrics and Evaluation) [36]; Fiji MoHMS [37, 38]; SPC (Pacific Community) [39].
Fig. 4.
Published estimates for life expectancy by sex, Fiji 1960–2018. Fiji Vital Statistics [16]; Fiji Census Analyses [6, 31, 32]; Fiji MoHMS [37, 38]; UN Data [34]; IHME GBD (Institute for Health Metrics and Evaluation) [36]; SPC (Pacific Community) [39].
Results
Infant and under 5 mortality (Table 2)
Table 2.
Infant mortality and under-five mortality rates, total, i-Taukei and Indian, Fiji 1996–2017
| Period | i-Taukei | Indian | Totalb | ||||||
|---|---|---|---|---|---|---|---|---|---|
| IMR | Births | IMR | 95% CI | Births | IMR | 95% CI | Births | IMR | 95% CI |
| 1996–1998 | 11,272 | 17.5 | 16.1–18.9 | 6059 | 17.8 | 15.8–19.7 | 18,349 | 17.2 | 16.1–18.3 |
| 1999–2001 | 11,353 | 16.2 | 14.8–17.5 | 5026 | 15.4 | 13.4–17.4 | 17,310 | 15.9 | 14.8–17.0 |
| 2002–2004 | 11,870 | 18.0 | 16.6–19.4 | 4750 | 17.6 | 15.4–19.8 | 17,542 | 17.6 | 16.4–18.7 |
| 2005–2007 | 12,651 | 19.8 | 18.4–21.2 | 4884 | 20.7 | 18.4–23.0 | 18,506 | 19.7 | 18.5–20.8 |
| 2008–2010 | 14,222 | 13.6 | 12.5–14.7 | 4840 | 14.7 | 12.8–16.7 | 19,962 | 13.7 | 12.8–14.7 |
| 2011–2013 | 15,247 | 15.5 | 14.4–16.7 | 4381 | 14.7 | 12.6–16.7 | 20,524 | 15.2 | 14.3–16.2 |
| 2014–2017a | 15,286 | 15.5 | 14.5–16.5 | 3757 | 16.0 | 14.0–18.0 | 19,896 | 15.5 | 14.6–16.3 |
| U5M | Births | U5M | 95% CI | Births | U5M | 95% CI | Births | U5M | 95% CI |
| 1996–1998 | 11,272 | 24.6 | 23.0–26.2 | 6059 | 20.8 | 18.8–22.9 | 18,349 | 22.8 | 21.6–24.1 |
| 1999–2001 | 11,353 | 24.9 | 23.2–26.6 | 5026 | 20.5 | 18.2–22.8 | 17,310 | 23.1 | 21.8–24.4 |
| 2002–2004 | 11,870 | 23.9 | 22.3–25.5 | 4750 | 21.2 | 18.8–23.6 | 17,542 | 22.7 | 21.5–24.0 |
| 2005–2007 | 12,651 | 25.6 | 24.0–27.2 | 4884 | 24.3 | 21.8–26.8 | 18,506 | 24.8 | 23.5–26.9 |
| 2008–2010 | 14,222 | 21.9 | 20.5–23.3 | 4840 | 19.6 | 17.3–21.8 | 19,962 | 21.2 | 20.1–22.4 |
| 2011–2013 | 15,247 | 20.6 | 19.3–21.9 | 4381 | 18.4 | 16.1–20.7 | 20,524 | 20.0 | 18.9–21.1 |
| 2014–2017a | 15,286 | 20.1 | 19.0–21.2 | 3757 | 19.0 | 16.8–21.1 | 19,896 | 19.8 | 18.8–20.8 |
| p trend U5M | 0.016↓ | 0.311 | 0.069 | ||||||
Deaths corrected for removal of stillbirths and duplicates. a2014–17 4 yr data. b Total include i-Taukei, Indians, others. Births: average per year. IMR infant mortality rate/1000 from deaths < 1 yr and live births, U5M under 5 yr mortality/1000 live births from deaths < 5 yrs. and live births. Bold: p < 0.05; Italics: p ≥ 0.05 to p < 0.06. Births by sex not available. CI confidence interval
An overall downward trend in IMR and U5M was observed over 1996–2017, however, IMR increased during 2002–07, and higher U5M was observed in 2005–07. The IMR stabilised during 2011–2017 at around 15/1000 live births annually for both major ethnicities. U5M was lower in Indians than i-Taukei, with a narrowing gap during 1996–2017. Sex-specific IMR and U5M were not calculated since live births by sex were not available from MoHMS.
Adult mortality (Table 3, Fig. 1)
Table 3.
Adult mortality, life expectancy, age standardised rates by age group, ethnicity, sex. Fiji 1996–2017
| Period | Male | Female | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| i-Taukei | Indian | Totalb | i-Taukei | Indian | Totalb | |||||||
| Young adult mortality 15–34 years: probability dying (%) and 95% CI | ||||||||||||
| 1996–98 | 3.6 | 3.3–4.0 | 3.6 | 3.2–3.9 | 3.6 | 3.3–3.8 | 2.6 | 2.3–3.0 | 2.4 | 2.1–2.8 | 2.5 | 2.3–2.7 |
| 1999–01 | 3.7 | 3.3–4.0 | 4.1 | 3.7–4.5 | 3.9 | 3.6–4.2 | 2.9 | 2.6–3.2 | 2.9 | 2.6–3.3 | 2.9 | 2.6–3.1 |
| 2002–04 | 3.3 | 3.0–3.6 | 4.0 | 3.6–4.4 | 3.6 | 3.3–3.8 | 3.0 | 2.7–3.3 | 2.9 | 2.6–3.3 | 2.9 | 2.7–3.1 |
| 2005–07 | 3.4 | 3.1–3.8 | 3.5 | 3.1–3.8 | 3.4 | 3.2–3.7 | 2.6 | 2.4–2.9 | 2.1 | 1.8–2.4 | 2.4 | 2.2–2.6 |
| 2008–10 | 3.0 | 2.7–3.3 | 2.8 | 2.4–3.1 | 3.0 | 2.8–3.2 | 2.6 | 2.4–2.9 | 2.3 | 1.9–2.6 | 2.5 | 2.3–2.7 |
| 2011–13 | 3.4 | 3.1–3.7 | 3.6 | 3.2–4.0 | 3.5 | 3.2–3.7 | 2.4 | 2.1–2.6 | 2.4 | 2.0–2.7 | 2.4 | 2.2–2.6 |
| 2014–17a | 3.0 | 2.8–3.3 | 3.7 | 3.4–4.1 | 3.3 | 3.1–3.5 | 2.6 | 2.4–2.9 | 2.5 | 2.2–2.9 | 2.5 | 2.3–2.7 |
| p trend | 0.040↓ | 0.470 | 0.134 | 0.237 | 0.481 | 0.270 | ||||||
| Mid age mortality 35–59 years: probability dying (%) and 95% CI | ||||||||||||
| 1996–98 | 24.0 | 22.8–25.2 | 30.1 | 28.8–31.4 | 26.7 | 25.8–27.5 | 19.8 | 18.7–20.9 | 17.9 | 16.8–19.0 | 18.5 | 17.8–19.3 |
| 1999–01 | 24.4 | 23.3–25.5 | 33.3 | 32.0–34.6 | 28.1 | 27.3–29.0 | 20.2 | 19.1–21.3 | 15.9 | 14.9–16.9 | 17.9 | 17.1–18.6 |
| 2002–04 | 23.4 | 22.3–24.5 | 28.2 | 27.0–29.4 | 25.5 | 24.7–26.2 | 20.8 | 19.7–21.8 | 16.0 | 15.0–17.0 | 18.3 | 17.6–19.0 |
| 2005–07 | 24.9 | 23.9–25.9 | 27.5 | 26.3–28.6 | 25.7 | 25.0–26.4 | 21.6 | 20.5–22.6 | 14.9 | 13.9–15.8 | 18.2 | 17.5–18.8 |
| 2008–10 | 23.1 | 22.2–24.1 | 26.5 | 25.3–27.6 | 24.2 | 23.5–24.9 | 21.4 | 20.5–22.4 | 16.4 | 15.4–17.3 | 18.7 | 18.1–19.4 |
| 2011–13 | 23.8 | 22.9–24.7 | 27.4 | 26.3–28.6 | 24.6 | 23.9–25.3 | 21.3 | 20.4–22.2 | 15.8 | 14.9–16.8 | 18.3 | 17.6–18.9 |
| 2014–17a | 24.2 | 23.4–24.9 | 27.5 | 26.5–28.4 | 24.5 | 23.9–25.1 | 21.8 | 21.1–22.6 | 16.0 | 15.2–16.9 | 18.7 | 18.2–19.3 |
| p trend | 0.830 | 0.086 | 0.025↓ | 0.006↑ | 0.304 | 0.259 | ||||||
| Adult mortality 15–59 years: probability dying (%) and 95% CI | ||||||||||||
| 1996–98 | 26.8 | 25.6–28.0 | 32.6 | 31.3–33.9 | 29.3 | 28.5–30.2 | 21.9 | 20.8–23.0 | 19.9 | 18.8–21.1 | 20.6 | 19.8–21.3 |
| 1999–01 | 27.2 | 26.0–28.3 | 36.1 | 34.8–37.3 | 31.0 | 30.1–31.8 | 22.5 | 21.5–23.6 | 18.4 | 17.3–19.4 | 20.2 | 19.5–20.9 |
| 2002–04 | 25.9 | 24.9–27.0 | 31.1 | 29.9–32.3 | 28.1 | 27.4–28.9 | 23.1 | 22.1–24.2 | 18.4 | 17.4–19.5 | 20.7 | 20.2–21.4 |
| 2005–07 | 27.5 | 26.5–28.5 | 30.0 | 28.8–31.1 | 28.3 | 27.5–29.0 | 23.6 | 22.6–24.6 | 16.7 | 15.7–17.6 | 20.2 | 19.5–20.8 |
| 2008–10 | 25.5 | 24.5–26.4 | 28.5 | 27.4–29.6 | 26.5 | 25.8–27.2 | 23.5 | 22.5–24.5 | 18.2 | 17.3–19.2 | 20.8 | 20.1–21.4 |
| 2011–13 | 26.4 | 25.5–27.3 | 30.0 | 28.9–31.2 | 27.2 | 26.5–27.9 | 23.2 | 22.2–24.1 | 17.8 | 16.8–18.8 | 20.2 | 19.6–20.8 |
| 2014–17a | 26.5 | 25.7–27.2 | 30.2 | 29.2–31.2 | 27.0 | 26.4–27.5 | 23.9 | 23.1–24.7 | 18.2 | 17.3–19.0 | 20.8 | 20.2–21.3 |
| p trend | 0.499 | 0.101 | 0.030↓ | 0.011↑ | 0.240 | 0.657 | ||||||
| Adult mortality 30–69 years: probability dying (%) and 95% CI | ||||||||||||
| 1996–98 | 50.9 | 49.2–52.4 | 59.8 | 58.0–61.4 | 54.4 | 53.2–55.5 | 42.1 | 40.5–43.7 | 41.3 | 39.4–43.1 | 41.1 | 39.9–42.2 |
| 1999–01 | 52.4 | 50.9–53.9 | 60.6 | 59.0–62.1 | 55.4 | 54.4–56.5 | 45.0 | 43.4–46.4 | 39.3 | 37.6–41.0 | 41.7 | 40.6–42.8 |
| 2002–04 | 50.3 | 48.9–51.7 | 55.4 | 53.8–56.9 | 52.0 | 51.0–53.0 | 44.8 | 43.4–46.2 | 37.4 | 35.8–39.0 | 40.8 | 39.3–42.4 |
| 2005–07 | 50.5 | 49.2–51.8 | 54.1 | 52.6–55.6 | 51.5 | 50.5–52.4 | 44.1 | 42.7–45.4 | 35.6 | 34.0–37.1 | 39.7 | 38.7–40.7 |
| 2008–10 | 47.9 | 46.6–49.2 | 53.0 | 51.5–64.5 | 49.4 | 48.4–50.3 | 43.2 | 41.9–44.5 | 40.2 | 38.6–41.6 | 40.9 | 40.0–41.9 |
| 2011–13 | 48.3 | 47.0–49.5 | 55.6 | 54.1–57.0 | 50.1 | 49.2–51.0 | 41.7 | 40.5–42.9 | 40.1 | 38.6–41.6 | 39.7 | 38.7–40.6 |
| 2014–17a | 49.4 | 48.4–50.4 | 57.6 | 56.3–58.8 | 51.0 | 50.2–51.7 | 42.4 | 41.4–43.4 | 39.9 | 38.6–41.2 | 39.9 | 39.1–40.7 |
| p trend | 0.062↓ | 0.268 | 0.029↓ | 0.340 | 0.970 | 0.061↓ | ||||||
| Life expectancy (LE) at birth: LE and 95% CI | ||||||||||||
| 1996–98 | 64.1 | 63.7–64.5 | 62.8 | 62.4–63.2 | 63.6 | 63.4–63.9 | 66.7 | 66.4–67.1 | 67.6 | 67.2–68.1 | 67.4 | 67.1–67.6 |
| 1999–01 | 63.8 | 63.4–64.1 | 61.8 | 61.5–62.2 | 63.0 | 62.8–63.3 | 65.9 | 65.5–66.2 | 68.0 | 67.6–68.4 | 67.0 | 66.7–67.2 |
| 2002–04 | 64.3 | 64.0–64.6 | 63.2 | 62.8–63.6 | 63.9 | 63.6–64.1 | 65.9 | 65.5–66.2 | 68.2 | 67.8–68.6 | 67.0 | 66.8–67.3 |
| 2005–07 | 64.0 | 63.7–64.4 | 63.4 | 63.0–63.8 | 63.9 | 63.7–64.2 | 66.0 | 65.7–66.4 | 68.9 | 68.5–69.3 | 67.4 | 67.1–67.6 |
| 2008–10 | 65.1 | 64.7–65.4 | 64.2 | 63.8–64.6 | 64.8 | 64.5–65.0 | 66.4 | 66.0–66.7 | 68.2 | 67.8–68.6 | 67.4 | 67.1–67.6 |
| 2011–13 | 64.9 | 64.6–65.2 | 63.7 | 63.3–64.1 | 64.6 | 64.4–64.8 | 66.9 | 66.6–67.2 | 68.3 | 67.9–68.6 | 67.8 | 67.5–68.0 |
| 2014–17a | 64.9 | 64.7–65.2 | 63.5 | 63.2–63.9 | 64.7 | 64.5–64.9 | 67.0 | 66.7–67.2 | 68.2 | 67.9–68.6 | 67.8 | 67.6–68.0 |
| p trend | 0.030↑ | 0.091 | 0.014↑ | 0.188 | 0.298 | 0.048↑ | ||||||
| Direct age standardised death rates (DASR): DASR and 95% CI | ||||||||||||
| 1996–98 | 9.27 | 9.01–9.54 | 10.6 | 10.3–11.0 | 9.75 | 9.55–9.95 | 7.29 | 7.06–7.52 | 6.76 | 6.51–7.02 | 6.89 | 6.73–7.05 |
| 1999–01 | 9.49 | 9.23–9.74 | 11.4 | 11.1–11.7 | 10.1 | 10.0–10.3 | 7.69 | 7.47–7.92 | 6.37 | 6.14–6.61 | 6.97 | 6.82–7.13 |
| 2002–04 | 8.95 | 8.72–9.19 | 9.81 | 9.5–10.1 | 9.21 | 9.04–9.39 | 7.61 | 7.40–7.82 | 6.07 | 5.85–6.29 | 6.82 | 6.67–6.96 |
| 2005–07 | 8.65 | 8.43–8.87 | 9.23 | 8.96–9.50 | 8.73 | 8.57–8.90 | 7.21 | 7.01–7.41 | 5.48 | 5.28–5.68 | 6.34 | 6.20–6.48 |
| 2008–10 | 7.94 | 7.74–8.15 | 8.69 | 8.42–8.95 | 8.12 | 7.96–8.27 | 7.09 | 6.90–7.28 | 6.03 | 5.82–6.24 | 6.48 | 6.34–6.61 |
| 2011–13 | 8.17 | 7.97–8.37 | 9.49 | 9.21–9.76 | 8.47 | 8.31–8.62 | 6.64 | 6.46–6.82 | 6.27 | 6.05–6.48 | 6.25 | 6.12–6.38 |
| 2014–17a | 8.23 | 8.06–8.40 | 9.79 | 9.55–10.0 | 8.50 | 8.37–8.63 | 6.72 | 6.57–6.87 | 6.50 | 6.32–6.69 | 6.35 | 6.25–6.46 |
| p trend | 0.010↓ | 0.143 | 0.017↓ | 0.021↓ | 0.718 | 0.011↓ | ||||||
a 2014–17 4-year data. b Total includes i-Taukei, Indians, others. Bold: p < 0.05; Italics: p ≥ 0.05 to p < 0.06. LE life expectancy at birth, CI confidence interval, DASR all age, direct age standardised death rate per 1000 population based on Fiji 2007 census by 5-year age groups, Probability dying (%) probability of dying in the specified age interval = cumulative risk from the cumulative rate (see Methods)
Adult mortality across all age groups and by major ethnicity was significantly higher for males than females (non-overlapping 95% CIs). In young adults (15–34 years), a downward linear trend was evident for i-Taukei males (p = 0.040) over 1996–2017. The probability of dying for females 15–34 years remained low (around 3%) over the study period, with no significant difference between or discernible trend for i-Taukei (p = 0.237) and Indians (p = 0.481). Mortality was significantly higher for Indian men than i-Taukei men aged 35–59, 15–59 and 30–69 years over the whole study period (non-overlapping 95% CI). Mortality was lower in women aged 35–59, 15–59 and 30–69 years for Indian than i-Taukei over the whole study period (non-overlapping 95% CI’s, excepting for some 30–69-year mortality).
Mid-age (35–59 years) male mortality remained unchanged for i-Taukei (p = 0.830) but declined slightly for Indians (p = 0.086) and declined for total males (p = 0.025). Mid-age female mortality increased for i-Taukei (p = 0.006) over 1996–2017 but was relatively unchanged for Indians (p = 0.304) and for total females (p = 0.259). Trends in the broader 15–59-years mortality for each ethnicity and sex are similar to those seen in 35–59 years mortality.
Direct age standardised death rates and life expectancy at birth (Table 3, Fig. 1)
DASRs decreased over 1996–2017 for both ethnicities and sexes, with trends statistically significant for the total population by sex (M: p = 0.017, F: p = 0.011) and for i-Taukei (M: p = 0.010, F: p = 0.021), but not for Indians.
Over 1996–2017, LE at birth increased in i-Taukei males (0.8 years, p = 0.030) and females (0.3 years, p = 0.188), and Indian males (0.7 years, p = 0.091) and females (0.5 years, p = 0.298). For the total population, LE increased 1.1 years in males (p = 0.014) and 0.4 years in females (p = 0.048) over 1996–2017.
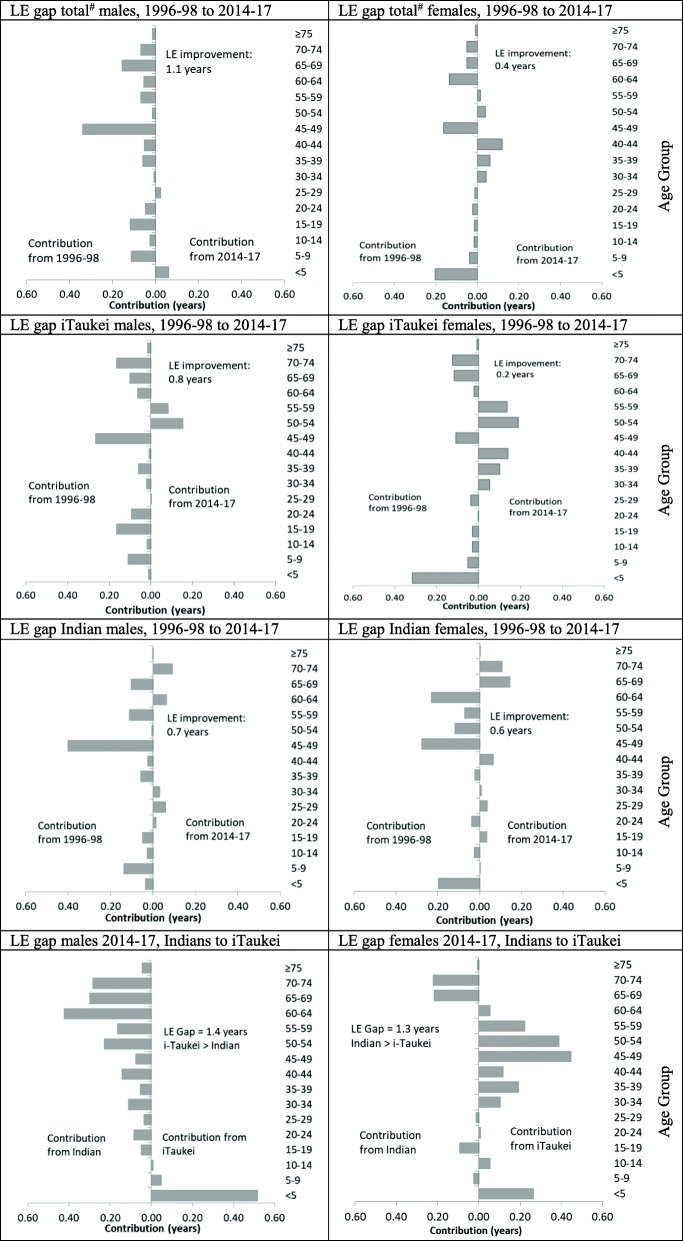
Decomposition of the life expectancy gap (Fig. 2)
Fig. 2.
Decomposition of differences in life expectancy between 1996 and 98 and 2014–17, and between populations in 2014–17. # Total includes i-Taukei, Indian, others. LE: Life expectancy. Grey bars show the estimated LE deficit contributed by age-specific mortality of each 5-year age group to the LE gap between populations. Each panel displays the decomposition of the LE gap between the first entity and the second entity named (by convention)
For males, all age groups except < 5 and 25–29 years contribute to a small increase in LE between 1996 and 98 and 2014–17. For females, the positive contributions to the LE improvement come from reduced mortality in most 5-year age groups but are offset by negative contributions in the 30–44- and 50–59-years age ranges, resulting in a smaller overall increase in LE compared to males. Most of the negative contribution to the overall LE change for females between 1996 and 98 and 2014–17 can be attributed to i-Taukei women in the 30–44- and 50–59-years age ranges, with mortality in the 65–74 years range for Indian women also negatively impacting the overall LE gain for women in Fiji.
For males in 2014–17, higher mortality in Indians in all age groups > 15 years contributes positively to the LE gap between i-Taukei and Indians, offset somewhat by the higher U5M in i-Taukei. For females in 2014–17, higher mortality in < 5- and 30–64-years in i-Taukei contributes positively to the LE gap but is partially offset by higher 65–74-years mortality in Indians, reducing the LE gap. Higher mortality in every 5-year-age group in the male population contributes to the LE gap between the sexes (not shown in Fig. 2).
Comparison with mortality trends from other sources (Figs. 3 and 4)
Published data from various sources show a plateau in IMR and U5M from 1995 (Fig. 3). The empirically based estimates in this study show lower levels than agency estimates from 2010, coinciding with exclusion of stillbirths from < 1-year deaths. MoHMS annual reports show even lower IMRs, possibly affected by late recording of deaths. Published agency trends of LE (at birth) by sex are higher than from empirical data in this study (Fig. 4). The Fiji MoHMS Annual Reports for 2014–16 [37, 38] estimate LE for males at 66.3–67.1 years; and for females 70.7–71.0. years. These estimates are higher, based on comparison of 95% CIs, than the LE estimates calculated in this study for 2014–17 (Table 3). The Fiji Vital Statistics Report estimates of LE at birth for 2015–17 (men 65.4; women 68.5) [16] are only slightly higher than LE estimates calculated here (2014–17). GBD estimates of LE increases in Fiji over 1995–2017 were limited to around 1 year, with estimates of male LE 65.9 and female LE 70.4 years in 2017, [40], compared to 64.6–64.9 and 67.6–68.0 years estimated in this study (Table 3). Analysis of LE in Fiji from FBoS is one of the few sources to report measures by ethnicity. Following the 2007 census, estimates of LE at birth for males was: 65.2 years for i-Taukei and 64.9 years for Indians; and for females: 67.4 years for i-Taukei and 72.2 years for Indians [17, 26]. The FBoS-reported LE’s show a similar pattern to that found in the current study, where average LE at birth increased progressively across the four groups (in order): Indian males, i-Taukei males, i-Taukei females and finally Indian females, who had the highest LE.
Discussion
Previous studies reported declines in IMR from 1976 to 1996–98, with larger declines in Indians compared with i-Taukei, resulting in similar IMRs for both ethnicities by 1996–98 [3]. In this study, the IMR decline continued over 1996–2017, with an interruption during 2002–07, and stability since 2011. Changes in foetal death-recording practices and electronic mortality recording systems may have contributed to inclusion of foetal deaths in mortality data and artefactually elevated IMRs reported elsewhere. During 2000–2008 the stillbirth form was not in use, with stillbirths identified on a new MCCD only after 2009. The IMR reported by the MoHMS in 2009 noted that infant deaths include some stillbirths, [37] also impacting reported trends in U5M.
IMRs published in MoHMS Annual Health Status Reports (HSR) from 2001 to 2015 [37] are generally lower than estimated in this analysis. Since live births are consistent with those in this study, differences are likely due to under-enumeration of infant deaths in the MoHMS HSR from late recording of deaths, after publication of annual reports. The lower values of IMR and U5M, used as baseline measures in setting targets for IMR and U5M by 2020 in the MoHMS National Strategic Plan 2016–20, [41] underestimate the reduction in infant deaths required. For 2006–08, the FBoS 2007 Census Analytical Report [26] provides aggregated deaths (18,984) identical to the present study prior to the exclusion of 54 stillbirths (ICD10 code P95). Higher IMRs reported by FBoS for 2006–08 can be attributed to inclusion of stillbirths.
For young adult men (15–34 years), the probability of death for i-Taukei was similar to Indians in 1996–98, but lower in i-Taukei by 2014–17 compared to Indians (p < 0.05), due to declines for i-Taukei (p < 0.05). For young adult women, the probability of death remained low, and similar for i-Taukei and Indians from 1996 to 98 to 2014–17, however decomposition of the LE gap highlights higher mortality at 30–34-years for i-Taukei offset by higher mortality at 15–19-years for Indians. The cause of death structure of these differences requires investigation. Trends in mid-age adult mortality over 1996–2017 differ by sex and ethnicity; reporting mortality only for the total population by sex, rather than by sex and ethnicity, obscures these divergences. Explanations for differing mortality trends by sex and ethnicity in the 35–59 age group may reflect risk factor prevalence trends [42].
Decomposition of LE gaps between 1996 and 98 and 2014–17 shows differing age contributions by sex and ethnicity. Decomposition of the LE gap by cause of death will further inform contributions to these LE gaps.
The LE plateau previously reported for both ethnicities and sexes in Fiji, based on analysis of death records to 2008 [3] has continued to 2017. For the total male population, LE increased more than in each ethnic group individually; the increase can be partially attributed to i-Taukei, with a higher LE, making up a larger proportion of the total male population in 2017 compared to 1996. The MoHMS Annual Health Status reports (2014 to 2016) do not describe the method for calculating LE [37]. However, the 2014 report includes an estimated population of 933,204, [37] based on projected average intercensal annual population increases of 1.6% [25] between 2007 and 2017, greater than the actual average annual growth rate of 0.6% [5]. The use of these higher population estimates for calculating mortality rates would partly account for the higher LE estimates than in the present analysis. Late registration of deaths is noted as a limitation in the Vital Statistics Report, [16] with 6992 deaths recorded for 2017, compared with 7403 deaths here, due to late death registrations. This demonstrates a source of considerable inaccuracy that can arise from premature use of death data which is under-registered.
The 2017 GBD study identified Fiji as one of 20 countries where male LE has increased by less than 10 years since 1950 [40]. While LE estimated in this study from empirical death data are lower than estimated by GBD, both sources show stagnation in LE over recent decades. GBD classifies Fiji as a middle Socio-Demographic Index (SDI) country, and in 2017 the average LE in middle SDI countries was 71.1 (males) and 77.4 (females), considerably higher than LE estimates for Fiji from both GBD and this empirical study. The increases in SDI in Fiji do not appear to have translated into parallel increases in LE.
The Mortality Transition in Fiji Report, published by FBoS following detailed analysis of the 2007 census, also reports stagnation in LE beginning in the 1980’s and continuing until 2007 [17]. This report suggests possible contributors to this outcome: economic factors, including unemployment and emigration of healthy, working age people following the instability of three political coups in 1987, 2000 and 2006, and an increase in “lifestyle disease” [17]. The MoHMS National Strategic Plan 2016–2020 targets significantly increasing the number of nurses, doctors and other health workers [41]. The increasing burden of health care needs created as populations age, with increasing levels of chronic disease, can be expected to further constrain the health care system’s ability to meet the health needs of the community, potentially contributing to increased morbidity and mortality.
According to the MoHMS National Strategic Plan 2016–2020, approximately 78% of all deaths and 40% of deaths < 60 years are due to NCDs [41]. The top three causes of mortality as reported by the MoHMS remain diseases of the circulatory system, endocrine and metabolic conditions (mostly diabetes), and neoplasms [37, 38]. Significant increases in the prevalence of high blood pressure in both sexes and both ethnicities occurred between 1980 and 2011 [11]. T2DM prevalence [12] and incidence [13] also increased in Fiji between 1980 and 2011. Obesity rates, using standard BMI cut-off points, are higher in i-Taukei than Indians, and higher in women than men, but T2DM prevalence is higher in Indians than i-Taukei [12]. Tobacco smoking in both sexes and ethnicities decreased over 1980–2011, with most of the reduction occurring before 2000 for i-Taukei men, after which prevalence formed a plateau; whilst for Indian men the decline continued until 2011 [43]. Mortality and LE trends from cardiovascular disease, T2DM and lung cancer are the result of cumulated exposure to risk factors over previous decades; and based on reported trends in risk factors the current plateau in LE is expected to continue.
This analysis utilises more complete primary data than previously employed for published estimates of mortality and LE in Fiji and uses 2017 Fiji census data as denominators, which enumerated a smaller population than previously projected. Exclusion of foetal deaths, inclusion of late reported infant and other deaths, and removal of duplicate records, allows calculation of IMR, as well as total mortality and LE, from more accurate primary data.
Limitations in the present analysis include lack of birth data by sex, missing age from some death records and lack of ethnicity data for the 2017 census. IMR and U5M were calculated by ethnicity but not by sex. Divergent trends in mortality in the < 5-year age group by sex are evident from deaths and census populations < 5-years, used in life tables. Decomposition analysis of LE gaps suggests that the improvements seen in U5M can be attributed to reductions in U5M for females, both i-Taukei and Indian, while little improvement is evident in U5M for males and comparison shows that higher U5M for i-Taukei, both male and female, contributes negatively to the LE gap between the ethnic groups. The results are also affected by an unusually high number of i-Taukei male infant deaths in 2014–17 for reasons that are not obvious. Births by sex should be routinely collated to allow calculation of IMR and U5M by sex as well as by ethnicity. Contributions of causes of death to these differences should be investigated. The small number of deaths with unknown age were redistributed proportionately prior to analysis, which is an approximation, and may not reflect that age is more likely to be missing in older descendants, and varies between years; however, is superior to some other reports [23] which appear to exclude incomplete records.
Populations by ethnicity were not published from the 2017 census. Between the 1996 and 2007 censuses the FBoS used the 1996 census as a base population and then continuously added births and immigration, and subtracted deaths and emigration, to maintain updated population statistics by ethnicity. These calculations were found to be in close agreement with the 2007 census population [26]. Populations by ethnicity for 2017 in this study were estimated by utilising ethnic-specific population projections published by the FBoS in 2017, [7] and the 2017 census data by sex and 5-year age groups. The ethnicity of the decedent was identified on the death certificate and may have been provided by the individual on hospital admission or by a family member. Differing sources of ethnicity between the death (numerator) and population (denominator) may bias results. Differences by ethnicity have been found to be an important explanatory variable in epidemiological, demographic and socio-economic analyses in Fiji, including in health-related studies [26].
Conclusions
IMRs reported in this study are higher than recent MoHMS estimates, and lower than those reported by international agencies, but are likely to be more accurate because of inclusion of more complete death records and exclusion of stillbirths. The reduction in young adult (15–34 years) male mortality can be attributed to reduction among i-Taukei, concealing the stagnation in mortality among Indians. The reduction in mid-age (35–59 years) mortality for men, due to reduction in Indians, conceals a stagnation in i-Taukei. Relatively unchanged mid-age mortality for women, conceals the mortality increase in i-Taukei women. Analysis following such stratifications improves understanding of the epidemiology of mortality in the whole population. The small increase in LE (at birth) in both sexes and ethnicities over 1996–2017 is significantly less than might be expected in a middle SDI country with LE’s in 1996–98 starting from a low base at 62–68 years. LE reported in this study is lower than reported by Fiji national agencies, and by several international agencies. Under-enumeration of deaths, inflated population estimates (projections from previous censuses), and incorrect modelling assumptions likely contribute to these discrepancies.
Acknowledgements
The authors would like to thank the Data Analysis Management Unit of the Fiji Ministry of Health and Medical Services for providing the unit record data analysed in this study. CD is supported through a Scientia PhD Scholarship from the University of New South Wales and through an Australian Government Research Training Program Scholarship.
Abbreviations
- BDM
Births, Deaths and Marriages
- BMI
Body mass index
- CI
Confidence interval
- DAMU
Data Analysis Management Unit
- DASR
Directly age-standardised death rate/s
- DoB
Date of birth
- DoD
Date of death
- FBoS
Fiji Bureau of Statistics
- GBD
Global Burden of Disease Study
- ICD
International Classification of Diseases
- IHME
Institute for Health Metrics and Evaluation
- IMR
Infant mortality rate
- LE
Life expectancy
- MCCD
Medical Certificate of Cause of Death
- MoHMS
Ministry of Health & Medical Services
- NCDs
Non- communicable diseases
- NoB
Notification of birth
- PICs
Pacific Island Countries
- SDG
Sustainable Development Goal
- SDI
Socio-Demographic Index
- SPC
Pacific Community
- T2DM
Type 2 diabetes mellitus
- U5M
Under-five mortality
- UN
United Nations
- UNICEF
United Nations Children’s Fund
- UNIGME
United Nations Inter-agency Group for Child Mortality Estimation
- WHO
World Health Organisation
Authors’ contributions
RT and SM conceived the study. CD and DN were responsible for acquiring the data. CD performed data cleaning, then statistical analysis with support from SM, RT and CL. CD wrote the first draft to which CL, RT and SM provided feedback during its development. CD, CL, ER, DN, SM and RT critically revised the manuscript and approved the final manuscript as submitted.
Funding
Not applicable.
Availability of data and materials
The mortality dataset analysed is not publicly available but may be requested by submission of a Data Request form to the Data Analysis Management Unit (DAMU) of the Ministry of Health and Medical Services, Fiji. The non-confidential information used in this publication, was compiled in accordance with the Information Act of 2018 of the Republic of Fiji but which DAMU has no authority to independently verify. The Data Analysis Management Unit of the Ministry of Health and Medical Services cannot and does not represent that the data was appropriate for this publication, or endorse or support any conclusions that may be drawn from the use of the data.
Declarations
Ethics approval and consent to participate
Approved by Fiji National Health Research and Ethics Review Committee (2018.72.NW) and by the University of New South Wales Human Research Ethics Committee (HC 180530)
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.AbouZahr C, de Savigny D, Mikkelsen L, Setel PW, Lozano R, Nichols E, Lopez AD, et al. Civil registration and vital statistics: progress in the data revolution for counting and accountability. Lancet. 2015;386(10001):1373–1385. doi: 10.1016/S0140-6736(15)60173-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. The utility of estimates for health monitoring and decision-making: global, regional and country perspectives: report of a technical meeting, WHO, Glion sur Montreux, Switzerland 24–25 June 2015. World Health Organization. https://extranet.who.int/iris/restricted/handle/10665/182163. Accessed 17 Jan 2020.
- 3.Taylor R, Carter K, Naidu S, Linhart C, Azim S, Rao C, Lopez AD. Divergent mortality trends by ethnicity in Fiji. Aust N Z J Public Health. 2013;37(6):509–515. doi: 10.1111/1753-6405.12116. [DOI] [PubMed] [Google Scholar]
- 4.Carter K, Cornelius M, Taylor R, Ali SS, Rao C, Lopez AD, Lewai V, Goundar R, Mowry C. Mortality trends in Fiji. Aust N Z J Public Health. 2011;35(5):412–420. doi: 10.1111/j.1753-6405.2011.00740.x. [DOI] [PubMed] [Google Scholar]
- 5.Fiji Bureau of Statistics . 2017 Population and Housing Census Release 1: Age, sex, geography and economic activity. Suva (FIJI): FBOS; 2018. [Google Scholar]
- 6.Fiji Bureau of Statistics . 1996 Fiji census of population and housing: analytical report, part 1 demographic characteristics. Suva (FJI): Government of the Republic of Fiji; 1998. [Google Scholar]
- 7.Fiji Bureau of Statistics – Key Statistics . 1.2A Census Population of Fiji by Ethnicity and 1.2B Estimated Population of Fiji by Ethnicity. Suva (FIJI): FBOS; 2017. [Google Scholar]
- 8.WHO Western Pacific . WHO Country Cooperation Strategy 2018-2022: Pacific Island countries and areas. Manila, Philippines: WHO Regional office for the Western Pacific; 2017. [Google Scholar]
- 9.World Health Organization. Regional Office for the Western Pacific . The Fiji Islands health system review. Manila, Philippines: WHO Regional Office for the Western Pacific; 2011. [Google Scholar]
- 10.Wiseman V, Lagarde M, Batura N, Lin S, Irava W, Roberts G. Measuring inequalities in the distribution of the Fiji Health Workforce. Int J Equity Health. 2017;16(1):115. doi: 10.1186/s12939-017-0575-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Linhart C, Tukana I, Lin S, Taylor R, Morrell S, Vatucawaqa P, Magliano D, Zimmet P. Continued increases in hypertension over three decades in Fiji, and the influence of obesity. J Hypertension. 2016;34(3):402–409. doi: 10.1097/HJH.0000000000000807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lin S, Tukana I, Linhart C, Morrell S, Taylor R, Vatucawaqa P, Magliano DJ, Zimmet P. Diabetes and obesity trends in Fiji over 30 years. J Diabetes. 2016;8(4):533–543. doi: 10.1111/1753-0407.12326. [DOI] [PubMed] [Google Scholar]
- 13.Morrell S, Lin S, Tukana I, Linhart C, Taylor R, Vatucawaqa P, Magliano DJ, Zimmet P. Diabetes incidence and projections from prevalence surveys in Fiji. Popul Health Metrics. 2016;14(1):45. doi: 10.1186/s12963-016-0114-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ministry of Health and Medical Services (MoHMS) 2014. Non-communicable diseases strategic plan 2015-2019. Accessed 26 Mar 2019. http://www.health.gov.fj/wp-content/uploads/2014/05/Final-NCD-Strategic-Plan-2015-2019.pdf
- 15.Government of Fiji. Births, Deaths and Marriages Registration Act, Act No. 7 of 1975. Office of the Attorney-General, Suva, Fiji. https://www.laws.gov.fj/Acts/DisplayAct/914#. Accessed 23 June 2018.
- 16.Fiji Bureau of Statistics . Republic of Fiji Vital Statistics Report 2012-2017. Suva, Fiji: Government of the Republic of Fiji and the Pacific Community (SPC); 2019. [Google Scholar]
- 17.Bakker ML. Fiji Bureau of Statistics. The Mortality Transition in Fiji: 2007 Fiji Census of Population and Housing. FIBOS: Suva (FIJI); 2014. [Google Scholar]
- 18.United Nations. Department of Economic and Social Affairs, Population Division . World Mortality 2017: Data Booklet. New York: United Nations; 2017. [Google Scholar]
- 19.Arriaga EE. Measuring and explaining the change in life expectancies. Demography. 1984;21(1):83–96. doi: 10.2307/2061029. [DOI] [PubMed] [Google Scholar]
- 20.United Nations, Sustainable Development Goals; 3. Good Health and Well-being. Accessed 15 Jan 2021. https://www.un.org/sustainabledevelopment/health/.
- 21.Chiang CL. The Life Table and its Applications. Malabar (Florida): Robert E Krieger Publishing Company; 1984. [Google Scholar]
- 22.Webb P, Bain C, Page A. Essential epidemiology: an introduction for students and health professionals. 3. UK: Cambridge University Press; 2017. [Google Scholar]
- 23.World Health Organisation 2018 . WHO mortality database. 2018. [Google Scholar]
- 24.Brass W. Methods for estimating fertility and mortality from limited and defective data. Carolina Population Centre: Chapel Hill; 1975. [Google Scholar]
- 25.Fiji Bureau of Statistics . General Tables: Population by Age and Sex and Marital Status by Province of Enumeration Fiji. Suva, Fiji: Fiji Bureau of Statistics; 2007. [Google Scholar]
- 26.Fiji Bureau of Statistics . 2007 Fiji census of population and housing: analytical report. Suva, Fiji: Government of the Republic of Fiji; 2012. [Google Scholar]
- 27.Waqavonovono, E. Census 2017, Statement on Ethnicity. Suva, Fiji: Fiji Bureau of Statistics (FBOS). Accessed 26 Mar 2018. https://www.statsfiji.gov.fj/index.php/census-2017/census.
- 28.Boyle P, Parkin DM. Statistical methods for registries. In: Jensen OM, Parkin DM, MacLennan R, Muir CS, Skeet RG, editors. Cancer Registration: Principles and Methods. Lyon, France: IARC Scientific Publication No 95; 1991. pp. 147–150. [PubMed] [Google Scholar]
- 29.School of Public Health and Community Medicine (SPHCM), NCD Downloads. University of New South Wales (UNSW), Sydney, NSW 2052, Australia. 2015. Accessed 21 Dec 2018. https://sphcm.med.unsw.edu.au/centres-units/international-ncd-research-group/downloads?qt-ncd_downloads_tabs=1#qt-ncd_downloads_tabs
- 30.Auger N, Feuillet P, Martel S, Lo E, Barry AD, Harper S. Mortality inequality in populations with equal life expectancy: Arriaga's decomposition method in SAS, Stata, and Excel. Ann Epidemiol. 2014;24(8):575–80.e1. doi: 10.1016/j.annepidem.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 31.Zwart F. Report on the Census of the Population 1976, Volume II: demographic characteristics. Parliamentary paper no 43. Suva (FJI): Parliament of Fiji; 1979. [Google Scholar]
- 32.Fiji Islands Bureau of Statistics . Report on Fiji Population Census 1986. Analytical Report on the demographic, social and economic characteristics of the population. Suva (FJI): Bureau of Statistics; 1989. [Google Scholar]
- 33.World Bank . Country profile Fiji. 2018. [Google Scholar]
- 34.United Nations. Department of Economic and Social Affairs, Population Division . World Population Prospects 2019, Online Edition. 2019. [Google Scholar]
- 35.UN Inter-agency Group for Child Mortality Estimation (UNIGME) 2018, Country Data and estimates, Fiji. Accessed 3 Apr 2019. https://childmortality.org/data.
- 36.Institute for Health Metrics and Evaluation (IHME) Country Profile 2017: Fiji. Seattle, WA: IHME, University of Washington, 2018. Accessed 19 Dec 2018. http://www.healthdata.org/fiji
- 37.Ministry of Health and Medical Services; Archive of Annual Health Status Reports 2005 to 2015. Accessed 17 Apr 2019. http://www.health.gov.fj/site-archives/
- 38.Ministry of Health and Medical Services (MoHMS). Health Status Report 2016. Accessed 26 Mar 2019. http://www.health.gov.fj/wp-content/uploads/2018/03/Health-Status-Report-2016.pdf
- 39.The Pacific Community (SPC), Statistics for Development Division, Pocket Statistical Summary 2013, 2018, 2020. Accessed 22 Jan 2021. https://sdd.spc.int/topic/life-expectancy-mortality-and-causes-death.
- 40.Dicker D, Nguyen G, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, Abbastabar H, Abd-Allah F, Abdela J, Abdelalim A, Abdel-Rahman O, Abdi A, Abdollahpour I, Abdulkader RS, Abdurahman AA, Abebe HT, Abebe M, Abebe Z, Abebo TA, Aboyans V, Abraha HN, Abrham AR, Abu-Raddad LJ, Abu-Rmeileh NME, Accrombessi MMK, Acharya P, Adebayo OM, Adedeji IA, Adedoyin RA, Adekanmbi V, Adetokunboh OO, Adhena BM, Adhikari TB, Adib MG, Adou AK, Adsuar JC, Afarideh M, Afshin A, Agarwal G, Aggarwal R, Aghayan SA, Agrawal S, Agrawal A, Ahmadi M, Ahmadi A, Ahmadieh H, Ahmed MLC, Ahmed S, Ahmed MB, Aichour AN, Aichour I, Aichour MTE, Akanda AS, Akbari ME, Akibu M, Akinyemi RO, Akinyemiju T, Akseer N, Alahdab F, al-Aly Z, Alam K, Alebel A, Aleman AV, Alene KA, al-Eyadhy A, Ali R, Alijanzadeh M, Alizadeh-Navaei R, Aljunid SM, Alkerwi A', Alla F, Allebeck P, Allen CA, Alonso J, al-Raddadi RM, Alsharif U, Altirkawi K, Alvis-Guzman N, Amare AT, Amini E, Ammar W, Amoako YA, Anber NH, Andrei CL, Androudi S, Animut MD, Anjomshoa M, Anlay DZ, Ansari H, Ansariadi A, Ansha MG, Antonio CAT, Appiah SCY, Aremu O, Areri HA, Ärnlöv J, Arora M, Artaman A, Aryal KK, Asadi-Lari M, Asayesh H, Asfaw ET, Asgedom SW, Assadi R, Ataro Z, Atey TMM, Athari SS, Atique S, Atre SR, Atteraya MS, Attia EF, Ausloos M, Avila-Burgos L, Avokpaho EFGA, Awasthi A, Awuah B, Ayala Quintanilla BP, Ayele HT, Ayele Y, Ayer R, Ayuk TB, Azzopardi PS, Azzopardi-Muscat N, Badali H, Badawi A, Balakrishnan K, Bali AG, Banach M, Banstola A, Barac A, Barboza MA, Barquera S, Barrero LH, Basaleem H, Bassat Q, Basu A, Basu S, Baune BT, Bazargan-Hejazi S, Bedi N, Beghi E, Behzadifar M, Behzadifar M, Béjot Y, Bekele BB, Belachew AB, Belay AG, Belay E, Belay SA, Belay YA, Bell ML, Bello AK, Bennett DA, Bensenor IM, Berhane A, Berman AE, Bernabe E, Bernstein RS, Bertolacci GJ, Beuran M, Beyranvand T, Bhala N, Bhatia E, Bhatt S, Bhattarai S, Bhaumik S, Bhutta ZA, Biadgo B, Bijani A, Bikbov B, Bililign N, Bin Sayeed MS, Birlik SM, Birungi C, Bisanzio D, Biswas T, Bjørge T, Bleyer A, Basara BB, Bose D, Bosetti C, Boufous S, Bourne R, Brady OJ, Bragazzi NL, Brant LC, Brazinova A, Breitborde NJK, Brenner H, Britton G, Brugha T, Burke KE, Busse R, Butt ZA, Cahuana-Hurtado L, Callender CSKH, Campos-Nonato IR, Campuzano Rincon JC, Cano J, Car M, Cárdenas R, Carreras G, Carrero JJ, Carter A, Carvalho F, Castañeda-Orjuela CA, Castillo Rivas J, Castro F, Catalá-López F, Çavlin A, Cerin E, Chaiah Y, Champs AP, Chang HY, Chang JC, Chattopadhyay A, Chaturvedi P, Chen W, Chiang PPC, Chimed-Ochir O, Chin KL, Chisumpa VH, Chitheer A, Choi JYJ, Christensen H, Christopher DJ, Chung SC, Cicuttini FM, Ciobanu LG, Cirillo M, Claro RM, Cohen AJ, Collado-Mateo D, Constantin MM, Conti S, Cooper C, Cooper LT, Cortesi PA, Cortinovis M, Cousin E, Criqui MH, Cromwell EA, Crowe CS, Crump JA, Cucu A, Cunningham M, Daba AK, Dachew BA, Dadi AF, Dandona L, Dandona R, Dang AK, Dargan PI, Daryani A, Das SK, Das Gupta R, das Neves J, Dasa TT, Dash AP, Weaver ND, Davitoiu DV, Davletov K, Dayama A, Courten B, de la Hoz FP, de leo D, de Neve JW, Degefa MG, Degenhardt L, Degfie TT, Deiparine S, Dellavalle RP, Demoz GT, Demtsu BB, Denova-Gutiérrez E, Deribe K, Dervenis N, Des Jarlais DC, Dessie GA, Dey S, Dharmaratne SD, Dhimal M, Ding EL, Djalalinia S, Doku DT, Dolan KA, Donnelly CA, Dorsey ER, Douwes-Schultz D, Doyle KE, Drake TM, Driscoll TR, Dubey M, Dubljanin E, Duken EE, Duncan BB, Duraes AR, Ebrahimi H, Ebrahimpour S, Edessa D, Edvardsson D, Eggen AE, el Bcheraoui C, el Sayed Zaki M, Elfaramawi M, el-Khatib Z, Ellingsen CL, Elyazar IRF, Enayati A, Endries AYY, Er B, Ermakov SP, Eshrati B, Eskandarieh S, Esmaeili R, Esteghamati A, Esteghamati S, Fakhar M, Fakhim H, Farag T, Faramarzi M, Fareed M, Farhadi F, Farid TA, Farinha CSS, Farioli A, Faro A, Farvid MS, Farzadfar F, Farzaei MH, Fazeli MS, Feigin VL, Feigl AB, Feizy F, Fentahun N, Fereshtehnejad SM, Fernandes E, Fernandes JC, Feyissa GT, Fijabi DO, Filip I, Finegold S, Fischer F, Flor LS, Foigt NA, Ford JA, Foreman KJ, Fornari C, Frank TD, Franklin RC, Fukumoto T, Fuller JE, Fullman N, Fürst T, Furtado JM, Futran ND, Galan A, Gallus S, Gambashidze K, Gamkrelidze A, Gankpe FG, Garcia-Basteiro AL, Garcia-Gordillo MA, Gebre T, Gebre AK, Gebregergs GB, Gebrehiwot TT, Gebremedhin AT, Gelano TF, Gelaw YA, Geleijnse JM, Genova-Maleras R, Gessner BD, Getachew S, Gething PW, Gezae KE, Ghadami MR, Ghadimi R, Ghasemi Falavarjani K, Ghasemi-Kasman M, Ghiasvand H, Ghimire M, Ghoshal AG, Gill PS, Gill TK, Gillum RF, Giussani G, Goenka S, Goli S, Gomez RS, Gomez-Cabrera MC, Gómez-Dantés H, Gona PN, Goodridge A, Gopalani SV, Goto A, Goulart AC, Goulart BNG, Grada A, Grosso G, Gugnani HC, Guimaraes ALS, Guo Y, Gupta PC, Gupta R, Gupta R, Gupta T, Gyawali B, Haagsma JA, Hachinski V, Hafezi-Nejad N, Hagos TB, Hailegiyorgis TT, Hailu GB, Haj-Mirzaian A, Haj-Mirzaian A, Hamadeh RR, Hamidi S, Handal AJ, Hankey GJ, Harb HL, Harikrishnan S, Haririan H, Haro JM, Hasan M, Hassankhani H, Hassen HY, Havmoeller R, Hay RJ, Hay SI, He Y, Hedayatizadeh-Omran A, Hegazy MI, Heibati B, Heidari M, Hendrie D, Henok A, Henry NJ, Heredia-Pi I, Herteliu C, Heydarpour F, Heydarpour P, Heydarpour S, Hibstu DT, Hoek HW, Hole MK, Homaie Rad E, Hoogar P, Horino M, Hosgood HD, Hosseini SM, Hosseinzadeh M, Hostiuc S, Hostiuc M, Hotez PJ, Hoy DG, Hsairi M, Htet AS, Hu G, Huang JJ, Husseini A, Hussen MM, Hutfless S, Iburg KM, Igumbor EU, Ikeda CT, Ilesanmi OS, Iqbal U, Irvani SSN, Isehunwa OO, Islam SMS, Islami F, Jahangiry L, Jahanmehr N, Jain R, Jain SK, Jakovljevic M, James SL, Javanbakht M, Jayaraman S, Jayatilleke AU, Jee SH, Jeemon P, Jha RP, Jha V, Ji JS, Johnson SC, Jonas JB, Joshi A, Jozwiak JJ, Jungari SB, Jürisson M, K M, Kabir Z, Kadel R, Kahsay A, Kahssay M, Kalani R, Kapil U, Karami M, Karami Matin B, Karch A, Karema C, Karimi N, Karimi SM, Karimi-Sari H, Kasaeian A, Kassa GM, Kassa TD, Kassa ZY, Kassebaum NJ, Katibeh M, Katikireddi SV, Kaul A, Kawakami N, Kazemeini H, Kazemi Z, Karyani AK, K C P, Kebede S, Keiyoro PN, Kemp GR, Kengne AP, Keren A, Kereselidze M, Khader YS, Khafaie MA, Khajavi A, Khalid N, Khalil IA, Khan EA, Khan G, Khan MS, Khan MA, Khang YH, Khanna T, Khater MM, Khatony A, Khazaie H, Khoja AT, Khosravi A, Khosravi MH, Khubchandani J, Kiadaliri AA, Kibret GDD, Kim CI, Kim D, Kim JY, Kim YE, Kimokoti RW, Kinfu Y, Kinra S, Kisa A, Kissimova-Skarbek K, Kissoon N, Kivimäki M, Kleber ME, Knibbs LD, Knudsen AKS, Kochhar S, Kokubo Y, Kolola T, Kopec JA, Kosek MN, Kosen S, Koul PA, Koyanagi A, Kravchenko MA, Krishan K, Krishnaswami S, Kuate Defo B, Kucuk Bicer B, Kudom AA, Kuipers EJ, Kulikoff XR, Kumar GA, Kumar M, Kumar P, Kumsa FA, Kutz MJ, Lad SD, Lafranconi A, Lal DK, Lalloo R, Lam H, Lami FH, Lan Q, Langan SM, Lansingh VC, Lansky S, Larson HJ, Laryea DO, Lassi ZS, Latifi A, Lavados PM, Laxmaiah A, Lazarus JV, Lebedev G, Lee PH, Leigh J, Leshargie CT, Leta S, Levi M, Li S, Li Y, Li X, Liang J, Liang X, Liben ML, Lim LL, Lim SS, Limenih MA, Linn S, Liu S, Liu Y, Lodha R, Logroscino G, Lonsdale C, Lorch SA, Lorkowski S, Lotufo PA, Lozano R, Lucas TCD, Lunevicius R, Lyons RA, Ma S, Mabika C, Macarayan ERK, Mackay MT, Maddison ER, Maddison R, Madotto F, Magdy Abd el Razek H, Magdy Abd el Razek M, Maghavani DP, Majdan M, Majdzadeh R, Majeed A, Malekzadeh R, Malik MA, Malta DC, Mamun AA, Manamo WA, Manda AL, Mansournia MA, Mantovani LG, Mapoma CC, Marami D, Maravilla JC, Marcenes W, Marina S, Martinez-Raga J, Martins SCO, Martins-Melo FR, März W, Marzan MB, Mashamba-Thompson TP, Masiye F, Massenburg BB, Maulik PK, Mazidi M, McGrath JJ, McKee M, Mehata S, Mehendale SM, Mehndiratta MM, Mehrotra R, Mehta KM, Mehta V, Mekonen T, Mekonnen TC, Meles HG, Meles KG, Melese A, Melku M, Memiah PTN, Memish ZA, Mendoza W, Mengistu DT, Mengistu G, Mensah GA, Mereta ST, Meretoja A, Meretoja TJ, Mestrovic T, Mezgebe HB, Miangotar Y, Miazgowski B, Miazgowski T, Miller TR, Mini GK, Mirica A, Mirrakhimov EM, Misganaw AT, Moazen B, Moges NA, Mohammad KA, Mohammadi M, Mohammadifard N, Mohammadi-Khanaposhtani M, Mohammadnia-Afrouzi M, Mohammed S, Mohammed MA, Mohan V, Mokdad AH, Molokhia M, Monasta L, Moradi G, Moradi M, Moradi-Lakeh M, Moradinazar M, Moraga P, Morawska L, Moreno Velásquez I, Morgado-da-Costa J, Morrison SD, Mosapour A, Moschos MM, Mousavi SM, Muche AA, Muchie KF, Mueller UO, Mukhopadhyay S, Mullany EC, Muller K, Murhekar M, Murphy TB, Murthy GVS, Murthy S, Musa J, Musa KI, Mustafa G, Muthupandian S, Nachega JB, Nagel G, Naghavi M, Naheed A, Nahvijou A, Naik G, Nair S, Najafi F, Nangia V, Nansseu JR, Nascimento BR, Nawaz H, Ncama BP, Neamati N, Negoi I, Negoi RI, Neupane S, Newton CRJ, Ngalesoni FN, Ngunjiri JW, Nguyen HT, Nguyen HT, Nguyen LH, Nguyen M, Nguyen TH, Ningrum DNA, Nirayo YL, Nisar MI, Nixon MR, Nolutshungu N, Nomura S, Norheim OF, Noroozi M, Norrving B, Noubiap JJ, Nouri HR, Nourollahpour Shiadeh M, Nowroozi MR, Nsoesie EO, Nyasulu PS, Ofori-Asenso R, Ogah OS, Ogbo FA, Oh IH, Okoro A, Oladimeji O, Olagunju AT, Olagunju TO, Olivares PR, Olusanya BO, Olusanya JO, Ong SK, Opio JN, Oren E, Ortiz JR, Ortiz A, Ota E, Otstavnov SS, Øverland S, Owolabi MO, Oyekale AS, P A M, Pacella R, Pakhale S, Pakhare AP, Pana A, Panda BK, Panda-Jonas S, Pandey AR, Pandian JD, Parisi A, Park EK, Parry CDH, Parsian H, Patel S, Patle A, Patten SB, Patton GC, Paudel D, Pearce N, Peprah EK, Pereira A, Pereira DM, Perez KM, Perico N, Pervaiz A, Pesudovs K, Petri WA, Petzold M, Phillips MR, Pigott DM, Pillay JD, Pirsaheb M, Pishgar F, Plass D, Polinder S, Pond CD, Popova S, Postma MJ, Pourmalek F, Pourshams A, Poustchi H, Prabhakaran D, Prakash V, Prakash S, Prasad N, Qorbani M, Quistberg DA, Radfar A, Rafay A, Rafiei A, Rahim F, Rahimi K, Rahimi-Movaghar A, Rahimi-Movaghar V, Rahman M, Rahman MHU, Rahman MA, Rahman S, Rai RK, Rajati F, Rajsic S, Raju SB, Ram U, Ranabhat CL, Ranjan P, Ranta A, Rasella D, Rawaf DL, Rawaf S, Ray SE, Razo-García C, Rego MAS, Rehm J, Reiner RC, Reinig N, Reis C, Remuzzi G, Renzaho AMN, Resnikoff S, Rezaei S, Rezaeian S, Rezai MS, Riahi SM, Ribeiro ALP, Riojas H, Rios-Blancas MJ, Roba KT, Robinson SR, Roever L, Ronfani L, Roshandel G, Roshchin DO, Rostami A, Rothenbacher D, Rubagotti E, Ruhago GM, Saadat S, Sabde YD, Sachdev PS, Saddik B, Sadeghi E, Moghaddam SS, Safari H, Safari Y, Safari-Faramani R, Safdarian M, Safi S, Safiri S, Sagar R, Sahebkar A, Sahraian MA, Sajadi HS, Salahshoor MR, Salam N, Salama JS, Salamati P, Saldanha RF, Salimi Y, Salimzadeh H, Salz I, Sambala EZ, Samy AM, Sanabria J, Sanchez-Niño MD, Santos IS, Santos JV, Santric Milicevic MM, Sao Jose BP, Sardana M, Sarker AR, Sarrafzadegan N, Sartorius B, Sarvi S, Sathian B, Satpathy M, Savic M, Sawant AR, Sawhney M, Saxena S, Sayyah M, Scaria V, Schaeffner E, Schelonka K, Schmidt MI, Schneider IJC, Schöttker B, Schutte AE, Schwebel DC, Schwendicke F, Scott JG, Sekerija M, Sepanlou SG, Serván-Mori E, Shabaninejad H, Shackelford KA, Shafieesabet A, Shaheen AA, Shaikh MA, Shakir RA, Shams-Beyranvand M, Shamsi MB, Shamsizadeh M, Sharafi H, Sharafi K, Sharif M, Sharif-Alhoseini M, Sharma M, Sharma J, Sharma R, She J, Sheikh A, Sheth KN, Shi P, Shibuya K, Shifa GT, Shiferaw MS, Shigematsu M, Shiri R, Shirkoohi R, Shiue I, Shokraneh F, Shrime MG, Shukla SR, Si S, Siabani S, Siddiqi TJ, Sigfusdottir ID, Sigurvinsdottir R, Silpakit N, Silva DAS, Silva JP, Silveira DGA, Singam NSV, Singh JA, Singh V, Sinha AP, Sinha DN, Sitas F, Skirbekk V, Sliwa K, Soares Filho AM, Sobaih BH, Sobhani S, Soofi M, Soriano JB, Soyiri IN, Sposato LA, Sreeramareddy CT, Srinivasan V, Srivastava RK, Starodubov VI, Stathopoulou V, Steel N, Stein DJ, Steiner C, Stewart LG, Stokes MA, Sudaryanto A, Sufiyan M'B, Sulo G, Sunguya BF, Sur PJ, Sutradhar I, Sykes BL, Sylaja PN, Sylte DO, Szoeke CEI, Tabarés-Seisdedos R, Tabuchi T, Tadakamadla SK, Takahashi K, Tandon N, Tassew AA, Tassew SG, Tavakkoli M, Taveira N, Tawye NY, Tehrani-Banihashemi A, Tekalign TG, Tekle MG, Temesgen H, Temsah MH, Temsah O, Terkawi AS, Teshale MY, Tessema B, Teweldemedhin M, Thakur JS, Thankappan KR, Thirunavukkarasu S, Thomas LA, Thomas N, Thrift AG, Tilahun B, To QG, Tobe-Gai R, Tonelli M, Topor-Madry R, Topouzis F, Torre AE, Tortajada-Girbés M, Tovani-Palone MR, Towbin JA, Tran BX, Tran KB, Tripathi S, Tripathy SP, Truelsen TC, Truong NT, Tsadik AG, Tsilimparis N, Tudor Car L, Tuzcu EM, Tyrovolas S, Ukwaja KN, Ullah I, Usman MS, Uthman OA, Uzun SB, Vaduganathan M, Vaezi A, Vaidya G, Valdez PR, Varavikova E, Varughese S, Vasankari TJ, Vasconcelos AMN, Venketasubramanian N, Vidavalur R, Villafaina S, Violante FS, Vladimirov SK, Vlassov V, Vollset SE, Vos T, Vosoughi K, Vujcic IS, Wagner GR, Wagnew FWS, Waheed Y, Wang Y, Wang YP, Wassie MM, Weiderpass E, Weintraub RG, Weiss DJ, Weiss J, Weldegebreal F, Weldegwergs KG, Werdecker A, Westerman R, Whiteford HA, Widecka J, Widecka K, Wijeratne T, Winkler AS, Wiysonge CS, Wolfe CDA, Wondemagegn SA, Wu S, Wyper GMA, Xu G, Yadav R, Yakob B, Yamada T, Yan LL, Yano Y, Yaseri M, Yasin YJ, Ye P, Yearwood JA, Yentür GK, Yeshaneh A, Yimer EM, Yip P, Yisma E, Yonemoto N, Yoon SJ, York HW, Yotebieng M, Younis MZ, Yousefifard M, Yu C, Zachariah G, Zadnik V, Zafar S, Zaidi Z, Zaman SB, Zamani M, Zare Z, Zeeb H, Zeleke MM, Zenebe ZM, Zerfu TA, Zhang K, Zhang X, Zhou M, Zhu J, Zodpey S, Zucker I, Zuhlke LJJ, Lopez AD, Gakidou E, Murray CJL. Global, regional, and national age-sex-specific mortality and life expectancy, 1950–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392(10159):1684–1735. doi: 10.1016/S0140-6736(18)31891-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ministry of Health and Medical Services (MoHMS) National Strategic Plan 2016–2020: Executive version. 2015. [Google Scholar]
- 42.Taylor R, Lin S, Linhart C, Morrell S. Overview of trends in cardiovascular and diabetes risk factors in Fiji. Ann Hum Biol. 2018;45(3):188–201. doi: 10.1080/03014460.2018.1465122. [DOI] [PubMed] [Google Scholar]
- 43.Linhart C, Tukana I, Lin S, Taylor R, Morrell S, Vatucawaqa P, Magliano D, Zimmet P. Declines and Plateaux in smoking prevalence over three decades in Fiji. Nicotine Tob Res. 2017;19(11):1315–1321. doi: 10.1093/ntr/ntw292. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The mortality dataset analysed is not publicly available but may be requested by submission of a Data Request form to the Data Analysis Management Unit (DAMU) of the Ministry of Health and Medical Services, Fiji. The non-confidential information used in this publication, was compiled in accordance with the Information Act of 2018 of the Republic of Fiji but which DAMU has no authority to independently verify. The Data Analysis Management Unit of the Ministry of Health and Medical Services cannot and does not represent that the data was appropriate for this publication, or endorse or support any conclusions that may be drawn from the use of the data.