Abstract
Background
Inflammatory bowel disease (IBD), including Crohn’s disease and ulcerative colitis, is a chronic, complex and unpredictable disease affecting an increasing number of patients worldwide from a young age. Inflammatory bowel disease is associated with multiple comorbidities and complications, requiring ongoing preventative, acute and chronic care. The purpose of this article is to review the literature on outpatient care models used to treat adults with IBD and to gain insight on how to improve quality of care and reduce costs.
Methods
A comprehensive review of recent literature on PubMed, Scopus and Google Scholar databases about care models used to treat IBD was performed. Key terms included ‘inflammatory bowel disease’, ‘organizational models’, ‘patient care team’ and ‘quality improvement’.
Results
Studies showed that an integrated care model decreases hospital admissions, IBD-related surgeries and comorbidities of IBD, ultimately decreasing direct and indirect costs of IBD compared with a more traditional patient-physician model. A gastroenterologist-led multidisciplinary team (MDT) involving comprehensive care by IBD nurses, a surgeon, psychologist, dietician, pharmacist, and other members as needed is recommended.
Conclusions
A holistic approach to IBD care delivered by a MDT with structured monitoring, active follow-up, patient education and prompt access to care improves outcomes for IBD patients. More research is needed on the cost-effectiveness of integrated care models to demonstrate long-term value and secure funding for implementation. Future research should compare integrated models of care and assess patient and physician satisfaction in these models of delivering IBD care.
Keywords: Ambulatory care, Inflammatory bowel disease, Integrated care models
Impact of Inflammatory Bowel Disease
Inflammatory bowel disease (IBD), including Crohn’s disease and ulcerative colitis (UC), is a group of chronic, relapsing and remitting immune-mediated conditions that cause inflammation and ulceration along the gastrointestinal tract. Inflammatory bowel disease affects a large number of the population worldwide, including approximately one in 150 Canadians (1). The average age of onset coincides with an important age of social, educational and career development, with the majority of individuals being diagnosed before the age of 30 (1). The etiology of IBD is multifactorial and still largely unknown, and there is currently no cure for these illnesses (1, 2).
Inflammatory bowel disease is associated with often debilitating comorbidities and can have a profound impact on both physical and mental health, greatly decreasing quality of life for those affected. Common symptoms of IBD include abdominal pain, bloating, frequent and urgent diarrhea, constipation, bloody stools, fatigue and weight loss. Complications of Crohn’s disease may include anal fissures, abscesses and fistulas, stricturing of the bowel with partial obstruction and in severe cases, complete bowel obstruction and perforation (3, 4). Persons with IBD affecting the colon are also at higher risk of developing colorectal cancer than the general population (1, 3). Although IBD primarily affects the gastrointestinal tract, due to chronic inflammation, IBD is also associated with multiple extraintestinal manifestations affecting the skin, joints, bones, eyes, liver and blood system (1, 3, 4). Additionally, psychiatric comorbidities such as anxiety and depression are common in patients with IBD (5).
Due to the complexity and unpredictability of IBD and its potential complications, maintenance therapy, ongoing monitoring and acute intervention are required at multiple levels of the health care system by a variety of health care providers (1, 3). Without coordinated care, structured follow-up and access to appropriate care in a timely fashion, IBD care is often episodic and reactive, with some patients only receiving care with an acute flare-up of the disease or when severe complications arise. This often results in patients requiring hospitalization and surgical intervention, rendering the treatment costly both directly and indirectly (6).
In Canada, where rates of IBD are among the highest in the world, the medical cost was estimated to total $2.8 billion CAD dollars in 2012, which equates to $11,900 per person affected (1). Direct medical costs, including medication, hospitalizations and physician visits, accounted for $1.2 billion. Indirect costs amounted to $1.6 billion, mainly through long-term work loss (1). The lifetime medical care cost of a patient with IBD can be comparable to a patient with other major chronic conditions such as diabetes mellitus (3).
Integrated Approach to IBD Management
Integrated models of care have been implemented worldwide with the goal of providing more comprehensive and holistic care to patients with chronic diseases (7). An integrated approach brings together a variety of health care services for patients to improve access to care, quality of care, patient satisfaction and health outcomes (1, 5). Randomized controlled trials have demonstrated a positive impact of an integrated model of care for patients with psychiatric illnesses and hepatitis C (8, 9). Exposure to an integrated model of care also improved care and decreased hospitalizations for elderly patients (7).
The complexity, cost, patient impact and the long duration of the disease that leads to an increasing burden in elderly patients make IBD a good candidate for management through an integrated model of care. Implementing an effective integrated care model with targeted resources for meeting the acute and chronic needs of patients with IBD is essential to improve overall health and quality of life and to decrease health care costs (1, 5–7). The purpose of this article is to review the literature on current outpatient care models for adults with IBD to gain an understanding of strategies and recommendations to optimize IBD care and decrease costs.
METHODS
A review of the literature pertaining to inflammatory bowel disease (IBD) care models published between 2008 and 2018 was performed in the online PubMed database. Key terms used to search the database included ‘inflammatory bowel disease’, ‘organizational models’, ‘patient care team’, ‘patient care planning’ and ‘quality improvement’. The filters used for inclusion were English language, human species, adult population (19+ years), peer-reviewed and free full-text articles. Articles were first screened by title or abstract and were included or excluded based on perceived relevance of the article to the core objectives of the literature review. Prospective and retrospective cohort studies, surveys and review articles were included. Studies pertaining to specific medical treatments of IBD, pediatric populations, primary care settings and inpatient groups were excluded. Additional articles were obtained by review of the reference sections in core articles retrieved in the literature search, with the same inclusion and exclusion criteria applied. Further information and data were obtained from a chapter in Cecil Essentials medical textbook and prominent IBD organization websites, such as Crohn’s and Colitis Canada, Crohn’s and Colitis UK, and the Canadian Digestive Health Foundation.
RESULTS
Article Selection
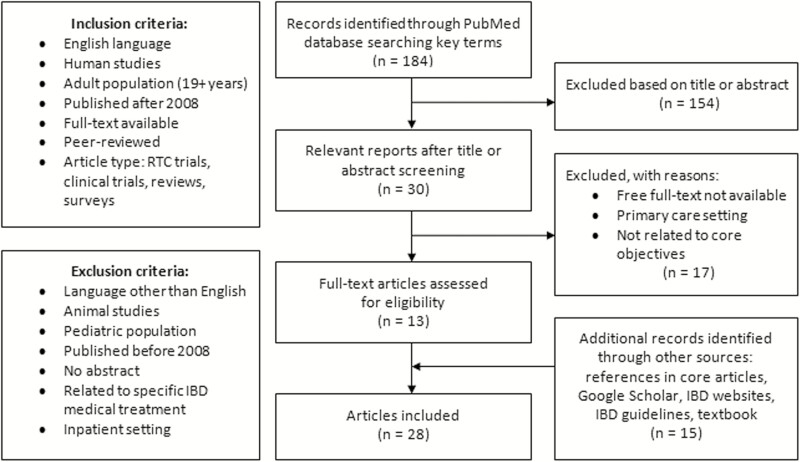
The initial search in the PubMed database using the key terms and inclusion filters described in the Methods section produced a total of 184 articles. After screening articles by title and abstract only, a total of 30 articles remained to be assessed. From the 30 articles, those not available in free full-text, those pertaining to primary care settings and those determined not to be related to the core objectives of the literature review were excluded, leaving a total of 13 articles appropriate to be included in the literature review (Supplemental Table 1). Prospective and retrospective cohort studies, international surveys and systematic review articles were used. An additional 15 articles obtained through other resources were also used in this literature review (Supplemental Table 2) (see Figure 1).
Figure 1.
Selection process with inclusion and exclusion criteria for the 24 resources included in the literature review.
Integrated Care Models Involving Multidisciplinary Teams
An integrated care model involves a multidisciplinary team (MDT), which consists of a team of health care professionals from different specialties working together to deliver comprehensive care to patients (Table 1). Experts in IBD support recommend an integrated care approach for the most effective management of IBD (1–3, 5, 6, 8), and the literature suggests that IBD care delivered by a gastroenterologist-led MDT is more effective (1–3, 5, 10) than the traditional patient-specialist model (Table 2). The patient-specialist model is a simpler approach to care, involving the specialist physician, the gastroenterologist in this case, without the integrated use of other health care professionals (1).
Table 1.
Summary of recommendations for core and ancillary IBD MDT members
| Core Members | Ancillary Members |
|---|---|
| Gastroenterologist | Rheumatologist |
| IBD nurses | Ophthalmologist |
| Colorectal surgeon | Dermatologist |
| Psychologist or counsellor | Obstetrician |
| Registered dietitian | Psychiatrist |
| Endoscopist | Social worker |
| Radiologist | Physiotherapy |
| Pathologist | Nutritional support team |
| Pharmacist |
Table 2.
Summary of advantages and disadvantages of specialist and integrated IBD care models
| Advantages | Disadvantages | |
|---|---|---|
|
Specialist Model
• Gastroenterologist |
- Lower cost to the health care system in terms of outpatient cost - Less coordination of care required by health care professional |
- Disease-focused approach - Fragmented care - Variable across settings - Potential of lower quality care - Higher overall cost due to inpatient treatment, surgeries, and productivity loss - Psychosocial concerns not adequately addressed - Gastroenterologist burnout |
|
Integrated Models
• IBD Centres • Medical Homes • Centres of Excellence |
- Patient-centred approach - Preventative, holistic care - Involves active monitoring - Better equipped to meet the needs of IBD patients - Improves patient outcomes and satisfaction - Lower overall direct and indirect costs - Opportunity for research and sharing best practices - Psychological health needs better addressed |
- Higher outpatient cost due to more resources required - More time required for interprofessional meetings, communication and collaboration |
Over the last decade, there has been a gradual global trend to deliver IBD care through an integrated team approach (1, 3, 5). In an international survey done in 2014 by health care providers working in IBD, 54% of respondents reported using an integrated care model, wherea only 5% reported using an exclusively biomedical care model, defined as one that does not address psychosocial factors in the management of IBD (2). The services provided through integrated care models vary from centre to centre depending on funding and perceived necessity.
Research supports that the ideal integrated model would involve a gastroenterologist-led team, with a colorectal surgeon, IBD nurse specialists, dietician, and psychologist or counsellor (1, 5, 10, 11). Some sources suggested that the ideal MDT would also include a pathologist, radiologist and pharmacist with a special interest in IBD as core members of the team (8, 9). Specialty services should be available and used based on individual patient needs (see Table 1). These services may include a rheumatologist, ophthalmologist, dermatologist, psychiatrist, obstetrician, nutritional support team, social worker and physiotherapist (1, 3, 5, 8, 9). The international survey reported that the specialists most commonly involved in IBD care were gastroenterologists, IBD nurses, colorectal surgeons and dieticians, followed by radiologists, pathologists, psychologists and pharmacists (2) (see Table 2).
The gastroenterologist specializes in the medical treatment of IBD, with the ultimate goal of preventing the progression of widespread bowel damage and complications of the disease (11). Inflammatory bowel disease often requires surgical intervention, which would involve a colorectal surgeon. The endoscopist, radiologist and pathologist all play an important role in the proper diagnosis of IBD, monitoring disease progression and treatment effectiveness, and detecting complications and colorectal cancer (10, 12). Most often the primary attending gastroenterologist is the endoscopist involved in the care. The dietician and psychologist are essential in the management of malnutrition and mental health issues, respectively, which are both common in patients with IBD. Specialist IBD nurses play an important role in the care, education, advocacy and support of patients (1, 2, 10, 11).
Rheumatologists, ophthalmologists and dermatologists may play a role in treating the extraintestinal manifestations of IBD in the joints, eyes and skin (1, 5, 10). Birth, fertility and breastfeeding can all be affected by IBD; thus referral to an obstetrician could be necessary (10). Specialized pregnancy planning and ongoing follow-up clinics for patients with IBD have emerged (13). A referral to psychology or psychiatry may be necessary for patients needing complex medical management of anxiety, depression, or other psychiatric comorbidities (1, 2, 5, 8, 9). A physiotherapist, social worker and nutritional support team are other resources recommended in the literature to support patients and families (1, 2, 10, 11). All members of the team play an important role in optimizing care for patients with IBD.
Many health care centres worldwide are now using an integrated model to improve care for patients with IBD. A paper published by Mikocka-Walus et al. in 2012 described six IBD centres in various countries that were active in clinical IBD research and utilizing aspects of an integrated care model to examine common features being implemented (5). All six IBD centres included a gastroenterologist, five of the six included IBD nurses, four included psychological services, and two included a surgeon as part of the MDT. Commonalities of the six models included patient-centred care, mechanisms for active patient follow-up, patient education about IBD, consideration of biopsychosocial function of the patient, significant role of an IBD nurse, access to a variety of health care professionals, and coordination between child and adult services. Overall, the integrated model of care for IBD management was recommended by all six IBD centres over a patient-gastroenterologist approach (5).
Benefits of Integrated Care Models
The ultimate goal of multidisciplinary, integrated care models is to optimize IBD care by improving patient satisfaction and patient and population outcomes and decreasing costs of IBD. An integrated approach provides a variety of targeted resources to patients to improve overall physical and mental health, reducing complications of IBD that lead to high health care costs and productivity loss. Of the IBD health care professionals who responded to the international survey conducted by Panes et al., 51% reported funding as the greatest perceived barrier to implementing the ideal model of care recommended for IBD patients (2). The next most commonly reported perceived barrier, by 14% of respondents, was that health care systems do not seem conducive to multidisciplinary care—despite the evidence that studies suggested that providing quality care to patients with IBD can actually reduce direct and indirect costs, proving to be cost-effective for the economy long-term.
A study conducted at the Royal Adelaide Hospital (RAH) in Australia demonstrated that the use of a gastroenterologist-led IBD service reduced hospital admissions, lowering health utilization and lowering inpatient costs (6). The authors hypothesized that a formal IBD service based on an integrated care model would be superior to the standard patient-physician model of care. In this prospective cohort study, authors compared IBD and non-IBD groups before and after the implementation of an IBD service program to improve care and reduce cost. Electronic hospital sources were used to identify IBD patients who attended the RAH within predetermined time frames, and each IBD case was randomly assigned five age- and gender-matched controls using a computer algorithm. The IBD service included specialty IBD nurses, a weekly IBD clinic, a joint medical-surgical IBD clinic and regular radiology review sessions. The service also included a telephone help line, formal protocols for blood test monitoring, post-clinic and post-hospital discharge phone follow-ups, patient education and information leaflets. The variables measured in the study included the number of inpatient admissions, the total length of stay in the hospital, the cost of inpatient care and the complexity of the care provided as determined by the number of comorbidities documented.
The results showed that after the implementation of the IBD service, the IBD-group had fewer inpatient hospital admissions, a reduced total length of stay in hospital and a lower complexity of illness in hospital admissions (6). Due to inpatient care being the main factor in direct health care costs of IBD and hospital admissions correlating to disease severity, the implementation of the IBD service is likely to be clinically relevant in terms of patient outcomes and economic impact (6). The authors concluded that having an integrated chronic care model for treating IBD patients leads to net savings in direct and indirect health care costs and improves clinical patient outcomes. The cost of the outpatient services was not measured in this study.
Another study done at the University of Saskatchewan in Canada supported the concept that integrated care delivered through an MDT can enhance quality of care and improve outcomes for patients with IBD (7). A retrospective population-based matched cohort study was conducted using administrative health data, comparing outcomes between patients exposed and not exposed to an integrated model of care. The integrated model of care was a patient-centred, multidisciplinary IBD clinic with IBD fellowship-trained gastroenterologists, nurse practitioners, nurse clinicians, a clinical health psychologist and a clinical dietician with expertise in gastrointestinal nutrition (7). This model included biopsychosocial assessments, disease education and active follow-up including nurse-led telephone follow-ups and telemedicine care for patients from rural communities. The variables measured in the study were IBD-related hospitalizations and surgical treatments, prescription medication claims and corticosteroid dependency between the two groups (7).
The results showed that patients exposed to the integrated model of care had fewer IBD-related hospital admissions, surgeries for IBD and corticosteroid dependence. Authors also found that patients receiving care at the integrated IBD clinic had earlier induction of medical treatments and a lower risk of hospitalizations (7). The cost-effectiveness of this model was not studied directly.
Recommendations for MDTs
Based on the global literature of best practices, delivery of IBD care through an MDT is strongly recommended (1). There are a variety of recommendations suggested in the literature regarding MDTs and how they optimize IBD care and address gaps in care. Recommendations about MDTs focus on IBD nurses, psychological services, other MDT members and communication, all of which are discussed separately later on. No research or recommendations about the use of physician assistants (PAs) in IBD care were found.
IBD Nurses
There are strong recommendations in the literature to include IBD nurse specialists in the MDT because they play an invaluable role in the care of IBD patients (1, 2, 10). In an international survey study, IBD health care providers considered an IBD nurse the most essential health care provider for good quality care, aside from the gastroenterologist (2). Several studies reported improvements in patient outcomes when IBD nurses are involved in care. Studies also showed that IBD nurses reduce referral times, risk of complications, hospital utilization and burden of disease on patients (1, 10, 11).
Nurses are trained under the biopsychosocial model of care and have an understanding of the pathophysiology, symptoms, diagnosis and treatment of diseases. Their role in IBD care may involve providing clinical care, providing patient education, advocating for patient needs, performing research duties, coordinating flow of care and ensuring consistent patient monitoring and support (1, 10). Responsibilities may also include running telephone clinics, laboratory follow-ups and prescription refills. An IBD nurse is also well suited to act as a case manager for patients (i.e., someone who coordinates and organizes the overall care of patients, including drug monitoring, laboratory testing schedules and monitoring and surveillance procedures) (1). Inflammatory bowel disease nurses with competency in stoma care are also recommended to improve care (3). An IBD nurse’s ability to fill a variety of roles in the care of patients with IBD makes them an essential part of optimal care.
Psychological Services
There is a growing body of literature recognizing the importance of psychosocial factors in IBD and the need for targeted resources to address the mental health of the patient with IBD. The symptoms of chronic pain, fatigue and unpredictable bowel habits are likely to disrupt education, employment, personal relationships and social functioning (3). For these reasons, it is no surprise that those with IBD may struggle with poor self-esteem, anxiety and low moods.
Research suggests that addressing psychological comorbidities improves not only mental health outcomes but physical outcomes as well (5). A prospective study on gastrointestinal diseases showed that greater anxiety and depression are related to more frequent relapses in the follow-up period in IBD (5). Psychological distress, depression and anxiety may actually trigger disease relapse (10). Despite evidence linking mental and physical health in IBD, mental health issues are not well addressed in IBD care (1, 2). The IBD clinic at the University Hospital of Vienna developed a patient questionnaire to assess the demand for psychological care and found that about one-third of IBD patients demonstrated a high need for psychological intervention (5). An audit done in the United Kingdom found that only 24% of adult IBD services had defined access to a psychologist with an interest in IBD (3). Other studies showed that less than 40% of IBD patients with high levels of anxiety or depression receive treatment (10).
There is strong support in the IBD literature to include a psychologist or counsellor as a core member of the MDT to address mental health needs (1, 2, 5, 10). Surveyed IBD experts agree that the ideal IBD model would include a psychological assessment for every patient, rather than just those expressing concern in mental health (2). The use of screening tools, such as a patient questionnaire done before or during an appointment, would be a quick, easy and effective way to assess the need for further psychological intervention by a psychologist, counsellor or psychiatrist. Psychological screening tools have been validated for use in the IBD population (14). Research is showing promise for psychotherapy treatment to improve outcomes in IBD (5).
Other MDT Members
Involving an endoscopist, radiologist, pathologist and pharmacist with special interest and knowledge in IBD is important because they all play a crucial role in the proper diagnosis, treatment and surveillance of IBD (1, 10). In a study conducted by Louis et al., experts in the field of IBD were invited to discuss, modify and vote on suggested recommendations identified in the literature to optimized IBD care (10). This study found that 81% agreed that an IBD unit should have an endoscopy suite or structured access to one, and 81% agreed that an IBD unit should have access to imaging, such as computerized tomography (CT), magnetic resonance imaging (MRI) and ultrasound, including a formalized discussion with a radiologist incorporated into care. In this same study, 94% agreed that an IBD unit should have a pharmacist with experience in the administration of all approved drugs for IBD (10). These recommendations reflect the Canadian consensus for IBD quality indicators (15).
IBD experts also recommended a dietician with special knowledge and interest in IBD as a core member of the MDT for nutritional assessments and management of malnutrition and nutritional deficiencies (1–3, 10). A nutritional support team is recommended as a specialty service that should be available to patients needing further nutritional intervention (10). Using a screening tool for nutritional assessment in every patient has been recommended as a strategy for targeting nutritional services to those with the highest need (2). A new IBD specific screening tool, the Saskatchewan IBD-Nutrition Risk tool, has been validated to detect nutrition risk in persons with IBD (16).
Adding a physician assistant to the MDT could be a logical, cost-effective addition to improving access to quality care. Physician assistants are medically educated clinicians who practice within a formalized relationship with a physician as an extension of his or her services (17, 18). A physician assistant’s autonomy is negotiated with a supervising physician, and PAs can perform any task that is within the physician’s scope of practice, making them well suited to fill gaps in the health care system. The American Gastroenterological Association predicts that midlevel providers, such as PAs and nurse practitioners, will provide the majority of routine care of patients with chronic gastrointestinal illnesses (19). The integration of the PA into specialty clinics is just now gaining traction in Canada, and their roles may be similar to that of the nurse specialist in IBD care (19).
Communication
The advantage of having an MDT is not only to provide multiple services but also to provide patients with an integrated, holistic management plan. Thus, an important part of the MDT approach to IBD care is communication and collaboration between health care providers about the different aspects of the patient care (3, 10, 11). Recommendations support structured interactions and meetings with members of the MDT. The United Kingdom IBD Standards recommend scheduled weekly MDT meetings with all members of the team to discuss complex cases (3). Of the IBD experts who voted on recommendations to optimize IBD care in the study by Louis et al., 93% agreed that there should be structured interaction between the members of the MDT. Ninety-four percent of experts agreed that there should be joint decision-making before and after surgery involving the gastroenterologist, colorectal surgeon, and IBD patient, and 80% agreed that an IBD unit should coordinate care with supporting providers such as the primary care practitioner, the pediatric transition team, obstetrician/gynecologist, rheumatologist and dermatologist (10).
Patient communication and education is also an important aspect of IBD care. The literature suggested that MDT meetings should be formally documented and discussed with the patient (3). Studies showed that proper communication between the patient and their health care team can improve treatment adherence (11). Patients who are well informed about their disease and treatment are more likely to adhere to the treatment plan, making them better able to reach remission, limit bowel damage, and reduce long-term disability, ultimately improving their quality of life (11). Inflammatory bowel disease care teams should empower patients to understand their disease and involve them in the management whenever possible.
Communication between the IBD team and the patient’s primary care provider (PCP) is also an important aspect of outpatient IBD care (1, 11). Although the PCP is not a member of the IBD team, he or she can play a key role in supporting, educating and encouraging adherence to medications implemented by the gastroenterologist. The PCP can also assist the gastroenterologist in providing services such as keeping vaccinations up to date, monitoring bone health, encouraging smoking cessation and providing treatment for mental health issues (20). Communication with the PCP can be a key component to improve patient outcomes.
Quality Improvement Initiatives in IBD Care
Quality improvement (QI) initiatives in IBD are implemented to address gaps in care and focus on delivering patient-centred care, improve patient and population outcomes, and reduce costs (21, 22). Quality improvement initiatives have been successful in improving outcomes in other chronic diseases such as cystic fibrosis and cardiac disease (23). Quality improvement measures offer a means to quantify changes in health care structure, clinical processes and patient outcomes. Structure measures address systems, staffing and availability of health services. Process measures are used to evaluate aspects of diagnosis, treatment, preventative care and health care maintenance. For example, one study found significant adherence improvement with influenza vaccination after implementing a simple vaccination questionnaire before an IBD clinic (23). Outcome measures assess days lost from work or school, hospitalizations, emergency room visits, steroid use, symptoms and comorbidities (24). With improvement in structure and process measures, health outcomes should also improve (23). New and innovative integrated care models are being implemented to improve outcomes and decrease costs, and the effectiveness of these models is being studied.
Medical Homes
A medical home is an integrated care model developed in the United States, traditionally used in a primary care setting to deliver patient-centred, comprehensive, team-based and accessible care to specific patient populations (25, 26). Specialty medical homes (SMH), which are medical homes with a specialist acting as the primary provider coordinating all aspects of the patient’s care, are now being used to treat patients with IBD in the United States. These models involve collaboration with an insurance company to improve value and reduce cost (25, 26). Elements necessary for the success of these integrated models include engaging patients in their own care and having a team approach that embraces collaboration with physician-extenders, nurses, dieticians, psychologists, pharmacists and other health care providers as needed (25).
The University of Pittsburgh Medical Center launched a specialty medical home for patients with IBD in 2015 for all health plan–insured IBD patients, with a focus on high-utilization patients (26). Services provided in this model included a personal nurse coordinator for each patient, 24/7 on-call gastroenterologist, telemedicine and home visits by nurses and rapid access outpatient care (25, 26). In this model, preventative, acute and chronic care is provided by the gastroenterologist, nurses, dietician, physician extenders and behavioural health and pain specialists (25). Key components of this model included psychological care, pain management, nutritional support, increased access to care and standardized checklists for vaccine-preventable illnesses, bone health, cancer prevention and medication-related toxicity evaluation. This model demonstrated significant overall cost savings and improved outcomes (25) through reduction in the total cost of care, a reduction in emergency room visits and hospital admissions within the first year, and improved patient-reported quality of life (22).
Centres of Excellence
A Centre of Excellence (CoE) is a framework for sharing best practices and addressing gaps in care and is being utilized in many areas of medicine for chronic and complex diseases (1). The development of IBD CoEs is organized around three pillars of excellence: patient care, research and education. Unlike specialty medical homes, CoEs are often built around the health care team, more typically at academic centres, and require collaboration with hospitals/medical centres (25). Integrated care delivered by an MDT at a centre of excellence appears to be an effective model for long-term IBD care (1, 11, 12), and there is support for the use of this model worldwide (11). The Canadian Digestive Health Foundation recommends adoption of a multidisciplinary team approach in a CoE throughout the country. An IBD CoE may not be realistic to have in every area due to the start-up costs required, but they provide insight into best practices and ideas to include in integrated IBD care models as resources allow (1, 11).
One example of a CoE comes from St. Mark’s Hospital in London, with an MDT made up of 15 gastroenterologists, 10 surgeons, five specialist nursing teams, a psychological medicine unit, pharmacy, radiology and pediatric services, and clinical research teams (11, 27). Specialist nursing teams include an IBD team, stoma and pouch team, nutrition team and endoscopy team. The role of the IBD nursing team involves patient education, advocacy in team meetings, management of difficult symptoms, psychological support and IBD telephone lines for better access to appropriate care. Several weekly MDT meetings take place, including an IBD MDT meeting to discuss complex patients, a virtual biologic meeting to discuss monitoring of medical treatment, a dysplasia/polyp meeting to discuss surveillance, a psychosocial meeting to discuss overall well-being of patients, and an IBD executive meeting to discuss service planning. Meetings are documented to allow communication with patients and primary care practitioners. To date, however, data have not been reported on the effectiveness of this model compared with other models of care.
In 2016, Canada launched the Promoting Access and Care through Centres of Excellence (PACE) network to unite CoEs across the country to close the gap in IBD care (28). Crohn’s and Colitis Canada is investing $2.8 million over four years in five leading IBD centres across the nation in Toronto, Calgary, Edmonton, Hamilton and Montreal. Each centre has a defined quality of care initiative that includes providing IBD specialist services to remote communities through telemedicine; monitoring patient health between visits through innovative and interactive mobile apps; the establishment of EMR-integrated clinical care pathways to reduce chronic steroid use; and the development of metrics and infrastructure for systematically measuring quality of care, including the PACE model itself. The telemedicine initiative has most elements of an MDT, including an IBD nurse coordinator, urgent care services, a dietician, a surgeon, psychological services for cognitive behavioural therapy and access to ancillary services as needed. The ultimate goal is to add more CoEs to the PACE network as a means of sharing information to advance best practices and improve the standard of care for all patients living with IBD. Evidence gathered through clinical care and research can be used to promote change to improve IBD care in the public health care system (28). The studies are incomplete, but early results indicate increased access and quality of care and decreased wait times for patients.
DISCUSSION
Integrated Models of Care
Poorly controlled IBD is associated with decreased quality of life, psychological distress, multiple comorbidities and potentially life-threatening complications, which are a burden not only to patients with IBD but also to the health care system and economy (1, 3). Without organization of resources and prompt access to care, treatment for IBD is often emergent, reactive and costly, requiring more hospital admissions, surgeries and medications. It is well established in the literature that integrated care delivered by a gastroenterologist-led MDT is the most effective care model for patients with IBD (1, 2, 5, 10, 11). A comprehensive integrated care model employs a proactive, preventative, team approach to care, superior to the more traditional patient-physician model.
Common features of integrated multidisciplinary care models include patient-centred care, prompt access to care, mechanisms for active follow-up, patient education about IBD and treatment, interprofessional collaboration and communication, and a focus on addressing the biopsychosocial factors affecting patients. Studies showed that implementing an MDT with targeted resources to meet the needs of patients with IBD can decrease emergency room visits, hospital admissions, length of stay in the hospital, disease comorbidity and IBD-relate surgeries, ultimately improving health outcomes and patient-reported quality of life while reducing overall IBD costs (6, 7, 21).
Recommendations put forth to optimize care focus on expanding the MDT of health care providers to better meet the needs of patients with IBD. In addition to the gastroenterologist, the MDT should include a surgeon, IBD nurse, psychologist or counsellor, dietician, radiologist, pathologist, and pharmacist with special knowledge and experience in IBD. As endoscopy specializes in terms of sophisticated imaging for cancer diagnosis and resection of complex polypoid lesions, there may be a need for a specialized endoscopist distinct from the gastroenterologist leading the team (3, 10). Supporting services should be available depending on patient need.
Aside from a gastroenterologist, the most crucial aspects of care come from IBD nurses and psychological services. Inflammatory bowel disease nurses perform a wide variety of tasks which improve quality, access and flow of care, and psychological services address mental health issues which are known to impact disease activity. Based on the literature, focusing more resources on psychological care in IBD patients has the potential for greatly improving quality of life for patients, reducing disability and reducing cost to the health care system and economy (5, 10).
A barrier to widely implementing a fully integrated care model for patients with IBD is the perceived cost associated. Although an MDT may initially be more resource-intensive than the simple patient-physician model of care, this proactive approach reduces the need for expensive health care utilization and reduces productivity loss of patients, which results in long-term cost saving. Higher quality of care is in fact less expensive in regard to IBD (22).
Promising initiatives for quality improvement have been implemented in different IBD clinics worldwide. Services such as telemedicine, telephone help lines, telephone follow-ups, team meetings, IBD clinics offering urgent care, protocols for blood work and screening all have the potential to optimize care for patients with IBD. Inflammatory bowel disease CoEs offer hope for improving patient and population outcomes and decrease overall cost of IBD in Canada.
In Canada, the initial funding for CoEs through programs such as PACE has been through philanthropic organization such as Crohn’s and Colitis Canada and through industry partners. However, these funding mechanisms are often not sustainable. Longer-term and more widespread funding for collaborative care models will need to be secured by partnering with provincial health ministries. In order to engage health policy makers and administrators, collaborative IBD centres will need to demonstrate improvement in measurable and economically impactful health outcomes such as reductions in IBD-attributable emergency department and hospital visits and surgeries. Importantly, they would have to demonstrate that initial financial investment in collaborative care models will yield sustainable cost-savings.
Limitations and Future Research
One limitation of this literature review is the availability of previously published research using the selection process outlined in the Methods section. For example, only one main database was used for the search, and only free articles available in full-text were considered for the review. Furthermore, certain article exclusion criteria used were based on the authors’ discretion of perceived relevance of the article to the core objectives of the literature review. Another possible limitation of this review is the use of webpage articles to collect information. Though each webpage used was considered reliable based on the authors’ judgement, these sources are not necessarily peer-reviewed and may be subject to bias.
There were also several limitations to the studies found on integrated care models used in IBD. Limitations exist due to the design and data sources of the studies available such as retrospective cohort studies and survey studies, which can be subject to confounding. For example, the international survey of IBD health professionals had a small sample size, and survey studies are often subject to selection bias. Also, changes and advances in medical treatment over time may confound prospective and retrospective cohort studies. Studies used in this literature review discuss limitations and account for them in their conclusions.
Another limitation of the studies on IBD care models was the lack of description of the point of reference for comparison. The integrated services being implemented were well described, but the services in place for IBD patients before implementation were not. Similarly, many articles that discussed the effectiveness of integrated care models compared with the patient-physician model do not explicitly state what the patient-physician models included. Studies comparing different integrated care models were not found.
Another limitation of research on integrated models of care is that indirect cost reduction is underreported and thus likely undervalued in the literature. More research is needed on the cost-effectiveness of integrated care models to support implementation, but indirect cost savings are difficult to quantify. Using outcome measures such as days lost from work or school is one way of determining indirect cost, but these have not been consistently reported in studies. This is of significance because the greatest barrier to implementing an MDT to improve IBD care is the perceived financial burden.
Despite the improvements in IBD care over the last decade, gaps in care still exist and must be addressed (1). Studies continue to quantify the impact of QI initiatives using a variety of different measures to determine which patient outcomes are improved by an integrated care model and by how much. More research is needed to support long-term cost benefit to secure government funding to sustain these models (5). Future research should also compare different integrated care models offering different services or aspects of IBD care to determine which services are most effective for improving outcomes and decreasing costs. Research is needed to determine how an MDT model would impact quality improvement initiatives and patient and physician satisfaction.
Supplementary Material
Acknowledgements
Author contributions: RS contributed to the concept, data extraction, drafting of manuscript and final manuscript approval. GN and CB contributed to the concept, manuscript revision and final approval.
Conflicts of Interest
CB is supported in part by the Bingham Chair in Gastroenterology. He has served on advisory boards for Abbvie Canada, Ferring Canada, Janssen Canada, Shire Canada, Takeda Canada, Pfizer Canada and Napo Pharmaceuticals. He has consulted to 4D Pharma and Mylan Pharmaceuticals. He has received educational grants from Abbvie Canada, Shire Canada, Takeda Canada and Janssen Canada. He has served on speaker’s panel for Abbvie Canada, Ferring Canada and Shire Canada. GN is supported by a CIHR Embedded Clinician Researcher Award. He has served on advisory boards for Abbvie and Janssen.
References
- 1. Best practices in IBD care [Internet]. Canadian Digestive Health Foundation, 2013. [cited 2018 Apr 1]. 1–36. <http://www.cdhf.ca/bank/document_en/75best-practices-in-ibd-care.pdf> (Accessed September 11, 2018). [Google Scholar]
- 2. Mikocka-Walus A, Andrews JM, Rampton D, et al. . How can we improve models of care in inflammatory bowel disease? An international survey of IBD health professionals. J Crohn’s Colitis 2014;8(12):1668–74. [DOI] [PubMed] [Google Scholar]
- 3. Standards for the Healthcare of People who have Inflammatory Bowel Disease [Internet]. Crohn’s and Colitis UK. The IBD Standards Group, 2013, 1–32. <https://www.crohnsandcolitis.org.uk/improving-care-services/health-services/ibd-standards> (Accessed April 1, 2018). [Google Scholar]
- 4. Miller H, Farraye F. Inflammatory bowel disease. In: Griggs R, Wing E, Fitz G, editors. Cecil Essentials of Medicine. 9th ed. Philadelphia, PA: Elsevier Inc., 2016:417–24. [Google Scholar]
- 5. Mikocka-Walus AA, Andrews JM, Bernstein CN, et al. . Integrated models of care in managing inflammatory bowel disease: A discussion. Inflamm Bowel Dis 2012;18(8):1582–7. [DOI] [PubMed] [Google Scholar]
- 6. Sack C, Phan VA, Grafton R, et al. . A chronic care model significantly decreases costs and healthcare utilisation in patients with inflammatory bowel disease. J Crohn’s Colitis 2011;6(3):302–10. [DOI] [PubMed] [Google Scholar]
- 7. Peña-Sánchez JN, Lix LM, Teare GF, et al. . Impact of an integrated model of care on outcomes of patients with inflammatory Bowel diseases: Evidence from a population-based study. J Crohn’s Colitis 2017;11(12):1471–9. [DOI] [PubMed] [Google Scholar]
- 8. Druss B, Rohrbaugh R, Levinson C, et al. . Integrates medical care for patients with serious psychiatric illness: A randomized trial. Arch Gen Psychiatry 2001;58:861–8. [DOI] [PubMed] [Google Scholar]
- 9. Ho S, Brau N, Cheung R, et al. . Integrated care increases treatment and improves outocme of patients with chronic hepatitis C virus infection and psychiatirc illness or substance abuse. Clin Gastroenterol Hepatol 2015;13:2005–14.e1-3. [DOI] [PubMed] [Google Scholar]
- 10. Louis E, Dotan I, Ghosh S, et al. . Optimising the inflammatory bowel disease unit to improve quality of care: Expert recommendations. J Crohn’s Colitis 2015;9: 685–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Panés J, Connor MO, Peyrin-biroulet L, et al. . Improving quality of care in inflammatory bowel disease: What changes can be made today?J Crohn’s Colitis 2014;8(9):919–26. [DOI] [PubMed] [Google Scholar]
- 12. Negreanu L, Bataga S, Prelipcean CC, et al. . Excellence centers in inflammatory bowel disease in Romania: A measure of the quality of care. J Gastrointest Liver Dis 2014;23:333–7. [DOI] [PubMed] [Google Scholar]
- 13. Shitrit A, Cohen Y, Hassin O, et al. . Antenatal management for women with inflammatory bowel disease: Experience from our “IBD MOM” clinic. Dig Dis Sci 2018;63(7):1774–1781. [DOI] [PubMed] [Google Scholar]
- 14. Bernstein C, Zhang L, Graff L, et al. . The validity and reliability of screening measures for depression and anxiety disorders in inflammatory bowel disease. Inflamm Bowel Dis 2018. doi: 10.1093/ibd/izy068. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bitton A, Vutcovici M, Lytvyak E, et al. . Selection of quality indicators in IBD: Integrating physician and patient perspectives. Inflamm Bowel Dis 2018. doi: 10.1093/ibd/izy259. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 16. Haskey N, Pena-Sanchez JN, Jones JL, et al. . Development of a screening tool to detect nutrition risk in patients with inflammatory bowel disease. Asia Pac J Clin Nutr 2018;27(4):756–62. [DOI] [PubMed] [Google Scholar]
- 17. What is a Physician Assistant? [Internet]. University of Manitoba, 2017. <http://umanitoba.ca/faculties/health_sciences/medicine/education/paep/whatisapa.html> (Accessed May 1, 2018). [Google Scholar]
- 18. Role of PAs in the Health System. Canadian Association of Physician Assistants. 2018. <https://capa-acam.ca/about-pas/pa-fact-sheet/> (Accessed April 1, 2018).
- 19. Dorn SD. Mid-level providers in gastroenterology. Am J Gastroenterol 2010;105(2):246–51. [DOI] [PubMed] [Google Scholar]
- 20. Greene L, Sapir T, Moreo K, et al. . Impact of quality improvement educational interventions on documented adherence to quality measures for adults with Crohn’s disease. Inflamm Bowel Dis 2015;21:2165–71. [DOI] [PubMed] [Google Scholar]
- 21. Van Deen WK, Spiro A, Ozbay AB, et al. . The impact of value-based healthcare for inflammatory bowel diseases on healthcare utilization: A pilot study. Eur J Gastroenterol Hepatol 2017;29(3):331–7. [DOI] [PubMed] [Google Scholar]
- 22. Berry SK, Siegel CA, Melmed GY. Quality improvement initiatives in inflammatory bowel disease. Curr Gastroenterol Rep 2017;19(8):41. [DOI] [PubMed] [Google Scholar]
- 23. Shah R, Hou JK. Approaches to improve quality of care in inflammatory bowel diseases. World J Gastroenterol 2014;20(28):9281–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Inflammatory Bowel Disease [Internet]. International consortium for health outcomes measurement. 2016. <http://www.ichom.org/medical-conditions/inflammatory-bowel-disease/> (Accessed September 11, 2018).
- 25. Regueiro MD, McAnallen SE, Greer JB, et al. . The inflammatory bowel disease specialty medical home: A new model of patient-centered care. Inflamm Bowel Dis 2016;22(8):1971–80. [DOI] [PubMed] [Google Scholar]
- 26. Kosinski LR, Brill J, Regueiro M. Making a medical home for IBD patients. Curr Gastroenterol Rep 2017;19(5):20. [DOI] [PubMed] [Google Scholar]
- 27. St Mark’s Hospital Foundation [Internet]. St Mark’s Hospital and Academic Institute, 2017. <http://www.stmarkshospital.nhs.uk/about/st-marks-hospital-foundation/> (Accessed April 1, 2018). [Google Scholar]
- 28. New Crohn’s and Colitis Canada Network Unites World-class Canadian Health care Centres [Internet]. Crohn’s and Colitis Canada, 2016. <http://crohnsandcolitis.ca/Research/Our-funded-research/PACE-Network> (Accessed April 1, 2018). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.