ABSTRACT
The inhibitory receptor TIGIT, as well as theectonucleotidases CD39 and CD73 constitute potential exhaustion markers for T cells. Detailed analysis of these markers can shed light into dysregulation of the T-cell response in acute myeloid leukemia (AML) and will help to identify potential therapeutic targets. The phenotype and expression of transcription factors was assessed on different T-cell populations derived from peripheral blood (PB, n = 38) and bone marrow (BM, n = 43). PB and BM from patients with AML diagnosis, in remission and at relapse were compared with PB from healthy volunteers (HD) (n = 12) using multiparameter flow cytometry. An increased frequency of terminally differentiated (CD45R−CCR7−)CD8+ T cells was detected in PB and BM regardless of the disease state. Moreover, we detected an increased frequency of two distinct T-cell populations characterized by the co-expression of PD-1 or CD39 on TIGIT+CD73−CD8+ T cells in newly diagnosed and relapsed AML in comparison to HDs. In contrast to the PD-1+TIGIT+CD73−CD8+ T-cell population, the frequency of CD39+TIGIT+CD73−CD8+ T cells was normalized in remission. PD-1+- and CD39+TIGIT+CD73−CD8+ T cells exhibited additional features of exhaustion by decreased expression of CD127 and TCF-1 and increased intracellular expression of the transcription factor TOX.
CD8+ T cells in AML exhibit a key signature of two subpopulations, PD-1+TOX+TIGIT+CD73−CD8+- and CD39+TOX+TIGIT+CD73−CD8+ T cells that were increased at different stages of the disease. These results provide a rationale to analyze TIGIT blockade in combination with inhibition of the purinergic signaling and depletion of TOX to improve T-cell mediated cytotoxicity in AML.
Abbreviations: AML: Acute myeloid leukemia; pAML: newly diagnosed AML; rAML: relapse AML; lrAML: AML in remission; HD: healthy donor; PB: peripheral blood; BM: bone marrow; TIGIT: T-cell immunoreceptor with Ig and ITIM domains; PD-1: Programmed cell death protein 1; CD73: ecto-5′-nucleotidase; CD39: ectonucleoside triphosphate diphosphohydrolase 1; ATP: adenosine triphosphate; ADO: adenosine; CD127: interleukin-7 receptor; CAR-T cell: chimeric antigen receptor T cell; TCF-1: transcription factor T-cell factor 1; TOX: Thymocyte selection-associated high mobility group box protein; NFAT: nuclear factor of activated T cells; NA: Naïve; CM: Central Memory; EM Effector Memory; EMRA: Terminal Effector Memory cells; FMO: Fluorescence minus one; PVR: poliovirus receptor; PVRL2: poliovirus receptor-related 2; IFN-γ: Interferon-γ; IL-2: interleukin-2; MCF: multiparametric flow cytometry; TNFα: Tumornekrosefaktor α; RT: room temperature.
KEYWORDS: Acute myeloid leukemia (AML), T cells, TIGIT, CD73, CD39, PD-1, TCF-1, CD127, TOX
Introduction
Novel immunotherapeutic strategies based on enhancement of T-cell function are constantly being developed for the treatment of acute myeloid leukemia (AML).1 These strategies include vaccines, T-cell recruiting bispecific antibody constructs, chimeric antigen receptor (CAR) T cells and immune checkpoint inhibitors.2 However, apart from allogeneic stem cell transplantation, the results of immunological approaches to treat AML have been less encouraging compared to other tumor entities.3 It is becoming increasingly apparent that AML is a heterogeneous disease with various immunosuppressive mechanisms to overcome immune surveillance. Therefore, a detailed knowledge of T-cell function during the course of the disease, e.g. at diagnosis, relapse and at remission, is essential.
Inhibitory receptors and their ligands such as programmed cell death protein 1/programmed cell death 1 ligand (PD-1/PD-L1) play a crucial role in the regulation of inflammatory responses by inhibiting T-cell effector activity. During chronic infection and cancer T cells are exposed to persistent antigen stimulation, which are often associated with loss of T-cell function and upregulation of multiple inhibitory receptors, a state called T-cell exhaustion.4 We and others have recently identified the coinhibitory receptor T-cell immunoglobulin and immunoreceptor tyrosine–based inhibitory motif (ITIM) domain (TIGIT) as a potential target for immunotherapeutic strategies in AML.5 TIGIT is expressed on (virus-specific) CD8+ and both conventional CD4+ (conCD4+) and regulatory CD4+ (regCD4+) T cells, as well as natural killer (NK) cells in chronic infections and cancer.6,7
The ectoenzymes CD73 (ecto-5′-nucleotidase) and CD39 (ectonucleoside triphosphate diphosphohydrolase 1) are related to the purinergic signaling that regulates lymphocyte activation and function. Adenosine triphosphate (ATP) released from cells under conditions of stress, inflammation or by regulated secretion is converted to adenosine (ADO) by sequential dephosphorylation by CD39 and CD73.8 ADO evokes predominantly anti-inflammatory signals.8 In cancer, CD73 and CD39 are upregulated in solid tumor cells and increasingly recognized as promising targets for immunotherapeutical approaches.9,10 Moreover, CD73 seems to play a role as costimulatory molecule for T-cell differentiation.11 CD39 is expressed on antigen-specific (tumor-infiltrating) CD8+ T cells, conCD4+, regCD4+ T cells and NK cells.12–14
The interleukin-7 receptor (CD127) and the transcription factor T-cell factor 1 (TCF-1) are involved in the development of long-living memory cells and self-renewal in T cell-populations.15 CD127 is required for the establishment and maintenance of memory CD4+ and CD8+ T lymphocytes.16 TCF-1 identifies antigen-experienced murine and human CD8+ T cells that retain potential for lymphoid recirculation and the ability for self-renewal.17
The transcription factor thymocyte selection-associated high mobility group box (TOX) regulates terminal T-cell exhaustion in chronic viral infections and cancer. Scott et al. showed that TOX was highly expressed in human dysfunctional T cells in melanoma, breast, lung and ovarian cancer. Its expression was driven by chronic T-cell receptor stimulation and activation of the NFAT (nuclear factor of activated T cells) family of transcription factors.18,19 Further, the expression of TOX has been associated with failure of CD8+ T-cell re-invigoration upon inhibitory receptor inhibition.18
In this study, we provide a comprehensive analysis of the expression of TIGIT, the ectonucleotidases CD39 and CD73, and of the transcription factors TCF-1 and TOX on CD8+, and conventional and regulatory CD4+ T-cell populations in peripheral blood (PB) and bone marrow (BM) samples from AML patients at different stages of the disease.
Material and methods
Clinical cohorts
Peripheral blood (PB) of AML patients (n = 38) and bone marrow (BM) of AML patients (n = 43) were collected at diagnosis, relapse and in remission before the start of intensive chemotherapy treatment as well as from healthy volunteers (HD, n = 12) after written informed consent in accordance with the Declaration of Helsinki and approval by the local ethics board of the Ärztekammer Hamburg (PV3469). All samples were taken from non-acute promyelocytic leukemia (APL) AML patients.
PB and BM samples were available from patients with newly diagnosed AML (pAML, PB, n = 20, median age 60 years; range 25–88 and BM, n = 24, median age 65 years; range 25–88), patients after chemotherapy-induced complete remission (lrAML, PB, n = 10, median age of 67 years; range 51–80 and BM, n = 10; median age of 62 years; range 51–79) and patients with relapsed AML (rAML, PB, n = 8, median age of 66 years; range 50–74 and BM, n = 9; median age of 66 years; range 48–77). Patients in remission were for a median of 620 days (rang 89–894 days) in CR. Paired PB and BM specimens were obtained from 17 patients with pAML, from 5 patients with rAML and from 7 patients with lrAML. Three patients donated PB and BM at diagnosis and at relapse, one patient donated PB and BM at diagnosis and in remission. PB of 12 healthy volunteers (HD) (with a median age of 48.5 years, range 25–86 years) were obtained as controls (Supplement 1).
Multiparameter flow cytometry, surface and intracellular staining (ICS)
For intracellular staining and multiparametric flow cytometry analysis (MCF), cryopreserved PB and BM mononuclear cells from patients with CD33+ AML were thawed and counted. After washing with PBS and FCR blocking PBMCs were stained with the LIVE/DEAD™ Fixable Near-IR dye (Thermo Fisher) according to the manufacturer’s protocol for exclusion of dead cells. For surface staining, cells were incubated with appropriate fluorochrome-conjugated antibodies, including anti-CD3 (OKT3), anti-CD4 (RPA-T4), anti-CD8 (RPA-T8), anti-CD25 (2A3), anti-CD127 (A019D5), anti-CD45RO (UCHL1), anti-CCR7 (G043H7), anti-TIGIT (A15153G), anti-PD-1 (EH12.2H7), anti-HLA DR (L243), anti-CD39 (A1), anti-CD73 (AD2) and anti-CD33 (P67.6), for 20 min at RT in the dark. For intracellular staining, the cells were subsequently fixed and permeabilized using the Foxp3 Fixation/Permeabilization Buffer Set (eBioscience) according to the manufacturer’s instructions. Subsequently, samples were stained with the fluorochrome‐labeled antibodies anti-TOX (TXRX10; REA473) and anti-TCF-1 (7F11A10) and incubated for 45 min at 4°C in the dark. Antibodies were obtained from Biolegend, ThermoFisher and BD Biosciences. Samples were washed with permeabilization buffer and then resuspended in PBS. Compensation controls were measured using single-stained Comp Beads (Anti-Mouse Ig,κ/Negative Control Compensation Particles Set, BD Biosciences). For live/dead compensation, Comp Beads stained with anti-CD14 (APC Cy-7, BioLegend) were applied. All samples were run on a BD LSR Fortessa flow cytometer with FACS Diva version 8 (BD Biosciences) on a PC.
Statistical analysis
All flow cytometric data were analyzed using FlowJo version 10.5.2. software (Treestar). Statistical analysis was carried out using Prism 7.0 software (GraphPad Software). All groups were tested for normal distribution with the Kolmogorov–Smirnov test. For normally distributed data, parametric tests were applied: for two groups t-tests, for more than two groups ANOVA multiple comparison test. Data that was not normally distributed was tested by the Mann-Whitney test for two unpaired groups, by the Wilcoxon test for paired groups, or Kruskal-Wallis test for more than two groups, respectively. Pearson’s correlation and Spearman’s rank correlation coefficient were applied for bivariate correlation analysis. Frequencies in the text are described as medians unless stated otherwise (as indicated in the figure legend). P-values smaller than 0.05 were considered significant, where *, ** and *** indicate p-values between 0.01 to 0.05, 0.001 to 0.01 and 0.0001 to 0.001, respectively. Statistical analysis and display of multicomponent distributions were performed with SPICE v5.1.
Results
Increased frequency of TIGIT+ and CD73−CD8+ T cells in peripheral blood and bone marrow from patients with newly diagnosed AML
The expression patterns of the coinhibitory molecules PD-1 and TIGIT and the ectonucleotidases CD73 and CD39 were assessed on CD8+, conCD4+ and regCD4+ T cells from the PB and BM of patients with pAML (PB, n = 20 and BM, n = 24) and PB from HDs (PB, n = 12).
A comparison of PB from HDs vs. patients with pAML revealed no differences in the frequency of PD-1 on CD8+, conCD4+ or regCD4+ T cells (Figure 1a-b). In contrast, we observed an increased frequency of TIGIT+ and CD39+CD8+ T cells and a decreased frequency of CD73+CD8+ T cells in the PB from patients with pAML in comparison to HDs (median of 35.6% vs. 17.6%; p = .0018, median of 3.3% vs. 0.9%; p = .05 and median of 44.1% vs. 76.8%; p = .0041) (Figure 1a-b). Comparison of CD8+ T cells in BM vs. PB from patients with pAML revealed similar frequencies of TIGIT+-, CD39+- and CD73+CD8+ T cells (Figure 1b). No differences in the frequency of PD-1, TIGIT, CD73 and CD39 expressing cells were found on conCD4+ and regCD4+ T cells between AML and HDs (Figure 1b). In summary CD8+ T cells in the PB and BM from patients with pAML exhibited an aberrant expression of TIGIT, CD39 and CD73 in comparison HDs.
Figure 1.
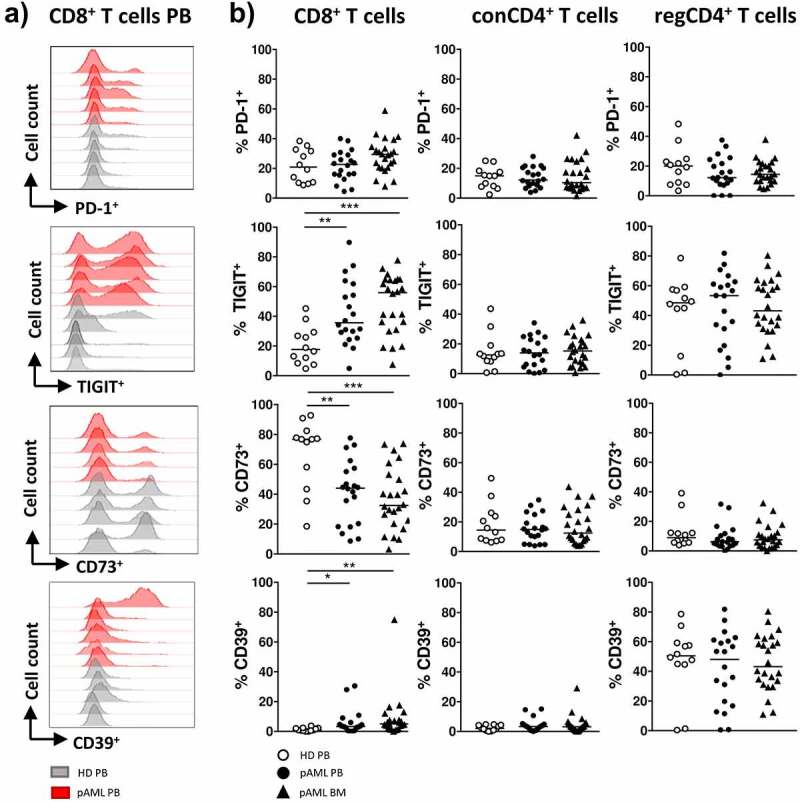
Expression of PD-1, TIGIT, CD73 and CD39 on CD8+ and conCD4+ and regCD4+ T cells in pAML and HDs
The expression of PD-1, TIGIT, CD73 and CD39 was analyzed in peripheral blood (PB) from healthy donors (HD, white circles, n = 12) and from patients with newly diagnosed AML (pAML, PB, black circles, n = 20) as well as in bone marrow aspirates (BM, black triangles, n = 24). The gating strategy is shown in Supplemental Figure 3. (A) Representative flow data showing the expression levels of PD-1, TIGIT, CD73, and CD39 on CD8+ T cells in the PB from HDs (gray) and PB from patients with pAML (red). (B) Frequencies of PD-1, TIGIT, CD73, CD39 expression on indicated T-cell subsets were shown in the PB from HDs and patients with pAML and in the BM. P values were obtained by the ANOVA and Kruskal-Wallis test. *P < .05, **P < .01, ***P < .001.
Peripheral blood and bone marrow CD8+ T cells of AML patients show a shift toward a terminally differentiated phenotype (CCR7−CD45RO−) regardless of the disease status
CD8+, conCD4+ and regCD4+ T cells in the PB and BM from AML patients with different disease status or HDs were further classified into the following subpopulations on the basis of their expression of CCR7 and CD45RO: Naïve (NA = CCR7+CD45RO−), Central Memory (CM = CCR7+CD45RO+), Effector Memory (EM = CCR7−CD45RO+) and terminal Effector Memory cells expressing CD45RA (EMRA, defined as CCR7−CD45RO−) (for gating strategy see Supplement 3). In comparison to HDs the frequency of CD8+ EMRA T cells was increased (median of 37.8% vs. 8.9%; p = .0013) whereas the frequency of the CD8+ NA T cells was decreased (median of 28.0% vs. 64.3%; p = .0021) in PB from patients with pAML (Supplement 2). Comparison of the CD8+ T cells in PB vs. BM revealed similar frequencies of CD8+ NA and EMRA T cells in both compartments (Supplement 2). Cross-sectional analysis of the PB and BM compartment of AML patients with different disease status showed a persistent increased frequency of the CD8+ EMRA T cells in the PB and BM from patients with pAML, patients in lrAML and with rAML in comparison to HDs (Supplement 2). Together our data show an increased terminally differentiated effector memory subset of CD8+ T cells in the PB and BM from patients with AML, thus providing a rationale to further analyze CD8+ T cells in AML.
Expression of PD-1, TIGIT, CD73 and CD39 is related to the differentiation status of CD8+ T cells in peripheral blood and bone marrow from patients with newly diagnosed AML
It has been shown that the expression of coinhibitory receptors and ectonucleotidases varies according to the differentiation status of the cell.11,20 Increased frequencies of TIGIT+ cells were observed in the CD8+ EM (p = .045) and CD8+ EMRA T-cell populations (p = .047) in PB from patients with pAML in contrast to HDs (Supplement 4A-B). In the BM of patients with pAML we found an increased frequency of TIGIT+ cells only in CD8+ EM T-cell subset in comparison to HDs (p = .06) (Supplement 4B). The decreased frequency of CD73+CD8+ T cells occurred in all four CD8+ differentiation stages in PB of patients with pAML in comparison to HDs (NA: p = .0104 and CM: p = .008 and EM: p = .09 and EMRA p = .023) (Supplement 4A-B). Similar results were observed in the BM from patients with pAML (Supplement 4B). The frequency of CD39+ cells was significantly higher in CD8+ EM (p = .002) and CD8+ EMRA T cells (p = .0092) in PB with similar results in the BM from patients with pAML in contrast to HDs (Supplement 4A+B). Overall, the CD8+ effector memory and terminally differentiated effector memory T-cell population in pAML showed increased expression of TIGIT and CD39 whereas the frequency of CD73+ cells was reduced in this CD8+ T-cell subsets in comparison to HDs.
Increased co-expression of CD39 and PD-1 in TIGIT+CD73−CD8+ T cells of patients with newly diagnosed AML
In our analysis, the most significant differences between newly diagnosed AML patients and HDs occurred in TIGIT and CD73 expression on CD8+ T cells in AML. The frequency of the TIGIT+CD73−CD8+ T-cell subset was significantly increased in the PB and BM from patients with pAML in contrast to HDs (Figure 2a). This specific phenotype of CD8+ T cells was located in the EM and EMRA CD8+ T-cell compartment (Supplement 5A+B). Hence, we further investigated the co-expression of PD-1 and CD39 on CD73+ and CD73−, as well as on TIGIT+ and TIGIT−CD8+ T cells in PB of AML patients. PD-1+ and CD39+ cells were significantly enriched in CD73− and TIGIT+CD8+ T cells in comparison to CD73+ and TIGIT-CD8+ T cells (Supplement 6A-B). Moreover, highest frequencies of PD-1+ cells were observed in the TIGIT+CD73−CD8+ T-cell subset in the PB and BM of patients with pAML in comparison to PB of HDs (PB vs. PB: 41.6% vs. 35.1%; p = .0494 and BM vs. PB: 44.2% vs. 35.1%; p = .0215) (Figure 2b). This was also true for CD39 within the TIGIT+CD73−CD8+ T-cell subset (PB vs. PB: median of 11.3% vs. 3.7%; p = .0063 and BM vs. PB: 13.9% vs. 3.7%; p = .0006) (Figure 2b). Of note, PD-1 and CD39 were not co-expressed on TIGIT+CD73−CD8+ T cells in pAML or HDs (Supplement 7). Analysis by t-distributed stochastic neighbor embedding (tSNE) confirmed that expression of CD39 and PD-1 in AML patients largely overlapped with TIGIT+CD73−CD8+ T cells and clustered within the CD8+ EM and EMRA T-cell subsets (Figure 2c+d). TIGIT expression correlated positively with CD39 expression and negatively with CD73 on CD8+ T cells in the PB from patients with pAML (r = 0.7; p = .003 and r = 0.54; p = .001) (Supplement 5D and 6 C). In summary, in pAML a significant increase of two CD8+ T-cell populations was observable: the PD-1+TIGIT+CD73− and a CD39+TIGIT+CD73−CD8+ T-cell subpopulation.
Figure 2.
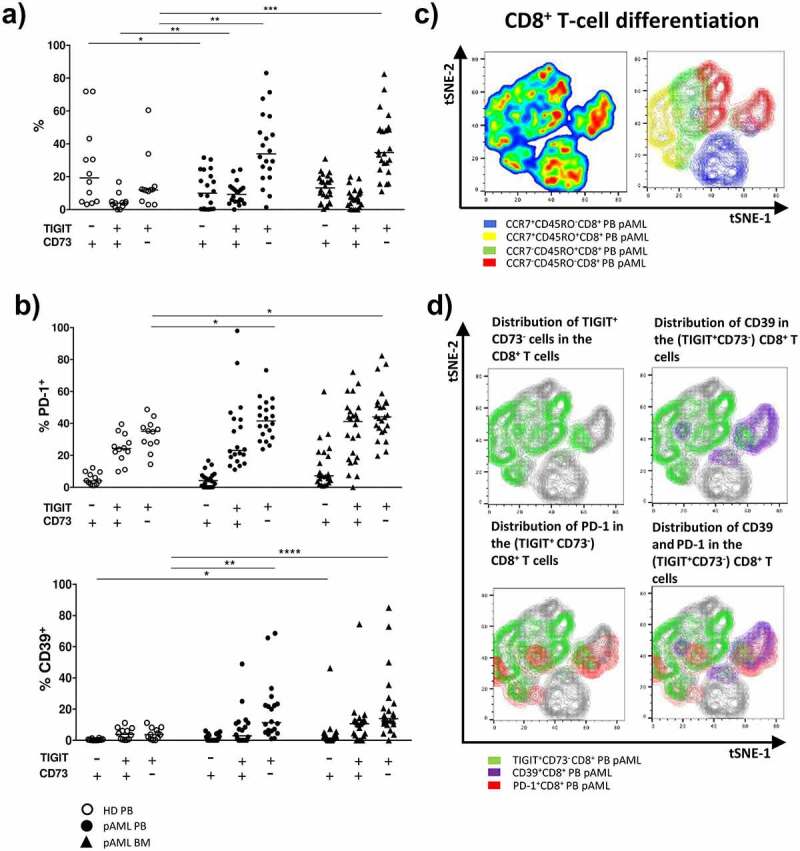
Increased expression of PD-1 and CD39 on TIGIT+CD73−CD8+ T cells in pAML
Flow cytometric analysis of the co-expression of PD-1 and CD39 with TIGIT and CD73 on CD8+ T cells was performed. (A) Summary data of the frequency of TIGIT± and CD73± CD8+ T-cell subsets in PB from healthy donors (HD PB, white circles, n = 12) and patients with newly diagnosed AML (pAML PB, black circles, n = 18), and bone marrow aspirates from pAML patients (pAML BM, black triangles, n = 24). (B) Summary data illustrating the frequency of PD-1+ and CD39+ cells on CD8+ T cells expressing TIGIT and/or CD73 from PB of HDs and pAML patients, and BM aspirates from pAML patients. (C) tSNE analysis showing a heat map of total CD8+ T cells from PB samples of five patients with pAML (left graph) and the position of CD8+ T-cell differentiation stages (blue = naïve; yellow = central memory; green = effector memory and red = terminal differentiated effector memory CD8+ T cells) on the tSNE map. (D) Distribution of TIGIT+CD73− cells (green overlay), PD-1+ cells (red overlay), and CD39+ cells (violet overlay) on the tSNE map of CD8+ T cells (gray). P values were obtained by ANOVA and Kruskal-Wallis test. *P < .05, **P < .01, ***P < .001.
PD-1+-, CD73– and CD39+CD8+ T cells are increased in PB and BM of patients with a relapse in comparison to newly diagnosed AML
As the expression of TIGIT, CD73, CD39, and PD-1 in pAML was altered in comparison to healthy controls, we set out to analyze their expression shortly after relapse and during stable remission. MCF was performed on CD8+ T cells isolated from patients in remission after intensive chemotherapy (lrAML PB: n = 10; BM: n = 10), and from patients with relapsed AML (rAML PB: n = 8; BM: n = 9) before the start of re-induction chemotherapy. In contrast to pAML the frequency of PD-1+CD8+ T cells was further increased in PB and BM from patients with rAML (PB: median of 33.6% vs. 20.3%; p = .027 and BM: median of 42.4% vs. 29.4%; p = .018) (Figure 3ab). Similar expression levels of TIGIT+ and CD39+ on CD8+ T cells were observed when we compared PB and BM from patients with rAML with samples from patients with pAML (Figure 3ab). The frequency of CD73+CD8+ T cells was further reduced in PB and BM from patients with rAML in comparison to patients with pAML (PB: CD73 median of 21.6% vs. 44.1%; p = .048 and BM: CD73 median of 12.8% vs. 32.5%; p = .028) (Figure 3a-b).
Figure 3.
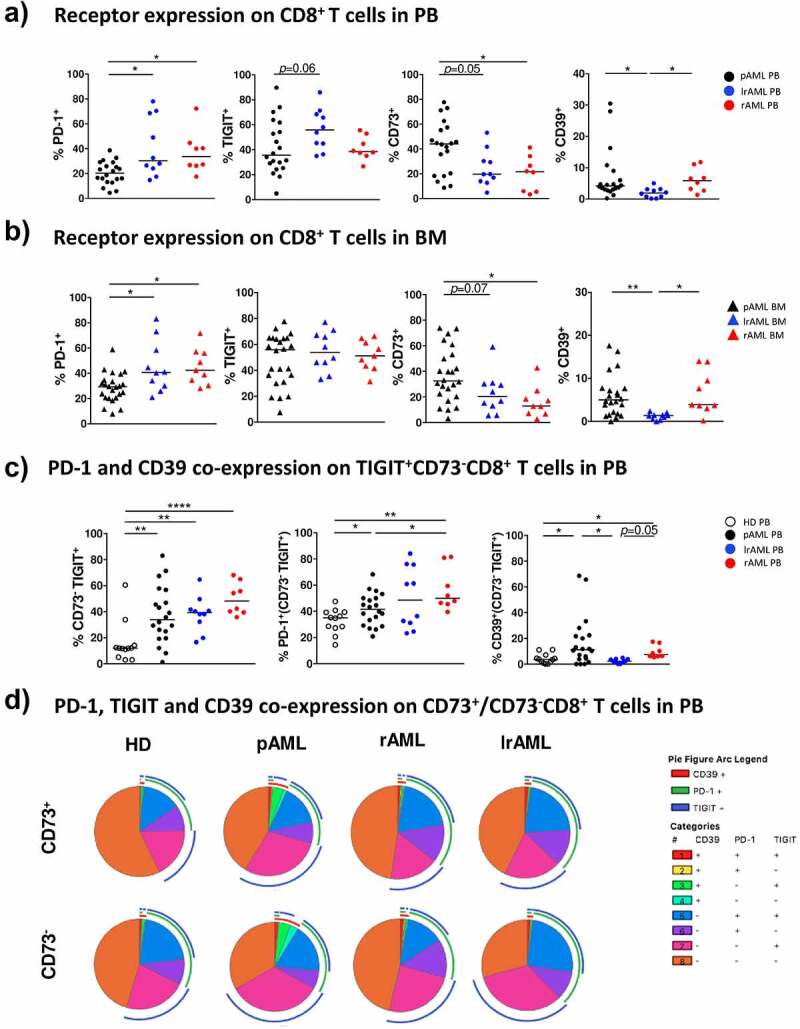
Comparison of the expression of TIGIT, PD-1, CD73 and CD39 on CD8+ T cells in pAML, rAML and lrAML
The expression of PD-1, TIGIT, CD73 and CD39 was analyzed on CD8+ T cells in PB (A) and/or BM samples (B) from patients with pAML (PB, black circles, n = 20; BM, black triangles, n = 24), lrAML (PB, blue circles, n = 10; BM, blue triangles, n = 10), and rAML (PB, red circles, n = 8, BM, red triangles, n = 9), and of healthy donors (HDs) (PB, white circles, n = 12). (C) Summary data are shown comparing the frequency of TIGIT+CD73−CD8+ T cells and the expression of PD-1 and CD39 on this population in PB from HDs, pAML, IrAML, and rAML patients. (D) Pie Charts showing the distribution of subsets expressing combinations of TIGIT, PD-1, and CD39 on CD73+ or CD73− CD8+ T cells from HDs, pAML, IrAML and rAML patients. P values were obtained by ANOVA and Kruskal-Wallis test. *P < .05, **P < .01, ***P < .001.
Next, we analyzed the co-expression of PD-1 and CD39 on the TIGIT+CD73−CD8+ T-cell subset in rAML. The frequency of PD-1+TIGIT+CD73−CD8+ T cells was further increased in PB from patients with rAML in comparison to patients with pAML and HDs (rAML vs. HD p = .0069; rAML vs. pAML p = .0420) (Figure 3c). Similar findings occurred in the BM of patients with rAML (data not shown). The CD39+TIGIT+CD73−CD8+ T-cell population in PB from patients with rAML was not different from pAML but increased in comparison to PB from HDs (p = .0312) (Figure 3c). As in pAML, TIGIT expression correlated with CD39 expression on CD8+ T cells in PB from patients with rAML (r = 0.8; p < .01) (Supplement 8B).
As in rAML, patients with AML in remission showed a significantly higher frequency of PD-1+CD8+ T cells in PB and BM than patients with pAML (PB: PD-1 median of 30.3% vs. 20.25%; p = .0482 and BM: PD-1 median of 40.74% vs. 29.4%; p = .0408) (Figure 3ab). The frequency of PD-1+CD8+ T cells in PB and BM from patients with lrAML was similar to that from patients with rAML (Figure 3ab). The TIGIT expression tended to be higher in PB from patients with lrAML in comparison to pAML (p = .06) (Figure 3a). In the BM, we observed similar levels of TIGIT expression in all three disease groups (Figure 3b). Patients with lrAML displayed lower frequencies of CD39+CD8+ T cells than patients with pAML or rAML, also CD73+CD8+ T cells were decreased in lrAML in comparison to patients with pAML (CD73 PB: 19.7% vs. 44.1%; p = .05 and BM 20.4% vs. 32.5%; p = .0671 and CD39 PB 1.92% vs. 4.2%; p = .013 and BM: 1.37% vs. 5.0%; p = .0023) (Figure 3ab). Strikingly, the frequency of CD39+TIGIT+CD73−CD8+ T cells in the PB of patients with lrAML did not differ from that observed in HDs, in contrast to the elevated frequencies seen in patients with pAML and rAML (rAML vs. lrAML p = .05 and pAML vs. lrAML p = .031) (Figure 3cd). Our data indicates that we have two distinct immunophenotypic CD8+ T-cell subpopulations in AML. The PD-1+TIGIT+CD73−CD8+ T cells persisted in lrAML whereas the CD39+TIGIT+CD73−CD8+ T-cell subpopulation was increased in pAML and rAML and then normalized in lrAML to the frequencies found in HDs.
Decreased expression of CD127 and the transcription factor TCF-1 in CD8+ T cells in peripheral blood and bone marrow of patients with AML
Expression of TCF-1 identifies antigen-experienced CD8+ T cells that retain the ability for self-renewal while producing differentiated effector cells.17 We analyzed TCF-1 expression in subsets of patients with pAML (PB, n = 7 and BM, n = 8), rAML (PB, n = 4 and BM, n = 4), and HDs (PB, n = 5) (Supplement 9A). The frequency of TCF-1+ cells was reduced in CD8+ T cells in PB and BM from patients with pAML compared to HDs (median of 54.0% vs. 78.1%; p = .03 and median of 34.2% vs. 78.1%; p = .0014) (Figure 4a). The reduced frequency of TCF-1+ cells was particularly prominent in the TIGIT+CD73−CD8+ T cells, with the greatest reduction observed in PB and BM of patients with pAML in comparison to HDs (median of 33.9% vs. 67.7%; p = .080 and median of 25.5% vs. 67.7%; p = .0261) (Figure 4b). Furthermore, expression of TCF-1 was inversely correlated with TIGIT expression in PB of patients with pAML (r = −0.87, p < .01) (Figure 4c).
Figure 4.
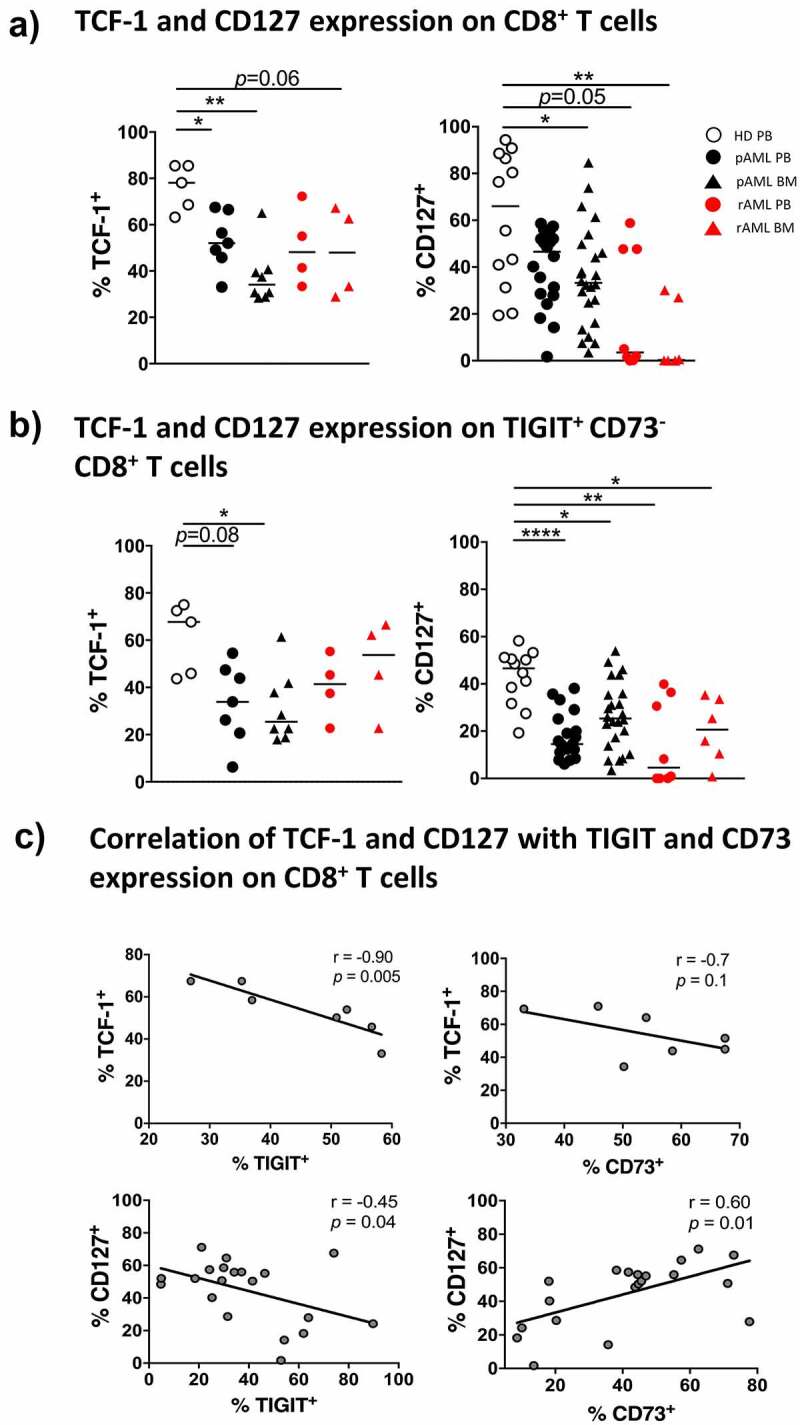
Reduced frequencies of TCF-1+- and CD127+ CD8+ T cells in pAML and rAML vs. HDs
The expression of TCF-1 and CD127 was analyzed on total CD8+ T cells (A) and TIGIT+CD73− CD8+ T cells (B) from PB and/or BM of HDs (white circles, n = 5), patients with pAML (PB, black circles, n = 7 and BM, black triangles, n = 8), and patients with rAML (PB, red circles, n = 4 and BM, red triangles, n = 4). P values were obtained by ANOVA and Kruskal-Wallis test. *P < .05, **P < .01, ***P < .001. (C) Correlative analysis of the expression of TCF-1 and CD127 with TIGIT and CD73 in PB from patients with pAML. Pearson’s test was used to test for correlations.
CD127 is expressed on long-living antigen-independent memory CD8+ T cells. Loss of CD127 expression is associated a diminished ability to form long-living memory cells.21 We therefore analyzed the expression of CD127 on CD8+ T cells of patients with pAML (PB, n = 20 and BM, n = 24), rAML (PB, n = 8 and BM, n = 6), and from HDs (PB, n = 12). The frequency of CD127+CD8+ T cells was significantly reduced in BM from patients with pAML compared to PB of HDs (median of 33.3% vs. 66.0%; p = 0.037, respectively) but not in PB of pAML patients (Figure 4a). TIGIT+CD73−CD8+ T cells were predominantly CD127− in PB and BM of patients with pAML in contrast to HDs (PB vs. PB: median of 14.5% vs. 46.6%; p < .0001 and BM vs. PB: median of 25.4% vs. 46.6%; p = .0110) (Figure 4b). Expression of CD127 also correlated with CD73 expression in pAML (r = 0.6; p = .01) (Figure 4c).
In the PB and BM from patients with relapsing AML, the frequency of CD127+CD8+ T cells was reduced in comparison to HDs and patients with pAML (p = .05, p = .0037) (Figure 4a). As in pAML, CD127+ cells were especially reduced in the TIGIT+CD73−CD8+ T-cell subset in PB and BM in patients with rAML in comparison to HDs (p = .0036 and p = .0388) (Figure 4b). However, although the frequency of TCF-1+CD8+ T cells was reduced in BM from patients with rAML compared to HDs (p = .0635) (Figure 4a), we observed no difference in the frequency of TCF-1+ cells in the TIGIT+CD73−CD8+ T cells in rAML or pAML (Figure 4b). Taken together, the frequency of TCF-1+ and CD127+CD8+ T cells was reduced in pAML and rAML. Moreover, we observed an inverse association between the expression of TCF-1 and with TIGIT, and a positive association between CD127 and CD73 on CD8+ T cells.
Increased expression of the transcription factor TOX in CD8+ T cells in peripheral blood and bone marrow from AML patients
To further evaluate the exhaustion state of the CD8+ T cells in AML, we analyzed the expression of the transcription factor TOX. Expression has been associated with loss of the capability for T-cell re-invigoration upon checkpoint blockade.22 Intranuclear TOX expression was assessed in CD8+ T cells of patients with pAML (PB, n = 14 and BM, n = 13), rAML (PB, n = 8 and BM, n = 6), and HDs (PB, n = 10) (Supplement 9A+B).
We detected a significantly increased frequency of CD8+ T cells expressing TOX in PB of patients with pAML compared to HDs (median of 47.9% vs. 26.2%; p = .0224) (Figure 5a). This upregulation of TOX was predominantly found in the TIGIT+CD73−CD8+ T-cell population in AML whereas in HDs no upregulation could be observed (PB vs. PB: 69.0% vs. 26.8%; p = .0152 (Figure 5a). Further co-expression analysis revealed an increased frequency of TOX+ cells in the PD-1+TIGIT+CD73− and the CD39+TIGIT+CD73−CD8+ T-cell subsets in PB from pAML patients compared to HDs (median of 24.1% vs. 12.2%; p = .0471 and median of 7.2% vs. 2.4%; p = .05) (Figure 5b). However, in BM from patients with pAML, the frequency of TOX+ cells was increased only in the CD39+TIGIT+CD73−CD8+ T-cell subset in comparison to HDs (median of 9.1% vs. 2.4%; p = .0415) (Figure 5b).
Figure 5.
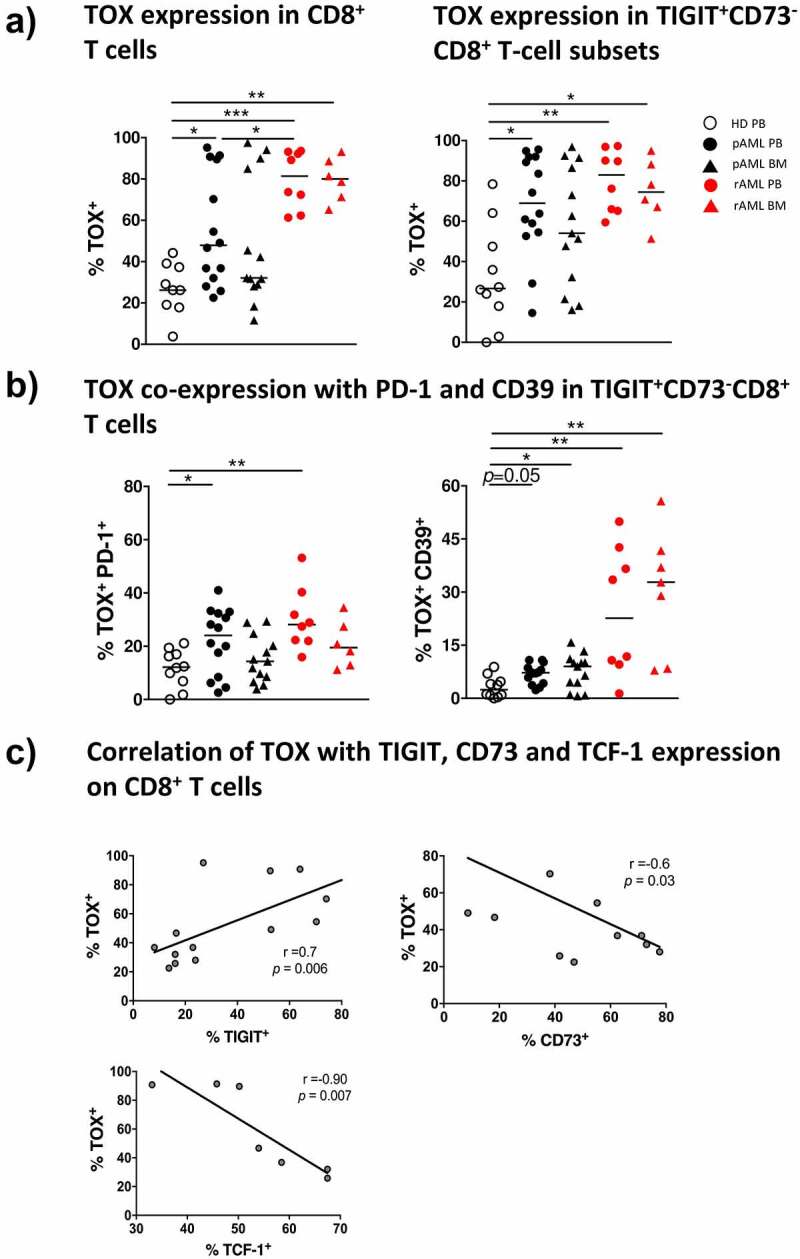
Increased TOX expression in pAML and rAML in comparison to HDs
The frequency of cells expressing TOX among (A) total CD8+ T cells and TIGIT+CD73−CD8+ T cells was analyzed by flow cytometry in PB and/or BM samples from healthy donors (white circles, n = 10), pAML patients (PB, black circles, n = 14; BM, black triangles, n = 13) and rAML patients (PB, red circles, n = 8; BM, red triangles, n = 8). (B) Summary data are shown for the co-expression of TOX with PD-1 or CD39 among TIGIT+CD73−CD8+ T cells. P values were obtained by ANOVA and Kruskal-Wallis test. *P < .05, **P < .01, ***P < .001. (C) Correlative analysis of the expression of TOX with that of TIGIT, CD73 and TCF-1 on CD8+ T cells in PB from patients with newly diagnosed AML. Pearson’s test was used to test for correlations.
In rAML, the frequency of TOX+CD8+ T cells further increased in PB and BM of the patients in contrast to HDs (median of 81.5% vs. 26.2%; p = .0008 and median of 80.5% vs. 26.2% p = .0039) (Figure 5a). At even higher levels than in pAML in rAML the frequency of TOX+ cells was increased in the TIGIT+CD73−CD8+ T-cell population in PB and BM in contrast to HDs (PB vs. PB: median of 83.0% vs. 26.8%; p = .0036 and BM vs. PB: median of 74.5% vs. 26.8%; p = .0278) (Figure 5a). TOX was dominantly increased in the CD39+TIGIT+CD73−CD8+ T-cell subsets in rAML in contrast to HDs (PB vs. PB: median of 22.7% vs. 2.4%; p = .0053 and BM vs. PB: CD39 median of 32.8% vs. 2.4% p = .0034) (Figure 5b). TOX correlated positively with expression of TIGIT (r = 0.7; p < .01), and negatively with CD73 (r = −0.6; p = .03) and TCF-1 (r = −0.9; p = <0.01) (Figure 5c). In conclusion, we observed an increased expression of TOX in the CD8+ T cells in active AML in comparison to HDs. Moreover, expression of TOX in CD8+ T cells was associated with the PD-1+TIGIT+CD73−CD8+- and CD39+TIGIT+CD73−CD8+ T-cell population.
Discussion
Persistent antigens in the tumor environment can promote T-cell exhaustion.4 Up to now, characterization of T cells in AML has yielded heterogeneous results with regard to whether immune exhaustion is characteristic of T cells in AML.23,24
Analysis of the differentiation status in our cohort confirmed that the frequency of CD8+ terminal differentiated (CD45R0−CCR7−) T cells was increased in the PB and BM regardless of the disease status. TIGIT+, CD39+ and CD73−CD8+ T cells were increased in the PB and BM of patients with pAML and rAML in comparison to HDs. Moreover, TIGIT+CD73−CD8+ T cells co-expressed PD-1 or CD39 in AML. During relapse, the PD-1+TIGIT+CD73−CD8+ T-cell subpopulations further increased and persisted after reaching stable disease remission while the frequency of CD39+TIGIT+CD73−CD8+ T cells returned to the levels found in HDs. CD8+ T cells especially the PD-1+- and CD39+TIGIT+CD73−CD8+ T-cell subsets in pAML and rAML exhibited further features of exhaustion as manifested by decreased expression of the surface molecule CD127 and increased intracellular expression of the transcription factors TOX combined with low levels of TCF-1. Correlation analysis of the multi-receptor expressing CD8+ T-cell subsets with blast counts, relapse or long-term remission as well as correlations with molecular or cytogenetic aberrations did not reach significant results due to the small numbers of patients, especially within the subgroups.
In agreement with other studies, we found that the frequency of PD-1+ cells was increased in patients during leukemia relapse, but also in remission.23 In pAML, however, we observed a significant elevation only for TIGIT on CD8+ T cells.6 TIGIT expression was explicitly related to the CD8+ effector memory T-cell subsets indicating that its expression is part of antigen-experience. TIGIT is expressed by dysfunctional T cells after chronic antigen stimulation in chronic infections and cancer.7,25 Regarding solid neoplasms, Chauvin et al. have demonstrated TIGIT upregulation on tumor antigen specific CD8+ T cells in the PB and tumor tissue of patients with advanced melanoma.25 Functionally, inhibition of the TIGIT or its ligands poliovirus receptor (PVR) and poliovirus receptor-related 2 (PVRL2) in T cells significantly enhanced in vitro cytotoxicity, and prolonged survival in AML mouse model in vivo.5 Importantly, high expression of PVR and PVRL2 was associated with a poorer prognosis in two independent AML patient cohorts, implying immune evasion in these patients.5 TIGIT+CD8+ T cells produced reduced levels of effector cytokines but showed a high proliferation and a high susceptibility to apoptosis, which were partially reverted by TIGIT knockdown.6 These results suggest that the TIGIT pathway is prominent in newly diagnosed AML, whereas multiple suppressive pathways contribute to leukemia relapse.
The expression of CD73 was significantly reduced on CD8+ T cells in PB and BM from patients with pAML in all four differentiation stages: naïve-, central memory-, effector memory- and terminally differentiated effector memory CD8+ T cells. These data are in line with a previous report and indicate that the reduced frequency of CD73+ T cells in AML is not only explained by variances in the differentiation status of cells.26 In oncology CD73 has been identified as a novel target of interest since its expression was shown to be upregulated in response to oncogenic signals, e.g. hypoxic microenvironment.27 High CD73 expression was associated with poor prognosis in the majority of these studies,28–30 but with a better clinical outcome in others.31,32 In our study CD73−CD8+ T cells showed characteristics of exhaustion (e.g. increased expression of PD-1, TIGIT, CD39 and TOX). Functionally, Kong et al. showed that CD73−CD8+ T cells displayed features of exhaustion such as a reduced capacity for cytokine production.26 These data support the hypothesis that loss of CD73 on CD8+ T cells in AML is associated with T-cell dysfunction and exhaustion.
Tumor-specific CD8+ T cells express high levels of CD39 in human cancer. These findings were also reported by independent groups for solid tumors and hematological malignancies.33–35 It has been demonstrated that T-cell receptor engagement in the presence of IL-6 and TGF-β induces CD39 upregulation.36 Moreover, CD39+CD8+ T cells were found not only to be enriched in the tumor microenvironment, but also in invaded lymph nodes and metastases compared to healthy tissues. Expression of CD39 on CD8+ T cells was associated with increased co-expression of PD-1, TIM-3, and LAG-3 as well as with decreased production of TNF, IL-2 and IFN-γ thus generating a characteristic phenotype of dysfunctional CD8+ T cells.12,37 In previous studies it has been demonstrated that inhibition of CD39 expressed by CD8+, CD4+ effector T cells and NK cells enhance proliferation, effector functions including anti-tumor cytotoxicity, and promote conversion from could to “hot” tumors with high immune infiltrates. Moreover, inhibition of CD39 on macrophages and myeloid-derived suppressor cells increased the inflammatory cytokine secretion and maturation of antigen-presenting cells.38,39 The reduced expression of CD39 in remission might be explained by an altered immune milieu, decreased inflammatory cytokines, reduced oxidative stress and hypoxia in remission.39
One of the most important features of T-cell dysfunction seem to be the co-expression of multiple inhibitory receptors.40 We observed increased frequencies of the PD-1+TIGIT+CD73−CD8+- and CD39+TIGIT+CD73−CD8+ T-cell subsets in PB and BM from patients with newly diagnosed and relapsed AML. These data strengthen the hypothesis that inhibitory immune pathways might be heterogeneric and specific for different disease stages. Co-expression of immune-suppressive targets e.g. PD-1, CD39 and TIGIT also provide a rationale for combinatorial targeting of different pathways to create effective leukemia therapeutics.25
Moreover, TIGIT and PD-1 are being evaluated as therapeutic targets in clinical trials or have already been approved for solid and hematologic malignancies.25,41,42 To date, there are several clinical trials investigating the potential of TIGIT alone or in combination with PD-1/PDL-1 inhibition to treat various advanced or metastatic solid malignancies.42 In addition, a specific CD39 inhibitor significantly enhanced the anti-tumor activity of anti-PD-1 and anti-CTLA-4 monoclonal antibodies in a NK cell and IFN-γ dependent manner in a lung metastasis models.14
CD127 and TCF-1 expression is associated with generation of CD8+ memory T-cell responses and long-term maintenance of an effective protective immunity.15 Overexpression of TCF-1 diminishes the expression of coinhibitory receptors e.g. PD-1.43 TCF-1lowPD-1+CD8+ T cells have been recently identified as a terminally differentiated exhausted T-cell subset. In chronic viral infection it has been demonstrated that only TCF-1+PD-1lowCD8+ T cells can be re-invigorated by blockade of the PD-1/PD-L1.44 Moreover, ectopic TCF-1 expression promotes the generation of a stem-like program in exhausted CD8+ T cells, thereby enhancing viral and tumor immunity.45
In our study the expression of TCF-1 correlated negatively with TOX expression in CD8+ T cells. In contrast to the reduced TCF-1 levels, we observed increased expression of TOX in CD8+ T cells in the PB and BM of patients with AML. TOX+ cells were significantly enriched in TIGIT+CD73−CD39+CD8+ T cells in pAML, and even more so in relapsed AML. Our findings underscore the reports that expression of TOX is induced in terminal exhausted CD8+ T cells. Overexpression of TOX boosts expression of PD-1 and additional inhibitory receptors and suppresses effector functions.18,19 These findings indicate that TOX is necessary for preventing over-activation of antigen experienced CD8+ T cells by induction of exhaustion.18 Expression of TOX also hampered re-activation of exhausted memory CD8+ T cells upon coinhibitory receptor blockade and led to fixation of the dysfunctional phenotype.19,46 As a central regulator of T-cell exhaustion, TOX is of great interest as a therapeutic target in immuno-oncology. Seo et al. showed that expression of TOX correlated with PD-1 expression and diminished effector cytokine production. Moreover, the partial knockdown of TOX improved the functionality of CAR-T cells directed against a tumor model, while Khan et al. showed that heterozygous deletion of TOX strengthens the anti-tumor T-cell responses.19,47
Conclusions
In our study CD8+ T cells in the PB and BM from patients with AML exhibit a key signature defined as TIGIT+CD73−CD8+ T cells. These cells can be further subdivided into two populations, the PD-1+TIGIT+CD73−CD8+- and the CD39+TIGIT+CD73−CD8+ T-cell subset. The frequency of PD-1+TIGIT+CD73−CD8+ T cells increased over progression of the disease and persisted in remission whereas the CD39+TIGIT+CD73−CD8+ T-cell population was normalized in remission to levels similar to HDs. These results provide a rationale to combine different immunotherapeutical approaches in AML. In our study, TOX expression was associated with TIGIT and CD73 expression on CD8+ T cells. TOX might regulate the expression of TIGIT, CD39, PD-1 and TCF-1 in the course of chronic antigen stimulation and thus provide an additional potential target to improve T-cell mediated cytotoxicity in AML.
Supplementary Material
Acknowledgments
We thank all our patients for their trust, understanding, and willingness to provide their blood samples for our
research. FB thank Elias Brauneck for reviewing the manuscript.
Funding Statement
FB was supported by the University Cancer Center Hamburg Research fellowshipand the Mildred Scheel Nachwuchszentrum Hamburg FB is funded by the Roggenbuck Stiftung 1672/100). JSzW and FH are funded by the DFG SFB1328.JSzW, CA and NW are funded by the DFG SFB841. AR is funded by the DFG, accession number RI 2952/1-1 Preliminary data were presented as abstracts at the 62nd ASH Annual Meeting. AR is funded by the DFG, accession number RI 2952/1-1.
Disclosure of potential conflicts of interest
FB: Travel grant Daiichi Sankyo, Servier, Novartis; advisory board by Jazz. GmbH, Daiichi Sankyo. WF: Membership on an entity’s board of directors or advisory Amgen, ARIAD/Incucyte, Pfizer, Novartis, Jazz Pharmaceuticals, Morphosys, Abbvie, Celgene, TEVA GmbH; patents and royalities Amgen; other support for meeting attendance Amgen, Gilead, Jazz Pharmaceuticals, Servier, Daiichi Sankyo; research funding Amgen, Pfizer; Travel grant, TEVA GmbH, Gilead Inc and Jazz. GmbH; research funding: Pfizer Inc, Amgen.CB: consulting or advisory Lilly/imClone, Merck, Sanofi, Bayer, GSO, AOK Health insurance; research funding Abbvie, ADC Therapeutics, Agile Therapeutics, Alexion Therapeutics, Amgen, Apellis Pharmaceuticals, Astellas Pharma, AstraZeneca, Boehringer Ingelheim, Celgene, Daiichi Sankyo, Gilead Sciences, Incucyte, Karyopharm Therapeutics, Millenium, MSD, Novartis and Roche, travel grants: Merck, Sanofi, Pfizer, Bristol-Meyer Squibb. The remaining authors declare that they have no conflict of interest.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding authors on
reasonable request.
Authors’ contributions
FB designed the research study, performed the experiments, analyzed the data, and wrote the manuscript. RW performed the experiments. NW discussed the data. FH, ET, and AR reviewed the data and the manuscript. GV collected the samples. JW and CB reviewed the manuscript. JSzW, CA and WF conceived the concept, oversaw the interpretation and presentation of the data and wrote the manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
The study was approved the local ethics board of the Ärztekammer Hamburg (PV3469). Informed written
consent was obtained from all patients.
Consent for publication
Not applicable.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website
References
- 1.Lamble AJ, Lind EF.. Targeting the immune microenvironment in acute myeloid leukemia: a focus on T cell immunity. Front Oncol. 2018;8:213. doi: 10.3389/fonc.2018.00213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lichtenegger FS, Krupka C, Haubner S, Köhnke T, Subklewe M. Recent developments in immunotherapy of acute myeloid leukemia. J Hematol Oncol. 2017;10(1):142. doi: 10.1186/s13045-017-0505-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Williams BA, Law A, Hunyadkurti J, Desilets S, Leyton JV, Keating A. Antibody therapies for acute myeloid leukemia: unconjugated, toxin-conjugated, radio-conjugated and multivalent formats. J Clin Med. 2019;8(8):8. doi: 10.3390/jcm8081261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wherry EJ, Ha SJ, Kaech SM, Haining WN, Sarkar S, Kalia V, Subramaniam S, Blattman JN, Barber DL, Ahmed R, et al. Molecular signature of CD8+ T cell exhaustion during chronic viral infection. Immunity. 2007;27(4):670–13. doi: 10.1016/j.immuni.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 5.Stamm H, Klingler F, Grossjohann EM, Muschhammer J, Vettorazzi E, Heuser M, Mock U, Thol F, Vohwinkel G, Latuske E, et al. Immune checkpoints PVR and PVRL2 are prognostic markers in AML and their blockade represents a new therapeutic option. Oncogene. 2018;37(39):5269–5280. doi: 10.1038/s41388-018-0288-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kong Y, Zhu L, Schell TD, Zhang J, Claxton DF, Ehmann WC, Rybka WB, George MR, Zeng H, Zheng H, et al. T-cell immunoglobulin and ITIM domain (TIGIT) associates with CD8(+) T-cell exhaustion and poor clinical outcome in AML patients. Clin Cancer Res. 2016;22(12):3057–3066. doi: 10.1158/1078-0432.CCR-15-2626. [DOI] [PubMed] [Google Scholar]
- 7.Ackermann C, Smits M, Woost R, Eberhard JM, Peine S, Kummer S, Marget M, Kuntzen T, Kwok WW, Lohse AW, et al. HCV-specific CD4+ T cells of patients with acute and chronic HCV infection display high expression of TIGIT and other co-inhibitory molecules. Sci Rep. 2019;9(1):10624. doi: 10.1038/s41598-019-47024-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Allard D, Allard B, Gaudreau PO, Chrobak P, Stagg J. CD73-adenosine: a next-generation target in immuno-oncology. Immunotherapy-Uk. 2016;8(2):145–163. doi: 10.2217/imt.15.106. [DOI] [PubMed] [Google Scholar]
- 9.Jiang T, Xu XF, Qiao M, Li X, Zhao C, Zhou F, Gao G, Wu F, Chen X, Su C, et al. Comprehensive evaluation of NT5E/CD73 expression and its prognostic significance in distinct types of cancers. BMC Cancer. 2018;18(1). ARTN 267. doi: 10.1186/s12885-018-4073-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bastid J, Regairaz A, Bonnefoy N, Déjou C, Giustiniani J, Laheurte C, Cochaud S, Laprevotte E, Funck-Brentano E, Hemon P, et al. Inhibition of CD39 enzymatic function at the surface of tumor cells alleviates their immunosuppressive activity. Cancer Immunol Res. 2015;3(3):254–265. doi: 10.1158/2326-6066.Cir-14-0018. [DOI] [PubMed] [Google Scholar]
- 11.Toth I, Le AQ, Hartjen P, Thomssen A, Matzat V, Lehmann C, Scheurich C, Beisel C, Busch P, Degen O, et al. Decreased frequency of CD73(+) CD8(+) T cells of HIV-infected patients correlates with immune activation and T cell exhaustion. J Leukocyte Biol. 2013;94(4):551–561. doi: 10.1189/jlb.0113018. [DOI] [PubMed] [Google Scholar]
- 12.Duhen T, Duhen R, Montler R, Moses J, Moudgil T, De Miranda NF, Goodall CP, Blair TC, Fox BA, McDermott JE, et al. Co-expression of CD39 and CD103 identifies tumor-reactive CD8 T cells in human solid tumors. Nat Commun. 2018;9(1). ARTN 2724. doi: 10.1038/s41467-018-05072-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mohme M, Schliffke S, Maire CL, Rünger A, Glau L, Mende KC, Matschke J, Gehbauer C, Akyüz N, Zapf S, et al. Immunophenotyping of newly diagnosed and recurrent glioblastoma defines distinct immune exhaustion profiles in peripheral and tumor-infiltrating lymphocytes. Clinical Cancer Research. 2018;24(17):4187–4200. doi: 10.1158/1078-0432.Ccr-17-2617. [DOI] [PubMed] [Google Scholar]
- 14.Zhang HY, Vijayan D, Li XY, Robson SC, Geetha N, Teng MWL, Smyth MJ. The role of NK cells and CD39 in the immunological control of tumor metastases. Oncoimmunology ARTN e1593809. 2019;8(6):e1593809. doi: 10.1080/2162402X.2019.1593809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wieland D, Kemming J, Schuch A, Emmerich F, Knolle P, Neumann-Haefelin C, Held W, Zehn D, Hofmann M, Thimme R, et al. TCF1(+) hepatitis C virus-specific CD8(+) T cells are maintained after cessation of chronic antigen stimulation. Nat Commun. 2017;8(1):15050. doi: 10.1038/ncomms15050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Renkema KR, Huggins MA, Da Silva HB, Knutson TP, Henzler CM, Hamilton SE. KLRG1(+) memory CD8 T cells combine properties of short-lived effectors and long-lived memory. Journal of Immunology. 2020;205(4):1059–1069. doi: 10.4049/jimmunol.1901512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kratchmarov R, Magun AM, Reiner SL. TCF1 expression marks self-renewing human CD8(+) T cells. Blood Adv. 2018;2(14):1685–1690. doi: 10.1182/bloodadvances.2018016279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Scott AC, Dundar F, Zumbo P, Chandran SS, Klebanoff CA, Shakiba M, Trivedi P, Menocal L, Appleby H, Camara S, et al. TOX is a critical regulator of tumour-specific T cell differentiation. Nature. 2019;571(7764):270-+. doi: 10.1038/s41586-019-1324-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Khan O, Giles JR, McDonald S, Manne S, Ngiow SF, Patel KP, Werner MT, Huang AC, Alexander KA, Wu JE, et al. TOX transcriptionally and epigenetically programs CD8(+) T cell exhaustion. Nature. 2019;571(7764):211-+. doi: 10.1038/s41586-019-1325-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bono MR, Fernandez D, Flores-Santibanez F, Rosemblatt M, Sauma D. CD73 and CD39 ectonucleotidases in T cell differentiation: beyond immunosuppression. FEBS Lett. 2015;589(22):3454–3460. doi: 10.1016/j.febslet.2015.07.027. [DOI] [PubMed] [Google Scholar]
- 21.Huster KM, Busch V, Schiemann M, Linkemann K, Kerksiek KM, Wagner H, Busch DH. Selective expression of IL-7 receptor on memory T cells identifies early CD40L-dependent generation of distinct CD8(+) memory T cell subsets. P Natl Acad Sci USA. 2004;101(15):5610–5615. doi: 10.1073/pnas.0308054101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim K, Park S, Park SY, Kim G, Park SM, Cho J-W, Kim DH, Park YM, Koh YW, Kim HR, et al. Single-cell transcriptome analysis reveals TOX as a promoting factor for T cell exhaustion and a predictor for anti-PD-1 responses in human cancer. Genome Med. 2020;12(1). ARTN 22. doi: 10.1186/s13073-020-00722-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schnorfeil FM, Lichtenegger FS, Emmerig K, Schlueter M, Neitz JS, Draenert R, Hiddemann W, Subklewe M. T cells are functionally not impaired in AML: increased PD-1 expression is only seen at time of relapse and correlates with a shift towards the memory T cell compartment. J Hematol Oncol. 2015;8(1). ARTN 93. doi: 10.1186/s13045-015-0189-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Williams P, Basu S, Garcia-Manero G, Hourigan CS, Oetjen KA, Cortes JE, Ravandi F, Jabbour EJ, Al‐Hamal Z, Konopleva M, et al. The distribution of T-cell subsets and the expression of immune checkpoint receptors and ligands in patients with newly diagnosed and relapsed acute myeloid leukemia. Cancer. 2019;125(9):1470–1481. doi: 10.1002/cncr.31896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chauvin JM, Pagliano O, Fourcade J, Sun Z, Wang H, Sander C, Kirkwood JM, Chen THT, Maurer M, Korman AJ, et al. TIGIT and PD-1 impair tumor antigen-specific CD8(+) T cells in melanoma patients. J Clin Invest. 2015;125(5):2046–2058. doi: 10.1172/Jci80445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kong YX, Jia B, Zhao CC, Claxton DF, Sharma A, Annageldiyev C, Fotos JS, Zeng H, Paulson RF, Prabhu KS, et al. Downregulation of CD73 associates with T cell exhaustion in AML patients. J Hematol Oncol. 2019;12(1). ARTN 40. doi: 10.1186/s13045-019-0728-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Soleimani A, Farshchi HK, Mirzavi F, Zamani P, Ghaderi A, Amini Y, Khorrami S, Mashayekhi K, Jaafari MR. The therapeutic potential of targeting CD73 and CD73-derived adenosine in melanoma. Biochimie. 2020;176:21–30. doi: 10.1016/j.biochi.2020.06.001. [DOI] [PubMed] [Google Scholar]
- 28.Ren ZH, Lin CZ, Cao W, Yang R, Lu W, Liu Z-Q, Chen Y-M, Yang X, Tian Z, Wang L-Z, et al. CD73 is associated with poor prognosis in HNSCC. Oncotarget. 2016;7(38):61690–61702. doi: 10.18632/oncotarget.11435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Leclerc BG, Charlebois R, Chouinard G, Allard B, Pommey S, Saad F, Stagg J. CD73 expression is an independent prognostic factor in prostate cancer. Clinical Cancer Research. 2016;22(1):158–166. doi: 10.1158/1078-0432.Ccr-15-1181. [DOI] [PubMed] [Google Scholar]
- 30.Gaudreau PO, Allard B, Turcotte M, Stagg J. CD73-adenosine reduces immune responses and survival in ovarian cancer patients. Oncoimmunology. 2016;5(5):e1127496. doi: 10.1080/2162402X.2015.1127496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Inoue Y, Yoshimura K, Kurabe N, Kahyo T, Kawase A, Tanahashi M, Ogawa H, Inui N, Funai K, Shinmura K, et al. Prognostic impact of CD73 and A2A adenosine receptor expression in non-small-cell lung cancer. Oncotarget. 2017;8(5):8738–8751. doi: 10.18632/oncotarget.14434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oh HK, Sin JI, Choi J, Park SH, Lee TS, Choi YS. Overexpression of CD73 in epithelial ovarian carcinoma is associated with better prognosis, lower stage, better differentiation and lower regulatory T cell infiltration. J Gynecol Oncol. 2012;23(4):274–281. doi: 10.3802/jgo.2012.23.4.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cai XY, Wang XF, Li J, Dong J-N, Liu J-Q, Li N-P, Yun B, Xia R-L, Qin J, Sun Y-H, et al. High expression of CD39 in gastric cancer reduces patient outcome following radical resection. Oncol Lett. 2016;12(5):4080–4086. doi: 10.3892/ol.2016.5189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kunzli BM, Bernlochner MI, Rath S, Käser S, Csizmadia E, Enjyoji K, Cowan P, d’Apice A, Dwyer K, Rosenberg R, et al. Impact of CD39 and purinergic signalling on the growth and metastasis of colorectal cancer. Purinergic Signal. 2011;7(2):231–241. doi: 10.1007/s11302-011-9228-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vaisitti T, Arruga F, Guerra G, Deaglio S. Ectonucleotidases in blood malignancies: a tale of surface markers and therapeutic targets. Front Immunol. 2019;10. ARTN 2301. doi: 10.3389/fimmu.2019.02301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Canale FP, Ramello MC, Nunez N, Furlan CLA, Bossio SN, Serrán MG, Boari JT, Del Castillo A, Ledesma M, Sedlik C, et al. CD39 expression defines cell exhaustion in tumor-infiltrating CD8(+) T cells. Cancer Res. 2018;78(1):115–128. doi: 10.1158/0008-5472.Can-16-2684. [DOI] [PubMed] [Google Scholar]
- 37.Thelen M, Lechner A, Wennhold K, Von Bergwelt-baildon M, Schlößer HA. CD39 expression defines cell exhaustion in tumor-infiltrating CD8(+) T cells—letter. Cancer Res. 2018;78(17):5173–5174. doi: 10.1158/0008-5472.Can-18-0873. [DOI] [PubMed] [Google Scholar]
- 38.Moesta AK, Li XY, Smyth MJ. Targeting CD39 in cancer. Nat Rev Immunol. 2020;20(12):739–755. doi: 10.1038/s41577-020-0376-4. [DOI] [PubMed] [Google Scholar]
- 39.Allard D, Allard B, Stagg J. On the mechanism of anti-CD39 immune checkpoint therapy. J Immunother Cancer ARTN e000186. 2020;8(1):e000186. doi: 10.1136/jitc-2019-000186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang Z, Liu S, Zhang B, Qiao L, Zhang Y, Zhang Y. T cell dysfunction and exhaustion in cancer. Front Cell Dev Biol. 2020;8:17. doi: 10.3389/fcell.2020.00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xin YJ, Hodge JP, Oliva C, Neftelinov ST, Hubbard-Lucey VM, Tang J. Trends in clinical development for PD-1/PD-L1 inhibitors. Nat Rev Drug Discov [published Online First: 2020/03/05]. 2020;19(3):163–164. doi: 10.1038/d41573-019-00182-w. [DOI] [PubMed] [Google Scholar]
- 42.Qin S, Xu LP, Yi M, Yu S, Wu K, Luo S. Novel immune checkpoint targets: moving beyond PD-1 and CTLA-4. Mol Cancer. 2019;18(1). doi: 10.1186/s12943-019-1091-2. ARTN 155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang YF, Hu JJ, Li YD, Xiao M, Wang H, Tian Q, Li Z, Tang J, Hu L, Tan Y, et al. The transcription factor TCF1 preserves the effector function of exhausted CD8 T cells during chronic viral infection. Front Immunol. 2019;10. ARTN 169. doi: 10.3389/fimmu.2019.00169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Utzschneider DT, Charmoy M, Chennupati V, Pousse L, Ferreira DP, Calderon-Copete S, Danilo M, Alfei F, Hofmann M, Wieland D, et al. T cell factor 1-expressing memory-like CD8(+) T cells sustain the immune response to chronic viral infections. Immunity. 2016;45(2):415–427. doi: 10.1016/j.immuni.2016.07.021. [DOI] [PubMed] [Google Scholar]
- 45.Shan Q, Hu SE, Chen X, Danahy DB, Badovinac VP, Zang C, Xue HH. Ectopic Tcf1 expression instills a stem-like program in exhausted CD8(+) T cells to enhance viral and tumor immunity. Cell Mol Immunol. 2020. doi: 10.1038/s41423-020-0436-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mann TH, Kaech SM. CD8(+) T CELLS Tick-TOX, it’s time for T cell exhaustion. Nat Immunol. 2019;20(9):1092–1094. doi: 10.1038/s41590-019-0478-y. [DOI] [PubMed] [Google Scholar]
- 47.Seo H, Chen J, Gonzalez-Avalos E, Samaniego-Castruita D, Das A, Wang YH, López-Moyado IF, Georges RO, Zhang W, Onodera A, et al. TOX and TOX2 transcription factors cooperate with NR4A transcription factors to impose CD8+ T cell exhaustion. P Natl Acad Sci USA. 2019;116(39):19761. doi: 10.1073/pnas.1914896116. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding authors on
reasonable request.


