ABSTRACT
Burkholderia pseudomallei is a tier 1 select agent that is associated with laboratory-acquired melioidosis, with international guidelines recommending isolate handling within a class II biosafety cabinet (BSC) in a biosafety level 3 (BSL3) facility. In low-resource settings, this may not be practical; therefore, we aimed to assess the risk of laboratory-acquired melioidosis during routine work. Prior exposure to the organism was determined with a questionnaire and concomitant serology. Of 30 laboratory scientists handling B. pseudomallei on 1,267 occasions outside a biosafety cabinet, no infections were documented and all participants remained seronegative. Additionally, we performed controlled environmental air sampling during 78 laboratory handling events, including plate opening, oxidase testing, and McFarland suspension creation. None of the experiments demonstrated aerosolization of the organism. This study suggests the risk of laboratory-acquired melioidosis is low. However, individual laboratories will need to undertake a risk assessment, including melioidosis endemicity, availability of resources for containment, the nature of routine handling to be undertaken, and the presence of predisposing risk factors for infection in the staff concerned. Additionally, laboratories should take region-specific guidelines into consideration. Further research is required to better inform on the overall risk of infection in the microbiology laboratory.
KEYWORDS: B. pseudomallei, biosafety cabinet, biosafety level, laboratory safety, laboratory acquired, melioidosis
INTRODUCTION
Burkholderia pseudomallei is the causative agent of melioidosis, an infection most commonly acquired through inhalation, inoculation, or ingestion, with a mortality rate of approximately 15% in Australia (1). It is a soil-dwelling bacterium endemic to Far North Queensland, the Northern Territory, and parts of Western Australia (1).
B. pseudomallei is classified by the U.S. Centers for Disease Control and Prevention as a tier 1 select agent with the ability to pose a significant public health threat (2). Additionally, there have been two reported cases of laboratory-acquired melioidosis to date, and, as such, an international consensus was published regarding prevention and management of occupational exposure and infection (2–4). These guidelines suggest handling of the organism in a biosafety level 3 (BSL3) facility within a class II biological safety cabinet (BSC). This recommendation is not necessarily practical in all regions, particularly low-resource settings. Where these guidelines were not applied, a reported 70 years of combined experience from the front line has revealed no laboratory-acquired infections (5). In Australia, B. pseudomallei is categorized as a risk group 2 organism requiring BSL2 containment, with the stipulation that a BSC should be used for organisms transmissible via the respiratory route or if handling may result in significant risk to humans from production of infectious aerosols (6).
While multiple laboratories in Queensland handle B. pseudomallei isolates, only the Queensland State Melioidosis Reference Laboratory, a BSL2 facility in Townsville, has a specific occupational safety procedure. Notably, this laboratory is located in a region of endemicity, and only staff with known risk factors for melioidosis are required to handle the organism within a class II BSC. These risk factors include, but are not limited to, diabetes mellitus, chronic kidney disease, chronic lung disease, and immunocompromise. The region serviced by this laboratory has a previously reported seropositive rate of 2.5% among asymptomatic blood donors, with the greater Far North Queensland area reporting 5.7% (7, 8).
Taking into account this significant divergence in practice, the authors sought to assess the potential risk to staff regarding both intended and accidental handling of B. pseudomallei isolates outside a class II BSC. The two features of the risk assessment were seroprevalence of staff compared to healthy individuals in the regions of endemicity and environmental air sampling during routine laboratory organism handling to determine aerosolization risk. This research was approved by the Royal Brisbane & Women’s Ethics Committee (LNR/2020/QRBW/61126).
MATERIALS AND METHODS
Seroprevalence.
Staff members who had previously handled B. pseudomallei isolates completed a questionnaire designed to assess an estimated total exposure over the preceding 10-year period. A handling event was classified as any contact with the bacterial isolate on an open laboratory bench in the context of organism identification, including Gram stain preparation, oxidase, catalase, and McFarland suspension creation. These included both intentional and accidental handling in the setting of unknown organism identification. Additionally, occupational exposure, defined as a needle stick injury or any other inoculating injury, aerosol inhalation of a culture, or ingestion, was also assessed. All participants underwent serological investigation for detection of B. pseudomallei serum antibodies. Two assays were performed to improve overall sensitivity. First, an indirect hemagglutination assay (IHA) for detection of total antibody was performed. For interpretation, titers of ≤1:5 were considered negative; titers of 1:10 to 1:20 were considered borderline, indicating past or present infection or a nonspecific reaction; and titers of ≥1:40 indicated past or present infection with B. pseudomallei (9). Second, an enzyme immunoassay (EIA) specific for detection of immunoglobulin G (IgG) was performed, with results considered positive, borderline, or negative depending on enzyme immunoassay units (EIU), as defined by Ashdown et al. (9).
Bioaerosol detection.
For detection of B. pseudomallei aerosols, Western Australia Culture Collection (WACC) isolate 201 Burkholderia thailandensis was used as a substitute for safety purposes. This substitution was considered likely to be bioequivalent due to previously reported size and volume data between species (10). Air sampling was performed using the MicroBio MB1 (Cantium Scientific, Kent, United Kingdom) single-stage sieve impactor at a flow rate of 100 liters/min (Fig. 1). A 220-hole sieve plate was used with a 55-mm tryptic soy agar (TSA) collection plate. Data from a biological efficiency validation report demonstrated >98% efficiency (efficiency [%] = air sampler recovery/nebulizer concentration × 100) at 51% relative humidity and 22°C using Staphylococcus epidermidis ATCC 14990, performed in a 1.82-m3 chamber (personal communication). B. thailandensis streak-plate cultures were created by subculturing from a stock culture using a 10-μl loop and incubated for 24, 48, and 72 h. Aerosol-generating experiments, which occurred in triplicate or quintuplicate, included plate opening and 30 s of continuous tilting to mimic organism inspection at 10-cm distance to the air sampler head; plate opening and tilting, oxidase reaction, catalase reaction, 0.5 McFarland suspension creation, susceptibility lawn plating, and mass spectrometer (MS) target spot creation were all performed at a 30-cm distance to the air sampler head. Continuous air sampling occurred throughout the experiment and for 1 min after the completion to maximize detection of potential aerosols. Each experiment occurred within an enclosed room, within a class II BSC without the laminar airflow engaged. Between each experiment, the BSC was meticulously cleaned with 80% ethanol and vented for 5 min to remove any potential airborne contamination (11). TSA collection plates were subsequently incubated aerobically at 35°C for 5 days, with plates reviewed on days 1, 2, and 5. Quantification of all organism growth, including environmental organisms, was calculated per the manufacturer’s instructions (12). All organisms were assessed according to colony morphology and benchtop oxidase testing. Further identification was performed via additional biochemical analysis and Vitek MS (bioMérieux, Marcy l’Etoile, France).
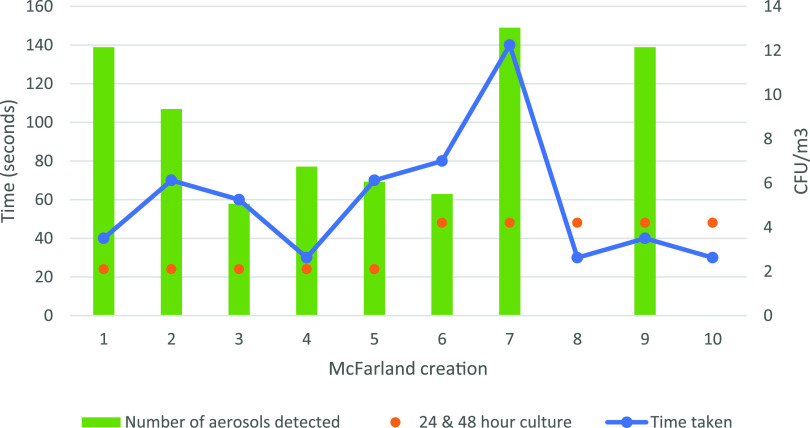
FIG 1.
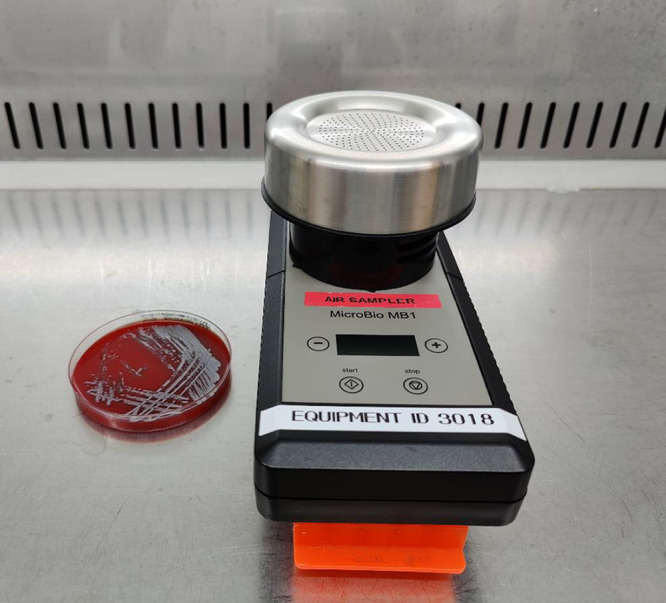
Air sampler 10 cm above an open B. thailandensis culture plate.
RESULTS
Seroprevalence.
In total, 30 participants across 4 laboratories were enrolled in this study. Laboratories in regions of endemicity included Townsville, Mackay, and Rockhampton, with 12, 5, and 2 participants, respectively, while the Brisbane laboratory accounted for 11 participants. Twenty-two (73%) were female, and 25 (83%) participants had previously lived or were currently living in a region of melioidosis endemicity. There were no previously diagnosed or treated melioidosis infections among the cohort. Seventeen (57%) reported a history of prior potential occupational exposure, although no prophylaxis had been prescribed, suggesting low-risk exposure in the context of routine B. pseudomallei handling, including benchtop oxidase testing and McFarland standard creation for automated identification or susceptibility testing. The estimated total number of handling events from all participants over a 10-year period was 1,419. During this time, approximately 300 culture-confirmed melioidosis cases were diagnosed in Queensland. However, these handling events include all additional work performed through the reference laboratory. Exposure to B. pseudomallei from intentional routine work outside a BSC accounted for approximately 923 (65%) events involving 17 (57%) participants. Unintentional handling outside a BSC accounted for 344 (24%) events, and intentional handling inside a BSC was 152 (11%). Total handling events outside a BSC were 1,267 (89%). Serology performed on each participant included combined indirect hemagglutination assay (IHA) and enzyme immunoassay (EIA) IgG, all of which were negative. This equals a 0% seropositive prevalence among laboratory staff (95% confidence interval, 0 to 12%).
Bioaerosol detection.
In total, 78 bioaerosol detection experiments were performed, including 33 with 24 and 48 h of organism growth and 12 with 72 h of growth. Table 1 demonstrates the type of handling, organism growth in hours, air sampler distance from the plate, and total number of environmental organisms detected. Additionally, 5 bioaerosol sampling controls were performed to assess the level of environmental contamination between experiments. The mean overall environmental organism growth per plate was 18 CFU/m3 ± 17 standard deviations (SD) (range, 0 to 55 CFU/m3). All growth data are represented in Fig. 2. When creating a 0.5 McFarland suspension for susceptibility testing, the time taken to create the suspension had limited effect on the amount of aerosol generated (Fig. 3).
TABLE 1.
Environmental bioaerosols detected per experiment
| Expt | Distance to sampler (cm) | Growth (h) | Bioaerosol detected (CFU/m3) in replicate no.: |
||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |||
| Plate opening | 10 | 24 | 0 | 34 | 7 | ||
| 48 | 20 | 34 | 20 | ||||
| 72 | 14 | 55 | 0 | ||||
| 30 | 24 | 7 | 20 | 20 | 7 | 34 | |
| 48 | 34 | 20 | 20 | 7 | 14 | ||
| 72 | 20 | 7 | 14 | ||||
| McFarland creation | 30 | 24 | 12 | 9 | 5 | 7 | 6 |
| 48 | 6 | 13 | 0 | 12 | 0 | ||
| 72 | 27 | 41 | 20 | ||||
| Catalase | 30 | 24 | 0 | 20 | 0 | 20 | 7 |
| 48 | 7 | 0 | 14 | 14 | 27 | ||
| 72 | 34 | 20 | 41 | ||||
| Oxidase | 30 | 24 | 7 | 0 | 0 | 0 | 0 |
| 48 | 20 | 20 | 14 | 0 | 27 | ||
| Susceptibility lawn | 30 | 24 | 0 | 0 | 20 | 20 | 14 |
| 48 | 0 | 0 | 7 | 7 | 14 | ||
| MS spot | 30 | 24 | 20 | 48 | 7 | 27 | 14 |
| 48 | 41 | 7 | 27 | 20 | 20 | ||
| Control | 30 | 41 | 10 | 26 | 20 | 26 | |
FIG 2.
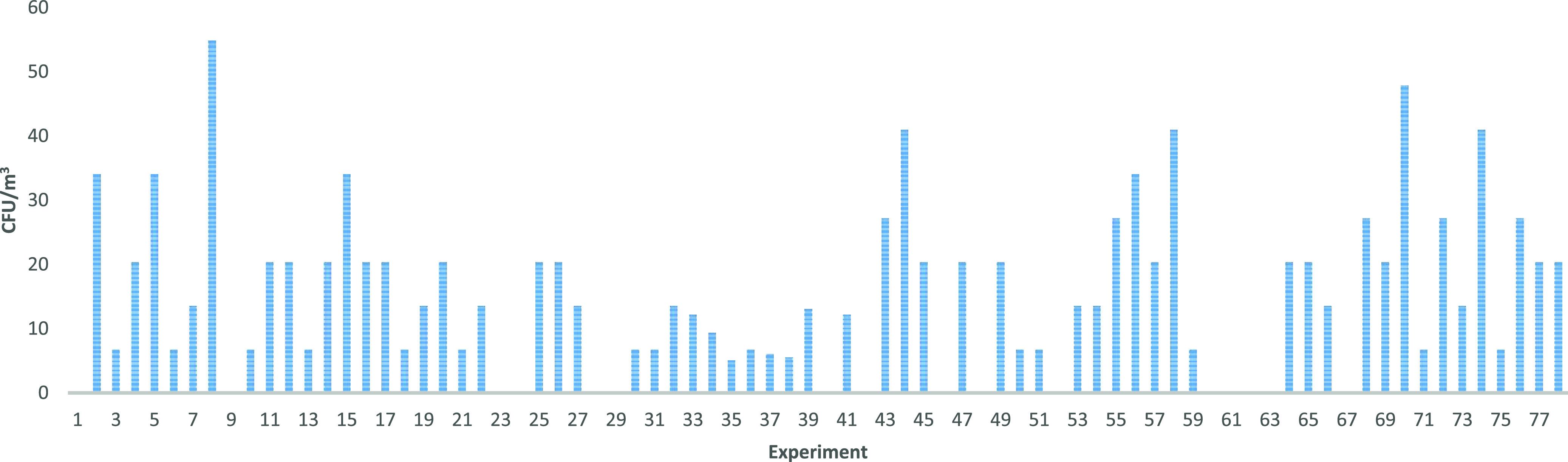
Total number of environmental organisms detected for each experiment performed.
FIG 3.
Time taken to create a 0.5 McFarland suspension and associated environmental aerosols detected.
Approximately 12,000 liters of environmental air was sampled during the course of the 78 handling experiments. While numerous environmental organisms were detected, no TSA experiment plates demonstrated growth of B. thailandensis. Therefore, the rate of B. thailandensis detection was <1 CFU/m3 per experiment. Across all experiments, the total detectable B. thailandensis organism number approximated to <9 × 10−5 CFU/m3.
DISCUSSION
This study aimed to determine the risk to laboratory staff when handling B. pseudomallei cultured isolates outside a class II BSC. There is no current evidence regarding laboratory aerosolization of B. pseudomallei while performing standard laboratory handling. Therefore, we aimed to provide insight regarding potential risks to staff by combining the best available methods for identification of prior exposure, in the form of B. pseudomallei-specific serology coupled with organism aerosolization dynamics, to describe the means and risk of acquisition.
Currently, there is no standard for environmental air sampling for the specific detection of B. pseudomallei. Factors that are likely to play a role in aerosolized organism detection include ambient temperature, relative humidity, and airflow, which, in a laboratory, are likely to be affected by both ventilation and human traffic (11, 13). Considering the potential for incomplete detection of all B. pseudomallei bioaerosols generated using the methods described above, it would be pertinent to estimate the risk to a laboratory scientist in this context. As a comparison to a scientist working with an isolate on a benchtop, the average ventilation rate of a seated car passenger or driver is 11.8 and 12.3 liters/min, respectively (14). Therefore, the average scientist may inhale one cubic meter of air within 81 to 85 min. Assuming each laboratory handling procedure results in 1 to 5 CFU B. pseudomallei/m3, a scientist working with one isolate would potentially inhale 1.25 × 10−2 to 6.25 × 10−2 CFU/min. However, our results suggest a significantly lower number of aerosols generated per procedure and, therefore, an inhalation exposure of <1.6 × 10−4 CFU/min.
The infectious dose for human melioidosis is unknown. Animal models have assessed the implications of inoculum concentration, route of infection, and organism-specific virulence (15–17). Healthy nonhuman primate inhalation models using highly virulent and less virulent strains demonstrate a lethal dose ranging from 1.14 × 102 to 1.53 × 103 CFU and an infectious nonlethal dose as high as 6.2 × 103 CFU (17, 18). These data suggest that even when handling a highly virulent B. pseudomallei strain in the laboratory, the likelihood of infection is low. However, it is important to continue to maintain good laboratory practices, which include laboratory-specific training and annual competence assessment, use of personal protective equipment, including gown and gloves, and the use of a class II BSC for laboratory activities associated with aerosolization, such as centrifugation (2, 19).
These results are supported by the substantial handling of B. pseudomallei isolates outside a BSC with no proven seroconversion or laboratory-acquired infection. To our knowledge, there are no reported cases of laboratory-acquired melioidosis in Queensland. Additionally, the Townsville laboratory has directly identified over 400 clinical isolates in the preceding 30 years without incident.
There are several limitations to this study. The participant sample size was small, leading to imprecise quantification of the risk. Handling events were evaluated through a questionnaire and, therefore, may be affected by recall bias. However, this does not take into account the potential for multiple exposures per isolate, including culture review on consecutive days, identification, and susceptibility testing. Therefore, the burden of exposure is likely far greater than reported. The risk outcome was assessed by serology, which may not be 100% sensitive or specific, with previous local IHA and EIA IgG test characteristics for diagnosis of infection revealing a sensitivity of 74% and 90%, respectively (9). However, compared to the previously reported seroprevalence data using a single method, our study included a secondary assay to improve sensitivity with the combination of the IHA and IgG EIA (8, 9, 20). Finally, environmental air sampling was only performed using one air sampler type. Additional experiments with multiple samplers would create a more robust understanding of aerosolization risks during standard laboratory handling.
Conclusions.
The data provided in this study suggest that current local guidelines that do not mandate a BSL3 facility are both practical and safe. In addition, these findings provide some reassurance to laboratory staff in regions of B. pseudomallei endemicity that have limited facilities for containment. This study suggests a low risk of laboratory-acquired melioidosis when handling B. pseudomallei on an open bench. However, individual laboratories will need to undertake a risk assessment, including melioidosis endemicity, availability of resources for containment, the nature of routine handling to be undertaken, and the presence of predisposing risk factors for infection in the staff concerned. Additionally, laboratories should take region-specific guidelines into consideration. Further research regarding the use of personal protective equipment, such as masks and eyewear, would be of additional benefit to understanding risk mitigation in low-resource settings.
ACKNOWLEDGMENTS
We thank all staff who participated in this study.
We have no conflicts of interest to disclose.
Funding for this research was provided by the Pathology Queensland Study & Education Committee.
Contributor Information
Ian Gassiep, Email: i.gassiep@uq.edu.au.
Patricia J. Simner, Johns Hopkins
REFERENCES
- 1.Gassiep I, Armstrong M, Norton R. 2020. Human melioidosis. Clin Microbiol Rev 33:e00006-19. 10.1128/CMR.00006-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peacock SJ, Schweizer HP, Dance DA, Smith TL, Gee JE, Wuthiekanun V, DeShazer D, Steinmetz I, Tan P, Currie BJ. 2008. Management of accidental laboratory exposure to Burkholderia pseudomallei and B. mallei. Emerg Infect Dis 14:e2. 10.3201/eid1407.071501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Green RN, Tuffnell PG. 1968. Laboratory acquired melioidosis. Am J Med 44:599–605. 10.1016/0002-9343(68)90060-0. [DOI] [PubMed] [Google Scholar]
- 4.Schlech WF, Turchik JB, Westlake RE, Klein GC, Band JD, Weaver RE. 1981. Laboratory-acquired infection with Pseudomonas pseudomallei (melioidosis). N Engl J Med 305:1133–1135. 10.1056/NEJM198111053051907. [DOI] [PubMed] [Google Scholar]
- 5.Dance DA, Limmathurotsakul D, Currie BJ. 2017. Burkholderia pseudomallei: challenges for the clinical microbiology laboratory-a response from the front line. J Clin Microbiol 55:980–982. 10.1128/JCM.02378-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Joint Standards Australia/Standards New Zealand Committee. 2010. Safety in Laboratories Standards Australia, Australia. Joint Standards Australia/Standards New Zealand Committee, Sydney, Australia. [Google Scholar]
- 7.Lazzaroni SM, Barnes JL, Williams NL, Govan BL, Norton RE, LaBrooy JT, Ketheesan N. 2008. Seropositivity to Burkholderia pseudomallei does not reflect the development of cell-mediated immunity. Trans Royal Soc Trop Med Hyg 102:S66–S70. 10.1016/S0035-9203(08)70018-X. [DOI] [PubMed] [Google Scholar]
- 8.Ashdown LR, Guard RW. 1984. The prevalence of human melioidosis in Northern Queensland. Am J Trop Med Hyg 33:474–478. 10.4269/ajtmh.1984.33.474. [DOI] [PubMed] [Google Scholar]
- 9.Ashdown LR, Johnson RW, Koehler JM, Cooney CA. 1989. Enzyme-linked immunosorbent assay for the diagnosis of clinical and subclinical melioidosis. J Infect Dis 160:253–260. 10.1093/infdis/160.2.253. [DOI] [PubMed] [Google Scholar]
- 10.Sagripanti J-L, Carrera M, Robertson J, Levy A, Inglis TJJ. 2011. Size distribution and buoyant density of Burkholderia pseudomallei. Arch Microbiol 193:69–75. 10.1007/s00203-010-0649-6. [DOI] [PubMed] [Google Scholar]
- 11.Pottage T, Jhutty A, Parks SR, Walker JT, Bennett AM. 2014. Quantification of microbial aerosol generation during standard laboratory procedures. Appl Biosaf 19:124–131. 10.1177/153567601401900303. [DOI] [Google Scholar]
- 12.Cantium Scientific Ltd. 2018. MicroBio MB1 operating manual, 5th ed. Cantium Scientific Ltd., Kent, United Kingdom. https://www.cantiumscientific.com/wp-content/uploads/MicroBio-MB1-Operating-Manual-Rev-5.pdf. [Google Scholar]
- 13.Griffiths WD, Stewart IW. 1999. Peformance of bioaerosol samplers used by the UK biotechnology industry. J Aerosol Sci 30:1029–1040. 10.1016/S0021-8502(98)00783-6. [DOI] [Google Scholar]
- 14.Zuurbier M, Hoek G, Hazel P, Brunekreef B. 2009. Minute ventilation of cyclists, car and bus passengers: an experimental study. Environ Health 8:48. 10.1186/1476-069X-8-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barnes JL, Ketheesan N. 2005. Route of infection in melioidosis. Emerg Infect Dis 11:638–639. 10.3201/eid1104.041051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nelson M, Dean RE, Salguero FJ, Taylor C, Pearce PC, Simpson AJH, Lever MS. 2011. Development of an acute model of inhalational melioidosis in the common marmoset (Callithrix jacchus). Int J Exp Pathol 92:428–435. 10.1111/j.1365-2613.2011.00791.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Trevino SR, Dankmeyer JL, Fetterer DP, Klimko CP, Raymond JLW, Moreau AM, Soffler C, Waag DM, Worsham PL, Amemiya K, Ruiz SI, Cote CK, Krakauer T. 2021. Comparative virulence of three different strains of Burkholderia pseudomallei in an aerosol non-human primate model. PLoS Negl Trop Dis 15:e0009125. 10.1371/journal.pntd.0009125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yeager JJ, Facemire P, Dabisch PA, Robinson CG, Nyakiti D, Beck K, Baker R, Pitt MLM. 2012. Natural history of inhalation melioidosis in rhesus macaques (Macaca mulatta) and African green monkeys (Chlorocebus aethiops). Infect Immun 80:3332–3340. 10.1128/IAI.00675-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization. 2020. Laboratory biosafety manual, 4th ed. World Health Organization, Geneva, Switzerland. [Google Scholar]
- 20.Kunakorn M, Boonma P, Khupulsup K, Petchclai B. 1990. Enzyme-linked immunosorbent assay for immunoglobulin M specific antibody for the diagnosis of melioidosis. J Clin Microbiol 28:1249–1253. 10.1128/JCM.28.6.1249-1253.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]