Abstract
The PRAPARE (Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences) tool is an instrument that has been used to assess social determinants of health within community health centers in the US. We sought to examine the association between PRAPARE scores and getting tested for and testing positive with the SARS-CoV-2 virus. We used medical record data collected from a community health center in the US between March-August 2020. Employing logistic regression analyzes, we explored the association between demographic factors, history of screening positive for depression, and PRAPARE scores and patients’ odds of getting tested and testing positive for COVID-19. While variables such as ethnicity mirrored similar findings from other sources, we found the PRAPARE score to be associated with increased odds of being tested for COVID-19; however, it was not significantly associated with testing positive. These findings can help health care workers and health educators craft messages to explain screening protocols for communicable diseases, such as COVID-19, to best reach vulnerable populations.
Keywords: PRAPARE, Community health center, COVID-19, Social determinants of health
Introduction
Since their inception in 1965, community health centers across the U.S. have served to reduce the burden of health disparities that routinely affect racial and ethnic minorities, those with low-income, and the uninsured [1]. Today, community health centers serve as the medical home to over 20 million Americans, providing affordable, comprehensive care to the disadvantaged regardless of their insurance status [2, 3]. America’s community health centers continue to seek innovations for public health issues and illness prevention as they provide a direct pathway to equitable healthcare for all in the U.S. [1].
In order to increase understanding of the disparities observed among the 5% of the U.S. population that are served annually by community health centers [1], the implementation of the PRAPARE (Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences) data tool has been used to determine how social determinants of health affect short-term, intermediate, and long-term health outcomes. Social determinants of health are considered any social factor that influences health and health outcomes and are measured via the PRAPARE instrument by using five domains: housing status, language, employment, transportation, stress, and income [4]. These variables help create a path for evaluating the upstream factors affecting health and health behaviors [5, 6] that have been used in prior research to explore health outcomes among vulnerable populations, including infants from birth until 1 year of age [7]. Understanding patients’ social determinants of health allows those who work at community health centers to better serve the needs of their patients by creating meaningful and well-rounded strategies for behavior change and providing access to important resources.
The coronavirus disease 2019 (COVID-19) pandemic reached the United States in early 2020, and on March 11, 2020, the World Health Organization established COVID-19 as a global pandemic [8]. Within the U.S., outbreaks were often seen within certain high density, socioeconomically disadvantaged geographic locations, and most attributed to travel [9, 10]. The U.S. instructed people to use face masks, social confinement, quarantine, and social distancing initiatives to reduce the spread of COVID-19 [11]. Although these critical prevention measures were used during previous infectious disease outbreaks [12], the effectiveness and compliance of these measures were not well understood across all populations [13], and preventive measures (e.g., wearing a mask or face covering) were politicized due to a polarized political climate at the time of the pandemic [14]. Therefore, some have argued that these strategies had adverse health effects on the mental wellness, social engagement, and overall wellbeing of marginalized and disparate communities [15]. Although some have provided guidelines for testing strategies of vulnerable populations via community health centers [16], little research has examined COVID-19 testing and rates of those who tested positive for the virus by these community health centers. Recent research indicates that low socioeconomic status populations, minority groups [17, 18], and those with underlying health conditions were at higher risk for contracting COVID-19 during the beginning of the pandemic [19]; however, it is unknown if risk factors were related to the rates at which these populations were tested for COVID-19. Thus, it is increasingly important for researchers to examine underlying factors, such as social determinants of health, that may be associated with seeking a test for COVID-19. To do this, we sought to explore the relationship between social determinants of health, measured by the PRAPARE tool, and getting tested for SARS-CoV-2. Furthermore, we examined the relationship between the PRAPARE tool and receiving a positive COVID-19 test result.
Methods
Participants
This retrospective study used a cross-sectional analysis of patients’ (N = 2,121) electronic medical records from a community health center that served as the primary medical home for vulnerable populations including a majority of non-English speaking, low income, disparate groups including those who identified as Hispanic and Native Hawaiian Pacific Islanders (NHPIs). At the time of the study, this area was home to over 15,000 NHPIs, most of whom were Marshallese Islander, which was the largest colonization of Marshallese Islanders outside of the Marshall Islands as well as a large Hispanic population. Care at this location was heavily advertised in English, Spanish, and Marshallese to effectively inform the diverse population of the COVID-19 related services being provided.
Protocol
All data were collected between March 18 and August 31, 2020. Electronic medical record data were assessed to determine if patients at the community health center were screened for COVID-19 (included if one’s test returned positive or negative), or if they were seen for a non-COVID-19 related visit. Patients seen at this time either attended the normal clinic for any visits unrelated to acute illness, or they were tested for COVID-19 at an outside free walk/drive-up COVID-19 testing center. The external testing centers served all patients who presented symptoms for COVID-19 testing, specifically due to possible or confirmed exposure to the disease or due to evidence of any acute respiratory or gastrointestinal symptoms. All patients who visited the community health center during this time (n = 2,121) were invited to complete the PRAPARE tool during the in-take process to better inform their healthcare provider of any crucial information that could benefit or hinder the effectiveness of care provided beyond the typical demographic and personal health information gathered in healthcare settings. Participants were informed that completion of the instrument was voluntary and informed consent was obtained before completing the PRAPARE tool. The PRAPARE instrument was administered by different staff at multiple points of contact including intake, after rooming patients/during triage, and during the visit with the provider. While there was a paper form available in English and Spanish, responses were ascertained through conversation, recorded, and transcribed into the electronic medical record [20]. A template was configured into the electronic medical record which produced the final score. The response rate of patients who completed all items within the PRAPARE tool was 76.3%, with 1,618 participants included in the final analysis. The current study was exempt from review by the [blinded for review] Institutional Review Board.
Measures
Demographic information used in this study included sex, age, race, ethnicity, marital status, and employment status. Race and ethnicity were categorized as non-Hispanic White, non-Hispanic NHPI, Hispanic, and other (which included African American, Asian, American Indian and Alaskan Native, and mixed race/ethnicity). Additional information used from the medical records included patient depression screening history (yes/no). Mental health disorders were measured by the patients’ response to a depression screener, which was measured at different points of care when patients were assessed on complementary information (e.g., PHQ-2, PHQ-9, and domestic violence screening) in addition to the screening questions of the PRAPARE tool. This item a was included due to the relationship between social and emotional risk factors [21].
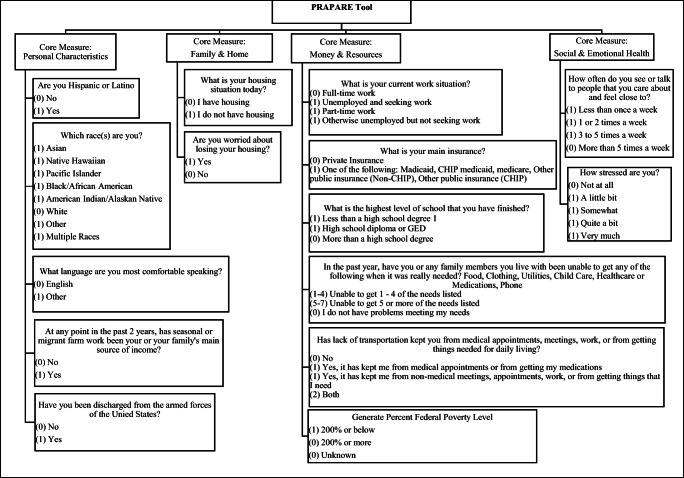
The 15-item PRAPARE tool measures social determinants of health by calculating a score based on participants’ risks [20]. Scores range from 0 to 22, with 0 indicating the participant reported no social determinant of health risks and 22 indicating the participant reported all measured risks [22]. The core domains measured in the PRAPARE include personal characteristics, family and home, finances and resources, and social and emotional health [20]. Areas measured within personal characteristics domain include ethnicity, race, and primary language spoken. The domain family and home are measured using housing status and stability. The finances and resources available to the patient are measured via employment status, insurance status, education level, income level, material security (given 1 point for each unmet need), and transportation need. Finally, the social and emotional health domain uses two items regarding social integration and stress that are measured via 5-point Likert-scales [20]. See Figure 1 for item wording and scores for each response. All PRAPARE items came from the national PRAPARE social determinants of health assessment protocol, developed and owned by the National Association of Community Health Centers, in partnership with the Association of Asian Pacific Community Health Organization, the Oregon Primary Care Association, and the Institute for Alternative Futures. For more information, visit www.nachc.org/prapare.
Figure 1.
PRAPARE Measures
Testing criteria required to receive a COVID-19 test at the time data were collected was defined as a patient who presented possible or known exposure to someone who tested positive for COVID-19 or who met Centers for Disease Control and Prevention’s (CDC’s) guidelines for testing. COVID-19 positivity was defined as a positive result produced from a polymerase chain reaction laboratory test. Positive results are defined as the detection of viral RNA congruent with SARS Cov2 (also referred to as COVID-19) [23].
Data Analysis
Because the community health center from where data were collected chose to exclude all pediatric patients from reported COVID-19-related reports, data were delimited to those 18 years of age and older. While across the nation, the average age of those most heavily affected by COVID-19 were 65 years old of age and older [24], this particular community health center served a robust population of those between 18–29 years; thus, this age category served as the reference group for all analyzes. Basic frequencies of demographics were reported, and then demographic variables were compared between those who were/were not tested for COVID-19 and those who did/did not test positive for COVID-19 using chi-square analyzes (i.e., sex, race/ethnicity, age categories, marital status, employment status, and depression screening) and independent t-tests (i.e., PRAPARE score). Next, multivariate logistic regression analyzes were used to estimate the association between predictive variables (e.g., demographic factors, history of a positive depression screening, and the PRAPARE tool score) and two outcome variables (received a COVID-19 test and tested positive for COVID-19). Only those who were tested for COVID-19 (n = 629) were included in the analyzes pertaining to those who tested positive. Adjusted odds ratio (aOR) and 95% Confidence Intervals (95% CI) were used to report findings from the logistic regressions. Statistical significance was evaluated based on an α of .05. Variability explained by each model was reported using Negelkerke R2. All analyzes were conducted using IBM SPSS 26 Software [25].
Results
The average age of the patients within the sample (n = 1,618) was 38 years (SD = 14.5), and 41% were male. Overall, 43.4% of the sample were non-Hispanic White, 3.3% were NHPI, and 44% were Hispanic. Among the sample, 36.9% were unemployed at the time of their visit to the community health center, and 46.5% were partnered or married. Within this study, 89.5% of the sample did not have a history of screening positive for depression. Among all the entire sample, 98.6% indicated at least one social risk, while only 1.4% respondents demonstrated no current risks, responses resulting in a score of zero (scores ranged from 0–15). Among those who were tested for COVID-19, 97.9% indicated at least one social risk (scores ranged from 0–13). See Table 1 for full demographic information.
Table 1.
Patient Demographics: Testing (n = 1,618) and Testing Positive (n = 629) for COVID
| Tested for COVID-19 | Tested Positive for COVID-19 | ||||
|---|---|---|---|---|---|
| N = 629 | N = 93 | ||||
| Variable | N (%) | N (%) | p-value | N (%) | p-value |
| Sex | .260 | .020 | |||
| Female | 954 (59) | 360 (57.2) | 43 (46.2) | ||
| Male | 664 (41) | 269 (42.8) | 50 (53.8) | ||
| Race/Ethnicity | .001 | .001 | |||
| Non-Hispanic White | 703 (43.4) | 294 (46.7) | 16 (17.2) | ||
| Native Hawaiian Pacific Islander | 54 (3.3) | 36 (5.7) | 15 (16.1) | ||
| Hispanic | 712 (44) | 257 (40.9) | 58 (62.4) | ||
| Other | 149 (9.2) | 42 (6.7) | 4 (4.3) | ||
| Age | .001 | .085 | |||
| 18-29 | 543 (33.6) | 233 (37.0) | 41 (44.1) | ||
| 30-39 | 396 (24.5) | 138 (21.9) | 22 (23.7) | ||
| 40-49 | 290 (17.9) | 105 (16.7) | 18 (19.4) | ||
| 50-59 | 232 (14.3) | 75 (11.9) | 7 (7.5) | ||
| 60+ | 157 (9.7) | 78 (12.4) | 5 (5.4) | ||
| Marital Status | .001 | .830 | |||
| Single | 866 (53.5) | 304 (48.3) | 49 (47.3) | ||
| Partnered or Married | 752 (46.5) | 325 (51.7) | 44 (52.7) | ||
| Employment Status | .001 | .388 | |||
| Employed | 1021 (63.1) | 476 (75.7) | 68 (73.1) | ||
| Unemployed | 597 (36.9) | 153 (24.3) | 25 (26.9) | ||
| Positive Depression Screening | .001 | .260 | |||
| No | 1445 (89.5) | 595 (94.6) | 89 (95.7) | ||
| Yes | 170 (10.5) | 34 (5.4) | 4 (4.3) | ||
| PRAPARE Score (m, sd) | (4.99, 2.71) | 4.24 (2.44) | .001 | 4.81 (2.14) | .008 |
Note. Tested positive for COVID-19 only included the 629 patients who were tested
COVID-19 Testing
Chi-square analyzes indicated there was a significant relationship between being tested for COVID-19 and race/ethnicity, with most patients who were tested identifying as non-Hispanic white (46.7%) or Hispanic (44%; Χ2 [3, N = 1,618] = 29.6, p < .001). Age was also found to have significant differences between the proportion of patients tested for COVID-19 (Χ2 [4, N = 1,618] = 19.2, p < .001); the majority of patients tested were between 18–29 (37%) and 30–-39 (21.9%) years of age. Overall, 51.7% were partnered or married (Χ2 [1, N = 1,618] = 11.2, p < .001), and 75% of those who visited the clinic to be tested for COVID-19 were employed (Χ2 [1, N = 1,618] = 69.9, p < .001). Most (94.6%) had never screened positive for depression (Χ2 [1, N = 1,618] = 28.5, p < .001), and the average PRAPARE score was 4.24 (SD = 2.44) out of 22. Those who visited the clinic and were not tested for COVID-19 (M = 5.46, SD = 2.77) had a significantly higher PRAPARE score than those who were tested for COVID-19 (M = 4.24, SD = 2.44; t[1458] = −9.24, p < .001).
When included in the regression model together, variables associated with being tested for COVID-19 among the community health center patients included age, with those 30–39 years of age having a higher odds of getting tested for COVID-19 when compared to the referent group of 18–29 year-olds (1.52 [95% CI = 1.13, 2.04]). Also, those between 40–49 (aOR = 1.48, 95% CI = 1.07, 2.04) and 50–59 (aOR = 1.51; 95% CI = 1.06, 2.16) years had significantly higher odds of being tested for COVID-19 when compared to those between 18–29 years of age. Those categorized as “other race/ethnicity” (aOR = 1.55, 95% CI = 1.02, 2.33) were also found to have significantly higher odds of being tested for COVID-19 compared to non-Hispanic whites. Patients who were unemployed at the time of their visit were at increased odds of being tested for a COVID-19 (aOR = 2.61, 95% CI = 2.04, 3.35) than their employed counterparts. Also, patients with a history of screening positive for depression had higher odds of being tested for COVID-19 (aOR = 1.77; 95% CI = 1.07, 2.04) than those without such diagnosis. Further, for each one-point increase in one’s PRAPARE scores, their odds of being tested for COVID-19 increased by 1.17 (95% CI = 1.11, 1.23) times. Finally, those who reported being married or partnered, were significantly less likely to undergo COVID-19 testing (aOR = 0.69, 95% CI = 0.55, 0.86) than their single counterparts, and those who identified as NHPI were significantly less likely to be tested for COVID-19 (aOR = 0.26, 95% CI = 0.14, 0.48) than non-Hispanic whites. Overall, the model explained 16.5% of the variability for being tested for COVID-19.
Testing Positive for COVID-19
When examining differences between those who tested positive for COVID-19 and predictor variables, sex, race, and the PRAPARE score were found to be related with testing positive for COVID-19. Sex was related with testing positive for COVID-19, with 53.8% of those who tested positive being males (Χ2 [1, N = 629] = 5.4, p < .05). Also, of the 629 patients who were tested for COVID-19, 62.4% (n = 58) were Hispanic, 17.2% (n = 16) were non-Hispanic white, 16.1% (n = 15) were NHPI, and 4.3% (n = 4) were grouped into the other category (Χ2 [3, N = 629] = 54.3, p < .001). Lastly, those who tested positive for COVID-19 (M = 4.81, SD = 2.14) were found to have significantly more social determinants of health risks than those who did not (M = 4.15, SD = 2.47; t[138] = −2.67, p < .01).
In the logistic regression model, sex and race/ethnicity were the only covariates found to increase one’s odds for testing positive for COVID-19 among our sample (see Table 2). Males were significantly more likely than females to test positive for COVID-19 (aOR = 1.66, 95% CI = 1.03, 2.69). When compared to non-Hispanic Whites (n = 16, 5.4% of non-Hispanic whites tested), NHPIs (n = 15, 41.7% of NHPI tested) were over 10 (95% CI = 4.32, 26.50) times as likely to test positive for COVID-19. Moreover, those who identifed as Hispanic were five (n = 58, 22.6% of Hispanics tested; 95% CI = 2.60, 9.64) times as likely to test positive for COVID-19 as non-Hispanic whites. Overall, the model explained 16.5% of the variability of testing positive for COVID-19.
Table 2.
Factors associated with testing (n = 1,618) and testing positive (n = 629) for COVID
| Variable | COVID-19 Testing | COVID-19 Positivity |
|---|---|---|
| aOR (95% CI) | aOR (95% CI) | |
| Sex | ||
| Female | 1.00 | 1.00 |
| Male | 1.17 (0.94, 1.47) | 1.66 (1.03, 2.69) |
| Race/Ethnicity | ||
| Non-Hispanic White | 1.00 | 1.00 |
| Native Hawaiian Pacific Islander | 0.26 (0.14, 0.48) | 10.7 (4.32, 26.50) |
| Hispanic | 0.84 (0.64, 1.09) | 5.01 (2.60, 9.64) |
| Other | 1.55 (1.03, 2.33) | 2.16 (0.67, 6.97) |
| Age | ||
| 18-29 | 1.00 | 1.00 |
| 30-39 | 1.52 (1.13, 2.04) | 0.92 (0.50, 1.71) |
| 40-49 | 1.48 (1.07, 2.04) | 0.89 (0.45, 1.76) |
| 50-59 | 1.51 (1.06, 2.16) | 0.65 (0.26, 1.61) |
| 60+ | 0.58 (0.39, 0.87) | 0.46 (0.16, 1.31) |
| Marital Status | ||
| Single | 1.00 | 1.00 |
| Partnered or Married | 0.69 (0.55, 0.86) | 0.89 (0.54, 1.48) |
| Employment Status | ||
| Employed | 1.00 | 1.00 |
| Unemployed | 2.61 (2.04, 3.35) | 1.41 (0.80, 2.49) |
| Positive Depression Screening | ||
| No | 1.00 | 1.00 |
| Yes | 1.77 (1.17, 2.68) | 0.70 (0.22, 2.22) |
| PRAPARE Score | 1.17 (1.11, 1.23) | 0.97 (0.87, 1.09) |
Discussion
The purpose of this study was to explore the relationship between social determinants of health and getting tested for COVID-19, as well as testing positive for COVID-19. Similar to findings reported by the CDC, we found NHPIs and Hispanics were at an increased risk for testing positive for COVID-19 when compared to their non-Hispanic White counterparts [13]. Further, we found some older age groups (30–39 years, 40–49 years, and 50–59 years) to be more likely to be tested for COVID-19 than those between 18–29 years of age, although there were no significant differences between age and testing positive for COVID-19. Also, those older than 60 years of age were significantly less likely to be tested for COVID-19. This may have been due to exposure to someone else who tested positive when the patient was uncertain if they were asymptomatic or pre-symptomatic [26]. Alternatively, older adults (those 60 years of age and older) may have had a greater need to attend the community health center for a non-COVID-19-related illness than their younger counterparts.
While there is a general consensus that the majority of determinants that drive health happen outside a clinical setting, there is a demand for healthcare providers to better understand a patients’ social risks when providing care [6]. Overall, our findings further support the benefits of recording social determinants of health among those seeking care from a community health center to identify patients who require a more robust care plan and follow-up as well as to mitigate poor health outcomes.
Uniquely, we explored the utilization of the PRAPARE tool to estimate a sample of community health center patients’ likelihood of being tested for COVID-19 and subsequently testing positive for the virus. Although few social determinants of health have been reported to aid in preventing the spread of this virus, our findings indicate that race/ethnicity, age, marital status, employment status, a positive depression screening, and the PRAPARE score may be associated with being tested for COVID-19. Further, sex and race/ethnicity may be associated with an increased odds of testing positive for COVID-19. Thus, the PRAPARE tool may help to identify certain social determinants of health that may have increased the community health centers patients’ odds of getting tested for COVID-19, which may have previously gone undetected in other healthcare settings that do not collect such data. Surprisingly, although social determinants of health are drivers for health outcomes across all areas of a person’s health [4, 20], PRAPARE scores were not significantly associated with COVID-19 positivity. Greater examination into each domain being measured in the PRAPARE tool is needed to explore possible risk factors (social or structural) that may be associated with COVID-19 risks or to identify risk factors not currently measured by the PRAPARE tool.
These findings are unique in that the PRAPARE tool, while used widely across the nation’s community health centers [6, 27], has not been examined as an instrument for predicting factors associated with infectious disease prevalence and epidemiology. Thus, our findings indicate that the utilization of PRAPARE tool may help to improve communication and response to infectious disease prevention and control during health crises, such as the COVID-19 pandemic, by increasing the care team’s knowledge of those seeking care and those disproportionally affected by the disease [6, 20]. This study can also provide insight into the need for strategies that intervene upstream to ultimately protect the public and prevent the spread of communicable diseases, such as COVID-19 [28].
In relation to the current COVID-19 pandemic, underserved populations with greater socioeconomic need have been found to have higher prevalence rates [17]. As we found in our study, those who were unemployed had increased odds of being tested for COVID-19 while those who were partnered or married had decreased odds of being tested than their single counterparts. Public health educators should explore alternative strategies to provide education to underserved populations, such as patients with nontraditional routines or those who lack social support, such as a domestic partner. More research is needed to better understand the impact particular social determinants of health, such as employment and marital status, have on seeking a COVID-19 test and testing positive for the virus. It is possible that some employed patients did not seek out COVID-19 testing due to financial inability to miss work in order to be seen by a medical provider. Research has highlighted that the most vulnerable to COVID-19 may also be less likely than their non-Hispanic white counterparts to take paid sick leave [29]. As NHPI and Hispanic patients within our sample were found to be disproportionally affected by COVID-19, it is important that public health policies ensure paid sick leave for all essential workers, especially among industries with higher rates of NPHI and Hispanic employees. Further, there is an increased need for testing to be made available in workplace environments, particularly those that do not offer paid sick leave or time off for seeking preventive care [16]. Though additional research is needed, our findings indicate that social determinants of health significantly impact prevention and control measures during a public health emergency.
The PRAPARE score findings also warrant further examination to understand why the increased number of present social determinants of health risks increased the odds of being tested for COVID-19. This may serve as an indicator that local public health officials are reaching more at-risk communities with health education, communication strategies, and promotion of COVID-19 testing. Additionally, results regarding patients with a positive depression screening warrant further investigation. It could be surmised that those who have been screened with a mental health disorder may be more likely to seek out testing of COVID-19. While this study did not seek to determine why this group may pursue testing of COVID-19, the significance of these additional findings may be critical for understanding the impact of these issues on one’s health.
Although this study identifies factors that increased odds of being tested and testing positive for COVID-19 among our sample, it did not examine reasons why those from particular ethnicities sought testing. Interestingly, NHPIs were less likely than non-Hispanic whites to be tested for COVID-19; however, when tested, NHPIs were significantly more likely to test positive than their counterparts. Moreover, Hispanic patients were significantly more likely to test positive for COVID-19 than non-Hispanic whites. While these findings are similar to previous studies [13], more research is needed to ensure that prevention education and announcements about screening and vaccination availability are made readily available to these specific populations in their native language to help address this health disparity.
This study was subject to limitations. All data, aside from clinical diagnosis or record of visit type (COVID-19/non-COVID-19-related), were self-reported and open to misclassification from low health literacy or for patient fear of sharing their information. Appointment availability for care at the community health center used in this study was limited to Monday through Friday from 8 a.m. to 5 p.m. Thus, it is possible that our findings are restricted to patients who could conveniently visit the community health center during normal working hours. Also, due to sample procedures employed and the cross-sectional nature of the data, findings are only representative of the sample who attended the community health center from where data were collected. Test results were not made available through the electronic medical records of patients who sought testing at a different facility or location; thus, findings cannot be generalized to the general public. Further, with a small sample of NHPIs, findings for testing positive for COVID-19 were found to have wide confidence intervals which should be interpreted with caution. Finally, because this was a single sample from one local community health center, the results may not be generalizable across all populations with differing social and demographic compositions. Alternatively, this study can provide a framework for other community health centers to explore the relationship between their patients’ social determinants of health scores and other prevalent health issues.
This study provides insight that unmet social needs among vulnerable populations may impact their need to be tested for infectious diseases, such as COVID-19. The results demonstrate a need to develop interventions that meet the social needs of a population on a community level. As recommended by a study examining China’s handling of the outbreak, local health departments and community health centers can implement this practice by serving as the primary voice of authority in the reduction in spread of the COVID-19 pandemic within this community [30]. Identifying factors associated with exposure to and positive diagnosis of infectious diseases, community health centers may be able to reduce prevalence of these diseases by targeting testing and immunization education and availability for vulnerable populations.
Acknowledgments
Availability of Data and Material
Data may be made available upon request.
Code Availability
Not applicable
Author’s Contribution
Conceptualization: [Abbie Luzius]; Methodology: [Abbie Luzius, Page D. Dobbs, Bart Hammig]; Formal analysis and investigation: [Abbie Luzius, Page D. Dobbs]; Writing—original draft preparation: [Abbie Luzius, Rebekah Kirkish, Monica Mojica]; Writing—review and editing: [Page D. Dobbs; Bart Hammig]; Supervision: [Page D. Dobbs, Bart Hammig.
Funding
None.
Declarations
Ethics Approval
All procedures for this study were exempt from review by the University of Arkansas Institutional Review Board (IRB: 2009284671, IRB Approval Date: 9/22/2020).
Consent to Participate
Informed consent was obtained before data were collected.
Consent for Publication
The publisher has the consent of all authors to publish this manuscript.
Conflict of Interest
The authors have no conflicts of interest to disclose.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Adashi EY, Geiger HJ, Fine MD. Health care reform and primary care—the growing importance of the community health center. N Engl J Med New England Journal of Medicine (NEJM/MMS) 2010;362:2047–2050. doi: 10.1056/NEJMp1003729. [DOI] [PubMed] [Google Scholar]
- 2.Bailey MJ, Goodman-Bacon A. The war on poverty’s experiment in public medicine: community health centers and the mortality of older Americans. Am Econ Rev American Economic Association. 2015;105:1067–1104. doi: 10.1257/aer.20120070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Larson AE, Hoopes M, Angier H, Marino M, Huguet N. Private/marketplace insurance in community health centers 5 years post-affordable care act in medicaid expansion and non-expansion states. Prev Med (Baltim) Academic Press Inc. 2020;141:106271. doi: 10.1016/j.ypmed.2020.106271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carey G, Crammond B. Help or hindrance? Social policy and the ‘social determinants of health.’. Aust J Soc Issues Wiley Blackwell. 2014;49:489–507. doi: 10.1002/j.1839-4655.2014.tb00325.x. [DOI] [Google Scholar]
- 5.Kusnoor SV, Koonce TY, Hurley ST, McClellan KM, Blasingame MN, Frakes ET, et al. Collection of social determinants of health in the community clinic setting: a cross-sectional study. BMC Public Health BioMed Central Ltd. 2018;18:1–9. doi: 10.1186/s12889-017-4524-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weir RC, Proser M, Jester M, Li V, Hood-Ronick CM, Gurewich D. Collecting Social Determinants of Health Data in the Clinical Setting: Findings from National PRAPARE Implementation. J Health Care Poor Underserved. 2020;31:1018–1035. doi: 10.1353/hpu.2020.0075. [DOI] [PubMed] [Google Scholar]
- 7.Falletta L, Redding M, Cairns J, Albugmi M, Redding S, Gittelman M, et al. Embracing the complexity of modifiable risk reduction: a registry of modifiable risks for 0-12 month infants. Prev Med (Baltim) Academic Press Inc. 2020:137. [DOI] [PubMed]
- 8.World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020. 2020.
- 9.Goyal MK, Johnson TJ, Chamberlain JM, Cook L, Webb M, Drendel AL, et al. Racial and ethnic differences in emergency department pain management of children with fractures. Pediatrics American Academy of Pediatrics. 2020;145. [DOI] [PMC free article] [PubMed]
- 10.McMichael TM, Currie DW, Clark S, Pogosjans S, Kay M, Schwartz NG, et al. Epidemiology of Covid-19 in a Long-Term Care Facility in King County, Washington. N Engl J Med Massachusetts Medical Society. 2020;382:2005–2011. doi: 10.1056/NEJMoa2005412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ebrahim SH, Ahmed QA, Gozzer E, Schlagenhauf P, Memish ZA. Covid-19 and community mitigation strategies in a pandemic. BMJ. BMJ Publishing Group; 2020. [DOI] [PubMed]
- 12.Markel H, Lipman HB, Navarro JA, Sloan A, Michalsen JR, Stern AM, Cetron MS. Nonpharmaceutical interventions implemented by US cities during the 1918-1919 influenza pandemic. J Am Med Assoc JAMA. 2007;298:644–654. doi: 10.1001/jama.298.6.644. [DOI] [PubMed] [Google Scholar]
- 13.Hernandez AL, Da Silva J, Martin D, Krow-Lucal E, Lilo E, Mazurek J, et al. Summary Report COVID-19 among Hispanic and Marshallese communities in Benton and Washington. 2020. [DOI] [PMC free article] [PubMed]
- 14.Flaskerud JH. Masks, Politics, Culture and Health. Issues Ment Health Nurs [Internet]. Taylor and Francis Ltd; 2020 [cited 2021 May 18];41:1–4. Available from: https://pubmed.ncbi.nlm.nih.gov/32644832/ [DOI] [PubMed]
- 15.Ammar A, Chtourou H, Boukhris O, Trabelsi K, Masmoudi L, Brach M, et al. COVID-19 Home Confinement Negatively Impacts Social Participation and Life Satisfaction: A Worldwide Multicenter Study. Int J Environ Res Public Health. 2020;17:6237. doi: 10.3390/ijerph17176237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oldfield BJ, Decosta S, Petterson L, Lagarde S, Olson DP. A Blueprint for Community Health Center and Nursing Home Partnership: testing for COVID-19 among Residents and Staff at Long-term Care Facilities. J Health Care Poor Underserved. 2021; [cited 2021 Mar 26];32:xi–xviii. Available from: 10.1353/hpu.2021.0001https://muse.jhu.edu/article/783087. [DOI] [PubMed]
- 17.Holmes L, Enwere M, Williams J, Ogundele B, Chavan P, Piccoli T, et al. Black–white risk differentials in covid-19 (Sars-cov2) transmission, mortality and case fatality in the united states: Translational epidemiologic perspective and challenges. Int J Environ Res Public Health. 2020;17:1–18. doi: 10.3390/ijerph17124322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liang Y, Gong Y-H, Wen X-P, Guan C-P, Li M-C, Yin P, et al. Social determinants of health and depression: a preliminary investigation from rural China. Laks J, editor. PLoS One. Public Library of Science; 2012;7:e30553. [DOI] [PMC free article] [PubMed]
- 19.Chow N, Fleming-Dutra K, Gierke R, Hall A, Hughes M, Pilishvili T, et al. Preliminary Estimates of the Prevalence of Selected Underlying Health Conditions Among Patients with Coronavirus Disease 2019—United States, February 12–March 28, 2020. MMWR Morb Mortal Wkly Rep. Centers for Disease Control MMWR Office; 2020;69:382–6. [DOI] [PMC free article] [PubMed]
- 20.National Association of Community Health Centers, Association of Asian Pacific Community Health Organizations, Oregon Primary Care Association. IMPLEMENTATION AND ACTION TOOLKIT. 2019.
- 21.Forbes CN, Tull MT, Xie H, Christ NM, Brickman K, Mattin M, et al. Emotional avoidance and social support interact to predict depression symptom severity one year after traumatic exposure. Psychiatry Res. Elsevier Ireland Ltd; 2020;284:112746. [DOI] [PMC free article] [PubMed]
- 22.National Association of Community Health Centers, Association of Asian Pacific Community Health Organizations, Oregon Primary Care Association. PRAPARE Risk Tally Scoring Methodology. 2016.
- 23.Santos S, Chiesa M. PCR positives: what do they mean?
- 24.Souch JM, Cossman JS. A Commentary on Rural-Urban Disparities in COVID-19 Testing Rates per 100,000 and Risk Factors. J. Rural Heal. Blackwell Publishing Ltd; 2021. p. 188–90. [DOI] [PMC free article] [PubMed]
- 25.IBM SPSS Statistics for Windows. Version 26.0. Armonk, NY: IMB Corp.; 2019.
- 26.Kimball A, Hatfield KM, Arons M, James A, Taylor J, Spicer K, et al. Asymptomatic and Presymptomatic SARS-CoV-2 Infections in Residents of a Long-Term Care Skilled Nursing Facility—King County, Washington, March 2020. MMWR Morb Mortal Wkly Rep [Internet]. Centers for Disease Control MMWR Office; 2020 [cited 2021 Mar 26];69:377–81. Available from: http://www.cdc.gov/mmwr/volumes/69/wr/mm6913e1.htm?s_cid=mm6913e1_w [DOI] [PMC free article] [PubMed]
- 27.Moore JE, Adams C, Tuck K. Medicaid Access & Coverage to Care in 2018. 2019.
- 28.Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep Association of Schools of Public Health. 2014;129:19–31. doi: 10.1177/00333549141291S206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vazquez J, Islam T, Beller J, Fiori K, Correa R, Correa DJ. Expanding Paid Sick Leave as a Public Health Tool in the Covid-19 Pandemic. J Occup Environ Med [Internet]. NLM (Medline); 2020 [cited 2021 Mar 30];62:e598–9. Available from: https://journals.lww.com/10.1097/JOM.0000000000001998, 62, e598, e599 [DOI] [PubMed]
- 30.Zeng W, Li G, Turbat V, Hu G, Ahn H, Shen J. Optimizing preventive medicine to bridge the gap between clinical medicine and public health for disease control in China: a lesson from COVID-19. Prev Med (Baltim) [Internet]. Academic Press; 2021 [cited 2020 Nov 17];143:106324. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0091743520303480 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data may be made available upon request.