Abstract
Companies are designing next-generation antibodies modeled on those taken from unique individuals whose immune systems can neutralize any COVID-19 variant—and related coronaviruses, too.
The US Food and Drug Administration (FDA) granted Emergency Use Authorization (EUA) in late May to sotrovimab, providing a new therapeutic weapon in the fight against SARS-CoV-2—and future coronaviruses with pandemic potential.
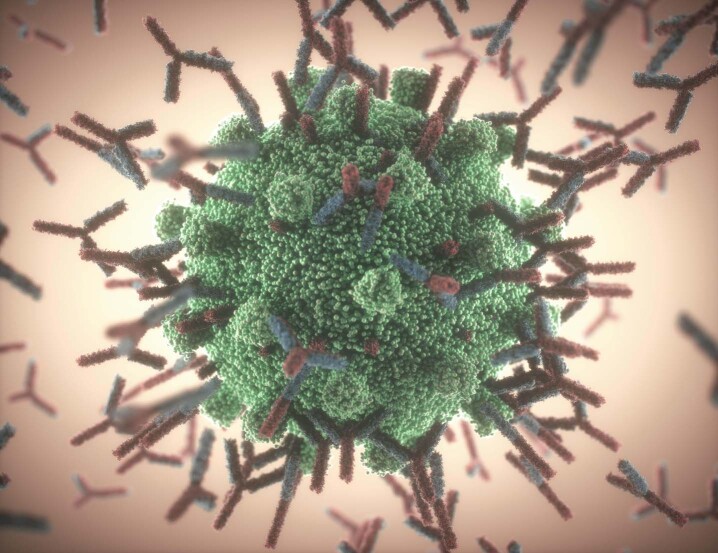
Antibodies attacking a coronavirus (artist’s impression). Super-antibodies that can neutralize even the most worrying versions of SARS-CoV-2 could be used both to prevent and to treat infections.
Kiyoshi Takahase Segundo / Alamy Stock Photo
According to analysts and researchers alike, so-called super-antibodies such as sotrovimab should have an edge over first-generation monoclonal antibody (mAb) therapies for COVID-19 because of their broad neutralization capacity in the face of emerging virus variants. “Physicians aren’t going to sequence what version of the virus people have, so they’ll go for the antibodies that have the higher barrier to resistance or the ones that work on [known] variants,” says Phil Nadeau, an analyst at Cowen.
The antibody therapy from Vir Biotechnology and GlaxoSmithKline, a recombinant human immunoglobulin G1 mAb, is now the third mAb-based treatment marketed for individuals with mild-to-moderate COVID-19 who are at high risk for progression to severe disease. (Eli Lilly and Regeneron each have a two-mAb cocktail with EUAs for the same indication.) And although sales opportunities should diminish for all these products as vaccination rates increase worldwide, Nadeau anticipates there will be a sustained market for COVID-19 mAbs to help treat individuals who, for medical reasons, can’t mount an appropriate immune response to vaccination or, for whatever reason, elect not to get the shot.
According to his models, sotrovimab should capture around 10% of the $3 billion global COVID-19 mAb market this year, rising to 30% of the $1.67 billion market in 2022.
Other broadly cross-reactive mAbs could soon be jockeying for market share as well, as investment money flows in to rush some of the leading candidates through late-stage clinical development. In April, for example, Adagio Therapeutics raised $336 million (on top of the $130 million war chest it amassed last year) to bankroll large-scale trials of ADG20, an mAb now being evaluated for use as a therapy and for prevention. Startups such as Centivax, Corat Therapeutics, IDBiologics, Leyden Labs, Memo Therapeutics and SpikImm are working on next-generation mAbs for COVID-19 as well.
Sotrovimab traces its roots back to blood drawn in 2013 from an individual who had recovered from the 2003 outbreak of severe acute respiratory syndrome (SARS); ADG20 has a similar origin story, while most other clinical-stage mAbs were inspired by antibodies found in more recent COVID-19 survivors. Many companies then optimized their mAbs by extending half-lives, enhancing neutralizing activity, manipulating constant region (Fc)-mediated effector functions, or applying some combination of these engineering strategies.
To stay relevant, all mAb developers need to account for the wildcard that is viral evolution, says Jane Osbourn, CSO of Alchemab and former head of the UK BioIndustry Association’s antibody taskforce on COVID-19. “A number of the clinical candidates out there are falling over against the [emerging] variants,” she says. “So, as a community, we should really be taking the time to think through how you stay ahead of the game in terms of that mutational drift.”
In lab studies, sotrovimab seems to maintain its neutralization capacity against all circulating variants of concern, including some of the most worrying versions of the virus, first identified in South Africa, Brazil and India. Several of the leading phase 3 mAb candidates—including Adagio’s ADG20, AstraZeneca’s AZD7442 and Brii Biosciences’ BRII-196 and BRII-198—do as well. But Eli Lilly’s two-mAb cocktail is hobbled by escape mutations found in these variants, as is one of the agents, casirivimab, in Regeneron’s mAb combination. The other Regeneron agent, imdevimab, retains its activity, in large part because the mAb targets an epitope that does not overlap with that of its cocktail companion.
That non-redundancy offers some degree of protection against variant-mediated resistance, says Aeron Hurt, principal global medical science director for influenza and COVID-19 therapeutics at Roche, which partnered with Regeneron to handle manufacturing and distribution outside of the United States. “Single antibodies are vulnerable to single mutations,” Hurt says—whereas a cocktail of antibodies that bind at discrete sites provides “an extra insurance policy.”
But an even better variant evasion tactic, asserts Adagio CSO Laura Walker, is what her company and Vir have done: both organizations independently screened for ultra-rare broadly neutralizing mAbs that recognize highly conserved epitopes found across the entire family of SARS-like coronaviruses.
The scarcity of these antibodies limits the evolutionary selection pressure for escape mutations in nature, Walker points out. And because conserved residues typically serve essential protein functions, “the virus often can’t mutate those residues without suffering a fitness cost,” she says, “which means the barrier to escape is typically higher for these broadly neutralizing antibodies.”
“But antibodies are not merely things that bind to and neutralize a viral protein,” notes Vir CSO Skip Virgin. Through their Fc domain, mAbs also induce innate and adaptive immune responses that help destroy infected cells—and those Fc-mediated activities, Virgin says, “are fundamentally important for treatment of SARS and COVID-19.”
Mouse studies published in Cell, in the Journal of Experimental Medicine and as a preprint in recent months now support this idea. But last year, as the COVID-19 mAb race was just heating up, many companies—including AstraZeneca, Eli Lilly, Abpro and others—chose instead to dial down effector functions in their mAbs. They wanted to minimize the risk of antibody-dependent enhancement of viral infection, a phenomenon in which virus-specific antibodies can promote, rather than inhibit, disease.
This can be a real problem with certain pathogens, including the respiratory syncytial virus and the dengue virus, but Virgin and his colleagues realized early on that it did not seem to be an issue with SARS-CoV-2. So Vir doubled down on the need for strong Fc receptor binding. Not only did the company leave the effector functions intact for sotrovimab, but it also engineered its successor, the follow-on mAb VIR-7832, to have even greater Fc binding activity.
“The concept is to make the antibody vaccinal,” explains Virgin. “We’re trying to make the antibody so it not only protects the individual, but it also generates an immune response that outlasts it” through the generation of pathogen-specific CD4+ and CD8+ T cells responses. The Vir team joined forces last year with Jeffrey Ravetch’s lab at Rockefeller University in New York City to demonstrate the Fc engineering concept with an anti-influenza mAb tested in mice.
The concept is to make the antibody vaccinal.
“These are predicted benefits. They haven’t been observed in people,” Virgin acknowledges, “but that’s why we’re taking the antibody forward.” VIR-7832 and sotrovimab—both of which possess an Fc mutation that confers extended half-life and enhances drug distribution to the lungs—are now part of a master protocol study taking place in the United Kingdom.
Adagio, for its part, has focused its engineering efforts largely on affinity optimization rather than Fc modifications. Although ADG20, like many other next-generation mAbs, does contain Fc changes that improve its circulation half-life, its most distinguishing selling point is the combination of potency and breadth that it offers.
“We took something from nature that was broad, but not very potent, and then improved the potency while maintaining the breadth to essentially make a molecule that would never arise in nature,” explains Walker.
Walker and her colleagues started with a natural mAb made in response to a 2003 SARS infection. They then used yeast display technologies to introduce diversity into the parent clone, ultimately finding an offshoot with a handful of genetic changes that gave it 500-fold greater binding affinity to the SARS-CoV-2 spike protein and a 70-fold improvement in neutralization capacity—with no compromise in its breadth of activity across other SARS-related coronaviruses.
In phase 1 testing, clinicians found that a single dose of ADG20 yielded a similar level of virus-neutralizing activity in the blood as that seen among people vaccinated against COVID-19 with one of the marketed mRNA-based products. Pharmacokinetic profiling also indicated that the protection might last for up to a year. Two large global trials are ongoing.
ADG20, like some other late-stage candidates such as AZD7442, also offers the convenience of intramuscular injections—a formulation advantage that Janice Reichert, executive director of the non-profit Antibody Society, argues can be just as important as innovative mAb designs in the throes of a pandemic or other public health crisis. “Having both would be best, of course,” she adds. All the mAbs that already have EUAs must be given intravenously, although versions formulated for intramuscular or subcutaneous administration are now in clinical testing.
Some companies are beginning to explore inhaled delivery as well. Boehringer Ingelheim, for example, is evaluating both infused and inhaled versions of its phase 2 mAb before deciding which administration route to advance into pivotal testing. On 3 June, scientists from IGM Biosciences described promising mouse data on their nasally spritzed product, the immunoglobulin M mAb IGM-6286. And earlier this year, Leyden Labs launched with €40 million ($49 million) to support a portfolio of intranasal products that protect against respiratory viruses such as influenza and SARS-CoV-2.
According to Dinko Valerio, co-founder and executive chairman of Leyden Labs, the company’s nasal spray is designed to thwart viral replication at the site of infection. And because of its localized delivery, patients can get away with much lower doses than they would otherwise need for any systemically administered agent. “If you put it in the nose,” Valerio says, “you just need a tiny bit” of the product.
Whatever the mechanism of mAb delivery, the fact that so much development and therapeutic experimentation is happening today in response to COVID-19 should improve preparedness for the future. Not only are there now products like sotrovimab on the market that offer broad protection against a viral clade that could easily seed the next outbreak, but the engineering approaches being tried now to combat coronaviruses should help inform best practices for creating mAbs designed to thwart other viral families.
“It’s good for public health that all these strategies are being tested,” remarks James Crowe, director of the Vanderbilt Vaccine Center in Nashville, Tennessee. (A co-founder of IDBiologics, Crowe helped discover the mAbs that form the basis of two cocktail therapies now in clinical testing, AZD7442 from AstraZeneca and another one from Resilience with support from the US Department of Defense.) “It’s very exciting scientifically that COVID has allowed this many manufacturers to participate,” he says. “Every target is different, but you can typically learn some general principles.”