Abstract
Thrombo-embolic episodes and invasive mucormycosis (IM) have shown a sudden surge after the second wave of novel coronavirus infection in India. Acute mesenteric ischemia secondary to coronavirus-19 is rare and that too due to invasive mesenteric mucormycosis has not yet been reported in Indian literature. We present a case of post-COVID diabetic woman who was on steroids and had mesenteric thrombosis with IM. The disease is associated with high mortality. Treatment of choice is wide surgical resection and iv liposomal amphotericin B. Since the pre-operative as well as intra-operative diagnosis is difficult, high index of suspicion for IM is necessary in post-COVID-19 patients presenting with mesenteric ischemia or bowel perforation.
Keywords: COVID-19, Coronavirus, Mucormycosis, Acute mesenteric ischemia, Mesenteric thrombosis
Introduction
While our country is fighting with the second wave of COIVD-19, there is a fear of another pandemic emerging from delayed complications of the disease. Thrombo-embolic episodes and invasive mucormycosis (IM) have shown a sudden surge after the second wave of novel coronavirus infection [1, 2]. We present a case of invasive gastrointestinal (GI) mesenteric mucormycosis resulting in acute mesenteric ischemia (AMI) and bowel gangrene.
Case Summary
A diabetic lady, 57 years old, presented in emergency with complains of pain abdomen for 3 days and abdominal distension and constipation for 1 day. There was no history of fever, vomiting or diarrhoea in the last 3 days. Patient was a known case of COVID-19 viral pneumonia (diagnosed 20 days back) and was managed conservatively in home isolation. She had not been on oxygen supplementation but was on oral steroids (methyl prednisolone 32 mg twice a day) for the last 15 days without any monitoring for blood sugar levels. She was on glimepiride 2 mg once daily for the last 3 years and continued the same without any dose modification. She was afebrile for the last 10 days and was on oral antibiotics, but no anti-fungal drug or blood thinners were used. Her CT scan done on day 5 of the fever was suggestive of viral pneumonia (COVID-19) with CT severity score of 12. At admission, her pulse rate was 105/min, BP was 130/90 mmHg, temperature 98.6 F, respiratory rate 22/min and SpO2 96% on room air. On examination, the abdomen was distended with mild tenderness in the lower abdomen. She was admitted in non-ICU bed, and her blood investigations revealed Hb 11.8 gm/dl, TLC 16,300 with 96% polymorphs and 3% lymphocytes, blood sugar 314, HbA1c 9.6% and serum albumin 2.08 gm/dl. Serum electrolytes, urea and creatinine were normal. Patient was started on iv fluids, analgesics and antibiotics (ceftriaxone + tazobactam, metronidazole). CT scan done on the next day revealed circumferential thickening of terminal ileum and caecum along with inflammation of peritoneal and retroperitoneal fat in right iliac fossa and right side of the pelvis.
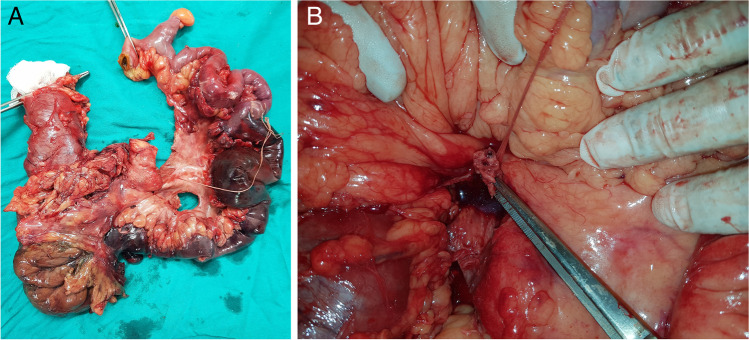
In view of persistent pain and CT findings, patient was planned for laparotomy. Intra-operatively, proximal small bowel was dilated, and distal ileum was gangrenous with thickened, edematous and indurated mesentery. Ileal gangrene was extending from two feet proximal to ileocaecal junction to ascending colon [Fig. 1A]. Hepatic flexure and transverse colon were normal. Pulsations of ileocolic trunk were not palpable. Intra-op diagnosis was post-COVID ileocolic trunk thrombosis [Fig. 1B] with acute mesenteric ischemia. Patient underwent right hemicolectomy with resection of distal two feet of ileum. End ileal stoma with colonic mucus fistula was made after thorough peritoneal lavage. Intra-operative blood loss was about 200 ml.
Fig. 1.
A: Gangrenous distal ileum, caecum and ascending colon. B Thrombosed ileocolic trunk
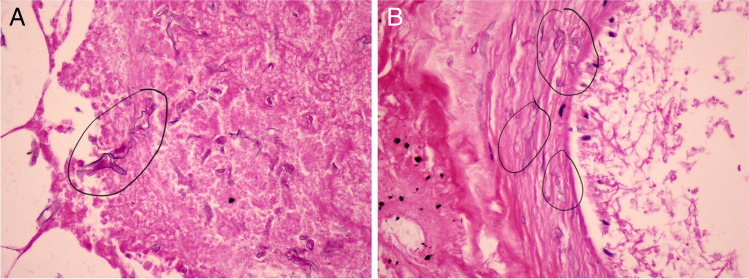
Post-operatively, patient was extubated but kept in ICU care. Antibiotics were escalated to imipenem + cilastatin and teicoplanin, and further labs were sent (CRP of 510, LDH 2650 and D-dimer > 9200). Anti-fungal was not started since the diagnosis could not be established by then. She was comfortable, pain free and hemodynamically stable for the first 24 h after which she complained of pain abdomen once again and had fall in BP and urine output. Patient was put on inotropic support, and iv analgesics were continued. She however continued to deteriorate over the next few hours and had cardio-pulmonary arrest which unfortunately could not be resuscitated. Post-mortem examination of the patient was not done. Histopathology examination of the specimen on gross revealed greenish black bowel with thickened mesentery but failed to show any lumps or blackish growths. On microscopic examination, acute necrotising transmural inflammation of the bowel was seen with gangrenous changes. Congested and thrombosed blood vessels were seen in mesentery with extensive fungal infestation (morphologically consistent with mucormycosis) [Fig. 2A] along with angioinvasion and vascular thrombosis [Fig. 2B].
Fig. 2.
A: Mucor hyphae seen in haemorrhagic necrotic tissue — marked with black circles (40 ×). B Angioinvasion with mucor hyphae seen invading the vessel wall — marked with multiple black circles (40 ×)
Discussion
Novel coronavirus disease (COVID-19) was first detected in Wuhan, China, in December 2019 and was declared a pandemic by WHO in march 2020. India saw the first wave of pandemic in mid-2020 with its peak in September. Usual symptoms in the first wave were fever, fatigue, myalgia and headache, and respiratory tract was the most common organ system involved. Most severe cases and fatality were a result of immunological cascade resulting in ARDS, hypoxia, shock and multi-organ failure. Mortality in the first wave was highest in the elderly group with pre-exiting co-morbidities. The second wave of this pandemic started in India somewhere in march 2021 with its peak in May. Although the wild strain of the virus was same, mutations had resulted in more severe form of disease and mortality even in younger population without pre-existing comorbidities. A new trend was seen this time in the form of delayed complications (thrombo-embolic episodes and mucormycosis) even after complete recovery and discharge from the hospital. Thrombotic complications usually presented as deep vein thrombosis, pulmonary embolism, acute coronary syndrome and stroke while mucormycosis was usually seen in the paranasal sinus extending into the orbit, mouth, face or brain and in lungs [1, 2]. Acute mesenteric ischemia secondary to coronavirus-19 is rare [3–5] and that too due to mesenteric mucormycosis has not yet been reported in Indian literature to the best of our knowledge.
Mucormycosis is characterised by necrosis of the host tissue due to invasion of its vascular supply by hyphae. Classically majority of patients with invasive mucormycosis are immunocompromised and/or have poor glycemic control [6]. This happens during the recovery phase of COVID-19 when patients are immunocompromised by viral infection and steroid use and simultaneously having poor glycemic control. Rampant use of wide spectrum antibiotics along with voriconazole may also be an added risk factor. While GI mucormycosis is rare (about 8% of cases), stomach and colon are the most commonly affected organs, and the mortality can be as high as 85% [7]. The symptoms of GI mucormycosis are non-specific and could be combinations of fever, nausea/vomiting, pain abdomen, GI bleeding, perforation or gangrene. Pre-operative as well as intra-operative diagnosis is difficult since signs and symptoms, imaging and intra-operative gross appearance may not suggest mucormycosis. Diagnosis is usually by histopathologic identification of fungal hyphae in biopsy specimen [7]. A high index of suspicion for IM is therefore necessary in post-COVID-19 patients presenting with mesenteric ischemia or bowel perforation especially if they were diabetic or used high dose steroids. Treatment of the disease is surgical debridement of the involved tissue along with antifungal therapy. Liposomal amphotericin B is the drug of choice for mucormycosis. It is administered as iv infusion at the dose of 5 mg/Kg body weight over 1 h for 6–8 weeks. Test dose should be administered prior to first dose with 1 mg infusion over 10 min and then wait for 30 min before starting infusion if no adverse effects are observed. Since the most common side effects are nephrotoxicity, hypokalemia and hypomagnesemia, all patients should be monitored at least weekly with renal function tests and potassium and magnesium levels.
Declarations
Ethics Approval
No ethical approval was needed for this study as this is a case report.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mayank Jain, Email: mayank.dr@gmail.com.
Ranvir Tyagi, Email: drranvirstyagi@gmail.com.
Rakesh Tyagi, Email: drrktyagi@yahoo.co.in.
Gaurav Jain, Email: Gaurav_jain1112@yahoo.co.in.
References
- 1.Revannavar SM, Supriya PS, Samaga L, et al. COVID-19 triggering mucormycosis in a susceptible patient: a new phenomenon in the developing world? BMJ Case Rep. 2021;13:e241663. doi: 10.1136/bcr-2021-241663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chennamchetty VK, Adimulapu S, Kola BP, et al. Post-COVID pulmonary mucormycosis- a case report. Ind J Immunol Respir Med. 2021;6(1):62–66. [Google Scholar]
- 3.Handaya AY, Andrew J, Hanif AS, et al. Covid-19 mimicing symptoms in emergency gastrointestinal surgery cases during pandemic: a case series. Int J Surg Case Rep. 2020;77:22–27. doi: 10.1016/j.ijscr.2020.10.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Keshavaraz P, Rafiee F, Kavandi H, et al. Ischemic gastrointestinal complications of COVID-19: a systematic review on imaging presentation. Clin Imaging. 2021;73:86–95. doi: 10.1016/j.clinimag.2020.11.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Karna SJ, Panda R, Maurya AP, et al. Superior mesenteric artery thrombosis in COVID-19 pneumonia: an underestimated diagnosis—first case report in Asia. Ind Journal of Surg. 2020;82:1235–1237. doi: 10.1007/s12262-020-02638-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jeong W, Keighley C, Wolfe R, et al. The epidemiology and clinical manifestations of mucormycosis: a systematic review and meta-analysis of case reports. Clin Microbiol Infect. 2019;25:26–34. doi: 10.1016/j.cmi.2018.07.011. [DOI] [PubMed] [Google Scholar]
- 7.Roden MM, Zaoutis ET, Buchanan WL, et al. Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis. 2005;41:634–653. doi: 10.1086/432579. [DOI] [PubMed] [Google Scholar]