ABSTRACT
A 19-year-old man with noncirrhotic portal hypertension status post transjugular intrahepatic portosystemic shunt, gastric esophageal varices status post coil embolization, and thrombophilia because of Factor V Leiden heterozygosity presented with jaundice and elevated liver enzymes. His cholangiogram during endoscopic retrograde cholangiopancreatography demonstrated biliary tract obstruction at the bifurcation of the right and left hepatic ducts. With the aid of digital single-operator cholangioscopy, the patient was found to have a perforation of the common hepatic duct from the shunt. This case presents a novel use for digital single-operator cholangioscopy in identifying this rare complication and appropriately differentiating biliary compression vs perforation from transjugular intrahepatic portosystemic shunt.
INTRODUCTION
Transjugular intrahepatic portosystemic shunt (TIPS) is first-line therapy for refractory portal hypertension.1–5 Biliary complications are rare and, when present, are noted to be due to biliary-shunt fistulas that form over time. We present an unusual complication of immediate biliary obstruction because of TIPS perforating the biliary tract, identified with the aid of digital single-operator cholangioscopy (d-SOC).
CASE REPORT
A 19-year-old man with noncirrhotic portal hypertension secondary to portal and splenic vein thrombosis with cavernous transformation status post TIPS, gastric esophageal varices status post coil embolization, and thrombophilia because of Factor V Leiden heterozygosity presented with jaundice. He had TIPS (Viatorr-covered TIPS device advanced into the main portal vein below the bifurcation, 10-mm diameter × 80-mm covered length) with prophylactic left gastric varices coil embolization without any procedural complications 2 days before admission. Total bilirubin on day of the procedure was 1.9 mg/dL. Since then, he has had worsening abdominal pain and jaundice. At presentation, he was found to have elevated liver enzymes with a total bilirubin of 18.4 mg/dL and direct bilirubin of 14.8 mg/dL (Table 1).
Table 1.
Trend in Liver Enzymes After Transjugular Intrahepatic Portosystemic Shunt Placement
| Test (reference range) | Day 0 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 |
| ALP (17–142 U/L) | 61 U/L | 429 U/L | 469 U/L | 641 U/L | 643 U/L | 519 U/L |
| ALT (7–52 U/L) | 63 U/L | 414 U/L | 480 U/L | 374 U/L | 272 U/L | 177 U/L |
| AST (13–29 U/L) | 119 U/L | 597 U/L | 502 U/L | 322 U/L | 119 U/L | 45 U/L |
| Total bilirubin (0.0–1.0 mg/dL) | 1.9 mg/dL | 18.4 mg/dL | 18.7 mg/dL | 24.8 mg/dL | 12.7 mg/dL | 10.8 mg/dL |
| Total protein (6.4–8.0 g/dL) | 6.7 g/dL | 7.0 g/dL | 7.4 g/dL | 6.4 g/dL | 6.3 g/dL | 6.7 g/dL |
| Albumin (3.5–5.0 g/dL) | 4.3 g/dL | 4.6 g/dL | 4.9 g/dL | 4.3 g/dL | 4.0 g/dL | 4.1 g/dL |
ALP, alkaline phosphatase; AST, aspartate aminotransferase; ALT, alanine aminotransferase; day 0, day of transjugular intrahepatic portosystemic shunt; day 3, day of endoscopic retrograde cholangiopancreatography; day 4, external and internal percutaneous biliary catheter placed by interventional radiology.
Triple-phase abdominal and pelvic computed tomography and ultrasound of the TIPS revealed patent flow through the TIPS. Because of his recent coil, he was unable to undergo magnetic resonance cholangiopancreatography to evaluate the biliary tract; therefore, endoscopic retrograde cholangiopancreatography was performed. The cholangiogram demonstrated biliary tract obstruction at the bifurcation of the right and left hepatic ducts (Figure 1). d-SOC was used to differentiate biliary compression from biliary perforation, which confirmed the presence of the shunt within the common hepatic duct (Figure 2). An external and internal percutaneous biliary catheter (10 French by 45-cm locking loop catheter) was placed for biliary decompression before surgical repair with a hepaticojejunostomy. Intraoperative findings during the hepaticojejunostomy performed 5 months later confirmed communication between the common hepatic duct and exposed stent from the anterior wall of the portal vein.
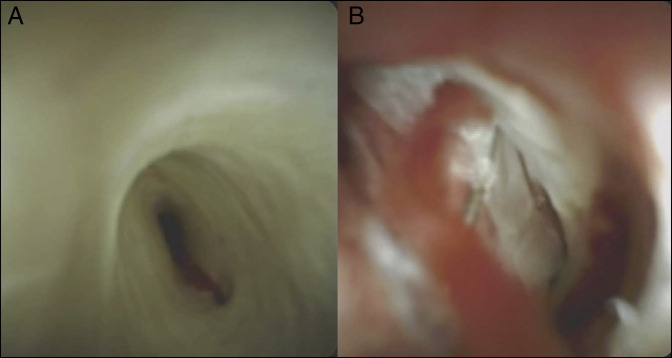
Figure 1.
Endoscopic retrograde cholangiopancreatography was performed to visualize the biliary tract better. This fluoroscopy image shows the transjugular intrahepatic portosystemic shunt (asterisk) appearing to compress the biliary duct at the level of the hepatic bifurcation (arrow).
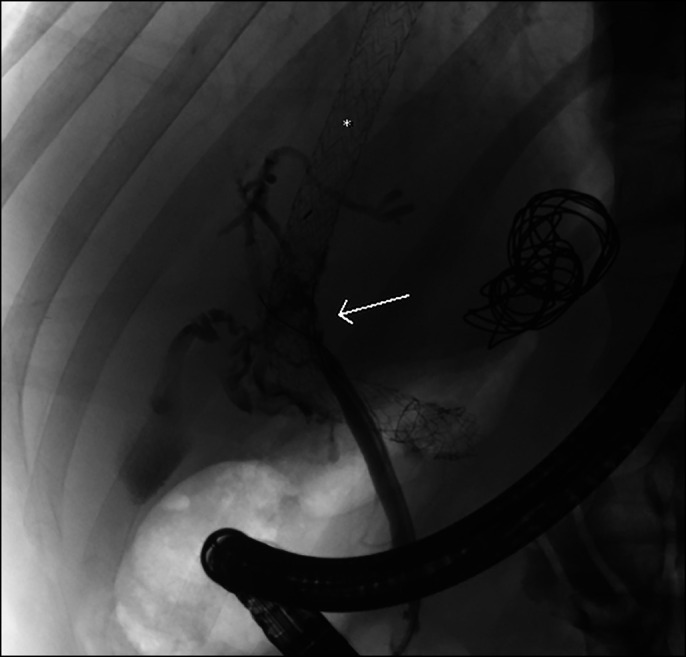
Figure 2.
Visualization of the biliary tract using digital single-operator cholangiopancreatoscopy reveals (A) bile duct compression and (B) the presence of the transjugular intrahepatic portosystemic shunt stent within the biliary tract.
DISCUSSION
This case demonstrates a rare biliary complication of TIPS. Even in TIPS procedures, biliary complications of hyperbilirubinemia and biliary peritonitis have been reported to occur up to 3% of the time,2 with less than 1% because of biliary duct injury.2,6 The most commonly cited reason for hyperbilirubinemia in the literature is due to biliary-shunt fistulas, which can be amenable to endoscopic therapy with biliary stenting.6–11 Many of these cases presented with concurrent biliary duct thromboses and ultimately required liver transplantation. Although nearly a dozen cases have noted biliary-fistula shunts as a complication of TIPS, only one other case has been reported in the literature of malpositioning and occlusion of the biliary tract.3,6–13 In that case, malpositioning of the TIPS into the common hepatic duct was suspected based on abdominal computed tomography and confirmed based on contrast studies during endoscopic retrograde cholangiopancreatography and percutaneous transhepatic cholangiography for the placement of biliary drainage catheters.3
The patient was also noted to have thrombosis of the TIPS and recurrent variceal bleeds, and he ultimately underwent liver transplantation. Although malpositioning of the TIPS within the biliary tract was clearly seen in the other case report, our patient's cholangiogram was difficult to distinguish compression from perforation of the biliary tract. d-SOC has been successfully used for diagnostic and therapeutic biliary interventions.14,15 In this case, the use of this imaging modality helped confirm the underlying cause for hyperbilirubinemia and enabled appropriate subsequent interventions. For other patients with post-TIPS biliary tract obstruction, our case presents a novel use for d-SOC in identifying this rare complication and appropriately differentiating biliary compression vs perforation from TIPS.
DISCLOSURES
Author contributions: F. Patel and B. Bick contributed equally to this manuscript. B. Bick is the article guarantor.
Financial disclosure: None to report.
Previous presentation: This case was presented at the American College of Gastroenterology Annual Scientific Meeting; October 23-28, 2020; Virtual.
Informed consent was obtained for this case report.
REFERENCES
- 1.Boyer TD. Transjugular intrahepatic portosystemic shunt in the management of complications of portal hypertension. Curr Gastroenterol Rep 2008;10(1):30–5. [DOI] [PubMed] [Google Scholar]
- 2.Dariushnia SR, Haskal ZJ, Midia M, et al. Quality improvement guidelines for transjugular intrahepatic portosystemic shunts. J Vasc Interv Radiol 2016;27(1):1–7. [DOI] [PubMed] [Google Scholar]
- 3.Paterno F, Khan A, Cavaness K, et al. Malpositioned transjugular intrahepatic portosystemic shunt in the common hepatic duct leading to biliary obstruction and liver transplantation. Liver Transpl 2011;17(3):344–6. [DOI] [PubMed] [Google Scholar]
- 4.Silva RF, Arroyo PC, Jr, Duca WJ, et al. Complications following transjugular intrahepatic portosystemic shunt: A retrospective analysis. Transplant Proc 2004;36(4):926–8. [DOI] [PubMed] [Google Scholar]
- 5.Siramolpiwat S. Transjugular intrahepatic portosystemic shunts and portal hypertension-related complications. World J Gastroenterol 2014;20(45):16996–7010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ripamonti R, Ferral H, Alonzo M, et al. Transjugular intrahepatic portosystemic shunt-related complications and practical solutions. Semin Intervent Radiol 2006;23(2):165–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Duller D, Kniepeiss D, Lackner C, et al. Biliary obstruction as a complication of transjugular intrahepatic portosystemic shunt. Liver Transpl 2009;15(5):556–7. [DOI] [PubMed] [Google Scholar]
- 8.Jawaid Q, Saeed ZA, Di Bisceglie AM, et al. Biliary-venous fistula complicating transjugular intrahepatic portosystemic shunt presenting with recurrent bacteremia, jaundice, anemia and fever. Am J Transplant 2003;3(12):1604–7. [DOI] [PubMed] [Google Scholar]
- 9.Mallery S, Freeman ML, Peine CJ, et al. Biliary-shunt fistula following transjugular intrahepatic portosystemic shunt placement. Gastroenterology 1996;111(5):1353–7. [DOI] [PubMed] [Google Scholar]
- 10.Singal AK, Kathuria MK, Malhotra A, et al. Bilhemia after trans-jugular intra-hepatic porto-systemic shunt and its management with biliary decompression. World J Gastroenterol 2009;15(29):3681–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sze DY, Vestring T, Liddell RP, et al. Recurrent TIPS failure associated with biliary fistulae: Treatment with PTFE-covered stents. Cardiovasc Intervent Radiol 1999;22(4):298–304. [DOI] [PubMed] [Google Scholar]
- 12.Boyvat F, Cekirge S, Balkanci F, et al. Treatment of a TIPS-biliary fistula by stent-graft in a 9-year-old boy. Cardiovasc Intervent Radiol 1999;22(1):67–8. [DOI] [PubMed] [Google Scholar]
- 13.Willner IR, El-Sakr R, Werkman RF, et al. A fistula from the portal vein to the bile duct: An unusual complication of transjugular intrahepatic portosystemic shunt. Am J Gastroenterol 1998;93(10):1952–5. [DOI] [PubMed] [Google Scholar]
- 14.Hüsing-Kabar A, Heinzow HS, Schmidt HH, et al. Single-operator cholangioscopy for biliary complications in liver transplant recipients. World J Gastroenterol 2017;23(22):4064–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Karagyozov P, Boeva I, Tishkov I. Role of digital single-operator cholangioscopy in the diagnosis and treatment of biliary disorders. World J Gastrointest Endosc 2019;11(1):31–40. [DOI] [PMC free article] [PubMed] [Google Scholar]