Abstract
Objective
Our study sought to determine whether there was a change in emergency department (ED) length of stay (LOS) during the coronavirus disease 2019 (COVID‐19) pandemic compared to prior years.
Methods
We performed a retrospective analysis using ED performance data 2018–2020 from 56 EDs across the United States. We used a generalized estimating equation (GEE) model to assess differences in ED LOS for admitted (LOS‐A) and discharged (LOS‐D) patients during the COVID‐19 pandemic period compared to prior years.
Results
GEE modeling showed that LOS‐A and LOS‐D were significantly higher during the COVID‐19 period compared to the pre‐COVID‐19 period. LOS‐A during the COVID‐19 period was 10.3% higher compared to the pre‐COVID‐19 time period, which represents a higher geometric mean of 28 minutes. LOS‐D during the COVID‐19 period was 2.8% higher compared to the pre‐COVID‐19 time period, which represents a higher geometric mean of 2 minutes.
Conclusions
ED LOS‐A and LOS‐D were significantly higher in the COVID‐19 period compared to the pre‐COVID‐19 period despite a lower volume of patients in the COVID‐19 period.
Keywords: COVID‐19, emergency department, length of stay
1. INTRODUCTION
1.1. Background
The coronavirus disease 2019 (COVID‐19) pandemic is an ongoing global crisis with far‐reaching consequences affecting every facet of life. As of April 21, 2021, there are more than 31.6 million confirmed cases in the United States, with 565,613 related deaths. 1 This has led to a significant stress on the healthcare system as a whole, with emergency departments (EDs) across the country taking the brunt of this stress given the fact that they are on the front line of the healthcare system. 2
1.2. Importance
It has been shown that the higher the volume of patients seen at an ED, the worse an ED's performance is in terms of length of stay (LOS), 3 , 4 which leads to overcrowding. ED overcrowding has a detrimental effect on patient morbidity and mortality in a variety of patient groups and cost to both the patient and the hospital. 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 Therefore, to combat this overcrowding, ED and hospital administrators will typically enact a surge protocol in times of predicted increased volumes, such as a pandemic. 2 However, unlike prior similar pandemics that presented with an initial surge, preliminary research from early in the pandemic actually demonstrated an unexpected steep decrease in ED volumes, 14 with a consequential expected improvement in ED LOS. 15 We presume that this led to confusion on the part of ED staff on how to further prepare their EDs for the current and future similar pandemics.
1.3. Goals of this investigation
To date, there has been limited research assessing the effects of the current COVID‐19 pandemic on ED performance as it relates to LOS. Our study therefore seeks to determine whether there was a significant change in ED LOS since the beginning of the COVID‐19 pandemic. Our study hypothesis was that reduced ED volumes seen during the COVID‐19 pandemic would be associated with a decrease in LOS for both discharged and admitted patients. We performed a retrospective analysis using ED performance data from 56 EDs across the United States, comparing ED LOS and ED volumes from before and after the first government‐mandated shutdowns on March 16, 2020. 16 We hope that these data will help EDs both in continuing to respond to the current pandemic and in future planning for a similar global health crisis.
2. METHODS
2.1. Study design and setting
This study was approved by the Arrowhead Regional Medical Center Institutional Review Board. This was a retrospective analysis that used ED LOS data from March 1 to December 31 in 2018, 2019, and 2020. Data were received from 56 EDs, encompassing 6,031,301 ED encounters. EDs in the study represented community hospitals from 5 different Centers for Medicare & Medicaid Services (CMS) regions in the same emergency medicine group. EDs in the study were contracted with a single physician group and provided timestamp data (ED arrival and ED departure timestamps) abstracted from their respective electronic medical record systems for both discharged and admitted patients, which are regularly monitored for the purposes of operational quality. In addition to timestamps, the data file also contained the patient's Emergency Severity Index (ESI) score and date of service. Individual hospitals provided data for all patients seen in their own ED via data files securely transferred (via secure file transfer protocol) to the physician group on a monthly basis. Data files are aggregated and stored in structured query language (SQL) databases for storage and querying purposes.
2.2. Measurements
Length of stay and ESI assessments were abstracted from hospital electronic medical records for each patient. Upon triaging, each patient is assigned an ESI number for prioritization purposes. Higher acuity patients are assigned an ESI level of “1” and lower acuity patients are assigned an ESI level of “5.” Our study used LOS, which the Emergency Department Benchmarking Alliance defines as “the interval from ED arrival to ED departure,” because it is a universally recognized metric of ED performance. 17 LOS was calculated from the point when patients were registered in the ED to when patients were discharged from the ED (LOS‐D) or when patients were moved to inpatient beds (LOS‐A). Patients who were transferred to another hospital were not included in the LOS‐A or LOS‐D metrics. In this study, we compared ED volumes on a monthly basis from March 2018 to December 2020, defining ED volume for a given month as the median number of ED encounters across all sites for that month.
For the purposes of the statistical analysis, the COVID‐19 period is defined as March 1, 2020 to December 31, 2020, and the pre‐COVID‐19 periods are defined as that same time period (March through December) in 2018 and 2019. Each month in the pre‐COVID‐19 period is compared to that same month in the COVID‐19 period in order to control for seasonal variability in LOS. For the pre‐COVID‐19 time period, data points include daily median LOS for March through December 2018 and March through December 2019 for all sites. For the COVID‐19 time period, data points include daily median LOS for all sites between March through December 2020.
The Bottom Line.
This retrospective analysis sought to determine whether emergency department length of stay changed during the COVID‐19 pandemic, based on data from 6 million visits at 56 sites from 2018–2020. A generalized estimating equation model found that length of stay increased by 10.3% for admitted patients and 2.8% for discharged patients, when comparing the pandemic with preceding years.
2.3. Outcomes
The goal of the study was to determine whether there was a change in ED LOS during the COVID‐19 pandemic time period compared to the previous time period. The primary outcome of this study was ED LOS, as defined by ED LOS for admitted patients (LOS‐A) and LOS for discharged patients (LOS‐D).
2.4. Analysis
Primary data analyses were conducted at the site level, meaning that individual patient data were aggregated at the site level. For analytic purposes, median times for each of the LOS metrics were calculated for each site per day as described previously. The analytic data set contains the site identifier, date of service, patient volume, median LOS‐A, median LOS‐D, and the percentage of patients in ESI levels 1 through 5 for each day. Using median values at the site level precludes the need for overcleansing of data to remove records because of aberrant low or high outlier values and is indicative of “typical” LOS times. A site must have at least 1 day of data in each of the months of the study time period in order to qualify for inclusion. A total of 56 sites were found to have data for each month of the study period.
Analysis to assess significance of differences in LOS times from pre‐COVID‐19 and COVID‐19 times was conducted using generalized estimating equation (GEE) models. GEE modeling was conducted using Python stats models module 0.12.0 (available at http://www.python.org). GEE models are a subset of generalized linear models and are used to adjust standard errors when there is correlation within or between observations. 18 GEE modeling is superior to the ordinary least squares (OLS) approach because it accounts for correlated data and corrects for clustering in the standard errors. The correlated data arise from both individuals clustered within EDs and data clustered longitudinally over time. Analysis of correlated data using OLS methods may result in artificially low variance and low P values. 19 The GEE uses maximum likelihood methods of estimating coefficients through a link function. The correlation or covariance structure must be determined a priori, although estimates are consistent despite incorrect specification. 18 An exchangeable correlation and gamma family structures are specified for these analyses and are appropriate where data are presented in clusters, longitudinally and where the dependent variable is presented as positive and continuous. 20
The GEE model contains variables that the researchers believe affect LOSs for both admitted and discharged patients, which include ED patient acuity and volumes. 4 , 21 , 22 Although controlling for these variables, the model tests for significance of the COVID‐19 time period compared to the pre‐COVID‐19 time period. The COVID‐19 time period is a categorical variable where “1” is the COVID‐19 time period and “0” is the pre‐COVID‐19 time period. ED patient volume is a continuous variable. ESI levels are presented as percentages of each of the 5 ESI levels. In the GEE model, we use the pre‐COVID‐19 time period and ESI level 5 as reference groups.
3. RESULTS
3.1. Characteristics of study subjects
Table 1 presents the characteristics of the encounters included in the study sample. There were slightly more females than males represented in the ED encounters (54.3% were female and 45.7% were male). The distribution of encounters among adult age groups was relatively similar, although there were more ED encounters among younger adult age groups (27.3% of all ED encounters were among 26–45 year olds, with 46–65 year olds and 65+ year olds representing 23.9% and 24.1% of ED encounters, respectively). The vast majority of ED encounters were for discharged (or outpatient) encounters (77.9%), and 19.3% of encounters were placed on observation status or admitted to inpatient beds in the hospital. The remaining 2.8% patients were transferred to another facility and, therefore, not included in the data as previously described. Similarly, breakdown by ESI levels corroborates discharge disposition data. Higher acuity patients (ESI levels 1 and 2) represented 15.9% of ED encounters, and lower acuity patients (ESI levels 3, 4, and 5) represented 83.1% of ED encounters (1% of encounters did not have an ESI level in the data file abstracted from emergency medical records).
TABLE 1.
Characteristics of emergency department encounters and description of hospital location for study sample (March through December 2018, 2019, 2020)
| Encounters (n) | Encounters (%) | |
|---|---|---|
| Gender | ||
| Female | 3,272,842 | 54.3% |
| Male | 2,758,459 | 45.7% |
| Disposition | ||
| Admit | 1,163,000 | 19.3% |
| Discharge | 4,698,491 | 77.9% |
| Transfer | 169,810 | 2.8% |
| ESI Level a | ||
| 1 | 53,435 | 0.9% |
| 2 | 904,956 | 15.0% |
| 3 | 3,234,974 | 53.6% |
| 4 | 1,596,915 | 26.5% |
| 5 | 179,082 | 3.0% |
| Age group | ||
| 0–13 years | 610,345 | 10.1% |
| 14–17 years | 182,962 | 3.0% |
| 18–25 years | 658,688 | 10.9% |
| 26–45 years | 1,649,217 | 27.3% |
| 46–64 years | 1,442,447 | 23.9% |
| 65+ years | 1,451,713 | 24.1% |
| CMS Region–regional office (56) | ||
| Region 3—Philadelphia | 141159 | 14.1% |
| Region 5—Chicago | 1346479 | 22.3% |
| Region 7—Kansas City | 51694 | 0.9% |
| Region 9—San Francisco | 4100531 | 68.0% |
| Region 10—Seattle | 391438 | 6.5% |
| Total | 6,031,301 | 100% |
aWithin each characteristic, total percentages may not sum up to 100 because of null values.
Abbreviations: CMS, Centers for Medicare & Medicaid Services; ESI, Emergency Severity Index.
The 56 ED facilities in the study represent 5 of the 10 CMS regions nationally. The majority of the ED encounters included in the study sample are from CMS Region 9—San Francisco (68.0%) followed by Region 5—Chicago (22.3%) (Table 1). All ED facilities were from community hospitals.
4. MAIN RESULTS
For the LOS‐A, the GEE results showed significant, positive relationships for the COVID‐19 period, ED encounters, and the percentages of patients who are ESI 1 and 2 (Table 2). This means that the LOS‐A was significantly longer during the COVID‐19 period compared to the pre‐COVID‐19 time period (Figure 1). Taking the exponentiated sum of the intercept and COVID‐19 estimates, LOS‐A was 28 minutes (geometric mean) longer during the COVID‐19 time period than during the pre‐COVID‐19 time period. Taking the exponent of the COVID‐19 estimate alone shows that, with all other variables being equal, patients in the COVID‐19 pandemic period showed a 10.3% higher LOS‐A than during the pre‐COVID‐19 time period.
TABLE 2.
Generalized estimating equation model for length of stay for admitted patients
| Estimate | SE | Z | P | |
|---|---|---|---|---|
| Intercept | 5.589 | 0.13 | 44.05 | *** |
| Pre‐COVID‐19 period | (Reference category) | |||
| COVID‐19 period | 0.098 | 0.02 | 6.11 | *** |
| ED encounters | 0.001 | 0.00 | 4.89 | *** |
| % ESI 1 | 0.007 | 0.00 | 2.67 | *** |
| % ESI 2 | 0.003 | 0.00 | 2.18 | ** |
| % ESI 3 | 0.000 | 0.00 | 0.08 | |
| % ESI 4 | 0.000 | 0.00 | ‐0.18 | |
| % ESI 5 | (Reference category) | |||
***P < 0.01; **P < 0.05; *P < 0.10.
Abbreviations: ED, emergency department; ESI, Emergency Severity Index.
FIGURE 1.
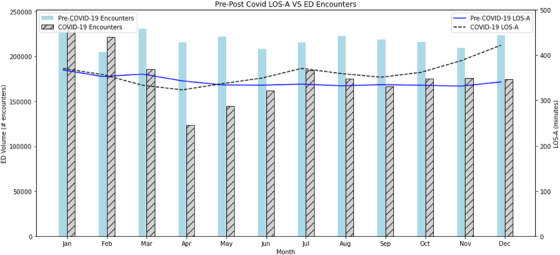
Emergency department volume by month with corresponding length of stay for admitted patients from 2018–2020. The pre‐COVID‐19 time period is an average of 2018 and 2019 data. The COVID‐19 time period is 2020 data. The vertical bars represent total monthly ED volume in a given month, measured in encounters in a single month. The horizontal lines represent length of stay measured in minutes. January and February data is represented for graphical purposes only. The GEE study data set contains only March through December data for 2018, 2019, and 2020. Abbreviations: ED, emergency department; GEE, generalized estimating equation; LOS‐A, length of stay, admitted
For the LOS‐D, the GEE results showed significant, positive relationships for the COVID‐19 period, ED encounters, and the percentages of patients who are ESI 1, 2, and 3 (Table 3). Similarly, the LOS‐D was significantly higher during the COVID‐19 period by 2 minutes (geometric mean) compared to the pre‐COVID‐19 time period (Figure 2). Taking the exponent of the COVID‐19 estimate alone shows that, with all other variables being equal, patients in the COVID‐19 pandemic period demonstrated a 2.8% higher LOS‐D than during the pre‐COVID‐19 time period.
TABLE 3.
Generalized estimating equation model for length of stay for discharged patients
| Estimate | SE | z | P | |
|---|---|---|---|---|
| Intercept | 4.297 | 0.08 | 53.74 | *** |
| Pre‐COVID 19 period | (Reference category) | |||
| COVID‐19 period | 0.028 | 0.01 | 3.35 | *** |
| ED encounters | 0.002 | 0.00 | 9.13 | *** |
| % ESI 1 | 0.015 | 0.00 | 9.32 | *** |
| % ESI 2 | 0.010 | 0.00 | 9.31 | *** |
| % ESI 3 | 0.007 | 0.00 | 8.87 | *** |
| % ESI 4 | 0.001 | 0.00 | 1.72 | |
| % ESI 5 | (Reference category) | |||
***P < 0.01; **P < 0.05; *P < 0.10.
Abbreviations: ED, emergency department; ESI, Emergency Severity Index.
FIGURE 2.
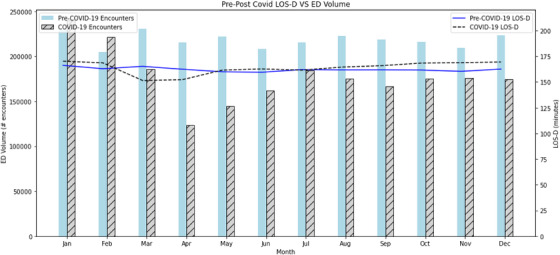
Emergency department volume by month with corresponding length of stay for discharged patients from 2018–2020. The pre‐COVID‐19 time period is an average of 2018 and 2019 data. The COVID‐19 time period is 2020 data. The vertical bars represent total monthly ED volume in a given month, measured in encounters in a single month. The horizontal lines represent length of stay measured in minutes. January and February data is represented for graphical purposes only. The GEE study data set contains only March through December data for 2018, 2019, and 2020. Abbreviations: ED, emergency department; GEE, generalized estimating equation; LOS‐D, length of stay, discharged
5. LIMITATIONS
One limitation of this study is that we were unable to collect any inpatient data from our study hospitals specifically regarding inpatient bed availability and the percentage of inpatient beds occupied by patients with COVID‐19, a metric that has previously been shown in several studies to strongly affect LOS‐A. 23 , 24 Instead, we did attempt to address this by taking data from the US Department of Health and Human Services (HHS) and the COVID Tracking Project in order to explain the increase in LOS‐A as a function of ED volume. 25 , 26 , 27 Another limitation is that we were unable to collect data regarding nurse staffing, specifically nursing hours worked as a function of time, number of furloughs, and number of nursing call‐offs. Having such data may have been useful in determining if and how much nurse staffing had any correlation with LOS. Lastly, it should be noted that our data comes from only 5 of 10 CMS regions, the majority (68%) of which are from region 9 (San Francisco), which could potentially threaten the external validity of this study.
6. DISCUSSION
As has been seen in prior literature, our study found a precipitous reduction in ED patient volumes from March 2020 onward when compared to the previous 2 years (Figures 1 and 2). 14 Given that ED patient volumes has been shown to increase LOS, 4 we hypothesized that a reduction in ED volume amid the COVID‐19 pandemic would correlate with a reduction in LOS‐A and LOS‐D. On the contrary, the GEE showed that both ED LOS‐A and LOS‐D had significantly increased during the COVID‐19 period.
During the first 2 months of the COVID‐19 period (March and April 2020), LOS‐A and LOS‐D actually decreased more than in the pre‐COVID‐19 period (Figures 1 and 2). There are several possibilities for this observation. First, in preparation for a surge of patients with COVID‐19, many EDs constructed medical tents outside the department for rapid triage and treatment of patients with suspected COVID‐19. 28 , 29 Second, many hospitals across the United States cancelled or postponed elective surgeries in March and April to preserve inpatient beds, 30 which could have decreased the LOS‐D, as elective surgical admissions have been shown to be associated with prolonged ED LOS. 31 However, despite hospitals and EDs taking these precautions, ED volumes dropped by 40%–60% in March and April of 2020. 14 , 21 , 32 Third, ED staffing remained at prepandemic levels during those same months, which led to more staff being available to care for fewer patients. 22 , 28 As has been shown before by Ramsey et al., 29 there is a direct relationship between ED nurse staffing and LOS; the more nursing hours, the shorter the LOS.
As the pandemic continued into May and beyond, LOS‐A and LOS‐D increased above the levels as expected from the pre‐COVID‐19 period, and this trend continued for the remainder of 2020 (Figures 1 and 2). One of the biggest contributing factors to this trend may have been hospital overcrowding due to rising COVID‐19 admission rates. Based on data from the HHS and the COVID Tracking Project, the rates of inpatient hospitalization due to COVID‐19 rose across the United States in April and May 2020. 25 , 26 , 27 This has likely contributed to a nationwide reduction in inpatient bed availability, which numerous studies have shown to have the strongest correlation with ED LOS‐A 23 , 24 ; the less inpatient bed availability, the longer the LOS‐A.
Changes in the proportion of high versus low acuity ED encounters during the pandemic also may have contributed to an increase in LOS. The GEE showed that an increase in the number of ESI 1 and 2 level encounters was associated with an increase in LOS‐D, with an even stronger associated increase with LOS‐A (Tables 2 and 3). This finding can be corroborated by multiple prior studies looking at ESI as it relates to LOS. 33 , 34 A prior study by Lucero et al. using a very similar cohort of EDs found that the proportion of ESI 1 and 2 encounters increased by 2.4% after March 16, 2020, 14 suggesting that a proportional increase in lower ESI encounters may have contributed to an increase in LOS.
Infection control measures, although necessary, also may have had detrimental effects on ED LOS. For example, hospitals limiting visitation may have delayed the ability to obtain collateral information and have goals of care discussions, therefore keeping patients in the ED for longer periods of time. 35 , 36 , 37 , 38 New COVID‐19 testing protocols for patients arriving by ambulance before entering the ED may have delayed emergency medical services offloading times. 29 Decontaminating imaging rooms and the proper donning and doffing of personal protective equipment create inherent delays in care. 29 , 39
The financial strain of preparing ED and inpatient units for the COVID‐19 pandemic may have also put pressure on hospitals to cut down on staffing. The unexpected drop in patient volume, coupled with suspending elective procedures, resulted in a lost income of $202 billion to hospitals, with a projected additional loss of $120 billion through December, according to the American Hospital Association. 40 , 41 , 42 Outdoor tent triage and treatment systems, although necessary, were costly, with 1 hospital system citing a cost of $100,000 per tent. 28 All of these factors combined put financial pressure on hospitals, eventually forcing them to furlough both inpatient and ED staff in an attempt to ameliorate further financial losses. 41 , 43 , 44 , 45 , 46 More than 1.5 million healthcare jobs were lost from February through April 2020. 47 To further complicate this issue, healthcare workers are at significantly increased risk of becoming exposed to and/or contracting COVID‐19, 48 meaning that at any given time, a certain number of staff members will likely be unable to work due to either illness or the need to quarantine. If staff members are furloughed, there is a smaller pool available to cover sick call‐outs. This leads to decreased nursing hours, which has already been shown to further increase ED LOS. 49
In summary, ED LOS‐A and LOS‐D increased during the COVID‐19 pandemic when compared to previous years, which is particularly concerning given that ED volumes have dropped by as much as 60% at their nadir. 14 , 32 A myriad of factors may have ultimately contributed to this finding, many of which are either directly related or done in response to the COVID‐19 pandemic. However, it is difficult to draw any direct conclusions about their effect on ED LOS given the retrospective design of this study.
CONFLICTS OF INTEREST
No conflicts of interest exist for any of the authors listed.
AUTHOR CONTRIBUTIONS
All authors conceived the study. JL obtained institutional review board approval. AL and KS drafted the abstract. AL, KS, and ED drafted the introduction, JH and LP drafted the methods and results sections, and JL and CK drafted the limitations and discussion sections. AL, KS, and GM contributed substantially to its revision. AL takes responsibility for the paper as a whole.
Biography
Anthony Lucero, MD, is an Emergency Medicine specialist at Kaweah Health Medical Center in Visalia, California.

Lucero A, Sokol K, Hyun J, et al. Worsening of Emergency Department Length of Stay during the COVID‐19 Pandemic. JACEP Open. 2021;2:e12489. 10.1002/emp2.12489
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
Supervising Editor: Nathan Hoot, MD, PhD
REFERENCES
- 1. Centers for Disease Control and Prevention . Cases in the US. 2020. Centers for Disease Control and Prevention. Available at: https://covid.cdc.gov/covid‐data‐tracker Accessed October 14, 2020. [Google Scholar]
- 2. Sugarman D, Nadeau KH, Lafond K. A survey of emergency department 2009 pandemic influenza A (H1N1) surge preparedness – Atlanta, Georgia, July‐October 2009. Clin Infect Dis. 2011;52(Suppl 1):S177‐S182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Welch SJ, Augustine JJ, Dong L, et al. Volume‐related differences in emergency department performance. Jt Comm J Qual Patient Saf. 2012;38(9):395‐402. [DOI] [PubMed] [Google Scholar]
- 4. Handel DA, Fu R, Vu E, et al. Association of emergency department and hospital characteristics with elopements and length of stay. J Emerg Med. 2014;46(6):839‐846. [DOI] [PubMed] [Google Scholar]
- 5. Sun BC, Hsia RY, Weiss RE, et al. Effect of emergency department crowding on outcomes of admitted patients. Ann Emerg Med. 2013;61(6):605‐611. e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jo S, Jin YH, Lee JB, et al. Emergency department occupancy ratio is associated with increased early mortality. J Emerg Med. 2014;46(2):241‐249. [DOI] [PubMed] [Google Scholar]
- 7. Jo S, Jeong T, Jin YH, et al. ED crowding is associated with inpatient mortality among critically ill patients admitted via the ED: post hoc analysis from a retrospective study. Am J Emerg Med. 2015;33(12):1725‐1731. [DOI] [PubMed] [Google Scholar]
- 8. Richardson DB. Increase in patient mortality at 10 days associated with emergency department overcrowding. Med J Aust. 2006;184(5):213‐216. [DOI] [PubMed] [Google Scholar]
- 9. Zhang Z, Bokhari F, Guo Y, et al. Prolonged length of stay in the emergency department and increased risk of hospital mortality in patients with sepsis requiring ICU admission. Emerg Med J. 2019;36(2):82‐87. [DOI] [PubMed] [Google Scholar]
- 10. Mowery NT, Dougherty SD, Hildreth AN, et al. Emergency department length of stay is an independent predictor of hospital mortality in trauma activation patients. J Trauma. 2011;70(6):1317‐1325. [DOI] [PubMed] [Google Scholar]
- 11. Guttmann A, Schull MJ, Vermeulen MJ, et al. Association between waiting times and short term mortality and hospital admission after departure from emergency department: population based cohort study from Ontario. Canada BMJ. 2011;342:d2983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Berg LM, Ehrenberg A, Florin J, et al. Associations between crowding and ten‐day mortality among patients allocated lower triage acuity levels without need of acute hospital care on departure from the emergency department. Ann Emerg Med. 2019;74(3):345‐356. [DOI] [PubMed] [Google Scholar]
- 13. Cha WC, Shin SD, Cho JS, et al. The association between crowding and mortality in admitted pediatric patients from mixed adult‐pediatric emergency departments in Korea. Pediatr Emerg Care. 2011;27(12):1136‐1141. [DOI] [PubMed] [Google Scholar]
- 14. Lucero AD, Lee A, Hyun J, et al. Underutilization of the emergency department during the COVID‐19 pandemic. West J Emerg Med. 2020;21(6):15‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cohen BA, Wessling EG, Serina PT, et al. Emergency department operations in a large health system during COVID‐19. Am J Emerg Med. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Moreland A, Herlihy C, Tynan MA, et al. Timing of state and territorial COVID‐19 stay‐at‐home orders and changes in population movement: United States, March 1‐May 31, 2020. MMWR. 2020;69(35):1198‐1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yiadom MYAB, Napoli A, Granovsky M, et al. Managing and measuring emergency department care: results of the fourth emergency department benchmarking definitions summit. Acad Emerg Med. 2020;27(7):600‐611. [DOI] [PubMed] [Google Scholar]
- 18. Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42(1):121‐130. [PubMed] [Google Scholar]
- 19. Hanley JA, Negassa A, Edwardes MD, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 2003;157:364‐375. [DOI] [PubMed] [Google Scholar]
- 20. Hardin JW, Hilbe JM. Generalized Estimating Equations. Boca Raton, FL: Chapman & Hall/CRC; 2003. [Google Scholar]
- 21. Butt AA, Azad AM, Kartha AB, et al. Volume and acuity of emergency department visits prior to and after COVID‐19. J Emerg Med. 2020;59(5):730‐734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Whiteside T, Kane E, Aljohani B, et al. Redesigning emergency department operations amidst a viral pandemic. Am J Emerg Med. 2020;38(7):1448‐1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Forster AJ, Stiell I, Wells G, Lee AJ, van Walraven C. The effect of hospital occupancy on emergency department length of stay and patient disposition. Acad Emerg Med. 2003;10(2):127‐133. [DOI] [PubMed] [Google Scholar]
- 24. Lucas R, Farley H, Twanmoh J, et al. Emergency department patient flow: the influence of hospital census variables on emergency department length of stay. Acad Emerg Med. 2009;16(7):597‐602. [DOI] [PubMed] [Google Scholar]
- 25. Estimated U.S . Hospital Utilization. HHS Protect Public Data Hub. https://protect‐public.hhs.gov/pages/hospital‐capacity Updated December 4, 2020. Accessed December 8, 2020. [Google Scholar]
- 26. The COVID‐19 Tracking Project. Covidtracking.com. https://covidtracking.com/data#summary‐charts. Updated December 7, 2020. Accessed December 8, 2020.
- 27. Barten DG, Kusters RWJ, Peters NAR. A swift and dynamic strategy to expand emergency department capacity for COVID‐19. Disaster Med Public Health Prep. 2020:1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Noble J, Degesys NF, Kwan E, et al. Emergency department preparation for COVID‐19: accelerated care units. Emerg Med J. 2020;37(7):402‐406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Miller GA, Buck CR, Kang CS, et al. COVID‐19 in Seattle‐Early lessons learned. J Am Coll Emerg Physicians Open. 2020;1(2):85‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Meredith JW, High KP, Freischlag JA. Preserving elective surgeries in the COVID‐19 pandemic and the future. JAMA. 2020;324(17):1725‐1726. [DOI] [PubMed] [Google Scholar]
- 31. Rathlev NK, Chessare J, Olshaker J, et al. Time series analysis of variables associated with daily mean emergency department length of stay. Ann Emerg Med. 2007;49(3):265‐271. [DOI] [PubMed] [Google Scholar]
- 32. Jeffery MM, D'Onofrio G, Paek H, et al. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the COVID‐19 pandemic in the US. JAMA Intern Med. 2020;180(10):1328‐1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Schull MJ, Kiss A, Szalai JP. The effect of low‐complexity patients on emergency department waiting times. Ann Emerg Med.. 2007;49(3):257‐264. 264.e1. [DOI] [PubMed] [Google Scholar]
- 34. Hocker MB, Gerardo CJ, Theiling BJ, et al. NHAMCS validation of Emergency Severity Index as an indicator of emergency department resource utilization. West J Emerg Med. 2018;19(5):855‐862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Siddiqi H. To suffer alone: hospital visitation policies during COVID‐19. J Hosp Med. 2020;11:694‐695. [DOI] [PubMed] [Google Scholar]
- 36. Navathe A, Liao J. Physician viewpoint: COVID‐19 visitor restrictions may hurt more than they help. The Philadelphia Inquirer. 2020. July 28. [Google Scholar]
- 37. Rosenbaum L. The untold toll: the pandemic's effects on patients without COVID‐19. N Engl J Med. 2020;382(24):2368‐2371. [DOI] [PubMed] [Google Scholar]
- 38. Glover RE, Van Schalkwyk ME, Akl EA, et al. A framework for identifying and mitigating the equity harms of COVID‐19 policy interventions. J Clin Epidemiol. 2020;128:35‐48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. ACR Recommendations for the use of Chest Radiography and Computed Tomography (CT) for Suspected COVID‐19 Infection. American College of Radiology website. https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection. Accessed November 6, 2020. [Google Scholar]
- 40. Hospitals and Health Systems Continue to Face Unprecedented Financial Challenges due to COVID‐19. American Hospital Association website. https://www.aha.org/system/files/media/file/2020/06/aha-covid19-financial-impact-report.pdf. Accessed December 8, 2020. [Google Scholar]
- 41. Respaut R, Spalding RUS. Hospitals halt lucrative procedures amid coronavirus crisis, job cuts follow. Reuters website. https://www.reuters.com/article/us-health-coronavirus-usa-hospitals/u-s-hospitals-halt-lucrative-procedures-amid-coronavirus-crisis-job-cuts-follow-idUSKBN21I388?utm_source=rss&utm_medium=rss. Accessed December 8, 2020. [Google Scholar]
- 42. Diaz A, Sarac BA, Schoenbrunner AR, et al. Elective surgery in the time of COVID‐19. Am J Surg. 2020;219(6):900‐902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Mellnik T, Karklis L, Ba Tran A. Americans are delaying medical care, and it's devastating health‐care providers. The Washington Post website. https://www.washingtonpost.com/nation/2020/06/01/americans-are-delaying-medical-care-its-devastating-health-care-providers/?arc404=true. Published June 2, 2020. Accessed November 4, 2020. [Google Scholar]
- 44. Paavola A. 266 hospitals furloughing workers in response to COVID‐19: many U.S. hospitals and health systems have suspended elective procedures to save capacity, supplies and staff to treat COVID‐19 patients. Beckers Hospital Review website. https://www.beckershospitalreview.com/finance/49-hospitals-furloughing-workers-in-response-to-covid-19.html. Accessed November 4, 2020. [Google Scholar]
- 45. Paavola A. 12 hospitals laying off workers in response to COVID‐19: To address the financial fallout from the COVID‐19 pandemic, hospitals across the nation are looking to cut costs by implementing furloughs, layoffs or pay cuts. Beckers Hospital Review website. https://www.beckershospitalreview.com/finance/12-hospitals-laying-off-workers-in-response-to-covid-19.html. Published July 2, 2020. Accessed November 4, 2020. [Google Scholar]
- 46. Ellison A. Financial fallout from COVID‐19: 9 hospitals laying off workers. The financial challenges caused by the COVID‐19 pandemic have forced hundreds of hospitals across the nation to furlough, lay off or reduce pay for workers, and others have had to scale back services or close. Beckers Hospital Review website. https://www.beckershospitalreview.com/finance/financial-fallout-from-covid-19-9-hospitals-laying-off-workers.html. Published September 22, 2020. Accessed November 4, 2020. [Google Scholar]
- 47. McDermott D, Cox C. What impact has the coronavirus pandemic had on healthcare employment?. Health System Tracker website. https://www.healthsystemtracker.org/chart-collection/what-impact-has-the-coronavirus-pandemic-had-on-healthcare-employment/#item-start. Published June 16, 2020. Accessed December 19, 2020. [Google Scholar]
- 48. Nguyen LH, Drew DA, Graham MS, et al. Risk of COVID‐19 among front‐line health‐care workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5(9):E475‐E483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Ramsey Z, Palter JS, Hardwick J, et al. Decreased nursing staffing adversely affects emergency department length of stay metrics. West J Emerg Med. 2018;19(3):496‐500. [DOI] [PMC free article] [PubMed] [Google Scholar]


