Key Points
We describe a 30-year-old woman who developed thrombocytopenia and multiple thromboses after she received the ChAdOx1 nCoV-19 vaccine.
A maximum 4T HIT score and a positive immunoassay for anti-PF4 antibodies indicated autoimmune HIT as a potential pathogenic mechanism.
Abstract
Recently, reports of severe thromboses, thrombocytopenia, and hemorrhage in persons vaccinated with the chimpanzee adenovirus-vectored vaccine (ChAdOx1 nCoV-19, AZD1222, Vaxzevria; Oxford/AstraZeneca) against severe acute respiratory syndrome coronavirus 2 have emerged. We describe an otherwise healthy 30-year-old woman who developed thrombocytopenia, ecchymosis, portal vein thrombosis, and cerebral venous sinus thrombosis the second week after she received the ChAdOx1 nCoV-19 vaccine. Extensive diagnostic workup for thrombosis predispositions showed heterozygosity for the prothrombin mutation, but no evidence of myeloproliferative neoplasia or infectious or autoimmune diseases. Her only temporary risk factor was long-term use of oral contraceptive pills (OCPs). Although both the prothrombin mutation and use of OCPs predispose to portal and cerebral vein thrombosis, the occurrence of multiple thromboses within a short time and the associated pattern of thrombocytopenia and consumption coagulopathy are highly unusual. A maximum 4T heparin-induced thrombocytopenia (HIT) score and a positive immunoassay for anti-platelet factor 4/heparin antibodies identified autoimmune HIT as a potential pathogenic mechanism. Although causality has not been established, our case emphasizes the importance of clinical awareness. Further studies of this potentially new clinical entity have suggested that it should be regarded as a vaccine-induced immune thrombotic thrombocytopenia.
Introduction
In the midst of the COVID-19 pandemic, several national health authorities across Europe decided to pause the administration of the chimpanzee adenovirus-vectored vaccine1 (ChAdOx1nCoV-19, AZD1222; Vaxzevria; Oxford/AstraZeneca) for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), after sporadic reports of severe cases of thrombocytopenia, bleeding, or thrombosis invaccinated individuals.2 We present a likely case and elaborate on the diagnostic and clinical course. This report is in accordance with the principles of the Declaration of Helsinki.
Case description and results
A 30-year-old woman presented with a 3-day history of headache and general malaise. Her medical history included migraine and her only regular medication was a third-generation (low thrombosis risk) estrogen/progestin oral contraceptive pill (OCP) taken for years. She had no history of autoimmune disease, venous thromboembolism, bleeding, or known genetic predisposition thereto and no prior exposure to heparin. She was prioritized for vaccination because of occupational risk of SARS-CoV-2 infection and received the first dose of ChAdOx1 nCoV-19 8 days before the onset of symptoms. Findings in her physical examination were unremarkable, and her body mass index was 22 kg/m2. She tested negative for SARS-CoV-2. Blood tests revealed thrombocytopenia (51 × 109/L), but no other remarkable findings (Table 1). Results of noncontrast computed tomography (CT) scan of the head were normal. Migraine treatment improved her symptoms, and she was discharged with referral to the hematology outpatient clinic.
Table 1.
Laboratory results of a patient presenting with thrombocytopenia and multiple thromboses after vaccination with ChAdOx1 nCoV-19
| 11 | 14 | 15 | 16 | 17 | 18 | 19 | |
|---|---|---|---|---|---|---|---|
| Hematology | |||||||
| Hemoglobin, g/dL (ref., 11.8-15.3) | 13.4 | 13.9 | 13.7 | 12.3 | 11.6 | 11.5 | 10.8 |
| Platelets, ×109/L (ref., 145-390) | 57 | 56 | 70 | 88 | 119 | 159 | 187 |
| Platelets, citrate, ×109/L (ref., 145-390) | 39 | 46 | |||||
| Leukocytes, ×109/L (ref., 3.-8.8) | 11.0 | 11.0 | 11.0 | 10.3 | 12.1 | 10.1 | 9.1 |
| Basophils, ×109/L (ref., 0.01-0.10) | 0.05 | 0.07 | 0.07 | 0.11 | 0.06 | — | — |
| Eosinophils, ×109/L (ref., 0.01-0.5) | 0.27 | 0.20 | 0.36 | 0.51 | 0.71 | — | — |
| Monocytes, ×109/L (ref., 0.2-0,80) | 0.98 | 0.71 | 1.13 | 1.10 | 0.88 | — | — |
| Neutrophils, ×109/L (ref., 1.6-5.9) | 6.25 | 4.51 | 4.45 | 6.10 | 4.02 | — | — |
| Lymphocytes, ×109/L (ref., 1.0-3.5) | 3.42 | 5.61 | 4.99 | 4.93 | 5.26 | — | — |
| D-dimer, mg/L FEU (ref., <0.5) | — | >20 | 12 | 5.9 | 4.1 | 1.6 | 1.2 |
| CRP, mg/L (ref., <10) | 36 | 19 | 14 | 18 | 21 | 26 | 22 |
| Hemostasis | |||||||
| INR | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.1 | 1.0 |
| Clotting factors II, VII, X (ref., >0.60) | 0.91 | 1.01 | 1.11 | 1.05 | 0.99 | 0.90 | 0.97 |
| aPTT, s (ref., 25-37) | — | 38 | 39 | 36 | 38 | 40 | 43 |
| Plasma fibrinogen, mg/dL (ref., 180-350) | — | 78 | 85 | 139 | 176 | 244 | 244 |
| ADAMTS13 protein, kIU/L (ref., 0.61-1.31) | — | — | — | 1.07 | — | — | — |
| Thrombophilia | |||||||
| Homocysteine, μmol/L (ref., <15.0) | — | — | — | 6.2 | — | — | — |
| Antithrombin, ×103IU/L (ref., 0.83-1.15) | — | 0.99 | 1.03 | 0.95 | 1.04 | 1.13 | 1.12 |
| Protein C, ×103 IU/L (ref., 0.70-1.30) | — | — | — | 1.20 | — | — | — |
| Protein S, ×103 IU/L (ref., 0.57-1.30) | — | — | — | 0.85 | — | — | — |
| Factor V Leiden R506Q mutation | — | — | — | Not detected | — | — | — |
| Prothrombin gene mutation (G20210A) | — | — | — | Heterozygous | — | — | — |
| Lupus anticoagulant | — | — | — | NA* | — | — | — |
| Cardiolipin IgG/IgM, ×103 IU/L (ref., <10.0) | — | — | — | 2.2/2.5 | — | — | — |
| β-2-GP1 IgG/IgM, kU/L (ref., 0-10) | — | — | — | <0.6 /<0.9 | — | — | — |
| Organ marker | |||||||
| ALT, U/L (ref., 10-45) | 29 | 61 | — | 134 | 123 | 115 | 95 |
| Serology | |||||||
| SARS-CoV-2, spike protein IgG, AU/mL (ref., 34-280) | — | — | — | 20.8 | — | — | — |
| SARS-CoV-2, nucleoprotein IgG (ref., <1.0) | — | — | — | <0.070 | — | — | — |
| Cytomegalovirus IgG/IgM | — | — | — | Pos/neg | — | — | — |
| Ebstein-Barr virus IgG/IgM | — | — | — | Pos/neg | — | — | — |
| Hepatitis A, hepatitis B s-Ab/s-Ag, hepatitis C | — | — | — | Neg | — | — | — |
| HIV1 and HIV2 (Ag+Ab) | — | — | — | Neg | — | — | — |
| Parvovirus B19 IgG /IgM | — | — | — | Pos/neg | — | — | — |
| Polymerase chain reaction | |||||||
| SARS-CoV-2 (oropharyngeal swab) | — | Neg | — | Neg | — | — | — |
| Influenza type A+B, adenovirus, metapneumovirus, parainfluenza, respiratory syncytial virus and rhinovirus (oropharyngeal swab) | — | — | — | Neg | — | — | — |
| Bacterial and viral meningitis panel (cerebrospinal fluid)† | — | Neg | — | — | — | — | — |
| Immunology | |||||||
| C3, g/L (ref., 0.811-1.570) | — | — | — | 1.42 | — | — | — |
| C4, g/L (ref., 0.129-0.392) | — | — | — | 0.345 | — | — | — |
| Antinuclear IgG (ref., <0.1) | — | — | — | 0.1 | — | — | — |
| Anti–double-stranded DNA IgG, kIU/L (ref., < 10) | — | — | — | 3.7 | — | — | — |
| Anti-Smith, anti-(U1) snRNP, anti-SSA, anti-SSB, anti-scl-70, anti-Jo1, anti-MPO, anti-PR3, anti-glomerular basement membrane, and immunoglobulin G | — | — | — | Neg | — | — | — |
Ab, antibody, Ag, antigen; ALT, alanine aminotransferase; anti-MPO, anti-myeloperoxidase; anti-PR3, anti-proteinase 3; aPTT, activated partial thromboplastin time; CRP, C-reactive protein; FEU, fibrinogen equivalent units; INR, international normalized ratio; PCR, polymerase chain reaction; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Lupus anticoagulant could not be assessed because of the heparinization of the blood.
No growth on cultures, and PCR testing for a panel of 14 pathogens was negative (BioFire FilmArray Meningitis-Encephalitis (ME) Panel; bioMérieux).
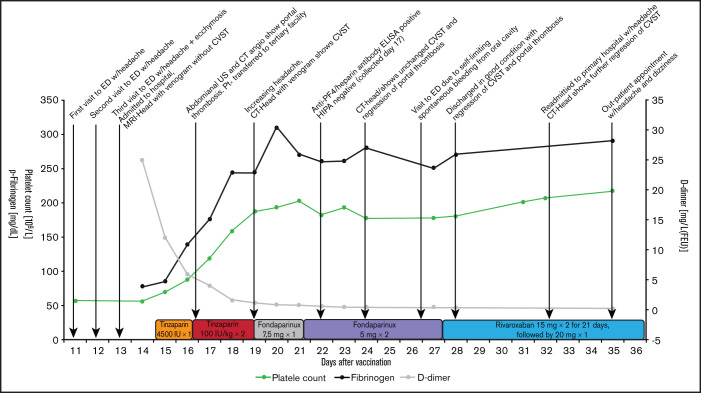
Two days later, she was readmitted for persistent headache and occurrence of ecchymosis. Blood tests showed thrombocytopenia and consumption coagulopathy with low levels of fibrinogen, high D-dimer, and marginally increased alanine aminotransferase (Figure 1). Thrombelastography demonstrated normal clot initiation, but decreased clot amplification and strength, reflecting decreased thrombin generation, low levels of fibrinogen, and reduced platelet function. A peripheral blood smear showed normal red blood cell morphology without the presence of schistocytes and a normal white blood cell count, but a reduced number of normal-sized platelets, including a few platelet aggregates.
Figure 1.
Timeline from presentation of first symptoms 8 days after vaccination with the ChAdOx1 nCoV-19 vaccine to outpatient postvaccination follow-up day 35. Serial coagulation test results are shown: platelet counts, D-dimer, and fibrinogen. Time points for the result of the anti-PF4 antibody test and key clinical events, including timing of thrombosis events and changes in anticoagulant treatment, are also shown. ED, emergency department; MRI, magnetic resonance imaging; ELISA, enzyme-linked immunosorbent assay; HIPA, heparin-induced platelet activation; FEU, fibrinogen equivalent units.
Magnetic resonance imaging of the head with venogram ruled out intracranial pathology, including cerebral venous sinus thrombosis (CVST). Analysis of the cerebrospinal fluid ruled out meningitis.
On clinical suspicion that the rare prothrombotic disorder being reported was associated with the ChAdOx1 nCoV-19 vaccine, prophylaxis with tinzaparin 4500 IU once daily was initiated.
Because of the coagulopathy, extended examination for thrombosis was performed. Duplex ultrasonography of the lower extremities and CT pulmonary angiography produced normal results. In contrast, duplex ultrasonography of the abdomen and confirmatory CT abdominal angiography demonstrated portal vein thrombosis. Anticoagulant treatment was intensified to tinzaparin 100 IU/kg twice daily, fibrinogen substitution targeting 100 mg/dL was given at a single occasion initially to ensure a noncritical level of fibrinogen to prevent bleeding, and the patient was transferred to a tertiary hospital, where extended laboratory workup, including anti-platelet factor 4/heparin (anti-PF4) antibody testing, was initiated upon arrival.
During the following 2 days, the symptoms improved in parallel with a gradual increase in platelet counts and improvement of coagulation parameters (Figure 1). Repeated ultrasonography showed no progression of the portal vein thrombosis. On the third day after initiation of therapeutic tinzaparin treatment the headache intensified, and cerebral CT venography demonstrated newly developed CVST. There were no signs of cerebral venous stasis, infarction, or bleeding. Risk scoring by the 4T HIT scale gave a maximum score of 8 and thus a high probability of autoimmune heparin-induced thrombocytopenia (aHIT).3 Accordingly, tinzaparin was replaced with fondaparinux 7.5 mg once daily, and the dose was increased 2 days later to 5 mg twice daily, based on anti-factor Xa monitoring.4 The patient was discharged after 15 days of hospitalization where rivaroxaban was prescribed upon discharge. Follow-up CT venography demonstrated regression of the CVST and portal vein thrombosis, and the patient recovered without major sequelae, although dizziness and light headache persisted.
Blood tests showed no signs of hemolysis, repeated peripheral blood smears were without the presence of schistocytes, a direct anti-globulin test was negative, and normal activity of ADAMTS13 (1.07 kIU/L) ruled out thrombotic thrombocytopenic purpura. The blood type was O RhD-positive. Increased levels of both factor VIII and von Willebrand factor were detected, consistent with signs of endothelial cell activation.
Assessment for inherited and acquired thrombophilia including myeloproliferative neoplasia, analyzed by an in-house myeloid malignancy gene panel using targeted next-generation sequencing, showed heterozygosity for the prothrombin G20210A mutation; otherwise. no variants were found (Table 1).
Anti-nuclear antibodies and anti-neutrophil cytoplasmatic antibodies were negative. Complement screening analysis (Complement System Screen WIESLAB; Euro-Diagnostica, Malmö, Sweden) demonstrated severely decreased activation of the classic pathway and slightly decreased activation of the lectin pathway, consistent with antibody-mediated consumption of complement proteins. Concentrations of complement C3 and C4 were within normal range.
Anti-platelet antibodies were detected against glycoprotein GPIIb-IIIa and GPIa-IIa but were inconclusive regarding human platelet–specific antibodies (Pak Lx Assay; Immucor, Waukesha, WI).
The HLA-type was A32,33; B14,44; C04,08; DRB1*01,11; DQB1*03:01,05; and DPB1*02:01,04:01 (polymerase chain reaction; QTYPE SSP; CareDX, Stockholm, Sweden). An extensive infectious disease workup was performed and returned negative results (Table 1).
At day 22 after vaccination, an enzyme-linked immunosorbent assay confirmed the presence of IgG antibodies to PF4-polyanion complexes, as indicated by an optical density of 2.2 (upper limit of normal, ≤0.4 (LIFECODES PF4 IgG by Immucor, Norcross, Georgia).5 A heparin-induced platelet activation assay was negative. The blood test for the anti-PF4 assay was performed 36 hours after initiation of tinzaparin.
Discussion
We report a case of a previously healthy young woman who presented with thrombocytopenia, ecchymosis, consumption coagulopathy, portal vein thrombosis, and a CVST the second week after administration of the ChAdOx1 nCoV-19 vaccine. An extensive diagnostic workup showed heterozygosity for the prothrombin mutation, which increases risk of venous thrombosis by ∼1.5-fold,6 with a further increase in risk when the vaccine is used in combination with OCP,7 although this risk decreases with duration of use and choice of third-generation OCPs.8 We found no evidence of myeloproliferative neoplasia or infectious or autoimmune disease. Both prothrombin mutation and use of OCP predispose to portal vein thrombosis and CVST, but the occurrence of several thromboses within a short time, despite therapeutic anticoagulation, and the associated pattern of thrombocytopenia and consumption coagulopathy, are unusual and support the notion of a highly prothrombotic state. Finally, the finding of anti-PF4 antibodies in a patient without prior heparin exposure entails other potential explanations.
HIT is an acquired prothrombotic disorder characterized by thrombocytopenia, coagulopathy, and a high risk of thrombosis9,10 that is induced by antibodies targeting neoepitopes formed by the binding of PF4 to heparin.11,12 Binding of these immune complexes to platelet FcγRIIa receptors leads to platelet activation, degranulation, NETosis, and endothelial activation, further aggravated by activation of the complement system.13
Autoimmune HIT, or spontaneous HIT, refers to a disorder clinically and serologically indistinguishable from HIT, but without prior exposure to heparin.14‐16 The pathophysiological background is incompletely understood, but it is hypothesized to be caused by other polyanions complexing with PF4-forming antigens to which anti-PF4/polyanion antibodies can bind. Several case reports have described aHIT caused by nonheparin triggers.17‐19
A maximum 4T HIT risk score gave a high predicted probability of HIT, and the demonstration of anti-PF4 antibodies by an immunoassay supported the diagnosis aHIT. The HLA-types DRB1*11 and DQB1*03:01 are associated with an increased risk of thrombocytopenic thrombotic purpura, and DRB1*11 is tightly linked to DRB3*01:01, identified as a potential risk factor for the development of HIT.20
Anticoagulant treatment with tinzaparin (100 IU/kg twice daily) was continued from day 17 to 19 after vaccination, despite suspicion of aHIT, as the clinical condition improved. Laboratory analyses in parallel showed normalization of platelet counts and improvement of the coagulopathy, and ultrasonography demonstrated no progression of the portal vein thrombosis (Figure 1). Tinzaparin was prioritized over alternatives (argatroban, fondaparinux, or direct oral factor Xa inhibitors) because of the estimated high risk of hemorrhage. Hence, use of an anticoagulant with a short half-life in combination with ease of administration outside of an intensive care unit was preferable. At the time of CVST diagnosis on day 19 after vaccination, monitoring of anti-factor Xa activity demonstrated levels in the lower therapeutic range, tinzaparin was deemed insufficient, and anticoagulant treatment was promptly switched to fondaparinux with a higher anti-Xa potency and casuistic use in HIT.4,21 The presence of anti-PF4 antibodies was confirmed on day 22 after vaccination by an immunoassay.
Intravenous immunoglobulin has been proposed to be a potentially beneficial treatment of aHIT.15 Given the small increased risk of thromboembolism associated with intravenous immunoglobulin,22 the predominantly prothrombotic state of the patient, and a recovering platelet count, this treatment was withheld.
Our data demonstrate activation of the classic pathway of the complement system. Complement cascade activation has been described as pathogenic in HIT,13 and modulation thereof by inhibition of C1 or C5 could represent a putative target for therapeutic intervention in refractory aHIT.23
Although causality has not been established, our case emphasizes the importance of undertaking further studies to characterize this potentially new clinical entity recently described with the suggested name of vaccine-induced immune thrombotic thrombocytopenia.24,25 It is important that clinicians be alert to this syndrome characterized by thrombosis at unusual sites, thrombocytopenia, and coagulopathy with risk of bleeding needing prompt attention.
Authorship
Contribution: A.L.T.S., M.R., J.H., Z.B.H., C.R., T.Ø.J., D.E.F., E.B.L., M.G-B., and J.S. analyzed and interpreted the data and wrote the manuscript; and L.K. J.H., A.R.-B., R.S.S., K.H., N.K., J.P.G., A.-M.H., and P.K. analyzed and interpreted the data.
Conflict-of-interest disclosure: A.L.T.S. is a former employee of Novo Nordisk Biopharm and has received honoraria for lecture from Takeda and advisory board honoraria from SOBI (both not related to the present case). Z.B.H. received an unrestricted research grant from the Independent Research Fund Denmark (not related to the present case), and received travel expenses for attending a medical conference from Pfizer. C.R. has received travel expenses for attending medical conferences from Pfizer and MSD. L.K. has received an honorarium for a lecture on pneumococcal disease from MSD. J.H. receives consulting fees for Novo Nordisk on drug delivery. E.B.L. has received honoraria from Amgen for a lecture on immune thrombocytopenia (not related to present case). A.-M.H. has received an unrestricted research grant from CSL Behring (not related to the present case) and has received honoraria for lectures from CSL Behring, Bayer, Astellas, and Boehringer-Ingelheim. P.K. has received honoraria for lectures from uniQure and Takeda and travel expenses for attendance at medical conferences from uniQure. The remaining authors declare no competing financial interests.
Correspondence: Casper Roed, Department of Pulmonary Medicine and Infectious Diseases, University Hospital of Copenhagen, North Zealand, Dyrehavevej 29, 3400 Hillerod, Denmark; e-mail: casper.roed@regionh.dk.
References
- 1.Voysey M, Clemens SAC, Madhi SA, et al. ; Oxford COVID Vaccine Trial Group. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet. 2021;397(10269):99-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.European Medicines Agency. COVID-19 Vaccine AstraZeneca: benefits still outweigh the risks despite possible link to rare blood clots with low blood platelets. Available at: https://www.ema.europa.eu/en/news/covid-19-vaccine-astrazeneca-benefits-still-outweigh-risks-despite-possible-link-rare-blood-clots
- 3.Lo GK, Juhl D, Warkentin TE, Sigouin CS, Eichler P, Greinacher A.. Evaluation of pretest clinical score (4 T’s) for the diagnosis of heparin-induced thrombocytopenia in two clinical settings. J Thromb Haemost. 2006;4(4):759-765. [DOI] [PubMed] [Google Scholar]
- 4.Greinacher A, Selleng K, Warkentin TE.. Autoimmune heparin-induced thrombocytopenia. J Thromb Haemost. 2017;15(11):2099-2114. [DOI] [PubMed] [Google Scholar]
- 5.Juhl D, Eichler P, Lubenow N, Strobel U, Wessel A, Greinacher A.. Incidence and clinical significance of anti-PF4/heparin antibodies of the IgG, IgM, and IgA class in 755 consecutive patient samples referred for diagnostic testing for heparin-induced thrombocytopenia. Eur J Haematol. 2006;76(5):420-426. [DOI] [PubMed] [Google Scholar]
- 6.Sode BF, Allin KH, Dahl M, Gyntelberg F, Nordestgaard BG.. Risk of venous thromboembolism and myocardial infarction associated with factor V Leiden and prothrombin mutations and blood type. CMAJ. 2013;185(5):E229-E237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aznar J, Vayá A, Estrellés A, et al. Risk of venous thrombosis in carriers of the prothrombin G2010A variant and factor V Leiden and their interaction with oral contraceptives. Haematologica. 2000;85(12):1271-1276. [PubMed] [Google Scholar]
- 8.Lidegaard Ø, Løkkegaard E, Svendsen AL, Agger C.. Hormonal contraception and risk of venous thromboembolism: national follow-up study. BMJ. 2009;339:b2890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greinacher A. CLINICAL PRACTICE. Heparin-Induced Thrombocytopenia. N Engl J Med. 2015;373(3):252-261. [DOI] [PubMed] [Google Scholar]
- 10.Marchetti M, Zermatten MG, Bertaggia Calderara D, Aliotta A, Alberio L.. Heparin-Induced Thrombocytopenia: A Review of New Concepts in Pathogenesis, Diagnosis, and Management. J Clin Med. 2021;10(4):683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kelton JG, Sheridan D, Santos A, et al. Heparin-induced thrombocytopenia: laboratory studies. Blood. 1988;72(3):925-930. [PubMed] [Google Scholar]
- 12.Chong BH, Ismail F.. The mechanism of heparin-induced platelet aggregation. Eur J Haematol. 1989;43(3):245-251. [DOI] [PubMed] [Google Scholar]
- 13.Khandelwal S, Ravi J, Rauova L, et al. Polyreactive IgM initiates complement activation by PF4/heparin complexes through the classical pathway. Blood. 2018;132(23):2431-2440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Warkentin TE, Makris M, Jay RM, Kelton JG.. A spontaneous prothrombotic disorder resembling heparin-induced thrombocytopenia. Am J Med. 2008;121(7):632-636. [DOI] [PubMed] [Google Scholar]
- 15.Warkentin TE. High-dose intravenous immunoglobulin for the treatment and prevention of heparin-induced thrombocytopenia: a review. Expert Rev Hematol. 2019;12(8):685-698. [DOI] [PubMed] [Google Scholar]
- 16.Poudel DR, Ghimire S, Dhital R, Forman DA, Warkentin TE.. Spontaneous HIT syndrome post-knee replacement surgery with delayed recovery of thrombocytopenia: a case report and literature review. Platelets. 2017;28(6):614-620. [DOI] [PubMed] [Google Scholar]
- 17.Pruthi RK, Daniels PR, Nambudiri GS, Warkentin TE.. Heparin-induced thrombocytopenia (HIT) during postoperative warfarin thromboprophylaxis: a second example of postorthopedic surgery ‘spontaneous’ HIT. J Thromb Haemost. 2009;7(3):499-501. [DOI] [PubMed] [Google Scholar]
- 18.Okata T, Miyata S, Miyashita F, Maeda T, Toyoda K.. Spontaneous heparin-induced thrombocytopenia syndrome without any proximate heparin exposure, infection, or inflammatory condition: Atypical clinical features with heparin-dependent platelet activating antibodies. Platelets. 2015;26(6):602-607. [DOI] [PubMed] [Google Scholar]
- 19.Warkentin TE, Basciano PA, Knopman J, Bernstein RA.. Spontaneous heparin-induced thrombocytopenia syndrome: 2 new cases and a proposal for defining this disorder. Blood. 2014;123(23):3651-3654. [DOI] [PubMed] [Google Scholar]
- 20.Karnes JH, Shaffer CM, Cronin R, et al. Influence of Human Leukocyte Antigen (HLA) Alleles and Killer Cell Immunoglobulin-Like Receptors (KIR) Types on Heparin-Induced Thrombocytopenia (HIT). Pharmacotherapy. 2017;37(9):1164-1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cuker A, Arepally GM, Chong BH, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: heparin-induced thrombocytopenia. Blood Adv. 2018;2(22):3360-3392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Daniel GW, Menis M, Sridhar G, et al. Immune globulins and thrombotic adverse events as recorded in a large administrative database in 2008 through 2010. Transfusion. 2012;52(10):2113-2121. [DOI] [PubMed] [Google Scholar]
- 23.Bartko J, Schoergenhofer C, Schwameis M, et al. A Randomized, First-in-Human, Healthy Volunteer Trial of sutimlimab, a Humanized Antibody for the Specific Inhibition of the Classical Complement Pathway. Clin Pharmacol Ther. 2018;104(4):655-663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schultz NH, Sørvoll IH, Michelsen AE, et al. Thrombosis and Thrombocytopenia after ChAdOx1 nCoV-19 Vaccination [published online ahead of print 9 April 2021]. N Engl J Med. doi: 10.1056/NEJMoa2104882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Greinacher A, Thiele T, Warkentin TE, Weisser K, Kyrle PA, Eichinger S.. Thrombotic Thrombocytopenia after ChAdOx1 nCov-19 Vaccination [published online ahead of print 9 April 2021]. N Engl J Med. doi: 10.1056/NEJMoa2104840. [DOI] [PMC free article] [PubMed] [Google Scholar]