Abstract
Cowden syndrome is a rare autosomal dominant disorder that is characterized by multiple hamartomatous neoplasms in a variety of tissues and is associated with germline mutations in the PTEN gene. Cowden syndrome does not have increased risk of gastric malignancy; however, complications of benign neoplasm can occur. The authors report a case of a patient with Cowden Syndrome and with gastric polyps that caused severe morbidity and a surgical approach was indicated. An antrectomy with troncular vagotomy was performed with a Billroth I reconstruction. In this case, this was of paramount importance so the duodenum can be revisited.
Keywords: Cowden syndrome, gastric polyps, Billroth I
INTRODUCTION
Cowden syndrome is an autosomal dominant disorder resulting from a mutation in the PTEN tumor suppressor gene [1]. The clinical diagnosis of Cowden syndrome is based on criteria from the National Comprehensive Cancer Network and the International Cowden Syndrome Consortium operational diagnostic criteria [2]. The life time risk of some cancers including thyroid, endometrial and breast is superior to the general population; therefore, clear evidence-based surveillance strategies for these individuals are required [3].
The hallmark of this disease is the appearance of multiple hamartomas that affects all three of the germ layers [4], but the most common clinical manifestations are mucocutaneous lesions (98%), gastrointestinal (GI) polyps (93%) and macrocephaly (93%) [5].
In PTEN mutation carriers, upper gastrointestinal polyps do occur with some frequency, as demonstrated by Heald and colleagues [6], and some of the patients have symptoms including haemorrhage, obstruction and pain. Microscopically, the most common findings are hyperplastic polyps, hamartomas and ganglioneuromas of the stomach [7], but there are not any specific histologic features that distinguish them from sporadic lesions [8]. Another characteristic finding in these patients is glycogenic acanthosis of the oesophagus, reported in up to 80% of patients going through endoscopic surveillance. It has been suggested that extensive glycogenic acanthosis of the oesophagus associated with benign gastrointestinal polyps is pathognomonic for Cowden disease [9].
The authors present a case in which not only the gastric polyps cause symptoms with severe morbidity, but also needed surgical treatment.
CASE REPORT
A 66-year-old female diagnosed with Cowden syndrome in 2007 with a history of treated breast, endometrial and ovarian cancer. She had valvular heart disease with mitral insufficiency and atrial fibrillation, and because of this, she was on edoxaban, an anticoagulant medication and (factor Xa inhibitor). She never had overt gastrointestinal haemorrhage, but she had symptomatic anaemia because of occult blood loss from the GI tract.
In 2017, an endoscopic removal of some polyps was performed, but she had gastric haemorrhage afterwards with necessity of blood transfusion. In 2018, an esophagogastroduodenoscopy (EGD) was repeated and multiple polyps with ulceration were observed, but due to the dimension of the polyps and possible complications, none of them was removed.
In April 2020, she needed hospitalization because of decompensated heart failure caused by symptomatic anaemia presented with an haemoglobin of 7,6 g/dl (hypochromic and microcytic) and a blood transfusion was needed. Thereupon, she was observed in a gastroenterology consultation to plan subsequent treatment: glycogenic acanthosis of the oesophagus, and multiple gastric and duodenal polyps were observed on EGD with very bulky polyps/conglomerate of polyps (50 mm) in the antrum with a very congestive, eroded surface and with some ulcers as observed in Fig. 1. It was considered endoscopic treatment but due to difficult access (if not impossible), probability of incomplete excision/recurrence and very high potential for complications it was consider inadequate an endoscopic approach.
Figure 1 .
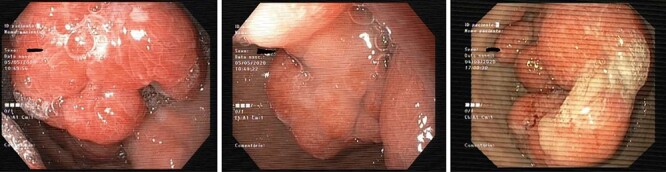
EGD image showing conglomerate of polyps in the antrum.
A computer tomography was made to complete the study and showed the presence of endoluminal expansive formations in the gastric antrum as can be seen in Fig. 2.
Figure 2 .
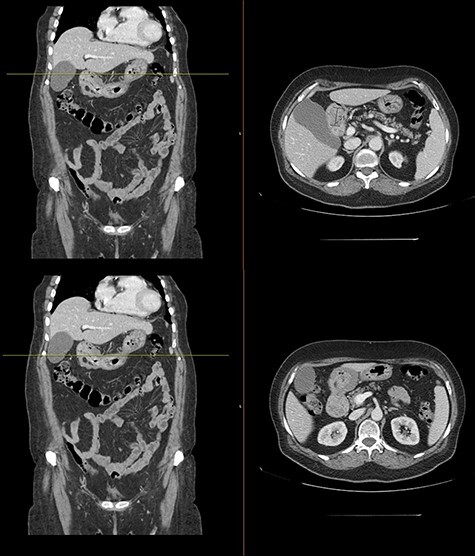
Computed tomography with intravenous contrast images demonstrating endoluminal expansive formations in the gastric antrum.
She was referred to the surgery consultation and surgical treatment was proposed: antrectomy with troncular vagotomy with a Billroth I reconstruction. It was operated in October 2020 and the post-operative period was uneventful.
The histological examination showed polyps with characteristics of hyperplastic polyps, located in the antrum and pre-pyloric region, the largest with 5.5 × 3 × 2.8 cm, without evidence of dysplasia or malignancy.
The patient is now asymptomatic and with an hemoglobin between 13,2 and 14,4 g/dl since the surgery.
DISCUSSION
The most serious consequences of Cowden syndrome relate to the increased risk of cancers but benign manifestations can also cause significant morbidity; management of these manifestations varies depending on the age and performance status of the individual [3].
In this case, the authors describe a case where a benign manifestation of this condition caused morbidity to the patient: anaemia, decompensate heart failure, hospitalization and blood transfusion.
The initial approach should always be endoscopic therapy as it is a less invasive and organ-sparing technique; however, in this case, several variables prevented this course of treatment from being followed. The fact of previously had an endoscopic removal attempt that, not only caused hemorrhage with a need of blood transfusion, but was also was incomplete, leads us to think that repeating this approach could be dangerous and lead to failure.
Therefore, surgical treatment is suggested as the solution for this patient. The key to the success of the treatment lies in the ability to solve the problem but taking into account the future need for surveillance.
The type of surgery performed in this context is essential and surgical planning is fundamental. Considering that it is a benign pathology and the risk of malignancy is low, the surgery should be as organ sparing as possible: in this case, considering that the polyps that caused the symptoms were in the antrum, the proposed surgery was an antrectomy.
Nowadays, the most used type of reconstruction after gastric resection surgery is Roux-en-Y reconstruction. This brings advantages such as the diversion of biliopancreatic secretions from the remaining stomach, avoiding bilio-gastric reflux and its complications such as reflux esophagitis, intestinal metaplasia and Barrett’s esophagus.
But, in this case, this type of reconstruction would make access to the duodenum impossible, where the patient had polyps and will need endoscopic surveillance and eventually therapy. In view of this limitation, the best reconstruction would be Billroth I: in this type of reconstruction, a gastroduodenostomy is performed, allowing future access by endoscopic route to the duodenum. In this case, the Billroth II reconstruction would also make it more challenging the access to the duodenum.
In conclusion, the authors intend to demonstrate that a patient with Cowden Syndrome, whose greatest concern will always be malignant manifestations, may have benign manifestations that are equally debilitating and whose treatment should be appropriate to the patient in question and the desired result.
CONFLICT OF INTEREST STATEMENT
None declared.
Contributor Information
Teresa Freitas Correia, General Surgery, Department of Surgery, Centro Hospitalar e Universitário do Porto (CHUP), Oporto, Portugal.
Isabel Mesquita, General Surgery, Department of Surgery, Centro Hospitalar e Universitário do Porto (CHUP), Oporto, Portugal.
Mário Marcos, General Surgery, Department of Surgery, Centro Hospitalar e Universitário do Porto (CHUP), Oporto, Portugal.
Carlos Nogueira, General Surgery, Department of Surgery, Centro Hospitalar e Universitário do Porto (CHUP), Oporto, Portugal.
Jorge Santos, General Surgery, Department of Surgery, Centro Hospitalar e Universitário do Porto (CHUP), Oporto, Portugal.
References
- 1. Ngeow J, Sesock K, Eng C. Clinical implications for germline PTEN spectrum disorders. Endocrinol Metab Clin North Am 2017;46:503–17. [DOI] [PubMed] [Google Scholar]
- 2. Pilarski R, Burt R, Kohlman W, Pho L, Shannon KM, Swisher E. Cowden syndrome and the PTEN hamartoma tumor syndrome: systematic review and revised diagnostic criteria. J Natl Cancer Inst 2013;105:1607–16. [DOI] [PubMed] [Google Scholar]
- 3. Tan M-H, Mester JL, Ngeow J, Rybicki LA, Orloff MS, Eng C. Lifetime Cancer Risks in Individuals with Germline PTEN Mutations. Clin Cancer Res 2012 January 15;18:400–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lelli JL. Pediatric Surgery, Chapter 93. 1177–85
- 5. Bubien V, Bonnet F, Brouste V, Hoppe S, Barouk-Simonet E, David A, et al. French Cowden disease network: high cumulative risks of cancer in patients with PTEN hamartoma tumour syndrome. J Med Genet 2013;50:255–63. [DOI] [PubMed] [Google Scholar]
- 6. Heald B, Mester J, Rybicki L, Orloff MS, Burke CA, Eng C. Frequent gastrointestinal polyps and colorectal adenocarcinomas in a prospective series of PTEN mutation carriers. Gastroenterology 2010;139:1927–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Goulas SS, Papaioannou DG, Papadeli DT, Psilopoulos DJ, Elefsiniotis IG, Mavrogiannis CK, et al. Cowden’s disease: a case report and review of the literature. Ann Gastroenterol 2003;16:70–3. [Google Scholar]
- 8. Rosty C. The role of the surgical pathologist in the diagnosis of gastrointestinal polyposis syndromes. Adv Anat Pathol 2018;25:1–13. [DOI] [PubMed] [Google Scholar]
- 9. Kay PS, Soetikno RM, Mindelzun R, Young HS. Diffuse esophageal glycogenic acanthosis: an endoscopic marker of Cowden’s disease. Am J Gastroenterol 1997;92:1038–40. [PubMed] [Google Scholar]


