INTRODUCTION
For older adults with serious, life-limiting illness, the decision to initiate intubation is complex and emotional. With seriously ill older adults in acute respiratory failure, emergency physicians are having some of the hardest conversations in medicine. During the last 6 months of life, 75% of older adults visit the emergency department (ED).1 ED visits are often important points in these patients’ illness trajectories, signaling a more rapid rate of decline.2–4 The incidence of intubation for older adults doubled between 2001 and 2020.5 Yet a systematic review revealed that the majority of patients do not possess advance directives in the ED,6 meaning that urgent conversations are needed in a time of crisis to ensure that patients receive care that aligns with their goals.7 Making these decisions in the ED is challenging. Emergency physicians recognize this pivotal moment to provide goal-concordant care8; however, the time-pressured environment, lack of longitudinal relationship with patients, and clinical instability further increase the complexity of these conversations.9 A practical method is needed to perform this procedural skill. In this article, we discuss the prognosis of older adults undergoing ED intubation in the context of framing the code status conversations and provide a practical framework to execute these difficult conversations.
FAMILIARITY WITH THE PATIENT’S PROGNOSIS IS ESSENTIAL BEFORE INITIATION OF A CODE STATUS CONVERSATION
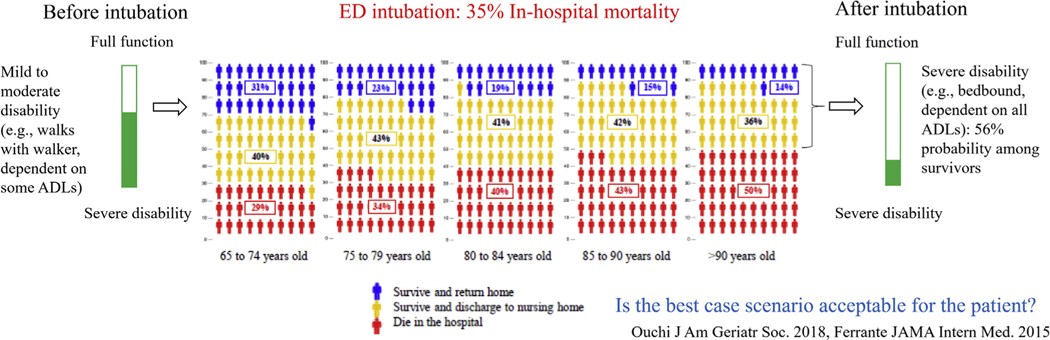
Effective code status conversations require emergency physicians to understand the prognosis of seriously ill older adults with acute respiratory failure and rapidly explore what matters most. More than 70% of older adults prefer quality of life rather than life extension.10 Furthermore, greater than or equal to 60% of older adults consider inability to “get out of bed” or “rely on a breathing machine to live” as equal to or “worse than death.”11 The majority (87%) of seriously ill older adults who are hospitalized express that they would even trade 1 year of a 5-year lifespan to avoid dying in the ICU.12 Unfortunately, the outcomes after ED intubation among seriously ill older adults are not as good as many patients think they will be, which may be predicted from prognosis calculators.13,14 One in 3 older adults dies in the hospital after intubation. The survival characteristics are influenced by age (eg, 50% mortality for individuals >90 years) and comorbid conditions (eg, 40% increased odds of death for those with Charlson comorbidity index score ≥4). Among survivors, greater than 80% will be discharged to places other than home.15 Furthermore, the resulting disability they will likely endure may be considered worse than death. For older adults with mild to moderate physical disability who are admitted to the ICU, a quarter will die, and among the survivors, 54% will develop severe disability even worse than that at their baseline.6 Considering prognosis and likely functional outcomes, emergency physicians must determine what patients would consider an acceptable quality of life (Figure 1).
Figure 1.
Older adults with serious illness: prognosis and function after ED intubation.
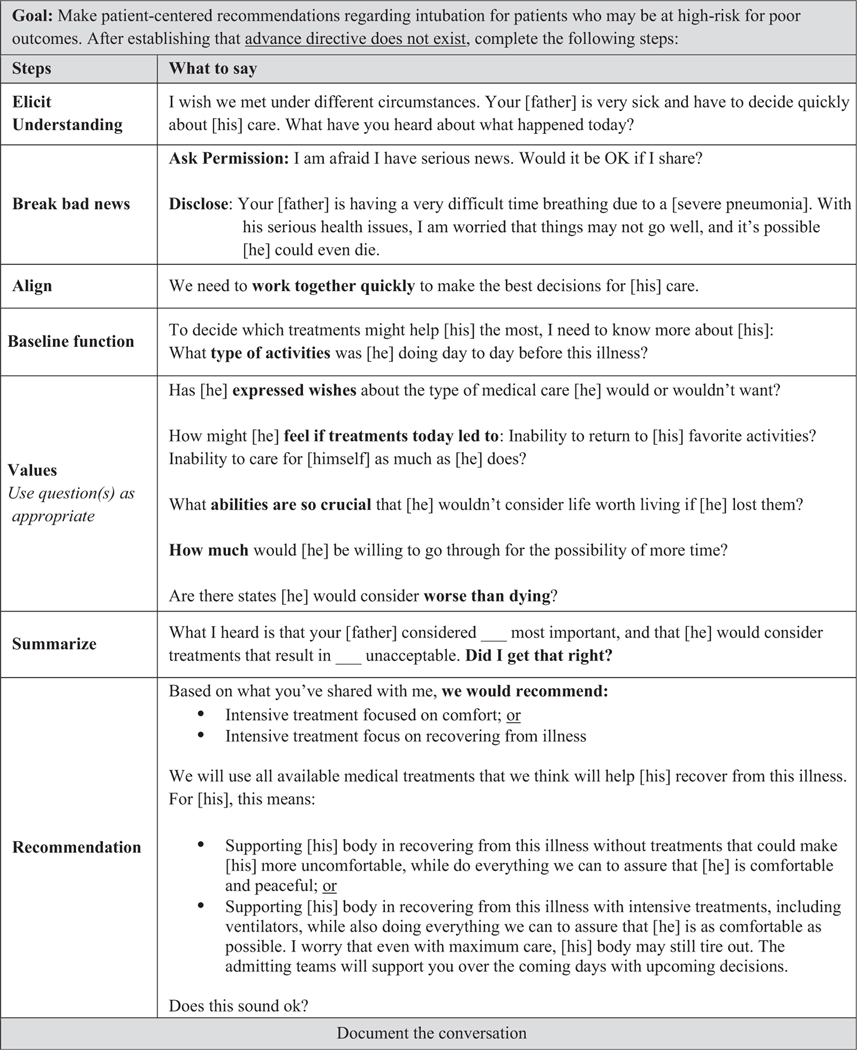
A STEPWISE APPROACH TO THE ED CODE STATUS CONVERSATIONS
As with any procedure, the code status conversations are mastered through deliberate practice of communication skills. We recommend reading the following steps out loud (Figure 2). Furthermore, we encourage emergency physicians to flexibly adjust the order of the following steps because these conversations may not occur linearly.
Figure 2.
ED code status conversation guide. See Appendix E1, available online at http://www.annemergmed.com, for how this guide was developed.33–36
STEP 1: ESTABLISH URGENCY AND ELICIT UNDERSTANDING
“I wish we had met under different circumstances. Your [father] is very sick and I have to decide quickly about [his] care. What have you heard about what happened today?” Explicitly describe the situation clearly and build rapport. Asking what the surrogates have heard allows them to express their understanding and not be redundant (Video E1, available online at http://www.annemergmed.com).
STEP 2: BREAK BAD NEWS
For seriously ill older adults, the development of respiratory failure requiring intubation is “bad news” (Video E2, available online at http://www.annemergmed.com).15,16 To allow the patient or surrogate to grasp the severity of the situation, 2 steps are needed:
-
Asking for permission: “I am afraid I have serious news. Would it be OK if I talk about it?”
Asking for permission enables the patient or surrogate a moment to emotionally prepare. Most important, it gives a sense of control in a situation that may feel out of control.
-
Disclose the headline: “Your [father] is having a very difficult time breathing because of [severe pneumonia]. With his serious health issues, I am worried that things may not go well, and it is possible [he] could even die.”
The news is delivered with little jargon. Using phrases such as “I am worried.” allows physicians to be candid about the prognosis without being emotionally distant. Emergency physicians must recognize that emotions may manifest in the form of a medical question (eg, “What medications and treatments are you giving him?”). Rather than answering only cognitively (eg, “The drug that we use for pneumonia is.”), respond directly to the patient’s or surrogate’s emotions (eg, “I can imagine that this is upsetting to hear”).17
STEP 3: DEVELOP THERAPEUTIC ALIGNMENT
“We need to work together quickly to make the best decisions for [his] care.”
Therapeutic alignment is key to building trust, which is necessary to make a patient-centered recommendation. Alignment is cultivated by using “we” statements, by eliciting input from the patient or surrogate, and by responding to the patient’s or surrogate’s emotions (Video E3, available online at http://www.annemergmed.com).17
STEP 4: ASCERTAIN BASELINE FUNCTION
“What type of activities was [he] doing day to day before this illness?”
To estimate functional outcomes after critical care, physicians need to ascertain the patient’s baseline function. A patient’s baseline health status before the onset of acute respiratory failure is necessary to inform the functional prognosis in the best-case scenario (Video E4, available online at http://www.annemergmed.com).
STEP 5: EXPLORE THE PATIENT’S VALUES AND GOALS, AND THEN SUMMARIZE
“Has [he] expressed wishes about the type of medical care [he] would or would not want?”
“How might [he] feel if treatments today led to inability to return to [his] favorite activities or inability to care for [himself] as much as [he] does?”
“What abilities are so crucial that [he] would not consider life worth living if [he] lost them?”
“How much would [he] be willing to go through for the possibility of more time?”25
“Are there states [he] would consider worse than dying?”
Patients may value particular scenarios differently (eg, avoidance of certain health states). The goal of exploring patient values is to understand the previously expressed wishes and reasoning behind that decisionmaking. Determine what the patient may consider acceptable quality of life. When a patient’s values are not clear, questions about trade-offs, such as how much more he or she would be willing to go through for the possibility of more time25 or what states would be considered worse than dying, may be required to explore the minimal quality of life a patient may consider acceptable (Video E5, available online at http://www.annemergmed.com).
STEP 6: SUMMARIZE
Once patient values are explored, physicians can reflect on what they heard about the baseline function and values and then reframe the information in a way that accurately reflects the patient’s desired health status (Video E6, available online at http://www.annemergmed.com). “What I heard is that your [father] considered spending time with [his] grandchildren the most important, that [he] has been too tired to do so for a while, and that [he] would consider treatments that result in [his] being bed bound unacceptable. Did I get that right?”
STEP 7: MAKE A RECOMMENDATION
“According to what you’ve shared with me, we would recommend
intensive treatment focused on comfort; or
-
intensive treatment focused on recovering from illness.
We will use all available medical treatments that we think will help [him] recover from this illness. This means
supporting [his] body in recovering from this illness without treatments that could make [him] more uncomfortable while doing everything we can to ensure that [he] is comfortable and peaceful; or
supporting [his] body in recovering from this illness with intensive treatments, including ventilators, while doing everything we can to ensure that [he] is as comfortable as possible. I worry that even with maximum care, [his] body may still tire out. The admitting teams will support you during the coming days with upcoming decisions. Does this sound OK?”
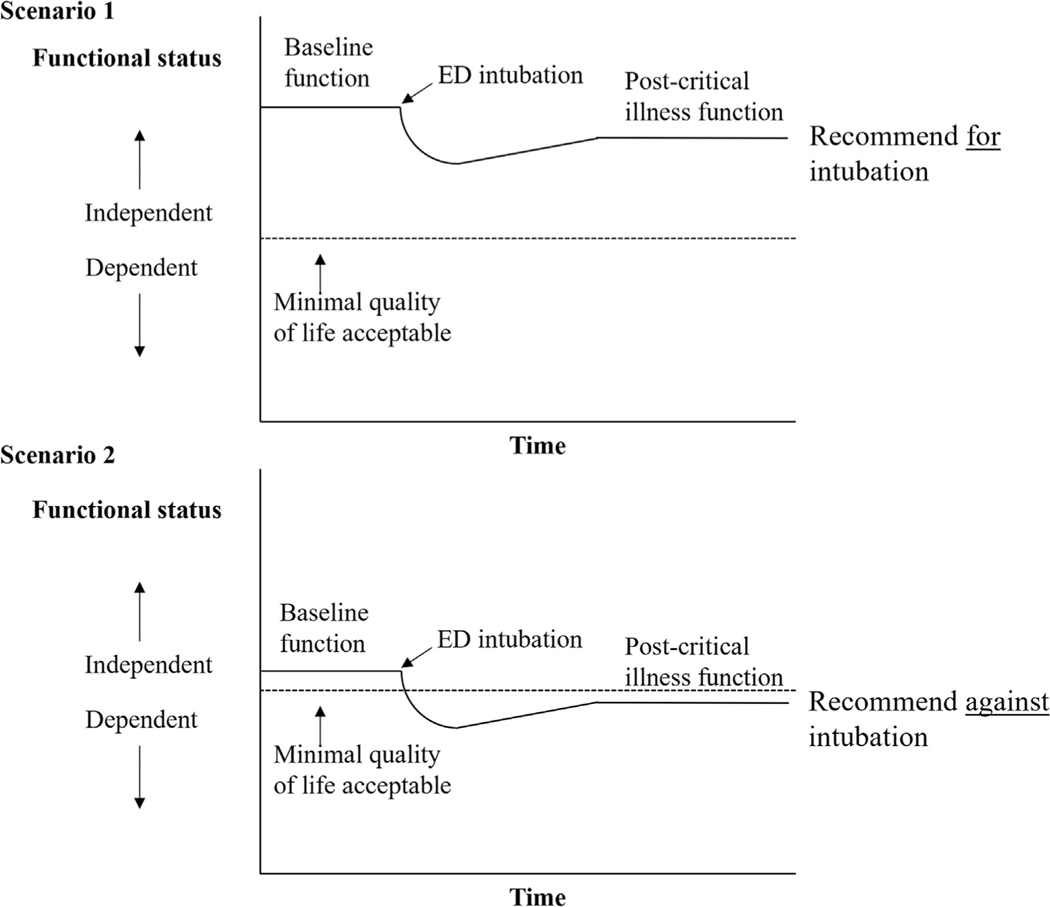
To make an empathic and goal-concordant recommendation, integrate the baseline function and values with knowledge of the patient’s prognosis (Video E7, available online at http://www.annemergmed.com). Ask yourself whether, in the best-case scenario, this patient would be able to achieve the minimal quality of life worth living for [him] after intubation or an ICU stay. If this answer is a clear no or the likely outcome would be considered worse than death for the patient, emergency physicians can confidently make a recommendation to focus the treatment on the patient’s comfort. If the answer is unclear (eg, the surrogate may not know the minimal quality of life that the patient would consider acceptable) or the likely outcome would be an acceptable quality of life worth living, emergency physicians can make a recommendation to focus the treatment on recovering from the illness (Figure 3). Emphasize what you will do (eg, focus on ensuring the patient’s comfort). Consider explaining why you would not recommend certain therapies in the context of the baseline function and values. Introduction of a time-limited trial may also be helpful.18,19
Figure 3.
Recommendation based on quality of life acceptable to patients.
PITFALLS: PROBLEMATIC APPROACHES
Nationally, only approximately half of emergency medicine residencies report teaching trainees primary palliative care skills.20 Most emergency physicians report that these skills are important, but they are not comfortable with them.21,22 In the time-pressured ED, our trainees are taught to use binary logic (eg, sick or not sick). In the absence of formal training in code status conversations, many physicians try to simplify these into similarly binary questions (eg, “Do you want us to do everything for your loved one if his or her heart stops?”). These well-intended questions can be traumatizing to patients and surrogates and also may seem impossible to answer during an acute health crisis. We categorize the patterns of well-intended yet clinically ineffective communication approaches into the following:
Describer: “If your heart stopped, would you want us to crack the ribs with chest compressions and put a breathing tube in the lungs?” It is physicians’ natural tendency to ensure that the patient or surrogate can visualize what invasive medical interventions involve. The description worsens anxiety and distracts from the patient’s goals in quality of life, which ultimately hinders his or her decisionmaking.23
Informer: “The chance of surviving and returning home is 25%.” Trained in informed consent, physicians want to ensure that patients and surrogates understand the scientific information about chance. Explaining the survival probability distracts from focusing the conversation on the patient’s desired quality of life. Furthermore, human beings misinterpret the probability in highly emotional circumstances.23,24
Decision Presser: “I want to make sure you realize that if we stop this now, your father will die; is that what you want?” Emotions peak when one is pressured to make decisions. We want the patient or surrogate to assume responsibility for our actions or inactions.
In the absence of formal training, many trainees continue to use code status scripts such as these, and subsequently pass them on to future generations of residents.
LIMITATIONS
The ED code state conversation guide does not fully convey all of the complexity of code conversations, much as advanced cardiac life support (ACLS) pocket cards25 do not provide clinicians with mastery of cardiology. Rather, both are designed to provide expert-based guidelines that help ensure standardization of care. Unlike the ACLS guidelines or the original Serious Illness Conversation Guide that our guide is based on,26,27 our guide has not been tested to demonstrate improvement in outcomes. Many models to execute code status conversations exist, and we encourage emergency physicians to seek further training to master these communication skills in established serious illness communication programs.28–30 This article does not address decisionmaking for other invasive procedures (eg, cardiopulmonary resuscitation, vasopressors), yet we hope that our approach will be adapted to those situations. Regardless of clinicians’ masterful communication skills, the decisionmaking may be equally influenced by patients’ or surrogates’ readiness to accept the difficult reality of an end-of-life situation.
CONCLUSION
Emergency physicians are expected to provide goal-concordant care during acute health decompensation for seriously ill older adults. Prognosis must be conveyed in a patient-centered manner: the survival probability is only important for emergency physicians to internally predict the best possible outcome should a patient survive. The ED code status conversation guide allows emergency physicians to succinctly make patient-centered recommendations for intubation decisions.
Supplementary Material
Acknowledgments
The authors acknowledge the Serious Illness Care Program, Ariadne Labs, for serving as the building block for their ED code status conversation guide (Susan Block, MD, Joanna Paladino, MD, Justin Sanders, MD, Msc, and the rest of the team)31,32; and the following experts in palliative medicine and serious illness communication teaching who served on the panel for the development of this guide: Erin Clarkson, MD (palliative care), Esme Finlay, MD (palliative care), Joshua Lakin, MD (palliative care), and Richard Leiter, MD, MA (palliative care).
Funding and support: By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). Dr. Ouchi and Dr. Bernacki are supported by the Sojourns Scholar Leadership Program from the Cambia Health Foundation.
Footnotes
Supervising editor: Steven M. Green, MD. Specific detailed information about possible conflict of interest for individual editors is available at https://www.annemergmed.com/editors.
REFERENCES
- 1.Smith AK, McCarthy E, Weber E, et al. Half of older Americans seen in emergency department in last month of life; most admitted to hospital, and many die there. Health Aff (Millwood). 2012;31:1277–1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilber ST, Blanda M, Gerson LW, et al. Short-term functional decline and service use in older emergency department patients with blunt injuries. Acad Emerg Med. 2010;17:679–686. [DOI] [PubMed] [Google Scholar]
- 3.Deschodt M, Devriendt E, Sabbe M, et al. Characteristics of older adults admitted to the emergency department (ED) and their risk factors for ED readmission based on comprehensive geriatric assessment: a prospective cohort study. BMC Geriatr. 2015;15:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nagurney JM, Fleischman W, Han L, et al. Emergency department visits without hospitalization are associated with functional decline in older persons. Ann Emerg Med. 2017;69:426–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lagu T, Zilberberg MD, Tjia J, et al. Use of mechanical ventilation by patients with and without dementia, 2001 through 2011. JAMA Intern Med. 2014;174:999–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oulton J, Rhodes SM, Howe C, et al. Advance directives for older adults in the emergency department: a systematic review. J Palliat Med. 2015;18:500–505. [DOI] [PubMed] [Google Scholar]
- 7.O’Connor AE, Winch S, Lukin W, et al. Emergency medicine and futile care: taking the road less travelled. Emerg Med Australas. 2011;23:640–643. [DOI] [PubMed] [Google Scholar]
- 8.Stone SC, Mohanty S, Grudzen CR, et al. Emergency medicine physicians’ perspectives of providing palliative care in an emergency department. J Palliat Med. 2011;14:1333–1338. [DOI] [PubMed] [Google Scholar]
- 9.Smith AK, Fisher J, Schonberg MA, et al. Am I doing the right thing? provider perspectives on improving palliative care in the emergency department. Ann Emerg Med. 2009;54:86–93, 93.e81. [DOI] [PubMed] [Google Scholar]
- 10.Steinhauser KE, Christakis NA, Clipp EC, et al. Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA. 2000;284:2476–2482. [DOI] [PubMed] [Google Scholar]
- 11.Rubin EB, Buehler AE, Halpern SD. States worse than death among hospitalized patients with serious illnesses. JAMA Intern Med. 2016;176:1557–1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rubin EB, Buehler A, Halpern SD. Seriously ill patients’ willingness to trade survival time to avoid high treatment intensity at the end of life. JAMA Intern Med. 2020;180:907–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.ePrognosis. Available at: https://eprognosis.ucsf.edu/. Accessed September 27, 2018.
- 14.Ouchi K, Hohmann S, Goto T, et al. Index to predict in-hospital mortality in older adults after non-traumatic emergency department intubations. West J Emerg Med. 2017;18:690–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ouchi K, Jambaulikar GD, Hohmann S, et al. Prognosis after emergency department intubation to inform shared decision-making. J Am Geriatr Soc. 2018;66:1377–1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.George N, Jambaulikar GD, Sanders J, et al. A time-to-death analysis of older adults after emergency department intubation. J Palliat Med. 2020;23:401–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alexander SC, Ladwig S, Norton SA, et al. Emotional distress and compassionate responses in palliative care decision-making consultations. J Palliat Med. 2014;17:579–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Quill TE, Holloway R. Time-limited trials near the end of life. JAMA. 2011;306:1483–1484. [DOI] [PubMed] [Google Scholar]
- 19.Scherer JS, Holley JL. The role of time-limited trials in dialysis decision making in critically ill patients. Clin J Am Soc Nephrol. 2016;11:344–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kraus CK, Greenberg MR, Ray DE, et al. Palliative care education in emergency medicine residency training: a survey of program directors, associate program directors, and assistant program directors. J Pain Symptom Manage. 2016;51:898–906. [DOI] [PubMed] [Google Scholar]
- 21.Quest TE, Asplin BR, Cairns CB, et al. Research priorities for palliative and end-of-life care in the emergency setting. Acad Emerg Med. 2011;18:e70–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lamba S, Pound A, Rella JG, et al. Emergency medicine resident education in palliative care: a needs assessment. J Palliat Med. 2012;15:516–520. [DOI] [PubMed] [Google Scholar]
- 23.Power TE, Swartzman LC, Robinson JW. Cognitive-emotional decision making (CEDM): a framework of patient medical decision making. Patient Educ Couns. 2011;83:163–169. [DOI] [PubMed] [Google Scholar]
- 24.Sunstein CR. Probability Neglect: Emotions, Worst Cases, and Law. 2001. Available at: https://chicagounbound.uchicago.edu/cgi/viewcontent.cgi?referer=&httpsredir=1&article=1384&context=law_and_economics. Accessed July 22, 2020.
- 25.Honarmand K, Mepham C, Ainsworth C, et al. Adherence to advanced cardiovascularlifesupport(ACLS)guidelinesduringin-hospitalcardiacarrest is associated with improved outcomes. Resuscitation. 2018;129:76–81. [DOI] [PubMed] [Google Scholar]
- 26.Bernacki R, Paladino J, Neville BA, et al. Effect of the Serious Illness Care Program in outpatient oncology: a cluster randomized clinical trial. JAMA Intern Med. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Paladino J, Bernacki R, Neville BA, et al. Evaluating an intervention to improve communication between oncology clinicians and patients with life-limiting cancer: a cluster randomized clinical trial of the Serious Illness Care Program. JAMA Oncol. 2019;5:801–809. [DOI] [PubMed] [Google Scholar]
- 28.Grudzen CR, Emlet LL, Kuntz J, et al. EM Talk: communication skills training for emergency medicine patients with serious illness. BMJ Support Palliat Care. 2016;6:219–224. [DOI] [PubMed] [Google Scholar]
- 29.Leiter RE, Yusufov M, Hasdianda MA, et al. Fidelity and feasibility of a brief emergency department intervention to empower adults with serious illness to initiate advance care planning conversations. J Pain Symptom Manage. 2018;56:878–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.EPEC for Emergency Medicine. Education in Palliative and End of LifeCare (EPEC) 2010. Available at: https://www.bioethics.northwestern.edu/programs/epec/curricula/emergency.html. Accessed December 9, 2019.
- 31.Bernacki R, Hutchings M, Vick J, et al. Development of the Serious Illness Care Program: a randomised controlled trial of a palliative care communication intervention. BMJ Open. 2015;5:e009032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bernacki RE, Block SD; American College of Physicians High Value Care Task Force. Communication about serious illness care goals: a review and synthesis of best practices. JAMA Intern Med. 2014;174:1994–2003. [DOI] [PubMed] [Google Scholar]
- 33.Childers JW, Back AL, Tulsky JA, et al. REMAP: a framework for goals of care conversations. J Oncol Pract. 2017;13:e844–e850. [DOI] [PubMed] [Google Scholar]
- 34.White JA, Tao X, Artuso RD, et al. Effect of physician-dispensed medication on workers’ compensation claim outcomes in the state of Illinois. J Occup Environ Med. 2014;56:459–464. [DOI] [PubMed] [Google Scholar]
- 35.Jacobsen J, Blinderman C, Alexander Cole C, et al. “I’d recommend.”: how to incorporate your recommendation into shared decision making for patients with serious illness. J Pain Symptom Manage. 2018;55:1224–1230. [DOI] [PubMed] [Google Scholar]
- 36.Curtis JR, Kross EK, Stapleton RD. The importance of addressing advance care planning and decisions about do-not-resuscitate orders during novel coronavirus 2019 (COVID-19). JAMA. 2020. 10.1001/jama.2020.4894. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.