Abstract
Background:
The outbreak of the COVID-19 virus has had many destructive impacts on socio-economic and health systems. The health systems of countries could be supportive in crisis management, but they also are affected by the impact of the crisis, consequently, their operational level has declined. This study pursued resilience in an overall national health system under pandemic stress.
Methods:
Based on WHO building blocks, by interviewing informants of the Ministry of Health and Medical Education, in Tehran-Iran, early 2021 a rich picture of the current situation depicted, the resilience model was extracted via a mixed method of Soft System Methodology (SSM) and total interpretive structural modeling (TISM). Dynamic capabilities were applied for the orchestration of the Iranian health system.
Results:
Particular functional and structural suggestions applicable for designing a ubiquitous resilience model for the country-wide health system are presented in this study. The variables of crisis sensing, opportunity seizing, and reconfiguration are the cornerstones of health system resilience.
Conclusion:
Well-suited health technology assessment (HTA) and health information system (HIS) play significant roles in the overall strengthening of the health system. All reforms for resilience will have a lasting result when the capabilities created by the resilience model are learned and reused in a dynamic cycle.
Keywords: Resilience, Health system, Dynamic capabilities, COVID-19, Soft systems methodology
Introduction
Knowing the complexity of a health system, resilience could be conceptualized and measured by aggregation of its components (1). Health systems preparedness amidst crises like pandemics is highly challenged by exposure to structural barriers. therefore, the importance of orchestration in health systems is evident (2,3). To build resilient health systems, a better perception of what it should contain is necessary (4).
Jamal et al for Syrian health system resilience on the course of war suggested absorptive, adaptive, and transformative capacities of the system as main factors for facilitating this resilience (5). Ling et al studied post epidemic outcomes of Ebola for Liberian health system resilience, their study analyzes the evolution of Liberia’s Ebola response, finding how much it shaped resilience in the health system (6). Global, national, and local players have different views on resilience. The health system elements most prioritized by global and national actors improved better, while elements valued by the community and local actors progressed less.
Several health system planning models were studied and scrutinized by researchers for displaying their monitoring and controlling ability plus extracting their functional key components.
An illustrative list of health systems frameworks is shown by Shakarishvili et al (7) as follows:
✔“Performance framework
✔Building blocks framework
✔Reforms framework
✔Systems framework
✔Primary health care framework” (7).
The World Health Organization’s framework classifies the functions of a health system within six building blocks, the exact terms used for them are listed as follows:
1) “Service delivery; 2) health workforce; 3) information; 4) medical products (medicines, vaccines, and technologies); 5) financing; and 6) leadership and governance” (8).
The building-block approach provides the inclusion of governance as one of its six blocks.
The building-block approach also focuses on hierarchical structures that orchestrate regularity, and efficiency within and between organizations (9).
The building blocks approach facilitates the recognition of the complex and intertwined essence of health system problems. Each of the blocks standalone does not constitute a functioning in the health system; instead, it is “the multiple interactivity among them, so the interactions in building blocks convert them into a system” (10).
Based on a scoping review by Fridell et al (11) which studied the papers that support the WHO building blocks framework for health system resilience, the followings were mentioned:
Five research works stated the effective financial resource allocation as significant for resilience. Five articles (All in reference 11) discussed the multi-skilled workforce role for adjustment to long-term changes and shocks. The continuous data gathering for a response to shocks was mentioned by eight articles as an essential leadership and governance mentioned by twenty sources. They emphasized accountability and transparency together with equity as the main attributes for an effective health system orchestration. The functionality of medical products, vaccines, and technologies was mentioned in four documents. Nine articles supported the service delivery role, mentioning the necessity of provision of auxiliary services besides routines to the people during a crisis (All in Reference 11).
Resilience in different scientific majors such as crisis management (12), medicine (13), supply chains (14–16), etc. has been studied. However, still, there is no consensus on a definition. Bankes defines resilience as “the ability to withstand or survive external shocks” (17). Francis & Bekera explains resilience as the ability of shock absorption and withstanding in the incident of a sudden decrease in performance, in the other word the resumption of normal performance (18).
Dynamic capabilities are capabilities that help organizations build, expand, or competently transform their operational capabilities to adapt or even create market changes. In this paper, the necessary capabilities for system resilience based on the theory of dynamic capabilities presented by Teece are analyzed (19).
Objectives
The Iranian health system is tackled by various additional problems, besides the COVID-19 pandemic, caused by severe political and economic sanctions. Therefore, the management of this system should be considered at a level higher than just the structural issues. The following questions are posed from a systemic point of view:
A: What are the components of the Iranian health system?
B: What are the characteristics of a resilient health system in the event of a corona outbreak?
C: What are the interconnectivity and interactions of the factors affecting the resilience of the health system?
This study pursued resilience in an overall national health system under pandemic stress.
Methods
This research work is a qualitative study focused on the concept of health system resilience. We conducted semi-structured in-depth interviews and focus group discussions in Tehran-Iran, early 2021. The soft system methodology was applied for designing the resilience model of the overall health system. This methodology engages the analyst in a process in which he/she can understand the real world while simultaneously improving the state of the system by analyzing the situation and providing solutions (20).
The interviewees were as follows: Group 1: Informants of the Ministry of Health and Medical Education of Iran (5 people); Second group: major health service providers (8 people).
To obtain data and also to obtain information for drawing a rich picture, questionnaires, and interviews with informants and members of the health system management have been used. The questionnaires used open-ended questions and were completed by various stakeholders. Interviews were also conducted with individuals who somehow played an influential role in the structure of the Iranian health system and had complete information. The next is given the step by step methodological approaches:
SSM technique
Via soft system methodology the problem is analyzed, then in the next step, by considering the results obtained from the problem analysis, all the factors of the problem and the views that exist regarding the situation of the problem are identified and examined.
For enhancing the resilience of the Iranian national health system during COVID-19 and post-disaster recovery guidelines, considering the current levied global economic sanctions and their consequences on the overall health system performance. To identify the variables in line with the theoretical foundations, then to increase the validity of the factors affecting the Iranian health system resilience, we discussed with experts and extracted proxies of functionality regarding the WHO framework, divided into three stages of the crisis. (Table 1).
Table 1:
Factors Affecting Health System Resilience (Researchers Findings)
| No. | WHO building blocks | Before the crisis | During the crisis | After the crisis |
|---|---|---|---|---|
| 1 | Leadership & governance | Crisis sensing System capacity Transparency Institutional design |
Ethics Opportunity seizing Operationalization Engagement |
Reconfiguration Lessons learning Public trust |
| 2 | Health Information system | Policymaking Accuracy & Integrity |
Surveillance | Knowledge management Evaluation |
| 3 | Health Workforce | Limited resources Incentive |
Diversity & Flexibility Re-motivation Community involvement |
Cross training Mental health support |
| 4 | Financing system | Funding mechanisms | Resource allocation Costing Global support |
Risk adjustment |
| 5 | Medical products | Capacity building | Sustainability | Flexible Production |
| 6 | Service delivery | CRM Prevention |
Response Alternative approaches |
Decentralization |
Rich Picture
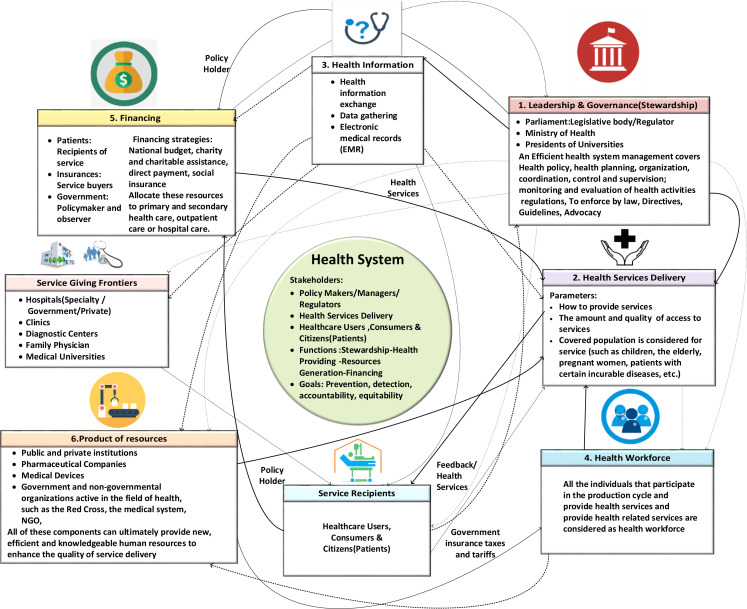
After the interviews, the main stakeholders of policymakers and managers were considered as service providers and service recipients. This diagram is drawn by authors based on the conceptual mapping model extracted from the interviews, depicting the roles and interconnections of the actors (Fig. 1).
Fig. 1:
Rich picture of Iran’s health system (Original)
In the rich picture above, the performance of the current health system of Iran as a developing country is drawn based on WHO building blocks. It is localized in six functional blocks.
CATWOE Analysis & definition
In this step, the soft systems methodology leaves the real world and enters the world of systems, and expresses the root definition based on various perspectives. The root definition expresses the problem and arises from a particular worldview. The accuracy of root definitions is checked using the CATWOE analysis presented in (Table 2).
Table 2:
CATWOE Elements and Their Definition
| CATWOE | Service recipients’ view | Service providers’ view | Policymakers and managers’ view |
|---|---|---|---|
| Customers | Patients and families | Insurance, patients and families, resource producers | Service Providers (Physician-Midwife-Nurse-Pharmacist) - Insurance - Hospitals - Universities of Medical Sciences - Health Centers - Staffs - Clinics - Family Physicians - Diagnosis and Treatment Centers - Private Hospitals |
| Actors | Implementation of the Patient Rights Charter by service providers | Policymakers and managers, physicians, pharmacists, nurses, midwives, and other health professionals | All stakeholders and the relationship between them: Ministry of Health - service providers, staff, insurance, and ... |
| Transformation Process | 1. Leadership & governance 2. HR, 3. Drugs and technology, 4. Financing, 5. Information systems, 6. Service delivery systems |
1.Leadership & governance 2. HR, 3. Drugs and technology, 4. Financing, 5. Information systems, 6. Service delivery systems |
1. Leadership & governance 2. HR, 3. Drugs and technology, 4. Financing, 5. Information systems, 6. Service delivery systems |
| World View | Providing, promoting, and maintaining the health of the people using the benchmarking method | Providing optimal and fast personal and public health services and establishing justice in the payroll system in accordance with the global standard | Ensuring the promotion and maintenance of public health to promote, and maintain the health and accountability of accountability by considering successful global models |
| Owner | Patient Rights Support Organizations, NGOs | Employment and Administrative Organizations, Universities of Medical Sciences | Ministry of Interior, Ministry of Health, Parliament, Municipalities |
| Environmental Constrains | Medical expenses, lack of medicine and medical facilities and equipment | Life threats, mental health threats, salary rates | Lack of budget, prioritization, lack of resources and equipment |
The root definition
A root definition is a term used to describe the ideal state of a system. This definition is a solid foundation for another output called the purposeful activity model or conceptual model.
Based on root definition, the resilient Iranian health system implements national health care rules and regulation, applies a national level functionality and stability guidelines, in order to 1) provide the community with the best available and equitable care 2) withstand shocks, endure crisis and support people against hardships and uncertainty of all kind when national health integrity is at risk. This resilient health system is deemed to be governed in good cooperation between public and private sector stakeholders, administrators, healthcare professionals, and policymakers. Operating in well-shaped orchestration. With Continual key role players’ involvement with promising sustainable and equitable product and service delivery, established on a platform of cooperation and interconnectivity among both national and international bodies (21).
Conceptual Model
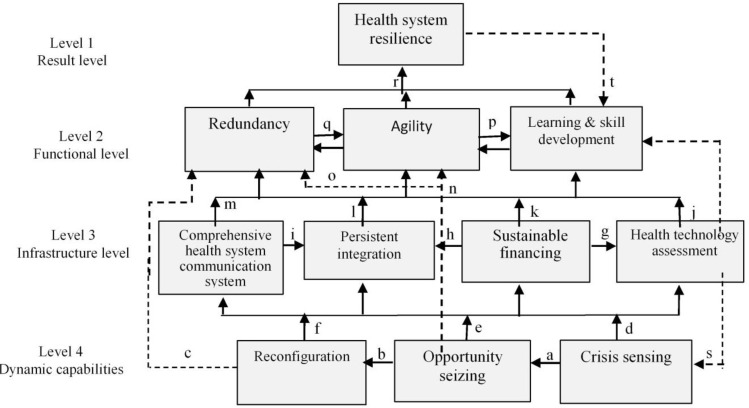
A conceptual model must be created based on root definitions. Since the soft systems method does not provide a specific method in the model drawing stage, in this research, the total interpretive structural modeling (TISM) approach has been used to draw the model. the combined method of soft systems and dynamic systems was used (22). TISM is an innovative technique for overcoming the limitations of ISM and provides causal relationships and their interpretation by experts. To implement TISM, first, the final factors affecting health system resilience were identified by studying previous research and expert opinions and conducting open-ended interviews and several rounds of screening; Factors affecting the resilience of the health system are C 1: Crisis sensing, C 2: Opportunity seizing, C 3: Reconfiguration, C 4: Health technology assessment, C 5: Sustainable financing, C 6: Persistent integration, C 7: Comprehensive health system communication, C 8: Learning & Skill development, C 9: Redundancy, C 10: Agility, C 11: Health system resilience.
Next, an SSIM (structural self-interaction matrix) is developed for the factors, which shows the paired relationships between the factors. The following symbols can be used to determine the type of relationship: (Table 3- part 1).
Table 3:
Total Interpretive Structural Modeling
| Part1- Structural Self-Interaction Matrix (SSIM) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | C1 | C2 | C3 | C4 | C5 | C6 | C7 | C8 | C9 | C10 | C11 | |
| C1 | Crisis sensing | 1 | V | O | V | V | V | V | x | O | O | O |
| C2 | Opportunity seizing | 1 | V | V | V | V | V | O | V | V | O | |
| C3 | Reconfiguration | 1 | V | A | V | V | O | V | O | O | ||
| C4 | Health technology assessment | 1 | O | O | O | V | V | V | O | |||
| C5 | Sustainable financing | 1 | V | O | V | V | V | O | ||||
| C6 | Persistent integration | 1 | A | V | V | V | O | |||||
| C7 | Comprehensive health system communication | 1 | V | V | V | O | ||||||
| C8 | Learning & Skill development | 1 | O | X | A | |||||||
| C9 | Redundancy | 1 | X | V | ||||||||
| C10 | Agility | 1 | V | |||||||||
| C11 | Health system resilience | 1 | ||||||||||
| Part 2- Final Matrix (FM) | ||||
|---|---|---|---|---|
| Variables | Reachability set | Antecedent set | Intersection set | levels |
| C11 | C11 | C11 | C11 | Level 1 |
| C10 | C8,C9,C10 | C8,C9,C10,C11 | C8,C9,C10 | Level 2 |
| C9 | C8,C9,C10 | C8,C9,C10,C11 | C8,C9,C10 | Level 2 |
| C8 | C8,C9,C10 | C8,C9,C10,C11 | C8,C9,C10 | Level 2 |
| C7 | C4,C5,C6,C7 | C4,C5,C6,C7,C9 | C4,C5,C6,C7,C8 | Level 3 |
| C6 | C4,C5,C6,C7 | C4,C5,C6,C7,C9 | C4,C5,C6,C7,C8 | Level 3 |
| C5 | C4,C5,C6,C7 | C4,C5,C6,C7,C9 | C4,C5,C6,C7,C8 | Level 3 |
| C4 | C4,C5,C6,C7 | C4,C5,C6,C7,C9 | C4,C5,C6,C7,C8 | Level 3 |
| C3 | C1,C2,C3 | C1,C2,C3,C5 | C1,C2,C3,C4 | Level 4 |
| C2 | C1,C2,C3 | C1,C2,C3,C5 | C1,C2,C3,C4 | Level 4 |
| C1 | C1,C2,C3 | C1,C2,C3,C5 | C1,C2,C3,C4 | Level 4 |
V: If criterion i only affects criterion j. X: Both criterion i affect j and criterion j affects criterion i. A: If the only criterion j affects criterion i. O: There is no effective relationship between the two criteria.
Creating an initial reachability matrix is the next step. The existence of a relation is denoted by the number 1 and the absence of relation by 0, and then the final reachability matrix is formed. In the ISM method, this step is achieved by entering the transitivity in the relationships of the variables of the final reachability matrix. This matrix is obtained using the Euler relation. M = (A +I) where A is the initial reachability matrix, I is the identity matrix and M is the final reachability matrix. In the TISM method, multiple and prominent relationships will be identified based on theoretical foundations and experts, not done in the ISM method. The variables are then graded. And this matrix is to extend the basic hypothesis in modeling. Then, by performing 8 repetition steps, the levels of variables in a combined table were performed as follows. (Table 3 – part 2).
Then the initial graph is formed which is created using the results of leveling and theoretical foundations of how the variables are related. (Fig. 2).
Fig. 2:
TISM-based resilience model
The theoretical basics of the relationships in the above model are named with regards to the TISM method from a tot, like the following: a,b,c: Dynamic Capability Theory, d,e,f: Strengths from dynamic capabilities, g,h: Network cooperation, i,m: Fourth-generation communication systems, n,o: The effect of dynamic capabilities on the main variables of resilience, i,k,l: The effect of infrastructure development on the main variables of resilience, p,q,r: The main variables of resilience, s,t: Lesson learnings from the crisis.
As shown in Fig. 2, the variables were classified into 4 categories, ranked from top to bottom, respectively. Lower level variables have the most impact and high-level variables have the most affectedness and intermediate variables have a certain amount of impact based on the type of variable. The variables of crisis sensing, opportunity seizing, and reconfiguration are the cornerstones of health system resilience. The dotted lines represent the indirect relationship of the variables and the text on the communication lines shows the scientific basis of the relationship between the variables.
Despite strengthening the theoretical foundations of the model in the TISM method and increasing its validity compared to the output of the ISM method, however, for the application of the model, it is necessary to confirm the validity of the model. The main focus was applied to the policy-making of the Iranian health system, a questionnaire designed to assess the validity of the model was completed by this group. Thus, the intensity of the relationship was considered in the range of 1 to 5, and relationships with an average score of more than 3 were accepted. The whole TISM model was approved since all links scored above 5. Therefore, this model was then used as a basis for comparison with the real world.
At this point, the methodology goes back to the real world and measures the differences between the resulting conceptual model and the real world. The analyst must provide measures to change the situation of the problem and propose measures that are systemically desirable and practical.
By comparing the rich picture of the system (what it is) and the model presented (what it should be), we can see what changes are needed to achieve a resilient health system.
Results
Accrued from its characteristics and complexity, the Iranian health system management requires to employ an ad hoc managerial science and technology as well as clinical management expertise. Medical specialists cannot manage the health centers efficiently, in this regard, to integrate clinical and managerial knowledge and skills, experts in both fields must get involved in the health system decision panel for the benefit of knowledge and experience sharing. Moreover, the inaptly integrated health information system (HIS) is among the main concerns, by which the orchestration of the entire health system and its monitoring and control is actualized.
For the case of medical equipment supply, a lot is being spent on the import of costly medical equipment, which sometimes has the least efficiency and suitability for the health system. Enriching the Health Technology Assessment (HTA) system supports the equipment supply management with better resource allocation and optimization. Meanwhile, well-trained staff for better operation of the medical equipment is necessary. Finally, the following suggestions are presented for the Iranian health system in pursuit of resilience:
Iranian health system requires comprehensive, coherent, and equitable health financing. Knowing that long-term austerity policy won’t get along with long-lasting resilience.
Technical and managerial training, interactivity among specialists for knowledge sharing
Empowering the integrated health information system for smart monitoring and overall control
Enriching the health technology assessment for better consultancy to technology transfer and procurement projects aimed at waste reduction and financial and operational optimization
Establishing an equitable pay structure for health system workers, setting up an impartial performance-based remuneration
Boosting cooperation among academic and executive bodies to respond to shocks and/or changes in the environment.
Increasing the transparency of health policies and programs to attract inter-sectoral cooperation
Strengthening customer relationship management (CRM) in favor of health service recipients
Increasing public participation in health programs and social trust recovery
Stabilizing stakeholder’s correlations especially in between finance and insurance system
Discussion
The purpose of this study was to design a resilience model for the Iranian health system. TISM method was used to analyze the relationships between variables and present their structural model. These variables were classified into 4 levels: dynamic capabilities, infrastructure, Functional, and result levels
We found that continuous learning is a very important factor because it has an impact on the first level variable, i.e. resilience, and the fourth level, i.e. dynamic capabilities. All the necessary measures for resilience will have a lasting result when the capabilities created by the resilience model are learned and reused in any new crisis emergence; this process takes place in a dynamic cycle. Resilience creates capabilities that can survive despite adverse conditions and be on the path of return and growth (23).
When austerity is advised by politicians, the health system becomes highly susceptible to socio-economic challenges, inequality rises, social capital declines and segregations occur inevitably (24). Health systems in long-term universal denial and exclusions are the most vulnerable systems of a country, knowing that its consequences are not limited inside the borders (25). No matter how good a national health agenda is provided in pursuit of resilience when it lacks global contribution and cooperation its short-term achievements are always prone to get reversing encountered by a real-life crisis (26).
Conclusion
Interactivity, transparency and continuous flow of information inbound and outbound of a national health system in times of vast crises such as global pandemics are shown as a necessity for normal state resumption. While the overall health system management of a country is under scrutiny by its various stakeholders with different impositions, the response in a way that could satisfy each party simultaneously is disturbingly paradoxical. a globally enriched and supported resilience model shows more promising outcomes comparing to standing alone regional and sector-specific resilience model.
Ethical considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
We acknowledge the assistance of Dr.Ali Shahabi, Department of Management of Technology, Science and Research Branch IAU for valuable methodological hints, Ms. Najmeh Nourbakhsh, Information Specialist of Iran University of Medical Sciences and Dr. Samaneh Heidari, Department of Trauma and injury research, Iran University of Medical Sciences for their cooperation in collecting data and arranging interviews.
Footnotes
Conflict of interest
The authors declare that there is no conflict of interest.
References
- 1.Holling C.S, Gunderson LH. (2002). Panarchy: understanding transformations in human and natural systems. 1st ed. Island Press, Washington. [Google Scholar]
- 2.Mikkelsen-Lopez I, Wyss K, De Savigny D. (2011). An approach to addressing governance from a health system framework perspective. BMC Int Health Hum Rights, 11:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.De Savigny D, Adam T. (2009). System Thinking for Health Systems Strengthening. alliance for health policy and syetem research, WHO. https://www.who.int/alliance-hpsr/resources/9789241563895/en/ [Google Scholar]
- 4.Blanchet K, Nam SL, Ramalingam B, Pozo-Martin F. (2017). Governance and capacity to manage resilience of health systems: Towards a new conceptual framework. Int J Health Policy Manag, 6(8):431–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jamal Z, Alameddine M, Diaconu K, et al. (2020). Health system resilience in the face of crisis: Analysing the challenges, strategies and capacities for UNRWA in Syria. Health Policy and Planning, 35(1):26–35. [DOI] [PubMed] [Google Scholar]
- 6.Ling EJ, Larson E, MacAuley RJ, et al. (2017). Beyond the crisis: Did the Ebola epidemic improve resilience of Liberia’s health system? Health Policy Plan, 32:iii40–iii47. [DOI] [PubMed] [Google Scholar]
- 7.Shakarishvili G, Lansang MA, Mitta V, et al. (2011). Health systems strengthening: A common classification and framework for investment analysis. Health Policy Plan, 26(4):316–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization (2007). Everybody’s business - strengthening health systems to improve health outcomes: WHO’s framework for action. WHO; Geneva. [Google Scholar]
- 9.Quinn Robert E., Bright David, Faerman Sue R., Michael P., Thompson MRM. (2015). Becoming a Master Manager: A Competing Values Approach. 6th ed. wiley; 2015. 151 p. [Google Scholar]
- 10.Manyazewal T. (2017). Using the World Health Organization health system building blocks through survey of healthcare professionals to determine the performance of public healthcare facilities. Arch Public Health, 75:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fridell M, Edwin S, Schreeb J von, Saulnier DD. (2020). Health system resilience: what are we talking about? A scoping review mapping characteristics and keywords. Int J Health Policy Manag, 9(1):6–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Park J, Seager TP, Rao PSC, et al. (2013). Integrating risk and resilience approaches to catastrophe management in engineering systems. Risk Anal, 33(3):356–67. [DOI] [PubMed] [Google Scholar]
- 13.Kim Y, Chen YS, Linderman K. (2015). Supply network disruption and resilience: A network structural perspective. Journal of Operations Management, 33–34(1):43–59. [Google Scholar]
- 14.Dolgui A, Ivanov D, Sokolov B. (2018). Ripple effect in the supply chain: an analysis and recent literature. International Journal of Production Research, 56(1–2):414–430. [Google Scholar]
- 15.Zhao K, Zuo Z, Blackhurst J V. (2019). Modelling supply chain adaptation for disruptions: An empirically grounded complex adaptive systems approach. Journal of Operations Management, 65(2):190–212 [Google Scholar]
- 16.Li Y, Zobel CW. (2020). Exploring supply chain network resilience in the presence of the ripple effect. Int J Prod Econ, 228: 107693. [Google Scholar]
- 17.Bankes S. (2010). Robustness adaptivity, and resiliency analysis. AAAI Fall Symp - Tech Rep, FS-10-03: 2–7.
- 18.Francis R, Bekera B. (2014). A metric and frameworks for resilience analysis of engineered and infrastructure systems. Reliability Engineering & System Safety, 121:90–103. [Google Scholar]
- 19.Teece DJ, Pisano G, Shuen A. (1997). Dynamic capabilities and strategic management. Strategic Management Journal, 18(7):509–33 [Google Scholar]
- 20.Checkland P. (2000). Soft systems methodology: a thirty year retrospective. Systems Research and Behavioral Science, 17(S1):S11–58. [Google Scholar]
- 21.Thomas S, Sagan A, Larkin J, et al. (2020). Strengthening health systems resilience: Key concepts and strategies. Heal Syst policy Anal, 33(3):369–377. [PubMed] [Google Scholar]
- 22.Shahabi A, Azar A, Radfar R, Asadifard RA. (2019). Combining soft systems methodology with interpretive structural modeling and system dynamics for network orchestration: case study of the formal science and technology collaborative networks in Iran. Systemic Practice and Action Research, 33(4):453–478 [Google Scholar]
- 23.Dixit V, Verma P, Tiwari MK. (2020). Assessment of pre and post-disaster supply chain resilience based on network structural parameters with CVaR as a risk measure. International Journal of Production Economics, 227(15):107655. [Google Scholar]
- 24.Massuda A, Hone T, Leles FAG, et al. (2018). The Brazilian health system at crossroads: Progress, crisis and resilience. BMJ Glob Health, 3(4): e000829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ammar W, Kdouh O, Hammoud R, et al. (2016). Health system resilience: Lebanon and the Syrian refugee crisis. J Glob Health, 6(2):020704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lapão LV, Silva A, Pereira N, et al. (2015). Ebola impact on African health systems entails a quest for more international and local resilience: the case of African Portuguese speaking countries. Pan Afr Med J, 22 Suppl 1(Suppl 1): 15. [DOI] [PMC free article] [PubMed] [Google Scholar]