Abstract
Introduction
Numerous complications can occur after a surgery, but gossypiboma is undoubtedly the most unwanted and undesirable complication of a procedure for any surgeon with legal implications. Once suspected, the minimally invasive surgical approach should be considered for its management.
Presentation of case
An adult P1L1E1 female presented to the surgery OPD with a painless abdominal mass which progressively increased in size in the past 4 months. She underwent emergency surgery for a ruptured ectopic pregnancy 6 months back at some other health centre.
On computed tomography scan of the abdomen, a well-defined heterogenous cystic lesion of size 9.8 cm × 9.2 cm × 7 cm was noted intraperitoneally. Few air foci with a hyperdense tubular structure within the lesion were seen, suggestive of a retained surgical sponge with its radio-opaque marker also visualised.
The retained sponge was successfully retrieved by the laparoscopic approach.
Discussion
Traditionally, the open approach for the removal of the sponge was more accepted compared to the laparoscopic approach. This was due to the belief that intense foreign body reaction and dense adhesions around the sponge may make the laparoscopic approach difficult. However, laparoscopy can prove to be beneficial with its advantages of early ambulation, reduced post-op pain, cosmetically improved results and shorter length of hospital stay.
Conclusion
All precautions must be taken to avoid retention of surgical sponge post-surgery. Case reports in which laparoscopy is used to retrieve gossypiboma are rare. The authors recommend the use of laparoscopy as a therapeutic option in the event of such mishaps.
Keywords: Gossypiboma, Laparoscopy, Retained surgical sponge
Highlights
-
•
Gossypiboma is undoubtedly one of the most unwanted and undesirable complication of a procedure for any surgeon with legal implications.
-
•
We present a case of an adult female who presented with a painless abdominal mass. Imaging was done and a diagnosis of gossypiboma was made.
-
•
The gossypiboma was successfully retrieved by the laparoscopic approach. Case reports in which laparoscopy is used to retrieve gossypiboma are rare.
-
•
Once suspected, the minimally invasive surgical approach should be considered for the management of gossypiboma.
1. Introduction
The term gossypiboma is used to depict a retained surgical sponge in the body after a surgery [1]. Various synonyms such as textiloma, muslinoma, gauzeoma, cottonoma, have been used in literature [[2], [3], [4]]. It is an avoidable complication of a surgery which can be disastrous for the patient and have medico-legal implications for the surgeon.
We report a case of a retained surgical sponge, 6 months after an emergency surgery in view of a ruptured ectopic pregnancy. The laparoscopic approach was successfully used for the retrieval of the surgical sponge.
This case has been reported in line with the SCARE criteria [5].
2. Case report
An adult P1L1E1 female presented to the surgery OPD of Atal Bihari Vajpayee Institute of Medical Sciences and Dr Ram Manohar Lohia Hospital, New Delhi with a painless abdominal mass which progressively increased in size in the past 4 months. She denied any history of fever, vomiting, or obstruction of bowel. She underwent emergency surgery for a ruptured ectopic pregnancy 6 months back at some other health centre. She also had a caesarean section 4 years back at some other hospital.
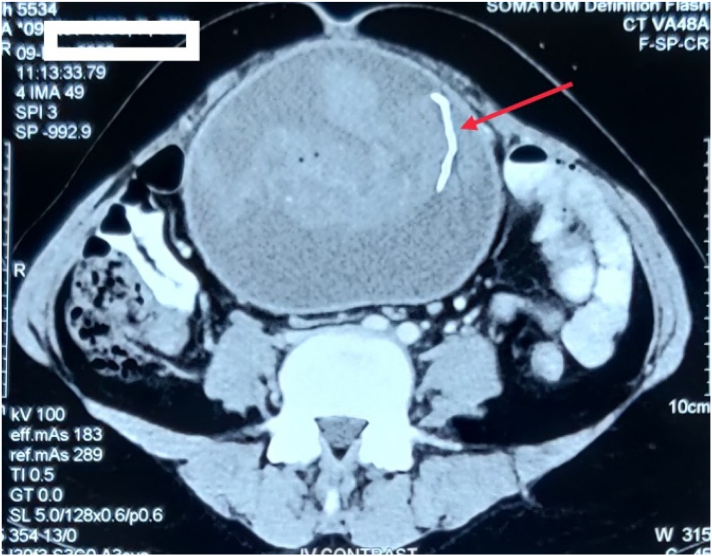
On abdominal examination, two vertical paramedian scars of previous surgeries were visible in the infra-umbilical region. A well-defined, large, cystic swelling of size approximately 10 cm × 10 cm occupying the centre of abdomen was palpable (Fig. 1). The swelling was mobile in all directions. Blood work was unremarkable. On computed tomography scan of the abdomen, a well-defined heterogenous cystic lesion of size 9.8 cm × 9.2 cm × 7 cm was noted intraperitoneally. Few air foci with a hyperdense tubular structure within the lesion were seen, suggestive of a retained surgical sponge with its radio-opaque marker also visualised (Fig. 2).
Fig. 1.
Pre-op image of the large swelling in the centre of the abdomen.
Fig. 2.
Arrow mark showing radio-opaque marker in the CT image of the abdomen.
Laparoscopic removal of the retained surgical sponge was planned. The procedure was performed by the unit head with a career of 20 years in advanced laparoscopy. With the patient laid supine and under general anaesthesia, the Veress needle was inserted at the Palmer's point to create pneumoperitoneum [6]. The periumbilical entry site was avoided in view of the large, central, cystic swelling, and in anticipation of dense adhesions around it. A 5 mm trocar was inserted at the Palmer's point after removing the Veress needle. A 0o high definition telescope was used for laparoscopy through the 5 mm port. Rest of the ports were inserted under vision at positions as depicted in Fig. 3. A 10 mm epigastric port to the left of falciform ligament was inserted and another 10 mm port at the level of umbilicus in the anterior axillary line.
Fig. 3.

Position of the laparoscopic ports.
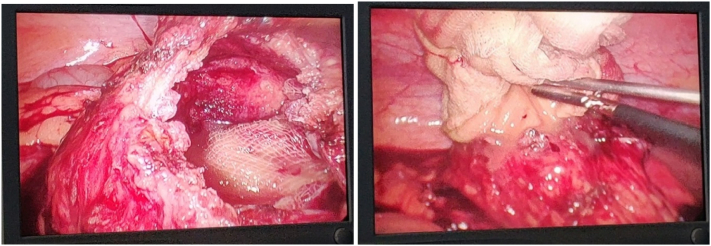
Intra-operatively a large cystic mass containing the surgical sponge encapsulated by omentum was found (Fig. 4). The mass was densely adhered to parietal wall at the previous incision site. Careful dissection was done to release the omental adhesions from the parietal wall using an ultrasonic energy device. Posterior dissection was not done since the cyst wall was adherent to the bowel. The cyst was opened at its apex and approximately 300 ml exudative fluid was suctioned. The surgical sponge was seen lying inside the cyst. It was taken out from the cavity and retrieved through anterior axillary port in a way similar to the gastric sleeve of sleeve resection. The cyst was marsupialized by excising the thick cyst wall all around its opening. After a thorough peritoneal lavage, a 16 Fr drain was placed in the pelvic cavity through the left lower quadrant port. All port sites were closed using nylon suture. Post-operatively, the patient was given intravenous injection ceftriaxone.
Fig. 4.
Retrieval of the surgical sponge from the cyst encapsulating it.
Histopathology of the cyst wall was suggestive of chronic granulomatous inflammation. Culture of the cyst fluid was sterile. The patient was mobilized on post-operative day (POD) 1 and allowed oral liquid diet on POD2. The pelvic drain was removed on POD4 in view of decreased output (<30 ml) and the patient was discharged on the same day. No complications were encountered at a four-week follow-up.
3. Discussion
Despite the advancement of techniques in modern surgery, the age-old problem of retained surgical sponge remains a nightmare for surgeons. Wilson et al. first reported a case of gossypiboma in 1884 [7] and its incidence varies between 1 in 8000 to 18,000 abdominal surgeries [8].
Gossypiboma has variable presentation depending upon the size, site, and inflammatory response. The patient may remain asymptomatic for a variable period or may present with vague pain and formation of a mass. An exudative response leads to abscess formation around the foreign body whereas an aseptic fibrinous response leads to encapsulation of the surgical sponge by avascular tissue. Often, the sponge erodes into the bowel wall due to pressure leading to fistula formation and rarely, can even be extruded with faeces [9,10].
Emergency procedures with heavy blood loss, change of scrub nurse, long duration surgeries, and obese patients are some of the major risk factors for this condition identified by Lincourt et al. [11]. In our case emergency surgery for ruptured ectopic pregnancy is the risk factor.
X-ray, ultrasound, computed tomography, and magnetic resonance imaging can all aid in the diagnosis of gossypiboma. Presence of a mass with air-foci within it, and a radio-opaque marker can straightaway lead to the diagnosis, as was in our case. However, expert radiological opinion may be needed in the absence of such marker [12,13].
Traditionally, the open approach for the removal of the sponge was more accepted compared to the laparoscopic approach. This was due to the belief that intense foreign body reaction and dense adhesions around the sponge may make the laparoscopic approach difficult. However, laparoscopy can prove to be beneficial with its advantages of early ambulation, reduced post-op pain, cosmetically improved results and shorter length of hospital stay. There are limited case reports of laparoscopic removal of gossypiboma and therefore this approach should be encouraged to minimize morbidity to the patient [14].
4. Conclusion
Gossypiboma can not only lead to significant morbidity to the patient, but can also lead to serious medico-legal consequences along with public and professional embarrassment to the surgeon. It is thus the combined responsibility of the surgeon and nursing staff to prevent such errors at all cost. The authors recommend the use of laparoscopy as a therapeutic option in the event of such mishaps.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
No ethical approval necessary.
Funding
None.
Guarantor
Dr Rohit Chauhan.
Research registration number
Not applicable.
CRediT authorship contribution statement
Dr Neeraj Saxena - study concept and design
Dr Dinesh Kumar Kardam - data collection
Dr Rohit Chauhan - data collection, analysis, and writing the paper
Dr Tayod Chaudhary - data analysis and interpretation
All the authors have read and approved the final manuscript.
Declaration of competing interest
None.
References
- 1.Margonis E., Vasdeki D., Diamantis A., Koukoulis G., Christodoulidis G., Tepetes K. Intestinal obstruction and ileocolic fistula due to intraluminalmigration of a gossypiboma. Case Rep. Surg. 2016 doi: 10.1155/2016/3258782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sistla S.C., Ramesh A., Karthikeyan V.S., Ram D., Ali S.M., Subramaniam R.V. Gossypiboma presenting as coloduodenal fistula—report of a rare case withreview of literature. Int. Surg. 2014;99:126–131. doi: 10.9738/INTSURG-D-13-00057.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tacyildiz I., Aldemir M. The mistakes of surgeons: “gossypiboma”. Acta Chir. Belg. 2004;104(1):71–75. doi: 10.1080/00015458.2004.11679521. [DOI] [PubMed] [Google Scholar]
- 4.Mouhsine E., Halkic N., Garofalo R., Taylor S., Theumann N., Guillou L. Soft tissue textiloma: a potential diagnostic pitfall. Can. J. Surg. 2005;48(6):495. [PMC free article] [PubMed] [Google Scholar]
- 5.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 6.Kondrup J.D., Sylvester B. Palmer’s point – go for it! The technique of LUQ anddirect view entry. JMIG. 2012;19(Supplement (6)) doi: 10.1016/j.jmig.2012.08.506. (Nov-Dec) [DOI] [Google Scholar]
- 7.Wilson C.P. Foreign bodies left in the abdomen after laparotomy. Gynecol. Tr. 1884;9:109–112. [Google Scholar]
- 8.Gawande A.A., Fisher E.S., Gruber J., Rosenthal M.B. The cost of health care – highlights from a discussion about economics and reform. N. Engl. J. Med. 2009;361(15):1421–1423. doi: 10.1056/NEJMp0907810. [DOI] [PubMed] [Google Scholar]
- 9.Patial T., Rathore N., Thakur A., Thakur D., Sharma K. Transmigration of a retained surgical sponge: a case report. Patient Saf. Surg. 2018;12 doi: 10.1186/s13037-018-0168-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agrawal H., Gupta N., Krishengowda U., Gupta A.K., Naskar D., Durga C.K. Transmural migration of gossypiboma: a rare cause of acute abdomen. Indian J. Surg. 2018;80:84–86. doi: 10.1007/s12262-017-1660-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lincourt A.E., Harrell A., Cristiano J., Sechrist C., Kercher K., Heniford B.T. Retained foreign bodies after surgery. J. Surg. Res. 2007;138(2):170–174. doi: 10.1016/j.jss.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 12.Kim H.S., Chung T.S., Sun S.H., Kim S.Y. MR imaging findings of paravertebral gossypiboma. Am. J. Neuroradiol. 2007;28(4):709–713. [PMC free article] [PubMed] [Google Scholar]
- 13.Malhotra M.K. Migratory surgical gossypiboma-cause of iatrogenic perforation: case report with review of literature. Niger. J. Surg. 2012;18(1):27–29. doi: 10.4103/1117-6806.95486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sankpal J., Tayade M., Rathore J., Parikh A., Gadekar D., Sa S.F. Oh, my gauze !!!-a rare case report of laparoscopic removal of an incidentally discovered gossypiboma during laparoscopic cholecystectomy. Int. J. Surg. Case Rep. 2020;72:643–646. doi: 10.1016/j.ijscr.2020.04.058. Epub 2020 May 16. PMID: 32513591; PMCID: PMC7365772. [DOI] [PMC free article] [PubMed] [Google Scholar]