Abstract
Background
The drive to eliminate viral hepatitis by 2030 is underway. However, locally generated data on active infection is required to focus such efforts. We performed a regionally-inclusive survey to determine prevalence of active HCV, genotypes and related factors among Ugandan blood donors.
Methods
Participants from regional blood banks and blood collection centers were surveyed for information on demographic, clinical and lifestyle factors. Blood was assayed for HCV infection, HCV genotypes and subtypes. Logistic regression was performed to determine factors associated with active HCV infection.
Results
Of 1243 participants, 1041 (83.7%) were male, average age (SD), 27.7 (9.8). Prevalence of active HCV infection was 7.8% and we identified 3 genotypes. Median age (adj. OR (95% CI) = 1.03 (1.01–1.06), p-value = 0.040)), Northern region of birth versus Central or Eastern (adj. OR (95% CI) = 10.25 (2.65–39.68), p-value = 0.001)), Northern residence, versus Central or Eastern (adj. OR (95% CI) = 0.23 (0.08–0.65), p-value = 0.006)), and being married (versus single/divorced) adj. OR 2.49(1.3–4.79), p-value = 0.006 were associated with active HCV infection.
Conclusion
Targeted interventions in at-risk populations coupled with linkage to care and treatment will help achieve the WHO elimination goals in this setting.
Keywords: Hepatitis C, blood donors, Uganda
Introduction
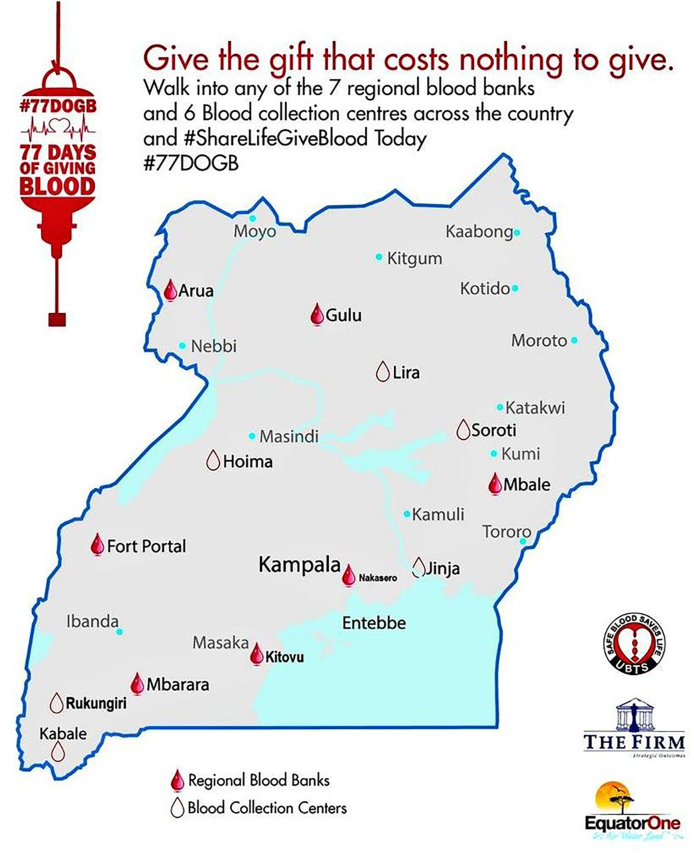
Globally hepatitis C virus (HCV) sero-prevalence is estimated at 2–3% with 71.1 million persons having active infection. In Africa, exact estimates have been difficult to define due to limited population data, but HCV is likely to have a high prevalence mainly due to unsafe medical procedures and injection practices that could predispose to infection transmission.1,2 (see Fig. 1)
Fig. 1.
Map of Uganda showing regional blood transfusion offices and blood collection centers.
Several HCV studies have been conducted in Uganda, most of them clinical, including children with sickle cell anemia, patients in medical emergency units, and HIV infected patients.3,4 These studies have shown an HCV antibody prevalence varying from 0 to 7%, and viremia ranging from 2 to 3%, but none has determined the national HCV prevalence. An initial study performed among blood donors using radioimmunoblot assay (RIBA) showed an antibody prevalence of 4.1% but this study was conducted in one region and could not establish if samples that tested positive had chronic HCV infection as nucleic acid testing (NAT) was not done.5
In line with the World Health Organization (WHO) declaration of elimination of viral hepatitis by 2030,6 there is a need to know the burden of viral hepatitis by testing and linkage to care. While the burden of hepatitis B (HBV) is relatively well defined in Uganda, this is not the case for HCV where it is thought that most infections are due to needle contamination, either nosocomially or through traditional scarifications. The role of other factors including injection drug use or sexual transmission have also not been determined. Micro-elimination of HCV has been adopted as a feasible approach to set achievable HCV eradication goals. It is a concept that entails eradicating HCV from targeted sections of the population as a progressive step to eventually achieve national HCV elimination. Regardless of how, setting up plans for elimination will be difficult without provision of national data regarding HCV distribution and determining the focus of infection for micro-elimination. Studies in Uganda have also reported false positive reactions with antibody testing, making it difficult to get actual estimates of the distribution of infection.4,5
In this study we aimed to determine the distribution of active HCV infection (including genotype distribution) and correlates of active infection in Uganda. This would form a proxy for a national prevalence and provide a basis for HCV elimination interventions.
Methods
Study site and setting
The study used the existing infrastructure of Uganda blood transfusion service (UBTS). The UBTS is a semi-autonomous, centrally coordinated organization in the Uganda's Ministry of Health. It is centrally located within the capital city Kampala, with services decentralized to all regions of the country-Western, Central, Northern and Eastern. The service operates within the framework of the National Health Policy and is mandated to provide sufficient, safe blood and blood components through voluntary blood donations for appropriate use in health care service delivery.
The study was performed at selected blood bank sites and blood collection centers in the North, Central, Eastern and Western regions. Blood banks are located within or near regional referral hospitals in each region.
Blood donation is voluntary. All donor blood undergoes routine screening for HIV, HBsAg, HCV antibody and syphilis before blood is released for use. Blood found to be contaminated by any of these infections is discarded. Donors are however informed on their infection status and usually referred for care, although linkage to care is not done systematically.
The UBTS protocol for screening donor blood
All donor blood was screened at the blood bank for HCV antibody, HBsAg, HIV and syphilis using a multiple test system Architect ci8200-system (Abbott, Weisbaden, Germany). Anti-HCV reactive samples were taken through a second line testing using Murex anti-HCV ELISA, V 4, (Diasorin, South Africa). If this was still reactive, the sample was declared “confirmed positive” and blood discarded. All regional blood banks are equipped to carry out donor blood screening for HBsAg, anti-HCV, anti-HIV and syphilis serologies.
The study used this screening protocol. Since fresh samples were to be drawn for this study, all those who were HCV antibody positive using the protocol were called back to have the study explained to them and get invited to participate.
Study design
This was a cross-sectional study design. We recruited participants from Gulu and Lira (North), Mbale and Soroti (East), Nakasero (Center) and Mbarara (West) regions, based on UBTS’ data on distribution of anti-HCV positivity (Arua - 6%, Fort portal - 5%, Mbale - 10.8%, Gulu - 17.1%, Mbarara - 4.6%, Nakasero - 7%).
Study procedures
Participant recruitment and data collection
All donors with blood being discarded due to HCV using the UBTS protocol were called by the blood bank staff through telephone contacts. At this visit, study staff explained the study to them and asked them to participate. Those willing to join were then taken through a consenting process for participation and for sample storage for future studies.
Each participant then completed a self-administered questionnaire that collected data on age, gender, number of life time sexual partners, history of blood transfusion, intravenous drug use, scarifications (cosmetic or therapeutic), tattoing, ethnic group, education, marital status, place of birth, place of residence, occupation, history of contact with a jaundiced person, previous blood donation, previous hospitalization, and a medical history focused on liver disease. We requested participants to allow us to use their routine test results performed at the blood bank, including HBsAg, anti-HCV, HIV and syphilis, and these were recorded in the data collection tool. The blood collected was assayed and analysed for complete blood count (CBC), liver function tests (LFTs), renal function tests (RFTs), HCV viral load assessment ± genotype and subtypes and anti-HBV core antibodies.
Participants were recalled after 3 weeks to be issued with their results. Participants with detected virus were referred to regional hospitals where hepatitis services are offered.
Laboratory procedures
Trained regular blood bank staff performed phlebotomies by venipuncture from each participant. Twenty mls of blood were drawn and transferred to the MBN laboratory, a commercial certified laboratory at the different recruitment sites. Sample processing and temporary storage at −20° Celsius were performed.
Qualitative HCV PCR was determined using AmpliSens HCV-FRT PCR Assay (3A Novogireevskaya Street Moscow 111123 Russia), reported as positive or negative. Samples that tested PCR positive were then reflexed to the HCV viral load test performed on the Roche COBAS 6800 HCV Test (Roche Diagnostics, USA) for quantitative RNA detection with lower limit of detection of 20 IU/mL. The same system was used for genotyping, and running genotypes 1 through 6 with subtypes 1а, 1b, 2, 3a, 4, 5a, 6.
Data management and analysis
Data were entered into Epidata, cleaned and exported to STATA (version 14.0) for statistical analysis. Quality assurance of this process was undertaken to ensure authenticity, completeness, and clarity of the data collected.
Statistical analysis
Descriptive analysis was performed to obtain summary statistics of variables, including means (standard deviation) for continuous variables and proportions for categorical variables. Prevalence of chronic HCV infection was estimated as a single proportion, with 95% CI, of samples that tested positive by NAT PCR assay, out of the total samples. Analysis of genotype and sub-type distribution by region was also done and presented.
We performed bivariable and multivariable logistic regression analyses to evaluate relationships between selected clinical and socio-demographic variables and chronic HCV infection. A p-value of 2.0 was used as a cut-off for the selection of variables entered into the multiple logistic regression model, and using a forward selection approach, a parsimonious model was obtained which showed factors associated with chronic HCV infection. A p–value of <0.05 and 95% confidence intervals were used to define statistical significance.
Ethical considerations
This study recruited consenting adults (18 years or more) presenting voluntarily to donate blood. Participants with chronic HBV infection were referred to regional referral hospitals by a physician, for hepatitis services as per the Ministry of Health guidelines. The protocol was approved by the ethics committee of the Makerere University College of Health Sciences School of Medicine Research and Ethics Committee (SOMREC, REF REC 2018 184)) and registered with the Uganda National Council of Science and Technology (UNCST, SS 4870)).
Results
During the period of June 2019 to March 2020, a total of 1243 participants were recruited from the regional blood banks and blood collection centers, as summarized in Table 1. Of these participants, 657 were from the Eastern region, while the Western region with 96 participants had the lowest recruitment proportion.
Table 1.
Regional distribution of blood donors with positive anti-HCV test results recruited in the study, 2019–2020 (N-1243).
| Region | Participants |
|---|---|
| Central (Nakasero) | 251 (20.2) |
| Eastern (Mbale, Soroti) | 657 (52.9) |
| Northern (Gulu, Lira) | 239 (19.2) |
| Western (Mbarara) | 96 (7.7) |
| Total | 1243 |
Participant background characteristics
The majority of participants (1024, 83.7%) were male, average age (SD) was 27.7 (9.8). More than half of them were born (710, 57%) and resided (659, 53%) in the Eastern region. About half (612, 49.2%) had a secondary education and almost a third (341, 27.9%) had post-secondary education. The majority (714, 57.4%) were single, while more than a third (466, 37%) self-identified as Catholic (provided as additional file 1).
Prevalence and genotype distribution of active HCV infection
As shown in Table 2, out of 1243 participants, HCV PCR assay results were available for 1227. Overall, 96 (7.8%) had active HCV infection. The Eastern region had the highest number with 69 (71.9%) cases while the Western region had none.
Table 2.
Regional distribution of active HCV cases and HCV genotypes 1 and 4.
| Region | HCV cases n(%), (N = 96) | Genotype 4an(%), N = 68 | Genotype 1an (%), N = 43 |
|---|---|---|---|
| Northern | 13 (13.5) | 9 (13.2) | 8 (18.6) |
| Eastern | 69 (71.9) | 48 (70.7) | 28 (65.1) |
| Central | 14 (14.6) | 11 (16.2) | 7 (16.3) |
| Western | 00 (0.0) | 00 (0.0) | 00 (0.0) |
Mixed infections occurred in a number of patients.
HCV genotypes
Out of 96 active HCV infections, three genotypes were identified; genotype 1, 4 and 5. For 14/96 active infections, no HCV genotypes were isolated. The overall distribution of HCV genotypes was: genotype 4: 68/96 (70.8%), genotype 1: 43 (44.8%) genotype 5: 1 (1.0%). Several individuals had more than one genotype (mixed infection). This mixed infection was found in 37/96 participants, with 36 of them having both genotypes 1 and 4, and only 1 participant having both genotypes 1 and 5, as shown in Table 3. For genotype 4, the regional distribution was as follows; 11/68 (16.2%), 9/68 (13.2%) and 48/68 (70.7%) were from Central, Northern and Eastern regions, respectively. For genotype 1, 7/43 (16.3%), 8/43 (18.6%) and 28/43 (65.1%) were from Central, Northern and Eastern regions respectively. Only 1 participant (not shown in Table) had genotype 5 and was from the Eastern region. Overall in all three regions, genotype 4 was predominant.
Table 3.
Bivariable and multivariable analysis of factors associated with active HCV infection.
| Unadjusted OR |
Adjusted OR |
|||||
|---|---|---|---|---|---|---|
| Characteristic | n (%) | (95%) CI) | p-value | (95%) CI) | p-value | |
| Gender | ||||||
| Male | 79(7.7) | 1.00 | 1.00 | |||
| Female | 17(8.9) | 1.18(0.68–2.05) | 0.551 | 1.78(0.98–3.25) | 0.060 | |
| Age | ||||||
| Mean (SD) | 27.8 (9.8) | 1.05(1.03–1.06) | <0.001 | 1.03(1.00–1.06) | 0.039a | |
| Education | ||||||
| Primary or lower | 29(11.3) | |||||
| Secondary | 40(6.6) | 0.56(0.34–0.92) | 0.023 | |||
| Post-Secondary | 27(8) | 0.68(0.39–1.18) | 0.175 | |||
| Marital status | ||||||
| Single | 31(4.4) | 1.00 | ||||
| Married | 62(12.6) | 3.13(2.00–4.90) | <0.001 | 2.49(1.3–4.79) | 0.006a | |
| Separated/divorced | 3(9.4) | 2.24(0.65–7.77) | 0.203 | 1.47(0.35–6.17) | 0.595 | |
| Region of residence | ||||||
| Central | 14(6.1) | 1.00 | ||||
| Northern | 13(5.9) | 0.96(0.44–2.09) | 0.918 | 0.23(0.08–0.65) | 0.006a | |
| Eastern | 69(10.6) | 1.80(0.99–3.27) | 0.052 | 1.64(0.70–3.80) | 0.252 | |
| Region of birth | ||||||
| Central | 4(3.1) | 1.00 | ||||
| Western | 1(0.8) | 0.26(0.03–2.34) | 0.229 | 0.7(0.07–7.06) | 0.762 | |
| Northern | 20(8.4) | 2.93(0.98–8.76) | 0.055 | 10.26(2.65–39.74) | 0.001a | |
| eastern | 70(9.9) | 3.51(1.26–9.78) | 0.017 | 2.23(0.61–8.08) | 0.223 | |
| Other | 1(3.3) | 1.09(0.12–10.17) | 0.937 | 1.21(0.13–11.64) | 0.870 | |
| Number of life time sexual partners | ||||||
| Median (IQR) | 2 (0–4) | 1.04(1.01–1.07) | 0.018 | |||
| Occupation | ||||||
| Peasant/Casual labourer | 45(12.8) | 1.00 | ||||
| Civil/Public servant | 13(7) | 0.51(0.27–0.97) | 0.733 | |||
| Businessman/Owner | 16(7.8) | 0.58(0.32–1.05) | 0.266 | |||
| Student | 19(4.8) | 0.34(0.20–0.59) | 0.001 | |||
| Ever been transfused with blood | ||||||
| No | 89(7.7) | 1.00 | ||||
| Yes | 7(13) | 1.8(0.79–4.09) | 0.163 | |||
| Ever been hospitalized | ||||||
| No | 53(6.7) | 1.00 | ||||
| Yes | 41(10) | 1.55(1.01–2.38) | 0.043 | |||
| Ever had any surgical operations | ||||||
| No | 83(7.6) | 1.00 | ||||
| Yes | 13(10.2) | 1.37(0.74–2.54) | 0.312 | |||
| Injection drug use | ||||||
| No | 92(7.7) | 1.00 | ||||
| Yes | 4(12.5) | 1.71(0.59–4.98) | 0.326 | |||
| Needle prick | ||||||
| No | 80(8) | 1.00 | ||||
| Yes | 13(7.3) | 0.91(0.49–1.68) | 0.774 | |||
| Ever had cuts on body | ||||||
| No | 88(8.1) | 1.00 | ||||
| Yes | 8(6.2) | 0.76(0.36–1.59) | 0.462 | |||
| Ever been in contact with a jaundiced person | ||||||
| No | 77(7.7) | 1.00 | ||||
| Yes | 17(9.1) | 1.21(0.69–2.09) | 0.495 | |||
| Ever had tattoos on body | ||||||
| No | 94(8) | 1.00 | ||||
| Yes | 2(4.3) | 0.51(0.12–2.14) | 0.358 | |||
Statistically significant.
Other transfusion transmissible infections (TTIs)
Overall, there were few participants with other TTIs. Out of 1200 donors with results of TTIs, 26 (2.2%) were HBsAg positive, 9 (0.8%) HIV seropositive, 15 (1.3%) positive for syphilis. Of all these, 1 participant was HCV antibody positive/HIV positive, 1 HCV/HBV and 2 HCV/Syphilis positive.
Factors associated with HCV infection
In multivariable logistic regression analyses (Table 3.), median age (adj. OR (95% CI) = 1.03 (1.01–1.06), p-value = 0.040)), being in a marital union, compared to being single, or divorced/separated (adj. OR (95% CI) = 2.48 (1.29–4.77), p-value = 0.006)), residing in the Northern region, compared to the Central or Eastern regions (adj. OR (95% CI) = 0.23 (0.08–0.65), p-value = 0.006)), and having been born in the Northern region (adj. OR (95% CI) = 10.25 (2.65–39.68), p-value = 0.001)), were associated with having active HCV infection.
There was a 3% increase in risk of having active HCV infection for each unit rise in median age. Also, having been born in the Northern region was associated with a ten-fold increase in risk, whereas residing in the Northern region was associated with a 77% reduced risk of having active HCV infection. Being in marital union was associated with a two-fold increase in risk of active HCV infection, compared to being single.
Also, being female tended to be associated with active HCV infection, though this estimate did not reach statistical significance in multivariable models.
Factors including history of needle pricks, body piercing or tattooing, history of injection drug use, blood transfusion, surgical operations, and of contact with a jaundiced person were not associated with active HCV infection.
Discussion
In this survey of a regionally-inclusive sample of blood donors, we found a prevalence of active HCV infection of 7.8% among donors who screened anti-HCV positive at the blood bank, and identified 3 genotypes. We identified age, region of birth and residence as well as marital status, as important factors associated to active HCV infection which could be effectively targeted for micro-elimination.
The finding of 7.8% of active infections in HCV antibody positive blood donors is high when compared to the blood bank protocol. This has already been highlighted before in this country where high rates of false positive reactions have been seen using various antibody assays, including enzyme linked assays.4,5 This also implies that there could be unnecessarily high rates of blood rejection in addition to causing anxiety to blood donors especially when treatment is not yet universally available in the country.
An even lower prevalence of co-infections with HIV, HBV and syphilis has been reported in other regions7, 8, 9
Our sample reported 3 HCV genotypes, with genotype 4 as the predominant one across regions, followed by genotype 1. This finding is consistent with current data on genotype distribution within Sub-Sahara Africa, where genotype 4 is common in Eastern Africa10,11 and genotype 1 and 2 in West Africa.12 In addition, a substantial proportion of our participants had two genotypes. This finding underscores the relevance of choosing pangenotypic directly acting antivirals for treatment of active HCV infection in this context where genotyping is likely to be unaffordable.13
We found several socio-demographic factors to be linked to active HCV infection. The finding of age as a risk factor is not unique to this study. A similar finding was described in a recent nation-wide survey in Rwanda,14 where older age was a risk factor for HCV infection. This is likely plausible as age is a proxy measure of time available for an individual to be exposed to potential risk factors. Studies in Pakistan and India8,9 have also found older age to be related to increased HCV risk among persons who regularly receive blood transfusions.
Being in a marital union compared to being single was associated with increased risk of HCV infection, contrary to the Rwandan study where being widowed, divorced or separated was a reported HCV risk factor. An important finding in this study was the observed relationship between gender and having active HCV infection. Being female tended to be associated with having active HCV infection. This relationship needs further evaluation in this setting, given that most studies have reported men to be at greater risk of HCV infection and disease progression.
The region was an important correlate of active HCV infection. Being born in the Northern region increased the risk , while residing in the same region was associated with a lower risk . Studies of HBV in Uganda have shown a higher burden of disease in the Northern and Northeastern regions than in other regions, with low rates in the Southwest where Mbarara is located,15,16 and our findings seem to corroborate those of HBV surveys. A plausible explanation for this observation is that HCV shares routes of transmission and other lifestyle behaviors that could increase exposure to infection.17, 18, 19 It remains to be explained why the Northern region has a higher risk of both HCV and HBV infections.
In our sample, history of exposure to blood through body cuts, surgical operations, blood transfusion and contact with a person who had jaundice did not show an association with HCV infection. This finding is contrary to a recent nation-wide study in Rwanda7 where scarification was associated with an elevated risk. Our failure to find an association could likely be due to a smaller sample size. In addition, our study population of blood donors is a highly selected population, with the possibility that individuals who have had such exposures may not qualify to donate blood and may be screened out during pre-donation assessments, in favor of healthier individuals.20
We found very few patients with other transfusion transmissible infections, a result of active screening of donor blood.
This study had notable limitations. Most of the information collected on socio-behavioral factors relied on self-reports, and as such, could not be assessed objectively. Also, recruitment did not achieve accurate regional balance and our sample size may have been underpowered to detect modest associations with some known HCV risk factors. The study also recruited in a highly selected population of blood donors. This therefore could not provide a national representation of the general population in the country. Larger studies may be warranted, especially in the general population, to further examine the prevalence of HCV active infection as well as associated factors in this setting. Our laboratory system could only identify genotypes 1 to 6 with limited sub-type detection, so we could have failed to detect genotypes such as genotype 7 that has been reported in some patients in sub-Saharan Africa.21 Nonetheless, our study used sensitive assays to determine active HCV infections, and coupled with rigorous statistical analyses, provides important findings to inform the initiation of HCV elimination efforts in Uganda.
Conclusion and recommendations
Our HCV screening intervention has resulted in increased detection of active HCV infection in an important population of blood donors, identified 3 genotypes and shown that current blood bank testing protocols lead to high rates of false positive detection of HCV antibody.
We recommend expansion of targeted interventions in at-risk populations such as in Eastern and Northern Uganda, to step up disease awareness, detection and linkage to care, thus propelling HCV micro-elimination goals. Better testing strategies will be needed in blood banks to provide more accurate results, reduce donor blood wastage and avoid anxiety among donors who are falsely found to be infected.
Statement of significance
The HCV burden in Uganda remains unknown, despite current global efforts geared towards viral hepatitis elimination as a public health threat by 2030. To support efforts for elimination, we performed a survey among blood donors across 4 regions of Uganda. Our survey found a high prevalence of HCV, identified three genotypes and several important correlates of active HCV infection. These findings support the efforts to scale-up testing and linkage to care and antiviral treatment, as key steps towards elimination of the public health risk due to HCV.
Contributions
JNM, BSA, PO, ES conceived the project, developed the proposal and spearheaded the data collection, JNM, LN, JN and MN performed the data analysis, GO and DBK led the laboratory analyses. All investigators reviewed the manuscript and approved the final version.
Ethical considerations
This study sought and obtained ethical clearance before study initiation, from the Ethics Committee of the Makerere School of Medicine, and from the Uganda National Council for Science and Technology.
Declaration of competing interest
PO received a grant for this study from Gilead Sciences.
Acknowledgments
Funding: This project was fully funded by Gilead Sciences under the grant ‘Conquering Hepatitis via Micro elimination (CHIME)’ grant ISR-UG-18-10468.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jve.2021.100041.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Karoney M.J., Siika A.M. Hepatitis C virus (HCV) infection in Africa: a review. Pan African medical journal. 2013;14(1) doi: 10.11604/pamj.2013.14.44.2199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blach S. Global prevalence and genotype distribution of hepatitis C virus infection in 2015: a modelling study. The lancet Gastroenterology & hepatology. 2017;2(3):161–176. doi: 10.1016/S2468-1253(16)30181-9. [DOI] [PubMed] [Google Scholar]
- 3.Namasopo S., Ndugwa C., Tumwine J. Hepatitis C and blood transfusion among children attending the sickle cell clinic at mulago hospital, Uganda. Afr Health Sci. 2013;13(2):255–260. doi: 10.4314/ahs.v13i2.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seremba E. Poor performance of hepatitis C antibody tests in hospital patients in Uganda. J Med Virol. 2010;82(8):1371–1378. doi: 10.1002/jmv.21817. [DOI] [PubMed] [Google Scholar]
- 5.Hladik W. Prevalence and screening costs of hepatitis C virus among Ugandan blood donors. Trop Med Int Health. 2006;11(6):951–954. doi: 10.1111/j.1365-3156.2006.01643.x. [DOI] [PubMed] [Google Scholar]
- 6.WHO Combating hepatitis B and C to reach elimination by 2030. Advocacy brief. 2016 https://www.who.int/hepatitis/publications/hep-elimination-by-2030-brief/en/ [Google Scholar]
- 7.Saini P.A. Hepatitis C virus: unnoticed and on the rise in blood donor screening? A 5 years cross-sectional study on seroprevalence in voluntary blood donors from central India. J Global Infect Dis. 2017;9(2):51. doi: 10.4103/0974-777X.205172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ehsan H. Prevalence of transfusion transmissible infections in beta-thalassemia major patients in Pakistan: a systematic review. Cureus. 2020;12(8) doi: 10.7759/cureus.10070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rawat A. Seroprevalence & changing trends of transfusion-transmitted infections amongst blood donors in a Regional Blood Transfusion Centre in north India. Indian J Med Res. 2017;146(5):642. doi: 10.4103/ijmr.IJMR_468_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kassa E., Bane A., Kefene H. Common genotypes and treatment outcomes of HCV infection among Ethiopian patients: a prospective study. Ethiop Med J. 2016;54(1) [PubMed] [Google Scholar]
- 11.Njouom R. Predominance of hepatitis C virus genotype 4 infection and rapid transmission between 1935 and 1965 in the Central African Republic. J Gen Virol. 2009;90(10):2452–2456. doi: 10.1099/vir.0.011981-0. [DOI] [PubMed] [Google Scholar]
- 12.Layden J.E. High frequency of active HCV infection among seropositive cases in west Africa and evidence for multiple transmission pathways. Clin Infect Dis. 2015;60(7):1033–1041. doi: 10.1093/cid/ciu965. [DOI] [PubMed] [Google Scholar]
- 13.Sonderup M.W. Hepatitis C in sub-Saharan Africa: the current status and recommendations for achieving elimination by 2030. The Lancet Gastroenterology & Hepatology. 2017;2(12):910–919. doi: 10.1016/S2468-1253(17)30249-2. [DOI] [PubMed] [Google Scholar]
- 14.Makuza J.D. Risk factors for viral hepatitis C infection in Rwanda: results from a nationwide screening program. BMC Infect Dis. 2019;19(1):688. doi: 10.1186/s12879-019-4322-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ochola E. High burden of hepatitis B infection in Northern Uganda: results of a population-based survey. BMC Publ Health. 2013;13(1):727. doi: 10.1186/1471-2458-13-727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bwogi J. Hepatitis B infection is highly endemic in Uganda: findings from a national serosurvey. Afr Health Sci. 2009;9(2) [PMC free article] [PubMed] [Google Scholar]
- 17.Riaz M. An overview of triple infection with hepatitis B, C and D viruses. Virol J. 2011;8(1):1–5. doi: 10.1186/1743-422X-8-368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fattovich G. Hepatitis C virus infection in chronic hepatitis B virus carriers. J Infect Dis. 1991;163(2):400–402. doi: 10.1093/infdis/163.2.400. [DOI] [PubMed] [Google Scholar]
- 19.Liu Z., Hou J. Hepatitis B virus (HBV) and hepatitis C virus (HCV) dual infection. Int J Med Sci. 2006;3(2):57. doi: 10.7150/ijms.3.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eller L.A. Reference intervals in healthy adult Ugandan blood donors and their impact on conducting international vaccine trials. PloS One. 2008;3(12):e3919. doi: 10.1371/journal.pone.0003919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Davis C. Highly diverse hepatitis C strains detected in sub‐saharan Africa have unknown susceptibility to direct‐acting antiviral treatments. Hepatology. 2019;69(4):1426–1441. doi: 10.1002/hep.30342. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.