Abstract
Background
Knowledge of how intrinsic capacity (IC) and neighbourhood physical environment shape functional ability (FA) trajectories in later life remains understudied. We investigated four-year trajectories of IC and their impact on FA trajectories and the association between neighbourhood physical environment and FA trajectories among community-dwelling older adults in Hong Kong, China.
Methods
We conducted a four-wave longitudinal study from 2014 to 2017 in Hong Kong with 2,081 adults aged 65 and above. FA was assessed by The Chinese Lawton Instrumental Activities of Daily Living Scale. We used cognition, affect, locomotion, sensory capacity, and vitality to capture the multiple domains of IC. Neighbourhood physical environment attributes included green space, land use diversity, and availability of facilities, assessed within 200- and 500-meter buffers of respondents’ homes. We used the parallel process of latent growth curve model.
Findings
IC (Unstandardized coefficient, β = −0.02, p<0.001) and FA (β = −0.20, p<0.001) each decreased significantly over time. Individuals with declines in IC experienced a faster decline in FA over time. Green space within a 200-meter buffer (β = 1.15, p = 0.023), the number of leisure (β = 0.03, p = .0.043) and public transport (β = 0.08, p = .0.003) facilities within a 500-meter buffer slowed the rate of FA decline.
Interpretation
The level of FA decreased over time in later life. Changes in IC shaped FA trajectories. Increased residential green space and the number of leisure and public transport facilities in the neighbourhood may help slow FA decline over time.
Funding
The Hong Kong Housing Society.
Research in context.
Evidence before this study
We searched Scopus, Web of Science, PubMed, ProQuest and PsycINFO for journal articles investigating the association between neighbourhood physical environment and functional ability, published up to 1 April 2021, without restrictions on language. We used three sets of keywords, “neighbourhood environment”, “functional ability”, and “older adults”, including possible variations of the terms and their synonyms. We identified two cohort and six cross-sectional studies, none of which included much information on the impact of neighbourhood physical environment on the continuous trajectory of functional ability. In particular, none of the studies incorporated the World Health Organizations (WHO) Healthy Ageing framework or the new concept of intrinsic capacity (IC) to examine the relationship between neighbourhood physical environment, IC and functional ability (FA).
Added value of this study
Our study is the first to apply confirmatory factor analysis (CFA) and the WHO’s multi-domain concept of IC to generate a composite IC score to test the Healthy Ageing framework. We used the continuous trajectory of functional ability as the outcome variable. We innovatively applied parallel latent growth curve modelling to estimate the relationships between the growth factors of IC and FA, and explored how changes of IC and neighbourhood physical environment jointly shape the trajectory of FA.
Implications of all the available evidence
Our findings suggest that the decline in IC was associated with a faster decline in FA among older adults, and neighbourhood physical environment attributes were associated with changes in FA over time. In particular, green space within a 200-meter buffer and the availability of leisure facilities and public transport with a 500-meter buffer attenuated downward trends in FA. We recommend that the development of age-friendly city initiatives should emphasize the provision of more residential green space and enhance the availability of leisure and public transport facilities in the community.
Alt-text: Unlabelled box
1. Introduction
Maintaining functional ability (FA) in later life is a longstanding public health policy goal. Worldwide, the prevalence of disability in old age, defined as functional limitations in instrumental activity of daily living, ranges from 5.7% to 21.7% [1], and incurs substantial costs to healthcare systems [3]. To provide a framework for action in public health, the World Health Organization (WHO) declared a Decade of Healthy Ageing (2020–2030) to reframe older people's health as a trajectory of FA rather than from a disability-based perspective [2]. FA is defined as all the health-related attributes that enable people to be and to do what they have reason to value [2]. The most essential FA for older adults is their ability to live independently in their community [3].
Instead of merely studying the onset of functional limitations, recent research has increasingly recognised the importance of understanding FA trajectories, because the change of FA can differ between individuals before and after the onset of functional limitations, as ageing is an ongoing and heterogeneous process [4]. Thus, investigating FA trajectories can provide more information on distinct subgroups in the ageing population to support public health policy development. Additionally, a close examination of FA trajectories can reveal valuable information on which factors affect the stability or accumulative loss in FA, contributing to more targeted prevention strategies.
One key factor affecting FA trajectories is intrinsic capacity (IC), defined as the composite of an individual's total underlying physical and mental capacities [3]. IC is a multidimensional construct representing the number of underlying competencies that an individual can tap to support their FA [5]. Previous studies have shown that each separate IC component is a predictor of adverse health events in later life [5]. However, these studies have focused on a single component of IC. Indeed, IC can be constructed as a composite of five domains of underlying physical and mental capacities: cognition, affect (e.g., depression), sensory function (e.g., hearing and vision), vitality (e.g., frailty), and locomotion (e.g., handgrip strength) [6], and should be considered simultaneously to provide a holistic profile of an individual's health status [6]. Although two recent studies moved from constructing the concept of IC to its validation and testing its impact on the prevalence rate of functional limitation over time [6,7], neither tested how changes in IC shape the FA trajectory.
Older adults’ FA can also be influenced by their immediate physical neighbourhood environment. The ecological model of ageing posits that older adults, particularly the oldest old and the most frail, tend to rely more on their neighbourhood physical environment for daily activities because their life activity space shrinks, and some are faced with various levels of mobility loss [8]. Neighbourhood physical environment can act as either a barrier or facilitator for older adults to age well. Lawton and Nahemow posited that unique combinations of personal competence (e.g., sensory loss, cognitive decline) and environmental features (e.g., the availability of facilities) can help lead to optimal functioning of older individuals, termed person-environment fit, or unfit [9].
Three important dimensions of neighbourhood physical environment may affect older adults’ FA, design (e.g., residential green space), diversity (e.g., land-use patterns), and destination (e.g., the availability of facilities) [10,11]. Green space has been recognised as an important setting for physical activities, a key factor enabling older adults to keep healthy [14]. Similarly, a neighbourhood characterised by diverse land use may offer more non-residential destinations for walking and reduce the risk of chronic disease [12]. Also, the availability of neighbourhood facilities, such as shops and public transportation, may facilitate more daily activities and transport-related journeys that may lower the risk of dependency among older adults [13,14]. Some existing research has found that older adults living in neighbourhoods with high residential green space, a high proportion of commercial and intermediate mixed land use, experience lower incidence of functional disability [14,15].
Although increasing attention has been paid to these three neighbourhood physical environment attributes, their importance in influencing FA trajectories in late life remains insufficiently recognised. Most existing research has been cross-sectional [13,[16], [17], [18], [19], [20]], and only two studies explored the longitudinal associations between neighbourhood physical environment and FA [14,15]. The latter studies were also limited by focusing on state transition (e.g., from no to one or more functional limitations), thus suppressing valuable information on FA trajectories preceding and occurring after these losses [2].
To address these gaps, the present study investigated how changes of IC and neighbourhood physical environment impact FA trajectories of older people, drawing on data from a four-wave longitudinal study conducted in public housing estates in Hong Kong. Hong Kong is characterised by compact, high-rise/high-density dwellings and mixed land use, presenting unique environmental features that may influence the FA trajectories of older adults [21]. Additionally, around 45% of older adults in Hong Kong live in poverty and 55.9% live in government-subsidised housing; most older residents have lived in public rental housing for more than 30 years [[22], [23], [24]]. Since low-income people rely more on their neighbourhood environment than those who are better off [25], studying older public rental housing residents presents an opportunity to explore the long-term effect of neighbourhood physical environment on FA. We proposed two research questions: (1) how do changes of IC influence the FA trajectory among low-income older people? (2) How do residential green space, land use mix, and the number of neighbourhood facilities influence the FA trajectory among low-income older people?
2. Methods
2.1. Study design and respondents
We conducted a cohort study between 2014 and 2017. Respondents were older adults aged 65 years and above, living in 12 public rental estates for low-income residents. Age-stratification random sampling was used to recruit respondents in three age strata (65–74 years, 75–84 years, 85 years and older), with target sample sizes for these groups of 50, 60, and 70, respectively, a total of 180 per estate. There was intentional over-sampling of the old-old (75–84 years) and oldest-old (85 years and older) age groups to take account of their higher attrition rates during a longitudinal study. Interviews were conducted during home visits by trained researchers. The process of data collection at each wave is illustrated in Supplementary Figure 1. Only data collected in 2014, 2015 and 2017 were used because the mechanical failure of one of the handheld dynamometers compromised the accuracy of handgrip strength data collected in 2016.
2.2. Ethical approval statement
The study was approved by the Human Research Ethics Committee of the University of Hong Kong (Reference Number: EA050814 & EA1610004). All respondents provided advanced written informed consent.
2.3. Measurements
2.3.1. Functional ability (FA)
FA was measured by The Chinese Lawton Instrumental Activities of Daily Living Scale (IADL), which has been validated in Hong Kong [26]. IADL comprises nine self-care items necessary for independent community living. The possible responses include: “not capable of doing it” (0), “need some help doing it” (1), and “fully capable of doing it and require no help to do it” (2). IADL scores range from 0 to 18, with a higher score indicating better FA. The Cronbach's alpha of this sample was 0.89.
2.3.2. Intrinsic capacity (IC)
We used the following measurements to capture the multiple domains of IC. Cognition was measured by the Cantonese Chinese Montreal Cognitive Assessment Version [27], comprising six cognitive domains of executive functions: attention, memory, orientation, abstraction and language [28]. Affect was measured by a validated Chinese version of the 15-item Geriatric Depression Scale [29]. Vitality was measured by the FRAIL Scale, comprising five components: fatigue, resistance, ambulation, illness, and weight loss, with the overall score ranging from 0 (“best”) – 5 (“worst”) [30]. Sensory capacity was measured by two single-item questions about respondents’ vision and hearing. The possible responses were “normal” (1), “minimal to moderate difficulty” (2), and “severe difficulty or no vision/hearing” (3). Locomotion was assessed by the handgrip strength and the steadiness [31]. We used a handheld dynamometer JAMAR Plus+Digital 563213 to test respondents’ handgrip strength (kg) [32]. Three values were recorded for each hand, and the average (mean) of three measures for each hand was used in the analysis. Steadiness was measured by a single-item self-report question inquiring whether respondents felt unsteady when walking and turning [33], with available responses of “moderate to severe unsteadiness” (0), “very little/minimal unsteadiness” (1), and “no unsteadiness” (2).
2.3.3. Environmental variables
We geocoded respondents’ residential addresses and employed spatial buffering analysis to create the road-network-based service area buffers adjusted by terrain and slope from respondents’ addresses to define the scope of their neighbourhoods. A road-network-based service area buffer encompasses all accessible streets tracing a given distance from a home address, as applied in previous studies [34]. ArcGIS 10.5 was used to perform geocoded and spatial buffering analysis. All neighbourhood physical environment measures were derived using a satellite image and ib1000 datasets provided by the Hong Kong government’s Lands Department. The 500- and 200-meter buffers were created to extract neighbourhood physical environment variables. The 500-meter buffer is regarded as the maximum comfortable walking distance between home and essential public services for older people [35], while 200 meter represents a short walking distance, the most immediate surrounding for older adults with functional limitations.
Green space was calculated by the percentage of natural greenery cover within the two selected buffers based on the Google Earth Engine [36].
Land use diversity was measured by entropy land use mix based on the evenness of distribution of five land-use types: residential areas, commercial/industrial buildings, institutions, open space, and others, within observed areas [37]. Values ranged from near 0, reflecting a single-use environment, to near 1, reflecting maximal mixed usage.
Availability of facilities. The availability of facilities was calculated by the number of each type of facility within the two buffers using Hong Kong’s GeoCommunity 3.0 Database. Five types of facility were included. Commercial facilities refer to supermarkets, shopping centres, markets, bazaars, and convenience stores. Community facilities refer to community centres, welfare centres and family service centres. Leisure facilities refer to parks, pavilions and minor open spaces. Public transportation refers to bus stops and railway stations. Healthcare facilities refer to clinics and hospitals.
2.3.4. Individual-level covariates
Control variables included age, sex, marital status, education, and the self-reported number of chronic diseases.
2.4. Statistical analysis
Descriptive analysis was conducted using Stata 15.1 software and modelling analysis using Mplus 8.3 software.
To answer the first research question, we performed a 2-step data analysis. First, we conducted confirmatory factor analysis (CFA) and generated a composite IC score for each study year. CFA is a statistical technique used to investigate causal relationships among latent and observed variables in a priori specified, theory-derived models [38]. Three separate CFAs were conducted to examine whether the data fitted the theoretically hypothesised one-factor model of IC for each study year. The omega coefficient (ω), defined as an estimate of the proportion of variance in the unit-weighted total score attributable to all sources of common variance, was calculated to understand the reliability of latent IC for each year [39]. A factor score for latent IC was generated from CFA by fixing the latent mean to 0 for each year, as suggested by previous research [7]. A factor score for IC was a linear combination of all the sub-domain measures of IC, weighted by the corresponding factor loading [40], which was used in subsequent analyses.
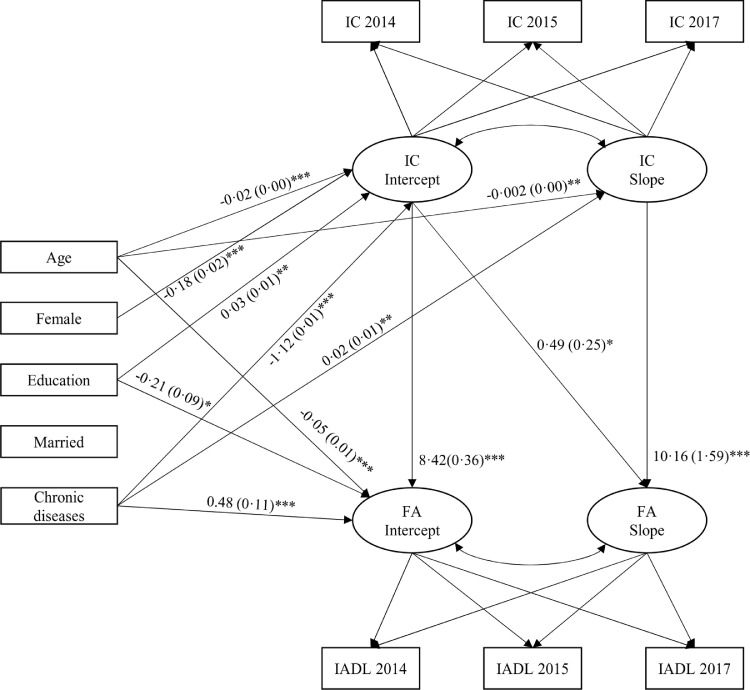
Second, we performed a parallel process of latent growth curve modelling with a stepwise approach [41]. Latent growth curve modelling is a method for modelling repeated measures as latent variables composed of a random intercept and random slope(s) that permit individual cases to have unique trajectories of change over time [42]. Intercept refers to the initial IC/FA status of the sample, while slope represents the change rate of IC/FA. The parallel process of latent growth curve modelling estimates the parameters of the growth factors (intercepts and slopes) of IC and FA and the relationship between the IC and FA growth factors. Thus, it was appropriate in this study [41]. We conducted two separate unconditional latent growth curve modelling to estimate the baseline (latent intercept) and change (latent slope) of IC and FA over time. We then added all covariates to the parallel process of latent growth curve modelling to examine the association between the change of IC and the FA trajectory. This model is graphically presented in Fig. 1.
Fig. 1.
Graphical representation of the parallel process of latent growth curve modelling to estimate baseline and change of IC and FA over time. IC=Intrinsic Capacity; FA=Functional ability; IADL= Instrumental Activities of Daily Living; only statistically significant paths are shown (unstandardised estimates) and standard error are displayed in parentheses. Model fit: χ2 = 258.57, df = 18, Root mean square error of approximation (RMSEA) = 0.080, Comparative fit index (CFI) = 0.963, Tucker-Lewis Index (TLI) = 0.907, Standardized root-mean-square residual (SRMR) = 0.032 *** p < 0.001; ** p < 0.01; * p < 0.05.
To answer the second research question, we added neighbourhood physical environment variables as predictors for latent intercept and slope of FA in the parallel process of latent growth curve modelling.
We conducted missing-data analysis using Little’s test with the command mcartest in Stata 15.1 software [43]. We first tested whether the data were missing completely at random, however, the results did not support the missing completely at random pattern. Then, we tested covariate-dependent missingness and found that data were missing at random (χ2 distance = 472.87, df = 472, p = 0.48). The available data on each variable are shown in Supplementary Table 1. Given the missing at random pattern, we ran CFA and models using a maximum likelihood estimation algorithm. The model fits the data well if it satisfies most of following criteria: χ2 statistic >0.05, comparative fit index and Tucker-Lewis Index >0.90, the root-mean-square error of approximation <0.06, and a standardised root-mean-square residual <0.08 [44]. Estimates with a p-value of < 0.05 were interpreted as statistically significant.
2.5. Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. TL had access to the full dataset and decide to submit the manuscript for publication.
3. Results
As Table 1 shows, the average age of the 2,081 respondents at baseline was 79.64 years (Standard Deviation, SD = 7.97), and 55.84% were women. Almost half (47.88%) had no formal education, and 59.53% were married. More than half (64.97%) reported two and more chronic diseases. In a 500-meter buffer, the average percentage of green space was 27% (SD=0.15), and the land use mix was 0.69 (SD=0.08). On average, commercial facilities comprised the greatest number of facilities (9.66, SD=6.10) and healthcare facilities the least (1.95, SD=1.91). Similar patterns of neighbourhood physical environment were found within a 200-meter buffer.
Table 1.
Baseline characteristics of respondents.
| Individual-level variables (N = 2,081) | Mean (S.D.) / N (%) | |
|---|---|---|
| Age, years (range = 65–101) | 79.64 (7.97) | |
| Women | 1,162 (55.84%) | |
| Education level | ||
| No formal education | 995 (47.88%) | |
| Primary | 636 (30.61%) | |
| Secondary | 406 (19.54%) | |
| Post-secondary | 41 (1.97%) | |
| Missing | 3 (0.14%) | |
| Marital status | ||
| Married | 1,234 (59.53%) | |
| Divorced/Widowed/Single | 839 (40.47%) | |
| Missing | 8 (0.38%) | |
| Number of chronic diseases | ||
| None | 282 (13.55%) | |
| One | 447 (21.48%) | |
| Two and more | 1,352 (64.97%) | |
| Built environment characteristics within 500- and 200- meter buffers of respondents' home | Mean (S.D.) | |
|---|---|---|
| 500-meter buffer | The percentage of green space (range = 0.06–0.57) | 0.27 (0.15) |
| Land use mix (range = 0.06–0.57) | 0.69 (0.08) | |
| Commercial facility (range = 1–25) | 9.66 (6.10) | |
| Community facility (range = 1–5) | 2.59 (1.28) | |
| Leisure facility (range = 2–16) | 7.04 (3.65) | |
| Transportation (range = 0–9) | 2.67 (2.29) | |
| Healthcare facility (range = 0–5) | 1.95 (1.91) | |
| 200-meter buffer | The percentage of green space (range = 0.01–0.37) | 0.17 (0.10) |
| Land use mix (range = 0.24–0.98) | 0.71 (0.17) | |
| Commercial facility (range = 0–6) | 1.54 (1.45) | |
| Community facility (range = 0–3) | 0.50 (0.71) | |
| Leisure facility (range = 0–7) | 1.35 (1.54) | |
| Transportation (range = 0–4) | 0.41 (0.77) | |
| Healthcare facility (range = 0–5) | 0.37 (0.95) | |
Notes: S.D. = standard deviation.
As Table 2 illustrates, all cognitive functions except attention significantly differed over time. The depression scores decreased over time. The level of steadiness, frailty and handgrip strength also differed significantly from 2014 to 2017. No difference over time was found for sensory impairment. The IADL scores also decreased over time.
Table 2.
Change of subdomains of intrinsic capacity and functional ability among older adults over time.
| Dimension | 2014 | 2015 | 2017 | Test for difference between means from 2014 to 2017 |
||
|---|---|---|---|---|---|---|
| Mean (S.D.) | Mean (S.D.) | Mean (S.D.) | F | p | ||
| Intrinsic capacities | ||||||
| Cognition | Executive | 2.72 (1.33) | 2.91 (1.39) | 2.8 (1.28) | 10.73 | <0.001 |
| Attention | 4.46 (1.57) | 4.56 (1.53) | 4.52 (1.52) | 2.57 | 0.08 | |
| Memory | 2.16 (1.94) | 2.31 (1.86) | 2.52 (1.89) | 17.61 | <0.001 | |
| Orientation | 5.47 (0.95) | 5.37 (1.05) | 5.22 (1.29) | 28.17 | <0.001 | |
| Abstraction | 1.06 (0.87) | 1.07 (0.85) | 0.89 (0.85) | 26.03 | <0.001 | |
| Language | 3.52 (1.59) | 3.68 (1.62) | 3.57 (1.62) | 5.98 | <0.001 | |
| Affect | Depression | 2.7 (3.17) | 2.45 (3.12) | 1.88 (2.90) | 32.87 | <0.001 |
| Vitality | Frailty | 0.80 (1.04) | 0.86 (1.06) | 0.94 (1.11) | 7.83 | <0.001 |
| Sensory | Vision impairment | 1.34 (0.50) | 1.26 (0.48) | 1.26 (0.50) | 12.88 | 0.25 |
| Hearing impairment | 1.25 (0.48) | 1.24 (0.47) | 1.26 (0.53) | 1.39 | 0.25 | |
| Locomotor | Steadiness | 1.56 (0.63) | 1.61 (0.60) | 1.54 (0.66) | 5.32 | 0.01 |
| Hand grip strength | 37.12 (16.14) | 39.07 (14.96) | 39.64 (15.13) | 30.84 | <0.001 | |
| Functional ability | ||||||
| IADL | 15.60 (3.40) | 15.51 (3.63) | 15.15 (4.11) | 14.43 | <0.001 | |
Notes: SD = standard deviation. IADL = Instrumental activities of daily living, with higher scores indicating better functional ability. Repeated measures ANOVA for the tests for the difference between means from 2014 to 2017. Six domains of cognition were measured by a Cantonese Chinese Montreal Cognitive Assessment Version, with higher scores indicating better cognition function; Depression was measured by 15-item Geriatric Depression Scale, with scores ranging from 0 to 15, with higher scores indicating more depressive symptom. The steadiness when walking was measured by a single-item self-report question that whether participants feel unsteady or at risk of losing their balance when walking and turning (range = 0–2), with higher scores indicating less unsteadiness. The frailty was measured by FRAIL scale (range = 0–5), with higher scores indicating more frailty. Vision and hearing were measured by two single-item questions about participants’ vision and hearing (range = 1–3), with higher scores indicating more impairment. The higher scores for handgrip strength indicates better conditions.
We conducted CFA for the IC subdomains. Most items loaded well (≥0.3) over time. The models fit the data well. These findings support the structural validity of IC as one general factor. The ω values for latent IC all reached significance, indicating that 75%, 72%, and 81% of the variance of the five subdomains can be attributed to the general IC scores in the three study years respectively, and suggesting that the total latent IC scores were sufficiently reliable measures of general factors (See Supplementary Table 2).
As shown in Table 3, two separate unconditional latent growth curve models were applied to capture the change of IC and FA over time. Model fits were good. On average, IC in our sample decreased significantly over the 4-year study period (β = −0.02, p<0.001), and older adults had different initial status (β = 0.18, p<0.001) and change rates in IC (β = 0.04, p<0.001). The intercept of IC was negatively associated with its slope (β = −0.04, p<0.001), revealing that respondents having higher initial IC tended to experience a steeper decline in IC over time. The mean initial FA score was 14.88. FA decreased significantly among all respondents over the 4-year study period (β = −0.20, p<0.001). Older adults had the various initial status of FA (β = 13.45, p<0.001) and experienced no significant difference in the change rates of FA (β = 0.26, p = 0.447).
Table 3.
Two separate unconditional latent growth curve modelling.
| LGCM for Intrinsic Capacity |
LGCM for Functional Ability |
|||||
|---|---|---|---|---|---|---|
| Estimate | S.E. | p | Estimate | S.E. | p | |
| Means | ||||||
| Intercept | 0.001 | 0.01 | 0.902 | 14.88 | 0.09 | <0.001 |
| Slope | −0.02 | 0.01 | <0.001 | −0.20 | 0.04 | <0.001 |
| Variances | ||||||
| Intercept | 0.18 | 0.01 | <0.001 | 13.45 | 0.75 | <0.001 |
| Slope | 0.04 | 0.00 | <0.001 | 0.26 | 0.34 | 0.447 |
| Covariance | ||||||
| Intercept-Slope | −0.04 | 0.01 | <0.001 | 0.57 | 0.43 | 0.181 |
| χ2 | 1.22 | <0.001 | 0.76 | >0.05 | ||
| RMSEA | 0.010 | 0.000 | ||||
| CFI | 1.000 | 1.000 | ||||
| TLI | 1.000 | 1.000 | ||||
| SRMR | 0.006 | 0.005 | ||||
Notes: Estimate = unstandardized coefficient; S.E. = standard error; RMSEA: Root-mean-square error of approximation; CFI = Comparative fit index; TLI = Tucker-Lewis Index; SRMR: Standardized root-mean-square residual.
We conducted a parallel process of latent growth curve modelling to estimate the longitudinal associations between IC and FA over time, controlling five time-invariant covariates: age, sex, education, marital status, and the number of chronic diseases. The models fit the data well. As shown in Fig. 1, at baseline a higher IC was associated with higher FA (β = 8.42, p<0.001) and less decline in FA over time (β = 0.49, p<0.05). Declines in IC scores were related to the faster decrease in FA over time (β = 10.16, p<0.001). The coefficients of covariates on the intercepts and slopes of IC/FA are presented in Fig. 1. The negative coefficient of predictors coupled with a negative slope indicates that higher values on covariates are related to steeper decline or more decline over time. Age was associated with lower IC scores (β = −0.02, p<0.001) and FA (β = −0.05, p<0.001) at baseline, more decline in IC scores over time (β = −0.002, p<0.01), but not significantly related to the change rate of FA (β = −0.002, p>0.05). Women had lower IC scores than men (β = −0.18, p<0.001), but there was no sex difference in FA at baseline, or in change rates of IC scores or FA over time. At baseline, individuals with more education had higher IC scores (β = 0.03, p<0.01), but lower FA than less educated individuals (β = −0.21, p<0.05). Older adults with more chronic diseases had lower IC scores (β = −1.12, p<0.001), but higher FA (β = 0.48, p<0.001) at baseline, and less decline in IC scores over time (β = 0.02, p<0.01).
Based on the results shown in Fig. 1, the intercept and slope of FA were further regressed on neighbourhood physical environment within 500- and 200-meter buffers, respectively. The models fit the data well. As Table 4 indicates, the percentage of green space within a 200-meter buffer was only significantly associated with less decline in FA over time (β = 1.15, p = 0.023), although this pattern was not found in a 500-meter buffer. No significant associations between land use diversity and the intercept and slope of FA were found. The number of commercial facilities within a 500-meter buffer was only significantly related to a faster decline in FA over time (β = −0.04, p = 0.004); the number of community centres within a 500-meter buffer was only significantly associated with lower FA at baseline (β = −0.18, p = 0.036); the number of leisure (β = 0.03, p = 0.043) and public transport facilities (β = 0.08, p = 0.003) within a 500-meter buffer were both significantly related to attenuated decline rate of FA over time. The number of healthcare facilities within both buffers was significantly associated with high FA at baseline (500-meter buffer: β = 0.17, p = 0.021; 200-meter buffer: β = 0.15, p = 0.008). Overall, neighbourhood physical environment within a 500-meter buffer showed stronger associations with FA both at baseline and over time than within a 200-meter buffer.
Table 4.
Longitudinal associations between intrinsic capacities (IC), neighbourhood physical environments and functional ability (FA) of older adults: Latent growth curve models.
| Model 1 (within a 200-meter buffer area) |
Model 2 (within a 500-meter buffer area) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intercept of FA |
Slope of FA |
Intercept of FA |
Slope of FA |
|||||||||
| β | 95% CI | p | β | 95% CI | p | β | 95% CI | p | β | 95% CI | p | |
| Variables | ||||||||||||
| Intercept of IC | 8.33 | (7.82, 8.84) | <0.001 | 0.29 | (0.03, 0.56) | 0.072 | 8.31 | (7.80, 8.81) | <0.001 | 0.33 | (0.06, 0.59) | 0.042 |
| Slope of IC | 9.08 | (7.21, 10.96) | <0.001 | 8.91 | (7.08, 10.75) | <0.001 | ||||||
| EN | ||||||||||||
| Green Space% | −0.31 | (−1.75, 1.12) | 0.720 | 1.15 | (0.32, 1.99) | 0.023 | 0.74 | (−0.25, 1.74) | 0.218 | −0.39 | (−0.95, 0.18) | 0.259 |
| Land use mix | −0.30 | (−1.07, 0.47) | 0.515 | −0.08 | (−0.53, 0.36) | 0.765 | −1.02 | (−2.84, 0.81) | 0.360 | −0.42 | (−1.47, 0.62) | 0.508 |
| # of commercial facilities | −0.12 | (−0.23, −0.01) | 0.072 | 0.04 | (−0.02, 0.11) | 0.272 | 0.001 | (−0.04, 0.03) | 0.872 | −0.04 | (−0.06, −0.02) | 0.004 |
| # of community centres | −0.01 | (−0.19, 0.17) | 0.938 | 0.01 | (−0.09, 0.12) | 0.843 | −0.18 | (−0.32, −0.04) | 0.036 | 0.01 | (−0.08, 0.09) | 0.910 |
| # of leisure facilities | −0.01 | (−0.09, 0.07) | 0.804 | 0.00 | (−0.05, 0.05) | 0.999 | 0.01 | (−0.04, 0.06) | 0.677 | 0.03 | (0.01, 0.06) | 0.043 |
| # of public transport facilities | −0.08 | (−0.28, 0.12) | 0.515 | 0.01 | (−0.11, 0.13) | 0.924 | −0.01 | (−0.09, 0.07) | 0.891 | 0.08 | (0.04, 0.13) | 0.003 |
| # of health care facilities | 0.17 | (0.05, 0.29) | 0.021 | −0.07 | (−0.14, 0) | 0.092 | 0.15 | (0.06, 0.25) | 0.008 | −0.02 | (−0.08, 0.04) | 0.547 |
| Mean of intercept | 19.26 | (17.77, 20.74) | <0.001 | 19.47 | (17.32, 21.63) | <0.001 | ||||||
| Mean of slope | −0.14 | (−0.49, 0.22) | 0.520 | 0.37 | (−0.57, 1.32) | 0.517 | ||||||
| Residual of intercept | 3.97 | (3.16, 4.79) | <0.001 | 3.93 | (3.12, 4.74) | <0.001 | ||||||
| Residual of slope | −0.43 | (−0.89, 0.02) | 0.118 | −0.44 | (−0.89, 0.01) | 0.107 | ||||||
| N | 2,078 | 2,078 | ||||||||||
| Chi-Square (df) | 311.165 (51) | <0.001 | 360.049 (51) | <0.001 | ||||||||
| RMSEA | 0.050 | 0.054 | ||||||||||
| CFI | 0.960 | 0.953 | ||||||||||
| TLI | 0.937 | 0.926 | ||||||||||
| SRMR | 0.025 | 0.027 | ||||||||||
Notes: β = unstandardized coefficient; CI = Confident Intervals; # = number; RMSEA = Root-mean-square error of approximation; CFI = Comparative fit index; TLI = Tucker-Lewis Index; SRMR = Standardized root-mean-square residual.
4. Discussion
To our knowledge, this is the first study to investigate how changes of IC over time and neighbourhood physical environment influence the trajectories of older adults’ FA, and thus provide longitudinal empirical evidence for the WHO Healthy Ageing framework.
We found that the trajectory of IC was heterogeneous among older adults, providing an opportunity to identify vulnerable older adults over time. Beard and colleagues found that lower IC scores were significantly associated with increasing age, female sex, low education, and chronic diseases [7]. Ma et al. found that age, low education, unmarried status and low income, less exercise were independently associated with a decline in any of the five domains of IC among older adults [45]. Similarly, we identified that being older, female and less educated, and having more chronic diseases were associated with lower IC at baseline. However, our study goes beyond Ma et al. [45] and advances the literature by identifying that IC as a whole decreased over time, and its trajectory varied among individuals; older individuals experienced faster IC decline than their younger counterparts, and older adults with more chronic diseases had lower IC at baseline, but also less decline in IC over time. This is either because they are already at a low level of IC, the possibility for further IC decline is limited, or that older adults suffering from chronic diseases utilise more healthcare resources to maintain their health status. Overall, our findings related to IC decline can inform policymakers of the importance of early detection and prevention of IC decline among older adults.
Using a theoretical-based score of IC, we further found that a higher initial IC status was associated with higher FA at baseline and predicted less decline in FA over time after controlling for covariates. We also found that a faster decrease in IC led to a faster decrease in FA over time. We extend existing research, most of which utilised information from each individual IC domain to establish associations with FA [31]. For example, previous research found that most of the five IC domains were separately associated with 3-year mortality and falls among nursing home residents, but when adding all the domains into the same model, only locomotion and vitality predicted death and falls among nursing home residents [6]. In other words, each domain closely interacts with each other, and without an appropriate statistical approach, important information on the holistic impact of IC on FA trajectories may be omitted. As the concept of IC and its operationalisation remain in their infancy, our study can provide a groundwork for future studies to investigate the impact of IC trajectory on FA from the life course perspective and how accumulative loss in IC leads to adverse health outcomes during catastrophic events such as COVID-19.
We provide the first evidence that neighbourhood physical environment was associated with FA trajectories in later life, lending support to the ecological model of ageing. We found that green space within a 200-meter buffer was significantly associated with less decline in FA over time, although no association was found at baseline, in contrast to the findings from previous cross-sectional studies [16,17]. Our results refine that the protective effects of neighbourhood green space against the decline of FA only exist in geographic proximity [15]. Previous research found that neighbourhood greenery is associated with increased walking and total walking time and protects against a decline in physical activities in later life [46,47]. Therefore, it is possible that neighbourhood green space may encourage physical activities and leisure walking, thus helping slow the decline of FA over time. Future studies can further examine the longitudinal mediating effects of walking behaviour on the relationship between green space and FA.
We found that the number of commercial, leisure and public transportation facilities were associated with FA trajectories. The number of commercial facilities within a 500-meter buffer was significantly related to a faster decline in FA over time, while no significant association was found within a 200-meter buffer. Our findings conflict with previous research reporting the protective effects of more commercial facilities in neighbourhoods on lower odds of functional limitation [14].
Perhaps a single location for groceries and shopping malls may be enough to cater for older residents’ daily needs. More commercial facilities, however, may generate additional traffic and noise, discouraging older adults from performing activities of daily living in the long run as previous research has pointed out that long-term exposure to noise, especially traffic/transportation noise, may cause dissatisfaction, exhaustion and older people’s withdrawal from daily activities [48]. As the variation in the number of commercial facilities within a 200-meter buffer was small, a similar effect to that found in a 500-meter buffer may not be detected in a 200-meter buffer. The associations between commercial facilities and FA trajectories require further study.
The number of leisure and public transportation facilities within a 500-meter buffer was significantly associated with less FA decline over time, although there were no effects on FA at baseline. Prior literature has found that the presence of public transportation facilitates social, leisure, and work role activities, and instrumental activities of daily living [17], and the availability of neighbourhood facilities facilitates older adults to social activities [49]. As such, more leisure and public transport facilities may help older adults better maintain an active lifestyle, such as undertaking more leisure, physical and social activities and travelling, further improving their health and FA. The significant effects of service facilities on the change and initial status of FA were found more within a 500-meter buffer, indicating that a 500-meter buffer may better capture older adults’ daily activity space.
The number of community centres within a 500-meter buffer was only significantly associated with lower FA at baseline, but no association was found with change in FA. In Hong Kong, the government began to promote the concept of “ageing-in-place” with implementation of the Ten-year Housing Program (1997–2006) to satisfy residents’ life cycle requirements [50]. Planning for building community centres in public housing developments may consider ageing population trends and the potential need for social activities [13]. Thus, community centres may be well-placed to cater for population ageing [51]. As we did not investigate the patterns of older adults’ usage of community centres, the underlying mechanism of community centres’ impact on the trajectory of FA requires further investigation.
We found that the number of healthcare facilities within both buffer areas was significantly associated with high FA at baseline. The availability of healthcare facilities is potentially associated with higher preventive healthcare utilisation and chronic disease management among older adults. Previous research suggests that adequate access to medical services significantly improves older adults’ physical functioning [52].
Our study has several strengths. It is the first to estimate IC trajectories over time among older adults using the WHO’s multi-domain concept and factor scores to represent the underlying latent trait of interest. Hence, our use of a theoretical-based score in all analyses to test the unique contribution of changes of IC in maintaining FA over time advanced existing research, which had only captured the impact of a single domain of IC. Our study is the first to reveal how neighbourhood physical environment is associated with the decline or the maintenance of FA among older adults, advancing existing literature that only focused on the onset of functional limitations. Thus, we provided empirical evidence of the WHO Healthy Ageing approach and can inform health policy planning. Finally, we used the parallel processes of latent growth curve modelling incorporating longitudinal data to avoid the methodological problems associated with cross-sectional data.
However, our study also has some limitations. First, our findings were based on older adults with low socioeconomic status living in public rental housing, so are not generalisable to other populations or to other developed cities with different modes of public housing. Future research should use a national population sample to validate our findings. Second, we focused on IADL to measure FA, ignoring other components of FA, such as social relationship building [3]. Therefore, our results may only apply to the ability of older adults to live independently in the community. Future studies should use multiple measurements to capture the comprehensive picture of FA among older adults. Third, we had longitudinal data for four years only, which are insufficient to capture the complexity of FA trajectories. Future studies should expand the observation time-frame and apply the life course perspective to examine the longitudinal relationship between neighbourhood physical environment and FA. Fourth, we did not have information on indoor or outdoor accessibility of the apartments and buildings in which residents lived, confounding the relationship between neighbourhood physical environment and FA found in our study. It would be difficult for residents to access the neighbourhood environment and destinations if their apartments or buildings had low indoor or outdoor accessibility [53]. Future studies should consider indoor and outdoor accessibility to provide enhanced scientific evidence.
In the Decade of Healthy Ageing, the maintenance of FA should be the top priority in the public health policy agenda. Our study highlights the importance of developing strategies to maintain IC among older adults. In addition, our study provides directions for developing WHO age-friendly city initiatives in the domains of outdoor space and buildings, transportation, community support and health services. It is imperative to create a supportive neighbourhood environment for older adults by increasing residential green space and the availability of leisure and public transport facilities in the community.
Contributors
Shiyu Lu contributed to the conceptualisation, writing - orginal draft and writing - review & editing. Yuqi Liu and Yingqi Guo contributed to the validation and writing - review & editing. Hung Chak Ho, Yimeng Song, Wei Cheng and On Fung Chan contributed to data curation and writing - review & editing. Cheryl Hiu Kwan Chui, Chris Webster and Rebecca Lai Har Chiu contributed to the supervision and writing – review & editing. Terry Yat Sang Lum contributed to the conceptualisation, funding acquisition, resources, supervision and writing – review and editing.
Data sharing statement
No additional unpublished data to share.
Funding
The Hong Kong Housing Society.
Declaration of Competing Interest
The Authors were supported by the Hong Kong Housing Society to conduct the longitudinal survey. They have no other conflicts to declare.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.eclinm.2021.100927.
Appendix. Supplementary materials
References
- 1.Lee J., Lau S., Meijer E., Hu P. Living longer, with or without disability? A global and longitudinal perspective. J Gerontol A Biol Sci Med Sci. 2019;75(1):162–167. doi: 10.1093/gerona/glz007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beard J.R., Officer A., de Carvalho I.A., Sadana R., Pot A.M., Michel J.-.P. The World report on ageing and health: a policy framework for healthy ageing. Lancet. 2016;387(10033):2145–2154. doi: 10.1016/S0140-6736(15)00516-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization . World Health Organization; Geneva: 2015. World report on ageing and heath. [Google Scholar]
- 4.Daskalopoulou C., Koukounari A., Wu Y.T., Terrera G.M., Caballero F.F., de la Fuente J. Healthy ageing trajectories and lifestyle behaviour: the Mexican Health and Aging Study. Sci Rep-Uk. 2019;9 doi: 10.1038/s41598-019-47238-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gill T.M., Gahbauer E.A., Han L., Allore H.G. Trajectories of disability in the last year of life. N Engl J Med. 2010;362(13):1173–1180. doi: 10.1056/NEJMoa0909087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Charles A., Buckinx F., Locquet M., Reginster J.-.Y., Petermans J., Gruslin B. Prediction of adverse outcomes in nursing home residents according to intrinsic capacity proposed by the World Health Organization. J Gerontol A Psychol Sci Soc Sci. 2019;75(8):1594–1599. doi: 10.1093/gerona/glz218. [DOI] [PubMed] [Google Scholar]
- 7.Beard J.R., Jotheeswaran A.T., Cesari M., Araujo de Carvalho I. The structure and predictive value of intrinsic capacity in a longitudinal study of ageing. BMJ Open. 2019;9(11) doi: 10.1136/bmjopen-2018-026119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wahl H.-.W., Iwarsson S., Oswald F. Aging well and the environment: toward an integrative model and research agenda for the future. Gerontologist. 2012;52(3):306–316. doi: 10.1093/geront/gnr154. [DOI] [PubMed] [Google Scholar]
- 9.Lawton M.P., Nahemow L. American Psychological Association; Washington, DC, US: 1973. Ecology and the aging process. The psychology of adult development and aging; pp. 619–674. [Google Scholar]
- 10.Ewing R., Tian G., Goates J.P., Zhang M., Greenwald M.J., Joyce A. Varying influences of the built environment on household travel in 15 diverse regions of the United States. Urban Stud. 2015;52(13):2330–2348. [Google Scholar]
- 11.Zhang L., Ye Y., Zeng W.X., Chiaradia A. A systematic measurement of street quality through multi-sourced urban data: a human-oriented analysis. Int J Env Res Pub He. 2019;16(10):1782. doi: 10.3390/ijerph16101782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Noordzij J.M., Beenackers M.A., Groeniger J.O., Timmermans E.J., Motoc I., Huisman M. Land use mix and physical activity in middle-aged and older adults: a longitudinal study examining changes in land use mix in two Dutch cohorts. Int J Behav Nutr Phy. 2021;18(1) doi: 10.1186/s12966-021-01083-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lu S., Liu Y., Guo Y., Ho H.C., Song Y., Cheng W. Neighborhood built environment and late-life depression: a multilevel path analysis in a Chinese society. J Gerontol B Biol Sci Med Sci. 2021 doi: 10.1093/geronb/gbab037. [DOI] [PubMed] [Google Scholar]
- 14.Danielewicz A.L., d’Orsi E., Boing A.F. Association between built environment and the incidence of disability in basic and instrumental activities of daily living in the older adults: results of a cohort study in southern Brazil. Prev Med. 2018;115:119–125. doi: 10.1016/j.ypmed.2018.08.016. [DOI] [PubMed] [Google Scholar]
- 15.Zhu A., Yan L.L., Wu C.-.D., James P., Zeng Y., Ji J.S. Residential greenness, activities of daily living, and instrumental activities of daily living: a longitudinal cohort study of older adults in China. Environ Epidemiol. 2019;3(5):e065. doi: 10.1097/EE9.0000000000000065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vogt S., Mielck A., Berger U., Grill E., Peters A., Doring A. Neighborhood and healthy aging in a German city: distances to green space and senior service centers and their associations with physical constitution, disability, and health-related quality of life. Eur J Ageing. 2015;12(4):273–283. doi: 10.1007/s10433-015-0345-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.White D.K., Jette A.M., Felson D.T., Lavalley M.P., Lewis C.E., Torner J.C. Are features of the neighborhood environment associated with disability in older adults? Disabil Rehabil. 2010;32(8):639–645. doi: 10.3109/09638280903254547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fogal A.S., Pessoa M.C., Fernandes E.I., Ribeiro A.Q. Built urban environment and functional incapacity: enabling healthy aging. J Transp Health. 2019;14 [Google Scholar]
- 19.Brenner A.B., Clarke P.J. Difficulty and independence in shopping among older Americans: more than just leaving the house. Disabil Rehabil. 2019;41(2):191–200. doi: 10.1080/09638288.2017.1398785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Song S.Q., Yap W., Hou Y.T., Yuen B. Neighbourhood built environment, physical activity, and physical health among older adults in Singapore: a simultaneous equations approach. J Transp Health. 2020;18 [Google Scholar]
- 21.Lai P.C., Chen S., Low C.T., Cerin E., Stimson R., Wong P.Y.P. Neighborhood variation of sustainable urban morphological characteristics. Int J Environ Res Public Health. 2018;15(3):465. doi: 10.3390/ijerph15030465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.HK Census and Statistic Department . HK Census and Statistic Department; Hong Kong: 2016. Hong kong 2016 population by-census - Thematic Report: older persons. [Google Scholar]
- 23.HK SAR Government . HK Census and Statistic Department; Hong Kong: 2019. Hong kong poverty situation report 2019. [Google Scholar]
- 24.Lum T.Y.S., Lou V.W.Q., Chen Y.Y., Wong G.H.Y., Luo H., Tong T.L.W. Neighborhood support and aging-in-place preference among low-income elderly Chinese city-dwellers. J Gerontol B. 2016;71(1):98–105. doi: 10.1093/geronb/gbu154. [DOI] [PubMed] [Google Scholar]
- 25.Tao S., He S.Y., Kwan M.-.P., Luo S. Does low income translate into lower mobility? An investigation of activity space in Hong Kong between 2002 and 2011. J Transp Geogr. 2020;82 [Google Scholar]
- 26.Tong A.Y.C., Man D.W.K. The validation of the Hong Kong Chinese version of the Lawton Instrumental Activities of Daily Living scale for institutionalized elderly persons. OTJR. 2002;22(4):132–142. [Google Scholar]
- 27.Chu L.W., Ng K.H., Law A.C., Lee A.M., Kwan F. Validity of the cantonese chinese montreal cognitive assessment in Southern Chinese. Geriatr Gerontol Int. 2015;15(1):96–103. doi: 10.1111/ggi.12237. [DOI] [PubMed] [Google Scholar]
- 28.Nasreddine Z.S., Phillips N.A., Bédirian V., Charbonneau S., Whitehead V., Collin I. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–699. doi: 10.1111/j.1532-5415.2005.53221.x. [DOI] [PubMed] [Google Scholar]
- 29.Wong M.T.P., Ho T.P., Ho M.Y., Yu C.S., Wong Y.H., Lee S.Y. Development and inter-rater reliability of a standardized verbal instruction manual for the Chinese Geriatric Depression Scale - Short Form. Int J Geriatr Psych. 2002;17(5):459–463. doi: 10.1002/gps.633. [DOI] [PubMed] [Google Scholar]
- 30.Morley J.E., Malmstrom T.K., Miller D.K. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging. 2012;16(7):601–608. doi: 10.1007/s12603-012-0084-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.George P.P., Lun P., Ong S.P., Lim W.S. A rapid review of the measurement of intrinsic capacity in older adults. J Nutr Health Aging. 2021 doi: 10.1007/s12603-021-1622-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim M., Shinkai S. Prevalence of muscle weakness based on different diagnostic criteria in community-dwelling older adults: a comparison of grip strength dynamometers. Geriatr Gerontol Int. 2017;17(11):2089–2095. doi: 10.1111/ggi.13027. [DOI] [PubMed] [Google Scholar]
- 33.Cyarto E.V., Dow B., Vrantsidis F., Meyer C. Promoting healthy ageing: development of the Healthy Ageing Quiz. Australas J Ageing. 2013;32(1):15–20. doi: 10.1111/j.1741-6612.2011.00585.x. [DOI] [PubMed] [Google Scholar]
- 34.Sun G.B., Webster C., Ni M.Y., Zhang X.H. Measuring high-density built environment for public health research: uncertainty with respect to data, indicator design and spatial scale. Geospat Health. 2018;13(1):35–47. doi: 10.4081/gh.2018.653. [DOI] [PubMed] [Google Scholar]
- 35.Burton E., Mitchell L. Elsevier; Oxford: 2006. Inclusive urban design—streets for life. [Google Scholar]
- 36.Tsai Y.H., Stow D., Chen H.L., Lewison R., An L., Shi L. Mapping vegetation and land use types in Fanjingshan National Nature Reserve using Google Earth Engine. Remote Sens. 2018;10(6):927. [Google Scholar]
- 37.Song Y., Merlin L., Rodriguez D. Comparing measures of urban land use mix. Comput Environ Urban. 2013;42:1–13. [Google Scholar]
- 38.Allen M. Factor analysis: confirmatory. In: Allen M., editor. The sage encyclopedia of communication research methods. Sage Publications, Inc; Thousand Oaks, CA: 2017. [Google Scholar]
- 39.Watkins M.W. The reliability of multidimensional neuropsychological measures: from alpha to omega. Clin Neuropsychol. 2017;31(6–7):1113–1126. doi: 10.1080/13854046.2017.1317364. [DOI] [PubMed] [Google Scholar]
- 40.Knafl G.J., Grey M. Factor analysis model evaluation through likelihood cross-validation. Stat Methods Med Res. 2007;16(2):77–102. doi: 10.1177/0962280206070649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bollen K.A., Curran P.J. John Wiley & Sons; NJ: 2006. Latent curve models: a structural equation perspective. [Google Scholar]
- 42.Howard A.L., Curran P.J. Latent growth curve modeling. In: Michalos AC, editor. Encyclopedia of quality of life and well-being research. Springer Netherlands; Dordrecht: 2014. pp. 3515–3517. [Google Scholar]
- 43.Li C. Little's test of missing completely at random. Stata J. 2013;13(4):795–809. [Google Scholar]
- 44.Hu Ll-T, Bentler P.M. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6(1):1–55. [Google Scholar]
- 45.Ma L., Chhetri J.K., Zhang L., Sun F., Li Y., Tang Z. Cross-sectional study examining the status of intrinsic capacity decline in community-dwelling older adults in China: prevalence, associated factors and implications for clinical care. BMJ Open. 2021;11(1) doi: 10.1136/bmjopen-2020-043062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dalton A.M., Wareham N., Griffin S., Jones A.P. Neighbourhood greenspace is associated with a slower decline in physical activity in older adults: a prospective cohort study. SSM Popul Health. 2016;2:683–691. doi: 10.1016/j.ssmph.2016.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lu Y., Sarkar C., Xiao Y. The effect of street-level greenery on walking behavior: evidence from Hong Kong. Soc Sci Med. 2018;208:41–49. doi: 10.1016/j.socscimed.2018.05.022. [DOI] [PubMed] [Google Scholar]
- 48.Foraster M., Eze I.C., Vienneau D., Brink M., Cajochen C., Caviezel S. Long-term transportation noise annoyance is associated with subsequent lower levels of physical activity. Environ Int. 2016;91:341–349. doi: 10.1016/j.envint.2016.03.011. [DOI] [PubMed] [Google Scholar]
- 49.Levasseur M., Gauvin L., Richard L., Kestens Y., Daniel M., Payette H. Associations between perceived proximity to neighborhood resources, disability, and social participation among community-dwelling older adults: results from the VoisiNuAge study. Arch Phys Med Rehab. 2011;92(12):1979–1986. doi: 10.1016/j.apmr.2011.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Deng Y., Chan E.H.W., Poon S.W. Challenge-driven design for public housing: the case of Hong Kong. Front Archit Res. 2016;5(2):213–224. [Google Scholar]
- 51.Wadu Mesthrige J., Cheung S.L. Critical evaluation of ‘ageing in place’ in redeveloped public rental housing estates in Hong Kong. Ageing Soc. 2020;40(9):2006–2039. [Google Scholar]
- 52.Zhang X.F., Dupre M.E., Qiu L., Zhou W., Zhao Y., Gu D.N. Urban-rural differences in the association between access to healthcare and health outcomes among older adults in China. BMC Geriatr. 2017;17(1):151. doi: 10.1186/s12877-017-0538-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rantakokko M., Iwarsson S., Portegijs E., Viljanen A., Rantanen T. Associations between environmental characteristics and life-space mobility in community-dwelling older people. J Aging Health. 2015;27(4):606–621. doi: 10.1177/0898264314555328. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.