Abstract
Background
The impact of coronavirus disease 2019 on healthcare has led to rapid changes in otolaryngology service provisions. As such, new standard operating procedures for the management of suspected tonsillitis or quinsy were implemented in our centre.
Methods
A retrospective audit was performed of acute referrals to ENT of patients with suspected tonsillitis, peritonsillar cellulitis or quinsy, during the 10 weeks before (group 1) and 10 weeks after (group 2) implementation of the new standard operating procedures.
Results
Group 2 received fewer referrals. Fewer nasendoscopies were performed and corticosteroid use was reduced. The frequency of quinsy drainage performed under local anaesthetic increased, although the difference was not statistically significant. Hospital admission rates decreased from 56.1 to 20.4 per cent, and mean length of stay increased from 1.13 to 1.5 days. Face-to-face follow up decreased from 15.0 to 8.2 per cent, whilst virtual follow up increased from 4.7 to 16.3 per cent. There were no significant differences in re-presentation or re-admission rates.
Conclusion
Management of suspected tonsillitis or quinsy using the new standard operating procedures appears to be safe and effective. This management should now be applied to an out-patient setting in otherwise systemically well patients.
Keywords: Tonsillitis, Peritonsillar Abscess, Coronavirus, Pandemics, Otolaryngology, Quality Improvement
Introduction
The impact of coronavirus disease 2019 (Covid-19) on healthcare provisions has been substantial.1 Otolaryngology services have needed to adapt to new pressures and risks, affecting both patients and staff alike, given the high risk of exposure and infection from aerosol and droplet contamination when performing examinations or procedures in the head and neck.2,3 Features of this response have included: rapid adoption of telemedicine, increased patient triage, surgical prioritisation, altered clinical area patient flow, flexible workforce planning and training, provision of wellbeing services, and enhanced personal protective equipment (PPE).4,5
In our department, clinical practice during the first wave of the pandemic was limited to urgent or emergency care. This included referrals from the emergency department with acute sore throat, tonsillitis or peritonsillar abscess (quinsy). Throat examination, flexible nasendoscopy and quinsy drainage were considered high-risk procedures for aerosol and droplet generation.
Traditionally, peritonsillar abscesses are managed on an in-patient basis, with intravenous antibiotics, corticosteroids, and drainage by needle aspiration, or incision and drainage.6–9 Although steroid use in patients with this condition is common and is thought to relieve symptoms by its anti-inflammatory effects,10–13 widespread steroid use was considered unsafe in the context of the pandemic.14 Furthermore, any avoidable in-patient admission to hospital was strongly discouraged, to preserve hospital resources for the increasing numbers of Covid-19 admissions and to reduce the risk of coronavirus transmission to non-Covid-19 patients.15,16
In order to mitigate such risks, new standard operating procedures for the management of ENT emergencies were implemented in our centre, in accordance with new guidance issued by ENT UK, the national body representing otolaryngology and its related specialties in the UK.17 The local standard operating procedures for patients referred with suspected tonsillitis or quinsy are shown in Appendix 1. Importantly, recommendations included: managing patients in a short stay or out-patient clinic setting, avoiding steroid use in high-risk groups, attempting drainage under local anaesthetic, and discharging patients promptly when they are able to safely swallow.
Given the rapid implementation of changes to the provision of emergency ENT care, we undertook a service evaluation to ensure the ongoing safety and effectiveness of the emergency management of patients during the Covid-19 pandemic. We aimed to compare the outcomes of care provided to patients with acute sore throat, tonsillitis or peritonsillar abscess before and after implementation of the updated ENT emergency standard operating procedures during the Covid-19 pandemic, and guide any further updates to the standard operating procedures.
Materials and methods
A retrospective audit was performed of all acute referrals from the emergency department of a busy London teaching hospital to the ENT department, during the 10 weeks immediately before and 10 weeks immediately after the implementation of new standard operating procedures. The new ENT emergency standard operating procedures came into effect on 16 March 2020. As such, the data collection period for group 1 (pre-implementation of the new standard operating procedures) was from 1 January 2020 to 15 March 2020, and the data collection period for group 2 (post-implementation of the new standard operating procedures) ran from 16 March 2020 to 31 May 2020. Referrals included in this study related only to acute sore throat, suspected tonsillitis, peritonsillar cellulitis or quinsy. The study excluded cases managed by the emergency department with no referral to or input from ENT. A total of 156 cases were included.
The data collected for each case included patient demographics, specific treatment measures and relevant outcome measures. Statistical analyses using the chi-square test were performed to compare groups 1 and 2 (p < 0.05).
Results
There was a decrease in the total number of referrals, with an increase in the percentage of quinsy referrals (Table 1). No significant difference was found in terms of the gender and mean age of patients referred.
Table 1.
Demographic data
| Parameter | Group 1* | Group 2† | P-value |
|---|---|---|---|
| Total referrals (n) | 107 | 49 | |
| Quinsy referrals (n (%)) | 48 (44.9) | 30 (61.2) | 0.042‡ |
| Gender (n (%)) | |||
| – Male | 58 (54.2) | 30 (61.2) | 0.412 |
| – Female | 49 (45.8) | 19 (38.8) | 0.412 |
| Age (mean (range); years) | 31 (17–86) | 35 (17–79) | 0.117 |
*Pre- and †post-implementation of new standard operating procedures. ‡Indicates statistical significance
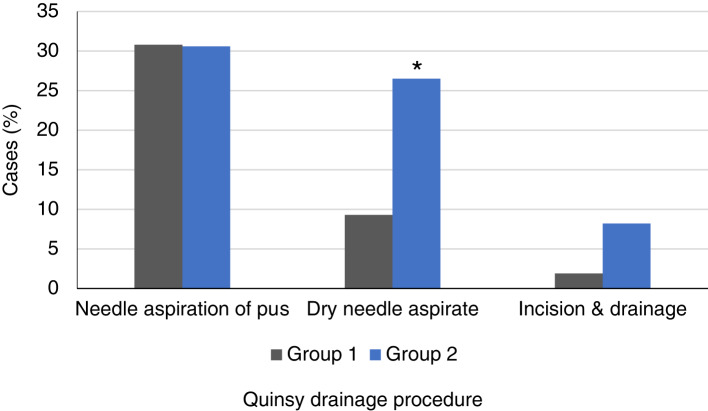
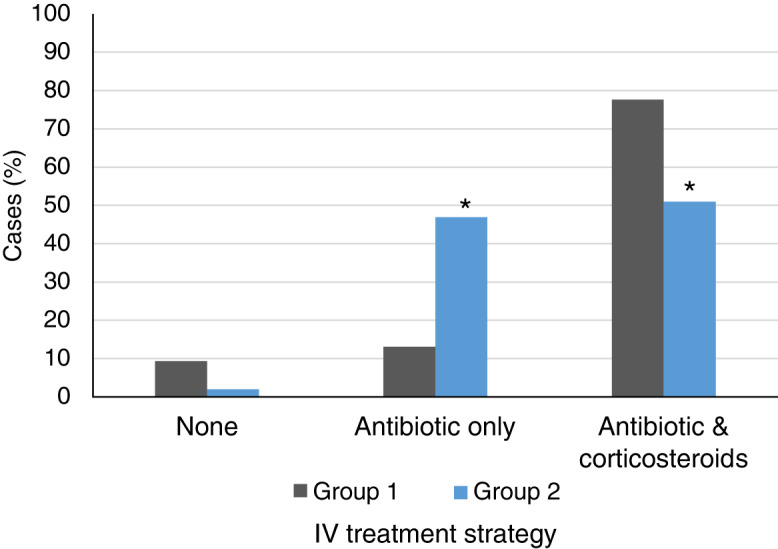
Treatment data showed no significant difference in time spent in the emergency department; however, significantly fewer nasendoscopies were performed and corticosteroid use was reduced (Table 2 and Figure 1). There was an apparent increase in the frequency of procedures performed under local anaesthetic for quinsy drainage (Table 2). Of those procedures, the percentage of successful needle aspiration of pus was unchanged, but there was a statistically significant increase in the percentage of dry aspirates. Use of incision and drainage increased, to a near statistically significant level (Figure 2).
Table 2.
Initial treatment measures
| Parameter | Group 1* | Group 2† | P-value |
|---|---|---|---|
| Time in emergency department (mean (range); minutes) | 293 (43–1557) | 276 (42–1468) | 0.576 |
| Examination (n (%)) | |||
| – Oronasal | 107 (100) | 49 (100) | – |
| – Nasendoscopy | 36 (33.6) | 7 (14.3) | 0.012‡ |
| Intravenous therapy (n (%)) | |||
| – None | 10 (9.3) | 1 (2.0) | 0.098 |
| – Antibiotic only | 14 (13.1) | 23 (46.9) | <0.001‡ |
| – Antibiotics & corticosteroids | 83 (77.6) | 25 (51.0) | 0.001‡ |
| Drainage (n (%)) | |||
| – None attempted | 62 (57.9) | 17 (34.7) | 0.007 |
| – Needle aspiration of pus | 33 (30.8) | 15 (30.6) | 0.977 |
| – Dry needle aspirate | 10 (9.3) | 13 (26.5) | 0.005‡ |
| – Incision & drainage | 2 (1.9) | 4 (8.2) | 0.058 |
| Covid-19 swab on admission (n (%)) | 0 (0) | 11 (22.4) | – |
*Pre- and †post-implementation of new standard operating procedures. ‡Indicates statistical significance. Covid-19 = coronavirus disease 2019
Fig. 1.
Intravenous (IV) treatment strategies for groups 1 and 2 (pre- and post-implementation of new standard operating procedures, respectively) (*p < 0.05).
Fig. 2.
Procedures performed for quinsy drainage under local anaesthetic, for groups 1 and 2 (pre- and post-implementation of new standard operating procedures, respectively) (*p < 0.05).
Outcome data revealed a significant reduction in admission rates, from 56.1 per cent to 20.4 per cent (p < 0.0005) (Table 3). Of those patients admitted, the mean length of stay increased from 1.13 days to 1.5 days (p = 0.029). Face-to-face follow up decreased from 15.0 per cent to 8.2 per cent, in favour of increased virtual follow up from 4.7 per cent to 16.3 per cent (p = 0.031). Importantly, no significant differences were found in the rates of re-presentation or re-admission in the follow-up period.
Table 3.
Outcome data
| Parameter | Group 1* | Group 2† | P-value |
|---|---|---|---|
| Mortalities (n (%)) | 0 (0) | 0 (0) | – |
| Admissions (n (%)) | 60 (56.1) | 10 (20.4) | <0.001‡ |
| Length of hospital stay (mean (range); days) | 1.13 (1–3) | 1.5 (1–3) | 0.029‡ |
| Follow up (n (%)) | |||
| – None, as routine | 86 (80.4) | 37 (78.7) | 0.490 |
| – Virtual | 5 (4.7) | 8 (16.3) | 0.015 |
| – Face-to-face | 16 (15.0) | 4 (8.2) | 0.031‡ |
| Re-presentation (n (%)) | |||
| – None | 96 (89.7) | 42 (85.7) | 0.467 |
| – Before day 10 | 8 (7.5) | 6 (12.2) | 0.333 |
| – On or after day 10 | 3 (2.8) | 1 (2.0) | 0.588 |
| Positive Covid-19 status (n (%)) | 0 (0) | – |
*Pre- and †post-implementation of new standard operating procedures. ‡Indicates statistical significance. Covid-19 = coronavirus disease 2019
Discussion
The profound impact of the Covid-19 pandemic on healthcare services resulted in rapid and widespread changes to local ENT service provision, requiring continual evaluation to ensure safety and effectiveness. Our results suggest that the emergency management of suspected quinsy using the updated guidelines is associated with: fewer in-patient hospital admissions, fewer nasendoscopies, reduced corticosteroid use, increased frequency of aspiration or drainage under local anaesthetic, increased virtual follow-up appointments, and no increase in mortality or re-admission rates. Although the mean length of stay was longer for those patients requiring in-patient admission, this represents a significant cost saving overall, as the proportion of suspected quinsy referrals requiring in-patient admission are significantly reduced.
Any reduction in in-patient hospital admissions is of added importance during the pandemic. Avoidable admissions to hospital are thought to increase the risk of viral exposure to shielding patients and prematurely exhaust the hospital surge capacity.1,4 Anecdotally, patients’ priorities during the pandemic may have also changed to reflect this, with greater preference to avoid hospital admission where possible.
Patients still requiring admission were more likely to be more systemically unwell in group 2 (post-implementation of the new standard operating procedures), which may explain the increased mean length of hospital stay observed, although data on physiological parameters or laboratory indicators were not collected. Co-morbidity data are also omitted, and so important risk factors are not identified. Bird et al. list the following criteria for admission of tonsillitis cases: immunocompromise, diabetes and features of breathlessness, severe dehydration, or septic shock.18 Additional data are thus necessary in future, to develop predictors of re-admission and standardised criteria for admitting these patients to hospital.
However, the unchanged rates of re-admission and mortality that we observed suggest that the management of suspected acute sore throat, tonsillitis or peritonsillar abscess using the updated standard operating procedures is safe. Although complications experienced in the community may be missed in this study, it is likely that any significant problems would re-present to the hospital.
Otolaryngology services must adapt to mitigate the risks of coronavirus disease 2019
An altered approach to tonsillitis and quinsy care can safely limit aerosol generation, and prevent widespread steroid use and unnecessary hospital admissions
Important features of this approach include performing quinsy drainage and providing virtual follow up
This paper supports the out-patient management of peritonsillar abscess in selected cases
Interestingly, our data support the role of peritonsillar abscess drainage. We observed an increased frequency of aspiration or surgical drainage under local anaesthetic in group 2. Unsurprisingly, a greater proportion of these were ‘dry taps’, suggesting a greater willingness to attempt aspiration or drainage in any suspected case. However, although we did not perform further subgroup analysis of confirmed cases of quinsy, recent evidence indicates no significant difference in outcomes between medical management and surgical drainage of peritonsillar abscess.19 Similarly, conservative medical management is reported as an effective treatment for co-existent peritonsillar abscess and Covid-19.20
Given the relative contraindication of corticosteroids in those at higher risk of Covid-19, we recorded more cases of suspected quinsy in group 2 that were managed with antibiotics alone. Traditionally, this is an effective treatment for simple acute bacterial throat infections.21–23 Corticosteroids are conventionally used in more severe cases and in those with suspected peritonsillar abscess, primarily for symptomatic relief.11–13,24 The unwanted effects of corticosteroids on immunity, in the context of uncertain viral exposure in the community, were considered with caution early on in the pandemic.11,25,26 However, widespread use of steroids in these cases appears to have continued during the pandemic, as reported in the ‘Integrate’ (the UK ENT Research Trainee Network) Covid-19 ENT emergency care audit.27 Although the survival benefit of dexamethasone in Covid-19 has also been demonstrated, this relates to a different patient group, and there is no suggestion that corticosteroid use prior to coronavirus infection has any protective effects.28,29 Large prospective studies of adverse outcomes from corticosteroid use during the pandemic are needed to address this contentious topic.
Notably, coronavirus status screening and testing in our centre was low. Given that symptoms of throat infection often met the criteria for suspected coronavirus infection, a greater proportion of tests were expected. Indeed, coronavirus status screening is now a prerequisite for any patient requiring admission to hospital, and rates of coronavirus testing in suspected peritonsillar abscess cases were higher nationally.27
As throat examination, flexible nasendoscopy and quinsy drainage are all considered high-risk procedures for aerosol and droplet generation, full PPE is advised for the treating clinicians, regardless of the patient's coronavirus status.30,31 The Liverpool Peritonsillar Abscess Score has undergone modification to support the triage of suspected cases without oral examination, thereby limiting clinicians’ risk of exposure.32 However, adequate access and supply of appropriate PPE, as well as improved patient testing, must be ensured to protect both patients and staff, and to avoid compromising patient care.
The expedited uptake of telemedicine has increased the availability of virtual follow-up consultations for patients, and has allowed remote working for staff to deliver healthcare, whilst minimising non-essential travel. This highlights the need for continual optimisation and allocation of resources to deliver safe and cost-effective care.
Ultimately, our data support the evidence base for out-patient management of quinsy.8,33–35 The findings are comparable to those of the national Covid-19 ENT emergency care audit,27 where approximately 45–55 per cent of patients with suspected tonsillitis or quinsy were discharged without admission, and only 10 per cent re-presented to hospital, with 3–5 per cent subsequently re-admitted. Therefore, developing a sustainable out-patient treatment protocol for peritonsillar abscess is an important next step,36 with consideration of bacteriological studies to support local antimicrobial policies.37
Importantly, Covid-19 also impacted the workforce. In our centre, specialty registrars in ENT were required to act down as resident on-call, responding to emergency referrals directly, in place of junior colleagues who were temporarily redeployed to other hospital services. Although this exclusively affected our Covid-19 dataset, the implemented changes in quinsy care are protocol-driven, and rarely require senior-led technical skills or clinical decision-making. Therefore, effective induction processes are needed to allow optimal clinical skills acquisition and familiarity with updated treatment guidelines amongst all treating clinicians. Further evaluation will be needed when services and staffing return to the pre-coronavirus levels, to ensure the sustainability of these results.
Further research could include the use of patient-related outcome measures in out-patient quinsy care, and assessment of correlation with objective markers of disease severity, so as to establish predictors of re-presentation or re-admission.
Our constantly changing understanding of Covid-19, a new clinical entity, and its associated risks, will undoubtedly continue to affect ENT services and hence require continued service evaluation. By comparing outcomes following changes in practice during the first wave of the pandemic to those immediately prior to the pandemic, studies such as ours are limited in terms of sample size and widespread reproducibility; nevertheless, they provide important insights into local service provision and present suggestions for further improvement.
Conclusion
Assessment of the impact of Covid-19 on otolaryngology services provides a unique opportunity to improve clinical practice. Our evaluation indicates the continued provision of safe and effective quinsy care during the Covid-19 pandemic. The findings can inform further emergency management protocols amidst ongoing regional and global outbreaks. The changes to peritonsillar abscess management should now be applied to patients (who are otherwise systemically well) in an out-patient setting.
Acknowledgement
The authors would like to thank colleagues who encouraged this research.
Appendix 1. Local standard operating procedures for acute management of peritonsillar abscess during Covid-19
| Management of peritonsillar abscess* |
|---|
| ATLS/ALS care & specialist ENT assessment where possible |
| Manage patient in short stay or out-patient clinic setting |
| Attempt aspiration or I&D |
| IV access, fluid resuscitation |
| IV dexamethasone (risks should be discussed with patient) |
| IV penicillin & metronidazole |
| Analgesia such as paracetamol, ibuprofen, codeine (dissolvable if appropriate) |
| Reassess after 1–2 hours; discharge if able to swallow water, with oral antibiotics & analgesia |
| Safety netting advice |
| Emergency clinic telephone follow up |
*Adapted from ENT UK guidelines. Covid-19 = coronavirus disease 2019; ATLS = advanced trauma life support; ALS = advanced life support; I&D = incision and drainage; IV = intravenous
Competing interests
None declared
References
- 1.Moghadas SM, Shoukat A, Fitzpatrick MC, Wells CR, Sah P, Pandey A et al. Projecting hospital utilization during the COVID-19 outbreaks in the United States. Proc Natl Acad Sci U S A 2020;117:9122–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Givi B, Schiff BA, Chinn SB, Clayburgh D, Iyer NG, Jalisi S et al. Safety recommendations for evaluation and surgery of the head and neck during the COVID-19 pandemic. JAMA Otolaryngol Head Neck Surg 2020;146:579–84 [DOI] [PubMed] [Google Scholar]
- 3.Stephenson K, Sowerby LJ, Hopkins C, Kumar N. The UK national registry of ENT surgeons with coronavirus disease 2019. J Laryngol Otol 2020;134:665–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bann DV, Patel VA, Saadi R, Gniady JP, Goyal N, McGinn JD et al. Impact of coronavirus (COVID-19) on otolaryngologic surgery: brief commentary. Head Neck 2020;42:1227–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Unadkat SN, Andrews PJ, Bertossi D, D'Souza A, Joshi A, Shandilya M et al. Recovery of elective facial plastic surgery in the post-coronavirus disease 2019 era: recommendations from the European Academy of Facial Plastic Surgery Task Force. Facial Plast Surg Aesthet Med 2020;22:233–7 [DOI] [PubMed] [Google Scholar]
- 6.Mehanna HM, Al-Bahnasawi L, White A. National audit of the management of peritonsillar abscess. Postgrad Med J 2002;78:545–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.ENT Trainee Research Collaborative – West Midlands. National prospective cohort study of peritonsillar abscess management and outcomes: the Multicentre Audit of Quinsies study. J Laryngol Otol 2016;130:768–76 [DOI] [PubMed] [Google Scholar]
- 8.Al Yaghchi C, Cruise A, Kapoor K, Singh A, Harcourt J. Out-patient management of patients with a peritonsillar abscess. Clin Otolaryngol 2008;33:52–5 [DOI] [PubMed] [Google Scholar]
- 9.National Institute for Health and Care Excellence. Sore throat (acute): antimicrobial prescribing: NICE guideline [NG84] In: https://www.nice.org.uk/guidance/ng84/chapter/Recommendations [13 April 2021]
- 10.Ozbek C, Aygenc E, Tuna EU, Selcuk A, Ozdem C. Use of steroids in the treatment of peritonsillar abscess. J Laryngol Otol 2004;118:439–42 [DOI] [PubMed] [Google Scholar]
- 11.Chau JKM, Seikaly HR, Harris JR, Villa-Roel C, Brick C, Rowe BH. Corticosteroids in peritonsillar abscess treatment: a blinded placebo-controlled clinical trial. Laryngoscope 2014;124:97–103 [DOI] [PubMed] [Google Scholar]
- 12.Hur K, Zhou S, Kysh L. Adjunct steroids in the treatment of peritonsillar abscess: a systematic review. Laryngoscope 2018;128:72–7 [DOI] [PubMed] [Google Scholar]
- 13.Sadeghirad B, Siemieniuk RAC, Brignardello-Petersen R, Papola D, Lytvyn L, Vandvik PO et al. Corticosteroids for treatment of sore throat: systematic review and meta-analysis of randomised trials. BMJ 2017;358:j3887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li X, Xu S, Yu M, Wang K, Tao Y, Zhou Y et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol 2020;146:110–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McCabe R, Schmit N, Christen P, D'Aeth JC, Løchen A, Rizmie D et al. Adapting hospital capacity to meet changing demands during the COVID-19 pandemic. BMC Med 2020;18:329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Public Health England. COVID-19: Guidance for maintaining services within health and care settings. Infection prevention and control recommendations. [Archived Guidance version 3.2 18 June 2020]. In: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/954690/Infection_Prevention_and_Control_Guidance_January_2021.pdf [13 April 2021]
- 17.ENT UK. COVID-19 Adult Tonsillitis & Quinsy Guidelines. In: https://www.entuk.org/covid-19-adult-tonsillitis-quinsy-guidelines [13 April 2021]
- 18.Bird JH, Biggs TC, King EV. Controversies in the management of acute tonsillitis: an evidence-based review. Clin Otolaryngol 2014;39:368–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Forner D, Curry DE, Hancock K, MacKay C, Taylor SM, Corsten M et al. Medical intervention alone vs surgical drainage for treatment of peritonsillar abscess: a systematic review and meta-analysis. Otolaryngol Head Neck Surg 2020;163:915–22 [DOI] [PubMed] [Google Scholar]
- 20.Sideris AW, Ghosh N, Lam ME, Mackay SG. Peritonsillar abscess and concomitant COVID-19 in a 21-year-old male. BMJ Case Rep 2020;13:e238104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centor RM, Witherspoon JM, Dalton HP, Brody CE, Link K. The diagnosis of strep throat in adults in the emergency room. Med Decis Making 1981;1:239–46 [DOI] [PubMed] [Google Scholar]
- 22.McIsaac WJ, Kellner JD, Aufricht P, Vanjaka A, Low DE. Empirical validation of guidelines for the management of pharyngitis in children and adults. JAMA 2004;291:1587–95 [DOI] [PubMed] [Google Scholar]
- 23.Harris AM, Hicks LA, Qaseem A; High Value Care Task Force of the American College of Physicians and for the Centers for Disease Control and Prevention. Appropriate antibiotic use for acute respiratory tract infection in adults: advice for high-value care from the American College of Physicians and the Centers for Disease Control and Prevention. Ann Intern Med 2016;164:425–34 [DOI] [PubMed] [Google Scholar]
- 24.Hardman JC, McCulloch NA, Nankivell P. Do corticosteroids improve outcomes in peritonsillar abscess? Laryngoscope 2015;125:537–8 [DOI] [PubMed] [Google Scholar]
- 25.Johnson RM, Vinetz JM. Dexamethasone in the management of covid-19. BMJ 2020;370:m2648. [DOI] [PubMed] [Google Scholar]
- 26.British Society of Skeletal Radiologists. Recommendations of the British Society of Skeletal Radiologists: The safety of corticosteroid injections during the COVID-19 global pandemic. In: https://acpomit.csp.org.uk/system/files/documents/2021-01/musculoskeletal_radiology_during_the_covid-19_global_pandemic-rhw001180-lap.pdf [13 April 2021]
- 27.Smith ME. Admission avoidance in tonsillitis and peritonsillar abscess: a prospective national audit during the initial peak of the COVID-19 pandemic. Clin Otolaryngol 2020;46:363–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mahase E. Covid-19: low dose steroid cuts death in ventilated patients by one third, trial finds. BMJ 2020;369:m2422. [DOI] [PubMed] [Google Scholar]
- 29.RECOVERY Collaborative Group, Horby P, Lim WS, Emberson JR, Mafham M, Bell JL et al. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med 2021;384:693–704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Patel B, Hardman JC, Yang W, Robson A, Putnam G, George A et al. Reusable respirators as personal protective equipment during ENT surgery. J Laryngol Otol 2020;134:732–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.OMFS and ENT surgeons issue new COVID-19 PPE guidance. Br Dent J 2020;228:57132332939 [Google Scholar]
- 32.Selwyn D, Yang D, Heward E, Kerai A, Thompson E, Shommakhi A et al. A prospective multicentre external validation study of the Liverpool Peritonsillar abscess Score (LPS) with a no-examination COVID-19 modification. Clin Otolaryngol 2021;46:229–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stringer SP, Schaefer SD, Close LG. A randomized trial for outpatient management of peritonsillar abscess. Arch Otolaryngol Head Neck Surg 1988;114:296–8 [DOI] [PubMed] [Google Scholar]
- 34.Powell J, Wilson JA. An evidence-based review of peritonsillar abscess. Clin Otolaryngol 2012;37:136–45 [DOI] [PubMed] [Google Scholar]
- 35.Ophir D, Bawnik J, Poria Y, Porat M, Marshak G. Peritonsillar abscess. A prospective evaluation of outpatient management by needle aspiration. Arch Otolaryngol Head Neck Surg 1988;114:661–3 [DOI] [PubMed] [Google Scholar]
- 36.Lamkin RH, Portt J. An outpatient medical treatment protocol for peritonsillar abscess. Ear Nose Throat J 2006;85:658–60 [PubMed] [Google Scholar]
- 37.Cherukuri S, Benninger MS. Use of bacteriologic studies in the outpatient management of peritonsillar abscess. Laryngoscope 2002;112:18–20 [DOI] [PubMed] [Google Scholar]