Abstract
Aims
Social isolation in people living with schizophrenia is associated with poor quality of life and increased symptom severity. Volunteer befriending interventions are a potential strategy for addressing social isolation, but evidence of their effectiveness is limited, particularly in low- and middle-income countries. We assessed the experiences of volunteer befriending and tested its effectiveness for improving the quality of life of patients with schizophrenia in Bosnia and Herzegovina.
Methods
Between March 2018 and July 2020, we conducted a parallel-group, randomised controlled trial in adults with schizophrenia and poor quality of life at an outpatient clinic in Sarajevo. Patients were randomised to either the intervention, in which they were matched with a volunteer befriender with whom they met fortnightly over the 6-month intervention period, or treatment as usual. The primary outcome was quality of life measured on the Manchester Short Assessment and secondary outcomes were psychiatric symptoms and objective social outcomes. Outcome measurement was conducted by blinded researchers at 6- and 12-months.
Results
In total, 65 patients were randomised into the intervention (n = 33) and control arms (n = 32) and 55 (85%) completed follow-up assessments at 6 months. Patients in the intervention showed a significantly more favourable quality of life at 6 months (primary outcome; mean difference: 0.7, 95% CI [0.3–1.1], p = 0.003) and 12 months (mean difference: 1.7, 95% CI [1.1–2.3], p < 0.001). They also had significantly lower symptom levels at both follow-ups, and a significantly more favourable objective social situation after 12 months. Participants reported largely positive experiences.
Conclusion
The exploratory trial conducted at one site found sustained improvements in quality of life and reductions in psychiatric symptoms. This suggests that volunteer befriending may be a feasible and effective treatment for patients with schizophrenia in resource-limited contexts, such as Bosnia and Herzegovina.
Key words: Befriending, community mental health, psychosis, social isolation, volunteers
Introduction
People living with schizophrenia have smaller social networks and experience more social isolation than the general population (Harley et al., 2012; Giacco et al., 2016), which is associated with poorer quality of life, increased symptom severity and reduced treatment adherence (Becker et al., 1998; Giacco et al., 2012; Stentzel et al., 2018). The symptoms of schizophrenia can affect an individual's ability and interest in establishing social contact. Positive symptoms, such as hallucinations and delusions, are associated with active social avoidance, while negative symptoms reduce the motivation to build and maintain social relationships (Hansen et al., 2009; de Sousa et al., 2018). Poorer psychosocial outcomes in people living with schizophrenia, such as reduced employment opportunities, insecure housing, financial difficulties and diminished social role, further reduce social networks (Harley et al., 2012). At the same time, mental health stigma and prejudice towards people with severe mental illness compound experiences of social isolation (Angermeyer and Dietrich, 2006; Livingston and Boyd, 2010).
Volunteer befriending interventions are a potential resource for addressing social isolation. These interventions link volunteers with patients to provide social and practical support through regular one-to-one meetings (Mitchell and Pistrang, 2011; Thompson et al., 2016; Siette et al., 2017). While evidence to support the effectiveness of volunteer befriending is mixed (McCorkle et al., 2008; Mead et al., 2010), there is some evidence befriending patients with severe mental illness improves perceived social support, reduces social isolation and leads to a long-term increase in social contacts (Hallett et al., 2012; Sheridan et al., 2015; Priebe et al., 2020). Further, the willingness for members of the public to voluntarily spend time with people with severe mental illness presents an inexpensive resource for the design and delivery of mental health services (Priebe et al., 2014; Klug et al., 2018). As a low-cost therapeutic model that addresses resources rather than deficits, volunteer befriending interventions could be a viable option for low- and middle-income countries where mental health workforce is limited and health systems are fragmented, such as Bosnia and Herzegovina (Kucukalic et al., 2005; Fuhr et al., 2014).
Bosnia and Herzegovina suffered four years of continuous conflict leading to an increased prevalence of trauma-related psychiatric disorders. At the same time, many psychiatric institutions, including long-term treatment facilities, were physically destroyed over the course of the war. These two events led to a reform of mental health services since the conclusion of the conflict (Kucukalic et al., 2005). Economic transition and political instability have discouraged the return of refugees and encouraged economic migration, particularly of health professionals, with implications for the mental health workforce. As a result, there is a lack of services for people with severe mental illness beyond pharmacological prescription, such as psychosocial interventions (Winkler et al., 2017; Hunter et al., 2020).
We test the feasibility and effectiveness of a volunteer befriending intervention for improving quality of life for patients with schizophrenia or non-affective psychosis in Bosnia and Herzegovina.
Methods
Study design and participants
We conducted an exploratory parallel-group, pragmatic, randomised controlled trial at the Clinical Centre, University of Sarajevo between March 2018 and July 2020. The study was part of a larger Global Health Research Programme, funded by the National Institute of Health Research in the United Kingdom, which included studies on resource-oriented interventions in Bosnia and Herzegovina, Colombia and Uganda. Full study details are outlined in a published protocol, (Priebe et al., 2019) and the trial was prospectively registered with the ISRCTN registry (ISRCTN: 51290984). Ethical approval was obtained from the University of Sarajevo (18/09/2018) and Queen Mary University of London (ref: QMERC2018/66, 30/10/2018).
Patients were eligible to participate if they had: a primary diagnosis of schizophrenia or non-affective psychosis (ICD-10 F20-29), were aged 18 years and older, had capacity to provide informed consent; were experiencing poor quality of life (defined as scoring ⩽5 on the Manchester Short Assessment of Quality of Life (MANSA) scale) (Priebe et al., 1999), and had been diagnosed with schizophrenia for more than 6 months. Exclusion criteria included a primary diagnosis of substance-use disorder, learning disability, dementia, organic psychosis or bipolar disorder, being an inpatient at the time of recruitment and participating in another research study.
Patients were recruited from one site with an outpatient clinic and day hospital. Members of the clinical team screened patients with the support of researchers to identify potentially eligible patients, who were then approached by researchers and provided information about the study. Patients who provided written consent then completed screening with the MANSA to assess eligibility.
Volunteer befrienders were recruited through medical and psychology student organisations. To participate, volunteers were required to commit to meet regularly with patients over a 6-month period, attend training and supervision and be 18 years of age or older. Eligible individuals were provided information about the study by a researcher and invited to apply if interested. After an interview to confirm eligibility and determine their motivation for participation, interests and availability, volunteers provided written consent to participate.
Following recruitment, patients were randomly assigned to the intervention or treatment as usual group at a 1:1 ratio. Randomisation was conducted by an independent researcher using sequential computer-generated random numbers to determine allocation. Allocation information was provided to the unblinded research coordinator at the site who conducted baseline assessments.
The trial was pragmatic. The study design did not influence any treatment that the patients received during the study period other than the befriending programme in the intervention group.
Intervention and procedure
A volunteer befriending intervention was developed following consultation with mental health professionals, service users, students and non-government organisations in Sarajevo. The intervention matched one volunteer befriender with one patient, and the pair agreed to meet every two weeks over the 6-month intervention period. The pair could decide what they would like to do at each meeting, including the option of meeting other pairs to take part in group social activities. During the intervention period, three group meetings were organised for pairs to join (an art class, a psychology workshop and a sports class). Pairs were matched based on their interests, preferences and availability, which was discussed during baseline assessments with patients and the recruitment interviews with potential volunteers. The volunteer coordinator then facilitated an initial meeting with each pair.
Before the intervention commenced, volunteers attended a one-day training course which covered general information about the programme, the symptoms of schizophrenia, the responsibilities and boundaries of befriending and available resources for supervision and support. They also received regular face-to-face supervision from a senior member of the research team and the volunteer coordinator, and three group supervision sessions were organised for the volunteers to share their experiences. The senior researcher was available to respond to any concerns that arose over the duration of the intervention. After 6 months, volunteers and patients could decide to continue meeting independently.
Outcome measures
A standardised case report form was used to collect primary and secondary outcome data at baseline, 6 and 12 months. Socio-demographic information and clinical characteristics were assessed at baseline. Health service utilisation were measured at baseline and at each follow-up. Blinded researchers conducted outcome assessment at 6 and 12 months.
The primary outcome was subjective quality of life at 6 months, measured using the MANSA, which has been widely used in mental health research (Priebe et al., 1999). A mean score is calculated from patient satisfaction ratings of 12 life domains on a scale of 1 (‘couldn't be worse’) to 7 (‘couldn't be better’).
A range of secondary outcomes was measured. Mental health symptoms were assessed using the 24-item, observer-rated Brief Psychiatric Rating Scale (BPRS). (Lukoff et al., 1986) Each symptom was rated between 1 (‘not present’) and 7 (‘extremely severe’). All researchers were trained in BPRS assessments and inter-rater reliability was established before baseline data collection. The Objective Social Outcomes Index (SIX) (Priebe et al., 2008) was used to assess objective quality of life. Patients' employment, accommodation and social contacts are scored between 0 (poorest situation) to 6 (best situation). Two binary outcome items were adapted from existing instruments to measure friendships (Oliver et al., 1997; Priebe et al., 1999): one objective measure (‘In the last week, have you visited a friend, been visited by a friend or met a friend outside both your home and work?’) and one subjective measure (‘Do you have anyone who you would call a close friend?’).
Volunteers reported the number and lengths of meetings with patients to the coordinator via text message over the 12-month study period.
Patient and public involvement
How to use volunteer befriending in Bosnia and Herzegovina was influenced by discussions with representatives of the patient organisations ‘Menssana’, ‘Dodir’ and ‘Fenix’. They welcomed the idea of the intervention and were also in support of a randomised controlled study design which is still unusual in the national context. They also supported recruitment of study participants, but were not involved in the conduct of the study. The organisations will receive a report with the findings of the study, once they have been published.
Statistical analysis
All analysis was conducted in accordance with a pre-agreed statistical analysis plan by a blinded researcher. A sample size of 72 was agreed to ensure a minimum of 30 patients were enrolled in each arm (De Jong and Davidson, 1994; Browne, 1995) and to allow for 20% study attrition, which has been observed in previous research with people with psychosis (Szymczynska et al., 2017).
Baseline characteristics of both trial arms are presented descriptively. We use generalised mixed linear models (with a fixed effect for treatment and adjusted for baseline values) to compare mean MANSA and BPRS scores in each arm at baseline to 6- and 12-months and proportional odds models (with treatment as a fixed effect) to compare objective social outcomes (SIX). All analysis was conducted on available cases on an intention-to-treat basis. Cohen's d is presented as a standardised measure of effect.
Results
Participants
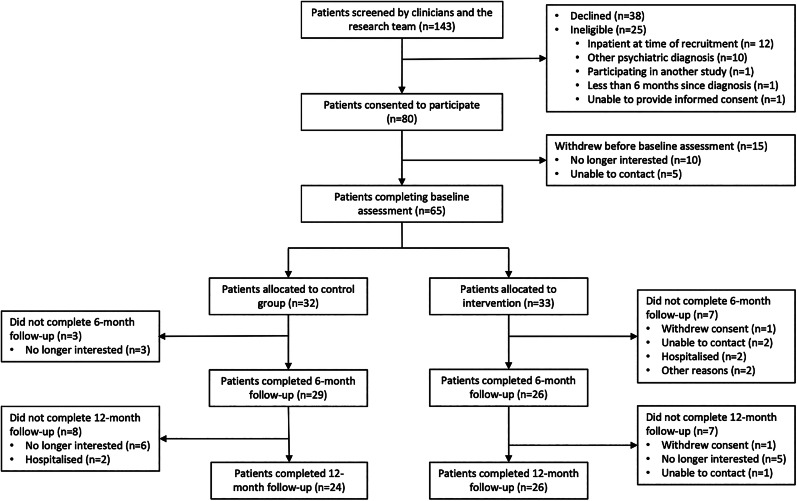
Of the 143 patient records screened for participation in the study, 118 met our eligibility criteria and 80 provided written consent to participate. The flow of patients through the study is summarised in Fig. 1.
Fig. 1.
CONSORT patient recruitment flow diagram.
During baseline assessment, five patients were unable to be contacted and 10 were no longer interested. The remaining 65 patients were randomised into the intervention (n = 33) and control arms (n = 32). Baseline characteristics of both groups are presented in Table 1.
Table 1.
Patient characteristics at baseline
| Intervention (n = 33) | Control (n = 32) | |
|---|---|---|
| Mean age in years (range) | 42 (21–68) | 44 (22–64) |
| Sex | ||
| Male | 14 (42%) | 16 (50%) |
| Female | 19 (58%) | 16 (50%) |
| Marital status | ||
| Single/unmarried | 18 (55%) | 16 (50%) |
| Married | 7 (21%) | 8 (25%) |
| Divorced/separated/widowed | 8 (24%) | 8 (25%) |
| Education | ||
| Primary or less | 4 (12%) | 3 (9%) |
| Secondary | 19 (58%) | 25 (78%) |
| Tertiary or higher | 10 (30%) | 4 (13%) |
| Living with | ||
| Family/partner | 28 (85%) | 29 (91%) |
| Alone | 4 (12%) | 2 (6%) |
| Friends/relatives | 1 (3%) | 1 (3%) |
| Employment | ||
| Full time | 6 (18%) | 8 (25%) |
| Part time | 2 (6%) | 4 (13%) |
| Unemployed | 11 (33%) | 12 (38%) |
| On pension | 6 (18%) | 6 (19%) |
| Other | 3 (9%) | 2 (6%) |
| Physical comorbidities | ||
| Cancer | 1 (3%) | 1 (3%) |
| Musculoskeletal problems | 5 (15%) | 1 (3%) |
| Diabetes | 1 (3%) | 2 (6%) |
| Cardiovascular disease | 2 (6%) | 4 (13%) |
| Hypertension | 7 (21%) | 7 (22%) |
| High cholesterol | 8 (24%) | 6 (19%) |
| Admitted to psychiatric in-patient treatment in the past 3 months | 7 (21%) | 9 (28%) |
| Seen by a psychologist in the past 3 months | 10 (30%) | 11 (34%) |
| Prescribed antipsychotic medication in the past 3 months | 33 (100%) | 29 (91%) |
The mean age of participants was 43 (range: 21–68) and 54% were female. The two groups did not show substantial differences on any of the assessed socio-demographic and clinical characteristics.
After advertising the intervention, 110 students applied to participate as volunteers and interviews were scheduled with 75. After checking eligibility, 36 volunteers were chosen to participate, and another six recruited as reserves in the case of drop out. The mean age of participating volunteers was 25 (range 22–29) and 75% were female. All volunteers were either full time (64%) or part-time (36%) university students.
Patients in the intervention group were matched with one volunteer to create 33 pairs. Twenty-eight pairs attended an initial meeting facilitated by the study coordinator, while five pairs never met one another. The pairs met on average five times over the 6-month intervention period (range 0–12), and 25 pairs (75%) attended the pre-defined threshold of at least three out of the 12 recommended meetings over 6 months. After the initial meeting, one patient withdrew from the study and one patient was rematched to another volunteer based on patient preferences. Fifteen pairs (45%) continued to meet together after the intervention period had ended.
During the 6-month follow-up, four patients in the intervention group and two patients (3) in the control group were seen by a psychologist, and 28 patients (23) in the intervention group and 25 patients (22) in the control group were prescribed anti-psychotics. No patient in any of the two groups received further psycho-social treatments during the study period.
Because the pandemic imposed restrictions on social contacts, further face-to-face meetings between volunteers and patients following the 6-month intervention period were difficult or impossible, and 30% of 6-month interviews and all 12-month interviews had to be conducted via telephone or online. There were no other deviations from the protocol.
Outcomes
At the end of the 6-month intervention period, 55 patients (intervention: n = 26, control: n = 29) completed follow-up assessments and at 12 months, 50 patients (intervention: n = 26, control: n = 24) completed an assessment. The results of outcome assessments are shown in Table 2.
Table 2.
Outcomes of patients at baseline, 6 and 12 months (primary outcome: MANSA at 6 months)
| Intervention | Control | Coefficient (95% CI)* | p-value | |||
|---|---|---|---|---|---|---|
| n | mean (SD) | n | mean (SD) | |||
| MANSA | ||||||
| Baseline | 33 | 4.4 ± 0.6 | 32 | 4.3 ± 0.6 | … | … |
| 6 months | 29 | 5.1 ± 0.8 | 26 | 4.3 ± 1.0 | −0.50 (−0.94 − −0.07) | 0.024 |
| 12 months | 26 | 5.7 ± 0.7 | 24 | 3.9 ± 1.2 | −1.52 (−2.37 − −0.67) | 0.001 |
| SIX | ||||||
| Baseline | 33 | 3.9 ± 1.2 | 32 | 4.1 ± 1.3 | … | … |
| 6 months | 29 | 4.2 ± 1.2 | 26 | 4.2 ± 1.5 | 1.48 (−0.13–3.08) | 0.072 |
| 12 months | 26 | 4.8 ± 1.3 | 24 | 3.6 ± 1.4 | 2.20 (0.50–3.90) | 0.011 |
| BPRS | ||||||
| Baseline | 33 | 33.8 ± 7.1 | 32 | 35.6 ± 7.1 | … | … |
| 6 months | 29 | 29.6 ± 3.7 | 26 | 36.8 ± 9.8 | 5.29 (1.94–8.64) | 0.003 |
| 12 months | 26 | 30.7 ± 4.5 | 24 | 37.7 ± 5.5 | 6.85 (3.02–10.67) | 0.001 |
*For the MANSA and BPRS, regression coefficients derived from mixed linear models with a fixed effect for treatment adjusted for baseline scores. For the SIX, proportional odds models with a random intercept and fixed effect for treatment.
After 6 months, there was no difference between participants and controls in the proportion reporting having someone they would call a close friend, or the proportion having seen a friend in the past week. However, at 12-month assessment participants were more likely to have someone they would call a close friend (92%) compared with controls (54%, p = 0.003). Similarly, they were more likely to have seen a friend in the past week (participants: 85%, controls: 29%, p < 0.001).
Primary and secondary outcome measurements at all three time points are presented in Table 2. The intervention had a significant effect on our primary outcome, quality of life at 6 months (Cohen's d = 0.88, p = 0.024,) and at quality of life at 12 months (d = 1.83, p = 0.001). Significant effects were also observed in psychiatric symptoms at 6 months (d = 0.97, p = 0.003) and 12 months (d = 1.39, p = 0.001). For objective social outcomes (SIX), there was a trend towards better scores at 6 months (proportional odds ratio = 1.48 [95% CI −0.13–3.08, p = 0.072]) and significant effect at 12 months (proportional odds ratio = 2.20 [95% CI 0.50–3.90, p = 0.011]).
In a sensitivity analysis, we repeated the analysis of the primary outcome of quality of life at 6 months with imputed data for missing patients, using multiple imputation by fully conditional specification. This did not alter the finding of the analysis of available cases as reported before (d = 0.91, p = 0.001).
Patient and volunteer experiences
After the 6-month intervention period, 15 patients and 15 volunteers were interviewed about their experiences and some of their accounts are presented in Table 3.
Table 3.
Patient and volunteer accounts of participating in the intervention
| Patient experiences |
| ‘Before the programme I was worried how it was all going to look like. Are we going to get along? What would we talk about? Who would the person be? I was wondering, why am I doing all this? But now I'm happy I did it. …Afterwards, it was easier for me to contact and talk to new people and even people I already know. I started to hang out more with other people, that's something I wasn't used to… ' (Patient 010) |
| ‘…in the beginning I was very sceptical, but as it started developing, I changed my mind and at this point I can say it is a great thing for people with mental illness… I think it is so important to have an intervention like this because I think it is important to have something more than just medication… you just need something beside the drugs.’ (Patient 051) |
| ‘Having someone to go out with beside my mum, was meaningful for me, especially just after the hospitalisation… my family was with me of course, providing support but having someone who is not from your house is very different. I believe I have one more friend now. I'm glad we were introduced to each other and matched this way. We've continued contact and meetings after the intervention too.' (Patient 058) |
| Volunteer experiences |
| Throughout our friendship, I felt like his self-confidence raised, he became to start the conversation, also to invite other people out, and that also made me feel happy and somehow, at least partly, responsible for that. That rewarding feeling was something that made me to go to the next meeting… I couldn't imagine a better feeling than helping that young man feel better about himself.' (Volunteer 032) |
| I noticed that he was a bit different, a bit more open every time we met. He started to talk more about going out with people… I believe that's what motivated me the most to continue with meetings.’ (Volunteer 025) |
| ‘I've never had contact with someone who has severe mental illness, but I didn't expect it to be this way. I expected to have much more difficulties in communication, so I was truly surprised when my friend and I started to talk about things easily, even some things I didn't used to share easily with some of my closest people.' (Volunteer 004) |
| ‘From this perspective, all those stereotypes about mentally ill people seem so unnecessary and exaggerated. I've never regretted being a part of this programme, and something similar ever happens again, I would be happy to be a part of it.’ (Volunteer 032) |
Discussion
This is the first randomised controlled trial of volunteer befriending for patients with schizophrenia in Bosnia and Herzegovina and one of the first conducted anywhere in the world (Harris et al., 1999; Davidson et al., 2004; Sheridan et al., 2015; Priebe et al., 2020). We observed large and sustained improvements in both objective and subjective measures of quality of life and reductions in psychiatric symptoms. Patients in the intervention group had more social contacts with friends and were more likely to have a close friend at 12-month follow-up, compared with controls. The intervention appears feasible and acceptable in this context. Pairs met regularly over the intervention period and 75% attended our pre-defined minimum number of meetings. We had lower than expected attrition from the study and 45% of pairs chose to stay in contact after the intervention period ended. These findings were illustrated by positive accounts by both patients and volunteers.
Patients in the intervention group had, as compared to the control group, a more favourable change in the mean MANSA score of 0.7 points at 6 months and of 1.7 points at 12 months. This is a clinically highly relevant benefit. An improvement of 0.7 points is equivalent to patients rating their satisfaction with at least eight of 12 life areas more positively by at least one of seven scale points. An improvement of 1.7 points is equivalent to patients rating on average all life domains more than one scale point more positively. The effect sizes are unusually high for psycho-social intervention with patients with psychotic disorders.
Strengths and limitations
The intervention was developed through consultation with local stakeholders (patients, clinicians and non-government organisations) and training sessions, supervision and support was provided to all volunteers. Valid and reliable outcome measures were used and data collected at multiple time points. These measures including a mix of both self-rated and observer-rated scales, and significant positive effects were found on both self-ratings and observer-ratings.
There are also some limitations in this study. The trial was conducted at only one site, which may affect the generalisability. Loss to follow-up at 6 months was 15% and 23% at 12 month, which may introduce some bias. However, this is below average for RCTs of non-pharmacological studies in people with severe mental illness (Szymczynska et al., 2017). Restrictions introduced due to the coronavirus disease 2019 pandemic interrupted data collection activities. At 6 months, 70% of follow-up assessments had been completed when restrictions were introduced. The remaining assessments, and all 12-month assessments, were conducted via telephone rather than face to face, which may have introduced an additional variance. This was the first psychosocial intervention trialled at the University of Sarajevo Clinical Centre. As research is not very common in Bosnia and Herzegovina and patients were unfamiliar with trial and randomisation processes, some screened patients who initially showed interest in the study were later not willing to participate. As a result, the target sample size of 72 patients was not achieved. Finally, as volunteers were predominantly recruited through advertisements at universities, they were generally younger (mean age: 25) than the patients they befriended (mean age: 43). This, together with the fact our volunteers were predominantly female, may limit the generalisability of our findings.
Comparison with literature
While there have been few studies examining volunteer befriending in other low- and middle-income countries, a group befriending intervention in Colombia for people with severe mental illness was found to be feasible and acceptable (Botero-Rodríguez et al.). Globally, peer support interventions, in which patients are matched with volunteers with lived experience of mental illness, are attracting increased attention (Ryan et al., 2019) and these programmes have been shown to be sustainable in low-resource settings (Atif et al., 2019).
Previous studies of befriending interventions for people with severe mental illness in high-income countries have found a positive effect of these programmes on social isolation and social functioning (McCorkle et al., 2008; Sheridan et al., 2015; Priebe et al., 2020). However, these studies found no subsequent improvements in quality of life or depressive symptoms. In Bosnia and Herzegovina, treatment as usual for patients with schizophrenia primarily consists of routine meetings with clinicians and pharmacotherapy, and rarely includes psychosocial support (Winkler et al., 2017). The large improvements in quality of life and symptom severity observed in our study may, in part, reflect the absence of a comprehensive package of usual care (Asher et al., 2017).
Evidence from other settings has shown that while most people with severe mental illness are willing to participate in befriending interventions, there is considerable variability in their preferences for delivery (Toner et al., 2018a). The improvements observed by participants may also reflect our decision to design an intervention which was flexibly delivered, in terms of the content, frequency and duration of meetings and activities.
Reviews of befriending programmes through volunteers in mental health show a large variation of personal characteristics of volunteers, often reflecting specific aspects of the local context and the set-up of the given programme (Hallett et al., 2012; Toner et al., 2018b). Like in a similar trial in London (Priebe et al., 2020), many volunteers in this study were young students. They had varied motivations and expectations from participating, but many hoped to gain experience and skills that might advance their future careers in psychology and medicine. Such motivation is frequent in volunteering programmes and has been described in more detail in qualitative studies (Cassidy et al., 2019). It is however different from the main motivation of volunteers in many other programmes, where volunteers are often older than the patients (Klug et al., 2018), and may influence feasibility, processes and outcomes of programmes.
Implications for research and practice
Volunteer befriending is a low-cost intervention, which appears feasible, acceptable and effective for patients with schizophrenia in Bosnia and Herzegovina, a middle-income country. Qualitative data show the intervention was valued by both patients and participants. This suggests volunteer befriending could be delivered and implemented in these settings. Future research is required to better understand implementation processes and explore the characteristics and motivations of volunteers and patients, in order to support the implementation and potential sustainability of these programmes in the longer term. This information may inform the wider adoption and implementation of volunteer befriending programmes in other low-resource settings.
Acknowledgements
The authors would like to thank the representatives of the patient organisations ‘Menssana’, ‘Dodir’ and ‘Fenix’ for their help in adapting the intervention and their support of the study.
Financial support
This research was funded by the National Institute for Health Research (NIHR) (The NIHR Global Health Group on developing psycho-social interventions, reference: 16/137/97) using UK aid from the UK Government to support global health research. The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR or the UK Department of Health and Social Care.
Conflicts of interest
None.
Data availability
Anonymised data arising from the study will be available to external researchers upon reasonable request based on a signed data-sharing agreement.
References
- Angermeyer MC and Dietrich S (2006) Public beliefs about and attitudes towards people with mental illness: a review of population studies. Acta Psychiatrica Scandinavica 113, 163–179. [DOI] [PubMed] [Google Scholar]
- Asher L, Patel V and De Silva MJ (2017) Community-based psychosocial interventions for people with schizophrenia in low and middle-income countries: systematic review and meta-analysis. BMC Psychiatry 17, 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atif N, Bibi A, Nisar A, Zulfiqar S, Ahmed I, LeMasters K, Rahman A (2019) Delivering maternal mental health through peer volunteers: a 5-year report. International Journal of Mental Health Systems 13, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker T, Leese M, Clarkson P, Taylor R, Turner D, Kleckham J and Thornicroft G (1998) Links between social networks and quality of life: an epidemiologically representative study of psychotic patients in South London. Social Psychiatry and Psychiatric Epidemiology 33, 299–304. [DOI] [PubMed] [Google Scholar]
- Botero-Rodríguez F, Hernandez MC, Uribe-Restrepo JM, Fung C, Priebe S and Gómez-Restrepo C Experiences and outcomes of group volunteer befriending with patients with severe mental illness: an exploratory mixed-methods study in Colombia. BMC Psychiatry. doi: 10.21203/rs.3.rs-119897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne RH (1995) On the use of a pilot sample for sample size determination. Statistics in Medicine 14, 1933–1940. [DOI] [PubMed] [Google Scholar]
- Cassidy M, Thompson R, El-Nagib R, Hickling LM and Priebe S (2019) Motivations and experiences of volunteers and patients in mental health befriending: a thematic analysis. BMC Psychiatry 19, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson L, Shahar G, Stayner DA, Chinman MJ, Rakfeldt J and Tebes JK (2004) Supported socialization for people with psychiatric disabilities: lessons from a randomized controlled trial. Journal of Community Psychology 32, 453–477. [Google Scholar]
- De Jong RM and Davidson J (1994) The Functional Central Limit Theorem and Weak Convergence to Stochastic Integrals I: Weakly Dependent Processes. Econometric Theory 16(5), 621–642. [Google Scholar]
- de Sousa P, Sellwood W, Eldridge A and Bentall RP (2018) The role of social isolation and social cognition in thought disorder. Psychiatry Research 269, 56–63. [DOI] [PubMed] [Google Scholar]
- Fuhr DC, Salisbury TT, De Silva MJ, Atif N, van Ginneken N, Rahman A and Patel V (2014) Effectiveness of peer-delivered interventions for severe mental illness and depression on clinical and psychosocial outcomes: a systematic review and meta-analysis. Social Psychiatry and Psychiatric Epidemiology 49, 1691–1702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giacco D, McCabe R, Kallert T, Hansson L, Fiorillo A and Priebe S (2012) Friends and symptom dimensions in patients with psychosis: a pooled analysis. PLoS ONE 7, e50119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giacco D, Palumbo C, Strappelli N, Catapano F and Priebe S (2016) Social contacts and loneliness in people with psychotic and mood disorders. Comprehensive Psychiatry 66, 59–66. [DOI] [PubMed] [Google Scholar]
- Hallett C, Klug G, Lauber C and Priebe S (2012) Volunteering in the care of people with severe mental illness: a systematic review. BMC Psychiatry 12, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen CF, Torgalsbøen A-K, Melle I and Bell MD (2009) Passive/apathetic social withdrawal and active social avoidance in schizophrenia: difference in underlying psychological processes. The Journal of Nervous and Mental Disease 197, 274–277. [DOI] [PubMed] [Google Scholar]
- Harley EW-Y, Boardman J and Craig T (2012) Friendship in people with schizophrenia: a survey. Social Psychiatry and Psychiatric Epidemiology 47, 1291–1299. [DOI] [PubMed] [Google Scholar]
- Harris T, Brown GW and Robinson R (1999) Befriending as an intervention for chronic depression among women in an inner city: 1: randomised controlled trial. The British Journal of Psychiatry 174, 219–224. [DOI] [PubMed] [Google Scholar]
- Hunter J, McCabe R, Francis JJ, Pemovska T, Ribić E, Me S … Jovanović N (2020) Implementing a mental health intervention in low- and-middle-income countries in Europe: is it all about resources? Global Psychiatry 4, 31–54. Available at https://globalpsychiatry.co.uk/article_1409_6d5c1820d6de8cb104fbe8c30b6c933d.pdf [Google Scholar]
- Klug G, Toner S, Fabisch K and Priebe S (2018) Characteristics and motivations of volunteers providing one-to-one support for people with mental illness: a survey in Austria. Social Psychiatry and Psychiatric Epidemiology 53, 841–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kucukalic A, Dzubur-Kulenovic A, Ceric I, Jacobsson L, Bravo-Mehmedbasic A and Priebe S (2005) Regional collaboration in reconstruction of mental health services in Bosnia and Herzegovina. Psychiatric Services 56, 1455–1457. [DOI] [PubMed] [Google Scholar]
- Livingston JD and Boyd JE (2010) Correlates and consequences of internalized stigma for people living with mental illness: a systematic review and meta-analysis. Social Science and Medicine 71, 2150–2161. [DOI] [PubMed] [Google Scholar]
- Lukoff D, Nuechterlein K and Ventura J (1986) Manual for the expanded brief psychiatric rating scale. Schizophrenia Bulletin 12, 594–602. [Google Scholar]
- McCorkle BH, Rogers ES, Dunn EC, Lyass A and Wan YM (2008) Increasing social support for individuals with serious mental illness: evaluating the compeer model of intentional friendship. Community Mental Health Journal 44, 359–366. [DOI] [PubMed] [Google Scholar]
- Mead N, Lester H, Chew-Graham C, Gask L and Bower P (2010) Effects of befriending on depressive symptoms and distress: systematic review and meta-analysis. The British Journal of Psychiatry 196, 96–101. [DOI] [PubMed] [Google Scholar]
- Mitchell G and Pistrang N (2011) Befriending for mental health problems: processes of helping. Psychology and Psychotherapy: Theory, Research and Practice 84, 151–169. [DOI] [PubMed] [Google Scholar]
- Oliver J, Huxley P, Priebe S and Kaiser W (1997) Measuring the quality of life of severely mentally ill people using the Lancashire quality of life profile. Social Psychiatry and Psychiatric Epidemiology 32, 76–83. [DOI] [PubMed] [Google Scholar]
- Priebe S, Huxley P, Knight S and Evans S (1999) Application and results of the Manchester Short Assessment of Quality of Life (MANSA). International Journal of Social Psychiatry 45, 7–12. [DOI] [PubMed] [Google Scholar]
- Priebe S, Watzke S, Hansson L and Burns T (2008) Objective social outcomes index (SIX): a method to summarise objective indicators of social outcomes in mental health care. Acta Psychiatrica Scandinavica 118, 57–63. [DOI] [PubMed] [Google Scholar]
- Priebe S, Omer S, Giacco D and Slade M (2014) Resource-oriented therapeutic models in psychiatry: conceptual review. The British Journal of Psychiatry 204, 256–261. [DOI] [PubMed] [Google Scholar]
- Priebe S, Fung C, Sajun SZ, Alinaitwe R, Giacco D, Gómez-Restrepo C … Slatina S (2019) Resource-oriented interventions for patients with severe mental illnesses in low- and middle-income countries: trials in Bosnia-Herzegovina, Colombia and Uganda. BMC Psychiatry 19, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Priebe S, Chevalier A, Hamborg T, Golden E, King M and Pistrang N (2020) Effectiveness of a volunteer befriending programme for patients with schizophrenia: randomised controlled trial. The British Journal of Psychiatry 217, 477–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan GK, Kamuhiirwa M, Mugisha J, Baillie D, Hall C, Newman C … De Silva MJ (2019) Peer support for frequent users of inpatient mental health care in Uganda: protocol of a quasi-experimental study. BMC Psychiatry 19, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheridan AJ, Drennan J, Coughlan B, O'Keeffe D, Frazer K, Kemple M … Kow V (2015) Improving social functioning and reducing social isolation and loneliness among people with enduring mental illness: report of a randomised controlled trial of supported socialisation. International Journal of Social Psychiatry 61, 241–250. [DOI] [PubMed] [Google Scholar]
- Siette J, Cassidy M and Priebe S (2017) Effectiveness of befriending interventions: a systematic review and meta-analysis. BMJ Open 7, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stentzel U, van den Berg N, Schulze LN, Schwaneberg T, Radicke F, Langosch JM … Grabe H-J (2018) Predictors of medication adherence among patients with severe psychiatric disorders: findings from the baseline assessment of a randomized controlled trial (Tecla). BMC Psychiatry 18, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szymczynska P, Walsh S, Greenberg L and Priebe S (2017) Attrition in trials evaluating complex interventions for schizophrenia: systematic review and meta-analysis. Journal of Psychiatric Research 90, 67–77. [DOI] [PubMed] [Google Scholar]
- Thompson R, Valenti E, Siette J and Priebe S (2016) To befriend or to be a friend: a systematic review of the meaning and practice of “befriending” in mental health care. Journal of Mental Health 25, 71–77. [DOI] [PubMed] [Google Scholar]
- Toner S, Cassidy M, Chevalier A, Farreny A, Leverton M, da Costa MP and Priebe S (2018a) Preferences for befriending schemes: a survey of patients with severe mental illness. BMC Psychiatry 18, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toner S, Hickling LM, Costa MPD, Cassidy M and Priebe S (2018b) Characteristics, motivations and experiences of volunteer befrienders for people with mental illness: a systematic review and narrative synthesis. BMC Psychiatry 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winkler P, Krupchanka D, Roberts T, Kondratova L, Machů V, Höschl C … Bitter I (2017) A blind spot on the global mental health map: a scoping review of 25 years’ development of mental health care for people with severe mental illnesses in central and Eastern Europe. The Lancet Psychiatry 4, 634–642. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Anonymised data arising from the study will be available to external researchers upon reasonable request based on a signed data-sharing agreement.