Abstract
Objective
The present cross-sectional study investigated quality of life (QOL) in a large cohort of German adults with congenital heart disease (ACHDs) in association with patient-related and clinical variables.
Design
Cross-sectional survey.
Participants
Between 2016 and 2019, a representative sample of 4014 adults with various forms of congenital heart defect (CHD) was retrospectively analysed. Inclusion criteria were confirmed diagnosis of CHD; participant aged 18 years and older; and necessary physical, cognitive and language capabilities to complete self-report questionnaires.
Primary and secondary outcome measures
QOL was assessed using the 5-level EQ-5D version (EQ-5D-5L). Sociodemographic and medical information was obtained by a self-devised questionnaire. Associations of QOL with patient-reported clinical and sociodemographic variables were quantified using multiple regression analysis and multiple ordinal logit models.
Results
Overall, ACHDs (41.8±17.2 years, 46.5% female) reported a good QOL comparable to German population norms. The most frequently reported complaints occurred in the dimensions pain/discomfort (mean: 16.3, SD: p<0.001) and anxiety/depression (mean: 14.3, p<0.001). QOL differed significantly within ACHD subgroups, with patients affected by pretricuspid shunt lesions indicating the most significant impairments (p<0.001). Older age, female sex, medication intake and the presence of comorbidities were associated with significant reductions in QOL (p<0.001). CHD severity was positively associated with QOL within the dimensions of self-care (OR 0.148, 95% CI 0.04 to 0.58) and mobility (OR 0.384, 95% CI 0.19 to 0.76).
Conclusion
Current findings temper widely held assumptions among clinicians and confirm that ACHDs experience a generally good QOL. However, specific subgroups may require additional support to cope with disease-related challenges. The negative correlation of QOL with age is especially alarming as the population of ACHDs is expected to grow older in the future.
Trial registration number
DRKS00017699; Results.
Keywords: cardiac epidemiology, preventive medicine, adult cardiology, congenital heart disease, epidemiology, mental health
Strenghts and limitations of this study.
First study of its kind exploring quality of life (QOL) among 4014 patients with different medical and patient-related backgrounds.
Uniform conceptualisation of QOL based on EQ-5D-5L, which is a highly reliable and valid outcome measure within the cardiovascular area.
Present findings help clinicians to identify specific subsets of patients who require extra psychological support and therefore constitute a major step in paving the way towards integrative cardiac care.
Causal inferences are not possible due to the cross-sectional design of this study.
Ambiguous findings open new avenues for future research in understanding the construction of self-rated health despite or as a consequence of congenital heart defect.
Introduction
Congenital heart defects (CHDs) are the most common isolated inborn organ malformations and affect 1.35–1.5 million children each year. Although 90% of patients with CHD survive into adulthood, many of them are not cured and need to adapt to their chronic medical condition throughout their lives.1 Besides symptoms related to their heart disease, lifelong psychosocial impairments may seriously impact the patients’ perceived quality of life (QOL).2 While clinical research traditionally focused on objective medical outcomes, the relevance of QOL and various related patient-reported outcomes is increasingly recognised in the evaluation of care for adults with congenital heart disease (ACHDs).3
Research on QOL in ACHDs is still relatively scarce and not conclusive. Empirical findings indicate that QOL among ACHDs is compromised by sociodemographic factors (unemployment, older age and single status), psychological features (negative illness perceptions and distressed personality) and medical characteristics (eg, hospitalisation and worse functional status). QOL has been found to be positively associated with higher socioeconomic and educational status, stronger social support, better functional class, better knowledge of CHD, stronger sense of coherence, as well as the absence of cardiac surgery. Existing findings are inconsistent regarding cardiovascular status, medication, age and gender, although these variables appeared to be the most frequently investigated determinants.4
These inconsistent results of existing research on QOL in ACHDs can be attributed to a lack of a clear conceptual background, inconsistent methods and insufficient sample sizes.4 Additionally, the high heterogeneity of ACHDs constitutes a substantial confounding factor due to their great anatomical and clinical disease complexity. Most studies on QOL in ACHDs focused on specific subgroups of patients, which limits their informational value. Consequently, clinical parameters were not sufficiently examined to explain potential differences in QOL by the underlying diagnosis or severity of CHD. Although a recent review attests temporal qualitative improvements in QOL studies over the past decades, the current research situation still fails to meet scientific quality criteria.5
The present study aimed to assess QOL within a large sample of ACHDs in Germany and to examine potential determinants of QOL in terms of patient-related and medical characteristics. Identifying determinants of QOL, along with special needs of ACHDs, could advance the improvement of healthcare for this growing patient population.
Methods
Design
The present study represents a subanalysis of the nationwide VEMAH initiative (Versorgungssituation von Erwachsenen mit angeborenen Herzfehlern, ‘Medical Care Situation of ACHD’ in English). Detailed information on the rationale, design and methods is documented in a former published paper.6 VEMAH is a multicentre, cross-sectional study to assess the healthcare situation of ACHDs in Germany. Coordination of VEMAH was initiated and carried out by the German Heart Centre Munich.
Population
A questionnaire package was consecutively addressed to ACHDs presenting at the Department of Congenital Heart Disease and Paediatric Cardiology of the German Heart Centre Munich and the Department of Cardiology of the University of Erlangen. Additionally, the health insurance provider AOK Bayern distributed questionnaires to their policyholders with CHD in Bavaria, and the National Register for Congenital Heart Defects in Berlin, Germany, invited its members to participate in the study online. Guidelines on good clinical practice and data protection guidelines were followed. Inclusion criteria were (1) confirmed diagnosis of CHD according to the definition of Thiene and Frescura7; (2) participant age of 18 years and older; and (3) necessary physical, cognitive and language capabilities to complete self-report questionnaires.
Measures
Patients completed a questionnaire either in person, online or by mail. Data collection took place between 2016 and 2019. QOL was measured using the generic questionnaire 5-level EQ-5D version (EQ-5D-5L).8
Demographic and clinical information
Sociodemographic and medical information was obtained by a self-devised questionnaire. Medical variables included leading CHD, medication, presence of cyanosis, (non-)cardiac comorbidities and hereditary diseases. Following the recommendations of the American College of Cardiology, patients were divided into three severity groups based on their CHD diagnosis.9
QOL (EQ-5D-5L)
QOL was measured using the updated five-level version of the EQ-5D,8 which provides a simple, generic measure of a patient’s perceived health status. The EQ-5D-5L consists of a descriptive system questionnaire and a Visual Analogue Scale (VAS). The descriptive system compromises five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Each patient was asked to indicate his perceived impairments on a 5-point Likert scale ranging from ‘no problems’ to ‘extreme problems/unable’. Responses were converted into a single weighted index score (EQ-5D Index), which indicates how good or poor the respondent’s health status is based on existing population norms. A value set for the EQ-5D-5L, based on a representative sample of the German population, has recently been developed.10 The VAS indicates a patient’s overall health state on the day of the questionnaire completion. It is a scale which ranges from 0 (‘the worst health you can imagine’) to 100 (‘the best health you can imagine’) and provides a quantitative measure of a patient’s perceived health. The EQ-5D-5L proved to be a reliable and valid method for measuring QOL in cardiovascular populations (Cronbach’s alpha=0.856).11
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics V.24.0. Descriptive measures were calculated for sample characteristics, including patient-reported sociodemographic and medical variables (absolute and relative frequencies, mean and SD). The relationships between CHD diagnosis groups and EQ-5D-index values, including the underlying dimensions mobility, self-care, usual activities, pain/discomfort and anxiety/depression were analysed. The comparison of ordinally scaled values was based on cumulative frequencies representing the relative proportion of patients with moderate to severe symptoms on the specific dimensions. Kruskal-Wallis tests were applied to reveal significant differences between EQ-5D-dimensions and metric index values. Furthermore, the relationship between EQ-5D VAS scores and dedicated index values was analysed with respect to various patient characteristics. Multiple regression models using ordinary least squares (OLS) estimates were calculated, while bivariate Pearson coefficients were used to analyse the correlation between VAS and index scores. Finally, multiple ordinal logit models were applied to identify significant predictors of the respective QOL dimensions. For all tests, the statistical significance level was set at a p value of <0.05. Data analysis was currently performed for complete cases on each variable. To rule out a potential distortion of findings, a further comparison between statistically included and excluded patients was conducted and revealed no significant differences concerning their QOL.
Patient and public involvement
Neither patients nor the public were involved in the design and conduct of this research. The methodology of this research was adapted in multidisciplinary collaboration.
Results
Sample characteristics
A total of 4014 patients was analysed (46.5% female) (table 1). The mean age of ACHDs was 41.8±17.2 (18–97) years. Patients were subclassified according to the underlying CHD into six main groups, consisting of complex CHD (n=581), pretricuspid shunts (n=621), post-tricuspid shunts (n=406), right heart or pulmonary artery anomalies (n=526), left heart or aortic anomalies (n=898) and miscellaneous CHD (n=602). Overall, 15.4% of patients (n=602) presented with cyanosis. The severity of CHD was determined according to the Warnes classification system as simple (n=1722, 62.0%), intermediate (n=650, 23.4%) or severe (n=406, 14.6%).12
Table 1.
Characteristics of the underlying study population
| Variables | n (%) |
| Age group (years) (n=3903) | |
| 18–34 | 1663 (42.6) |
| 35–64 | 1733 (44.4) |
| 65+ | 507 (13.0) |
| Gender (n=3898) | |
| Male | 2087 (53.5) |
| Female | 1811 (46.5) |
| Residence (n=3855) | |
| City | 775 (20.1) |
| Town | 590 (15.3) |
| Rural | 2490 (64.6) |
| Insurance (n=3905) | |
| Public | 3679 (94.2) |
| Private | 219 (5.6) |
| No insurance | 7 (.2) |
| Type of congenital heart defect (CHD) (n=4014) | |
| Complex congenital heart defects | 581 (14.5) |
| Primary pretricuspid shunts | 621 (15.5) |
| Primary post-tricuspid shunts | 406 (10.1) |
| Right heart/pulmonary artery anomalies | 526 (13.1) |
| Left heart/aortic anomalies | 898 (22.4) |
| Miscellaneous CHD | 602 (15.0) |
| Unclassifiable | 380 (9.5) |
| Warnes class (n=2778) | |
| Simple | 1722 (62.0) |
| Moderate | 650 (23.4) |
| Severe | 406 (14.6) |
QOL and ACHDs
EQ-5D dimensions were found to be differently associated with CHD subgroups. Significant differences between the underlying diagnosis were found on all dimensions (p<0.001). Compared with all other subgroups, pretricuspid shunts were particularly impaired in mobility, daily activities, pain/discomfort and anxiety/depression (table 2). In contrast, complex CHD showed the least problems on the respective descriptive dimensions (figures 1–5).
Table 2.
Leading diagnosis of CHD and EQ-5D-results
| EQ-5D | Total | Complex CHDs | Primary pretricuspid shunts | Primary post-tricuspid shunts | Right heart/pulmonary artery anomalies | Left heart/aortic anomalies | Unclassifiable | Miscellaneous | P value |
| Dimension | N=4014 | n=581 | n=621 | n=406 | n=526 | n=898 | n=380 | n=602 | |
| Mobility | 12.2 | 8.6 | 13.6 | 10.4 | 9.6 | 10.5 | 15.0 | 16.6 | <0.001* |
| Self-care | 3.5 | 2.0 | 3.0 | 2.3 | 3.2 | 3.5 | 4.4 | 5.4 | 0.017* |
| Usual activities | 13.2 | 13.7 | 13.5 | 11.2 | 12.6 | 11.1 | 14.1 | 16.8 | <0.001* |
| Pain/discomfort | 16.3 | 13.7 | 20.4 | 12.3 | 11.8 | 14.3 | 19.5 | 22.7 | <0.001* |
| Anxiety/depression | 14.3 | 14.8 | 17.5 | 14.2 | 12.6 | 12.0 | 14.4 | 15.5 | 0.002* |
| EQ-5D VAS | n=3761 | n=540 | n=605 | n=388 | n=485 | n=844 | n=351 | n=548 | <0.001* |
| Mean | 76.15 | 78.21 | 73.29 | 77.28 | 79.50 | 77.36 | 74.32 | 72.80 | |
| SD | 18.97 | 17.12 | 19.93 | 19.90 | 17.48 | 18.55 | 19.56 | 19.57 | |
| EQ-5D Index | n=3690 | n=540 | n=583 | n=383 | n=489 | n=828 | n=344 | n=523 | <0.001* |
| Mean | 0.90 | 0.92 | 0.89 | 0.91 | 0.92 | 0.91 | 0.88 | 0.87 | |
| SD | 0.15 | 0.14 | 0.15 | 0.14 | 0.15 | 0.14 | 0.16 | 0.18 |
Data for EQ-5D-dimensions represent relative percentages of patients, who indicated moderate to severe problems with respect to each dimension. Significant differences were calculated using Kruskal-Wallis tests for independent samples.
*P<0.05.
CHD, congenital heart defect; VAS, Visual Analogue Scale.
Figure 1.
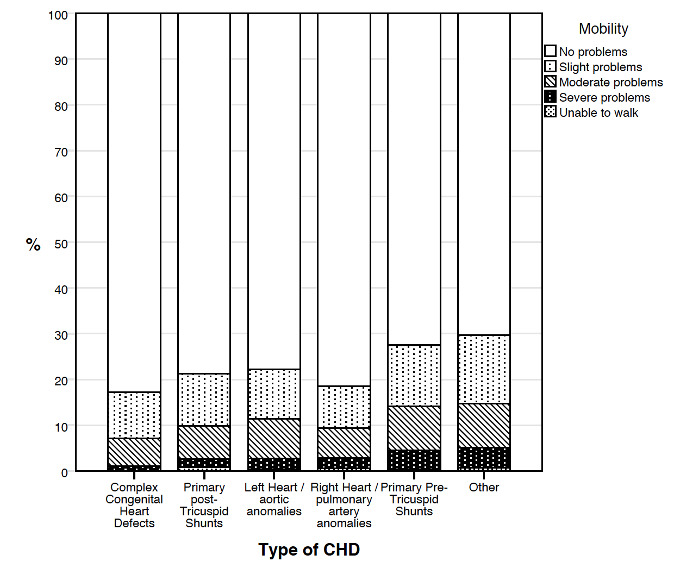
Distribution of scores for mobility. CHD, congenital heart defect.
Figure 2.
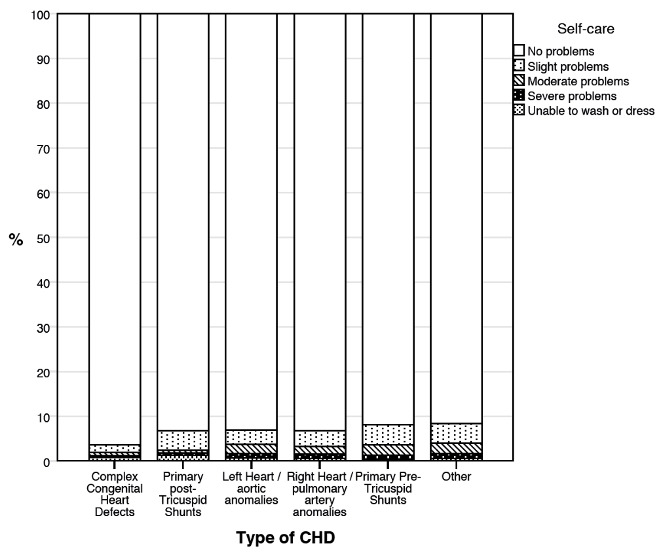
Distribution of scores for self-care. CHD, congenital heart defect.
Figure 3.
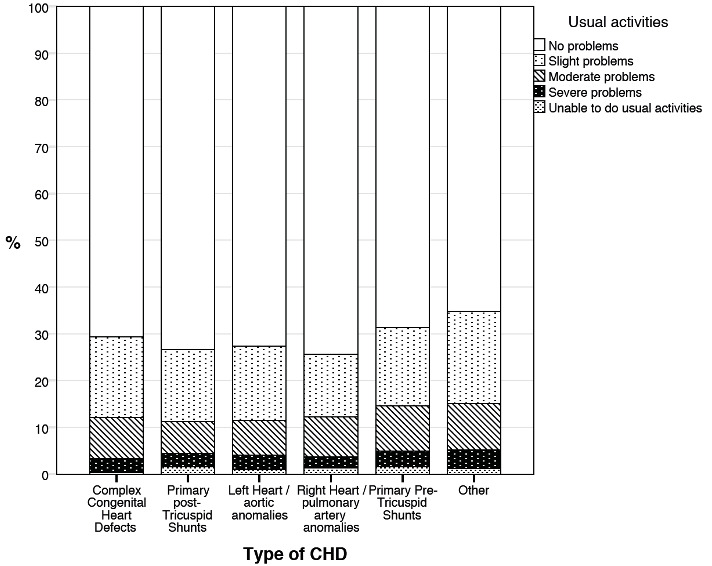
Distribution of scores for usual activities. CHD, congenital heart defect.
Figure 4.
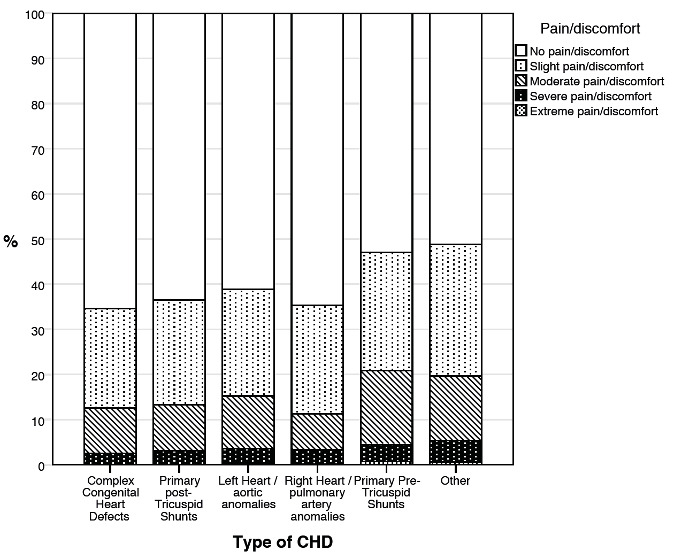
Distribution of scores for pain/discomfort. CHD, congenital heart defect.
Figure 5.
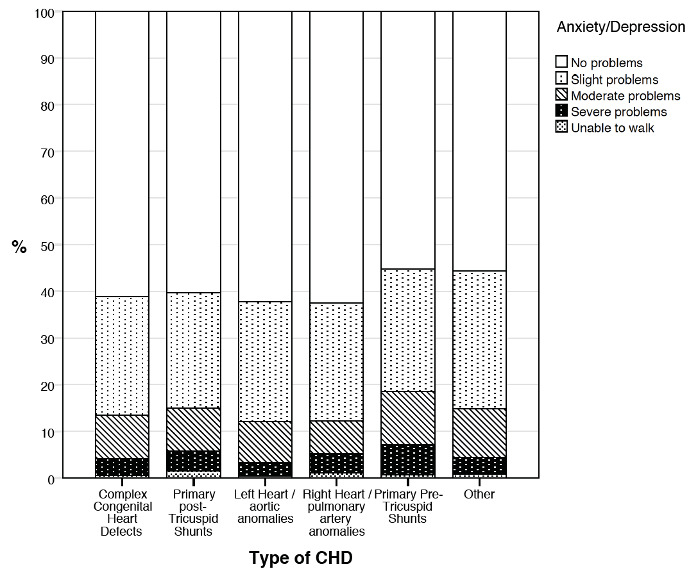
Distribution of scores for anxiety/depression. CHD, congenital heart defect.
Similar results were reflected by EQ-5D VAS and index values (p<0.001) with EQ-5D VAS values being highest in patients with right heart/pulmonary artery anomalies and complex CHD and lowest in patients with pretricuspid shunts. Observed differences were less extreme between descriptive EQ-5D Index values. Both EQ-5D values were positively correlated (r=0.623, p<0.001), with coefficients being the lowest for patients with complex CHD (r=0.579, p<0.001) and highest for patients with left heart/aortic anomalies (r=0.653, p<0.001). Variations in QOL were observed, depending on the type of measurement which was applied. Accordingly, the mean VAS score displayed a significantly lower QOL than the descriptive EQ-5D Index value.
Patient-related determinants of QOL
OLS regression models were applied to analyse relationships of sociodemographic variables with EQ-5D VAS and index values (table 3). At the 5% level of significance, age had the highest negative impact on VAS values (β=−0.32) and index values (β=−0.22). Thus, QOL decreased with advancing age. Patients aged 65+ years indicated the lowest values on both scales. Means for both EQ values were slightly higher in male patients than in female patients. Medication intake had significant negative effects on QOL in both measures. Model fit was slightly higher for the dependent variable in VAS values (R²=0.190) than EQ-5D Index values (R²=0.112).
Table 3.
Patient characteristics and their correspondence with EQ-5D vas and index values
| Variables | EQ-5D VAS | EQ-5D Index | ||||||
| Mean | SD | ß | p | Mean | SD | ß | p | |
| Age group | −0.32 | <0.001* | −0.22 | <0.001* | ||||
| 18–34 | 83.46 | 14.75 | 0.94 | 0.11 | ||||
| 35–64 | 73.44 | 18.99 | 0.89 | 0.15 | ||||
| 65+ | 62.23 | 20.83 | 0.82 | 0.21 | ||||
| Sex | 0.01 | <0.001* | 0.04 | 0.004 | ||||
| Female | 76.11 | 19.07 | 0.90 | 0.15 | ||||
| Male | 76.55 | 18.85 | 0.91 | 0.14 | ||||
| Residence | 0.02 | 0.084 | 0.03 | 0.060 | ||||
| City | 76.30 | 17.49 | 0.90 | 0.15 | ||||
| Town | 77.08 | 18.26 | 0.90 | 0.15 | ||||
| Rural | 76.01 | 19.46 | 0.90 | 0.15 | ||||
| Medication | −0.22 | <0.001* | −0.19 | <0.001* | ||||
| No | 79.16 | 17.13 | 0.92 | 0.13 | ||||
| Yes | 65.17 | 20.69 | 0.83 | 0.20 | ||||
Multivariate analysis was performed using ordinary least squares regression models with EQ-5D VAS and index values as dependent variables.
*P<0.05.
VAS, Visual Analogue Scale.
CHD-related determinants of QOL
EQ-5D-dimensions were analysed more specifically in regard to different medical features such as connective tissue diseases with cardiovascular involvement, cyanotic status and severity codes of CHD. Several ordered logistic regression models were applied using each of the five dimensions as dependent variables (table 4). Generally, patients with comorbidities had significantly increased odds of reporting problems on all dimensions than patients without comorbidities (p<0.05). Non-cardiac comorbidities accounted for significantly higher odds of having problems than cardiac comorbidities. No significant effects could be observed for cyanotic status. Furthermore, regression models showed no effects for patients with simple or moderate disease severity classes. Apparently, severely classified patients indicated decreased odds of suffering from issues related to mobility or self-care than patients in lower Warnes’ classes.
Table 4.
Impact of medical features with respect to EQ-5D dimensions
| Variable | n | Mobility n=3070 |
Self-care n=3073 |
Usual activities n=3068 | Pain/discomfort n=3051 | Anxiety/depression n=3061 |
| Comorbidities | ||||||
| Cardiac cmorbidities | 1463 | 0.302* (0.25 to 0.36) | 0.525* (0.38 to 0.73) | 0.348* (0.29 to 0.41) | 0.331* (0.28 to 0.39) | 0.467* (0.40 to 0.54) |
| Non-cardiac comorbidities | 819 | 0.263* (0.22 to 0.32) | 0.281* (0.20 to 0.39) | 0.222* (0.18 to 0.27) | 0.311* (0.26 to 0.37) | 0.243* (0.20 to 0.29) |
| Cyanosis | ||||||
| Cyanotic | 744 | 0.904 (0.49 to 1.68) | 0.396 (0.12 to 1.26) | 0.880 (0.50 to 1.56) | 1.088 (0.65 to 1.82) | 0.850 (0.51 to 1.41) |
| Acyanotic | 2176 | 1.452 (0.70 to 3.02) | 0.774 (0.20 to 3.04) | 1.207 (0.63 to 2.30) | 1.011 (0.58 to 1.77) | 0.695 (0.40 to 1.19) |
| Warnes class | ||||||
| Simple | 1722 | 1.396 (0.69 to 2.84) | 0.707 (0.18 to 2.84) | 1.109 (0.60 to 2.06) | 0.984 (0.57 to 1.69) | 0.739 (0.44 to 1.24) |
| Moderate | 650 | 0.848 (0.50 to 1.45) | 0.538 (0.17 to 1.69) | 0.985 (0.60 to 1.61) | 0.884 (0.57 to 1.37) | 0.921 (0.60 to 1.41) |
| Severe | 406 | 0.384* (0.19 to 0.76) | 0.148* (0.04 to 0.58) | 0.710 (0.39–1.30) |
0.620 (0.36–1.08) |
0.742 (0.43–1.27) |
Displayed are ORs and upper and lower bounds (95% CI), respectively, which were obtained from several ordered logistic regressions using EQ dimensions as dependent variable.
*P<0.05.
Discussion
QOL is one of the most important measures used to assess the psychosocial impact of chronic disease on a patient’s life. This is the first study to investigate patient-reported QOL within a cohort of 4014 patients encompassing a broad spectrum of CHD. QOL in ACHDs was assessed by using the EQ-5D-5L, a highly reliable and valid outcome measure within the cardiovascular area.13 It compromises two types of measurement and therefore provides a global view on QOL in terms of general life satisfaction. This allowed to revelation of genuine differences in QOL among patients with different medical and sociodemographic backgrounds, regardless of methodological considerations. Within the context of this study, QOL quantifies the influence of CHD on a patient’s ability to function and derive personal satisfaction from life.
QOL in ACHDs
In line with previous findings,14 ACHDs in general reported a good level of well-being which is comparable to German population norms.15 The twofold measure of QOL revealed that the type of measurement affects QOL scores differently. Apparently, the overall VAS score indicated a significantly lower QOL than the descriptive EQ-5D Index value. One explanation for this discrepancy is differences in the QOL coverage of both measures. It can be assumed that the descriptive system encourages a patient to examine QOL from various angles as the system breaks down QOL into various components. Thus, QOL is regarded as a subjective concept being influenced by multiple causal factors.16 In contrast, VAS picks up a one-dimensional view of perceived health where patients may indicate a higher occurrence of problems by focusing on somatic health restrictions imposed by their CHD. When comparing the quantitative association of CHD with QOL to other chronic disorders, the average reduction in VAS values in the current sample roughly resembles observations of various other heart diseases.15 In line with previous research, patients most frequently reported problems in the areas of pain/discomfort (16.3%) and anxiety/depression (14.3%).17 These rates lie considerably above German population standards, which document symptoms of anxiety/depression in 4.7% of the general public. This result further supports previous research showing that ACHDs are specifically prone to increased psychological distress and therefore require additional psychosocial support.18
A closer look at different diagnosis groups reveals that patients with pretricuspid shunts were particularly impaired in QOL. Comparable data have previously documented that QOL is not necessarily congruent with the complexity or severity of a heart disease. Even mild primary pretricuspid shunts can have a considerable negative impact on QOL.19 Clinical reality shows that pretricuspid shunts are often detected incidentally and later in life creating a different psychological situation than diagnosis of CHD early in life. Children who grew up with the awareness of their CHD may acquire a greater sense of appreciation for life and expectations consistent with their capabilities and limitations.20 Qualitative research on ACHD indicates that patients perceive the awareness of their childhood condition as a ressource to re-evaluate life priorities and develop a new life perspective.21 A recent study has further established that sense of coherence is a highly significant predictor of QOL in ACHD.22 Based on theoretical considerations, Sense of Coherence (SOC) develops during childhood and is thought to be fully developed by the age of 30 years.23 Patients who may be diagnosed later in life may have missed the chance to develop and refine coping mechanisms and may therefore experience the effects of their CHD more negatively leading to higher emotional distress. Life-stage variables, such as age at diagnosis or years of survival, need to be further investigated as possible determinants of QOL.
Socioeconomic determinants of QOL
Despite good overall QOL, EQ-5D Index and VAS values deteriorated with increasing age. This might be explained by the uncertainty in disease prognosis manifesting itself in an increased sense of vulnerability in this patient group.24 Most patients with CHD are known to do well in the first decades of life until they eventually develop unexpected age and disease-related comorbidities. This development deserves special attention as the group of ACHD is expected to grow steadily in the future.1
In contrast to previous findings,14 the present study revealed modest gender-related differences in QOL. Women were more likely to report poor QOL than men. These findings may be attributed to psychosocial factors rather than gender per se.25 In general, gender is found to influence health expectations, health behaviours and perceived health outcomes.26 Women may face a triple burden shouldering family responsibility, professional ambition and demands of their chronic disease. Research has demonstrated that women were less likely to return to work, more likely to recline psychological counselling and more socially isolated than men.27 It has also been argued that women were more willing to disclose problems than men concerning their QOL, which may partly explain the difference in their QOL.26 Engelfriet et al also showed that women with CHD were more often symptomatic and presented functional impairments, despite a higher overall mortality in men over a 5-year period.28 Gender disparities in patient–provider communication and dissatisfaction with healthcare might be another reason for decreased QOL in women. They might have higher expectations and a stronger demand for more participatory encounters with their healthcare providers.25 Improved recognition and understanding of these gender-specific differences and challenges among ACHDs is vital to improve their cardiovascular health over the long term.
Reported medication intake was inversely associated with QOL in the present study. This appears plausible because extensive or inappropriate medication can lead to severe side effects and even higher morbidity, which may considerably impair QOL.29 Aside from incorrect pharmaceutical treatment, the daily intake of medication is a constant reminder of illness and may have a negative impact on life satisfaction. Consequently, medication may be either a facilitator by providing new opportunities or an intensifier of problems by adverse psychological and somatic side effects.
Clinical determinants of QOL
Despite all advances in cardiac care, many patients with CHD are left with significant residua, sequels or complications from the underlying anomaly.9 30 The impact of comorbidities in ACHD is largely underestimated.31 The current study indicates that the presence of comorbidities increases the risk of problems on all dimensions of the EQ-5D. It is conceivable that affected patients report a lower health status since they may experience serious restrictions in various life domains. As comorbidities become increasingly dominant with advancing age, they may also explain the recorded deterioration of QOL with age in the present sample.
It is remarkable that patients with a more complex CHD scored significantly better in QOL domains. Until now, research has failed to demonstrate a clear-cut correlation between disease complexity and QOL.4 Although the present finding may seem counterintuitive at first, there are various possible explanations for a better QOL in the light of a chronic condition. Keyes’ two-continua model of mental health32 provides an important framework for explaining why patients might experience a good QOL despite their CHD. Accordingly, mental health is a complex state resulting from an interplay of environmental and psychological factors that have a profound influence on one’s subjective well-being. Keyes’ model holds that mental health (sometimes referred to as mental well-being) and mental illness are orthogonally related phenomena and not two endpoints of a single continuum. Although the current state of research confirms elevated levels of mental illness among ACHDs,18 this does not necessarily imply impaired mental well-being or decreased QOL among these patients. Furthermore, the disability paradox explains why individuals may perceive a high QOL despite serious limitations. Accordingly, QOL depends on finding a balance in life and maintaining harmonious social relationships.33 The characteristics associated with a severe CHD may potentially include favourable and compromising factors and thus explain both extremes of QOL in ACHDs. Lastly, growing up with a CHD can lead to a so-called ‘response shift’ in terms of redefining priorities in one’s life.34 It is perceivable that patients develop values different from those of healthy persons in the face of a life-threatening, chronic illness. In this context, Sprangers and Schwartz35 proposed a theoretical model to clarify and predict changes in QOL as a result of various dispositional characteristics, a patient’s health status and mechanisms to accommodate to these changes.35
Despite the extensive power of the present study, current results should be interpreted with caution due to certain limitations. The study was retrospective and cross-sectional in nature and does not allow disentanglement of any conclusions about the directionality of effects or the development of QOL over time. Since all information was based on patient-reported outcomes, medical data may have been classified incorrectly due to a patient’s limited knowledge of his or her condition. Consequently, surgical status of patients could not be identified. Subsequently, it would be advisable to synchronise these data with medical records in order to disentangle the effects of empirical–medical observations on QOL. As the enrolment was voluntary, selection bias could not be excluded and may hamper representativeness. Further, this study was performed at a tertiary care centre for ACHD, which does not reflect the typical population of CHD. Further doubts must be raised about whether the applied EQ-5D-5L provides an accurate tool to evaluate QOL among AHCDs. Although the updated 5L version demonstrates superior performance compared with its predecessor, psychometric properties in terms of high ceiling effects and weak discriminatory power have previously been questioned.36 It has further been shown that the choice of value set has an impact on EQ-5D scores.37 Since the present study used a population-based value set to construct QOL estimates, we strongly encourage to re-evaluate current findings on the basis of experience-based value sets. Further, the inventory was administered in three different ways. However, measurement invariance across the survey methods was not tested, and the equivalence across the survey methods remains questionable. Since the primary aim of this study was to assess clinical determinants of QOL, sociodemographic variables were not explicitly reviewed within the present analysis. Based on the German healthcare system, the depicted sociodemographic variables are crucial indicators of access to medical supply and were therefore separately analysed. Given previously documented associations between sociodemographic factors and QOL, generalisation of the conclusions and transmission to patients from differing socioeconomic conditions are debatable. The present survey assessed biological sex with a binary value. Given the increasing incidence of transgender and gender non-binary individuals and that large health disparities exist for this population,38 future research should increasingly expand measures of sex/gender to be trans-inclusive. Finally, no control group was involved, and data could only be compared with published national EQ-5D studies.
Conclusion
The present study shows that ACHD experience—on aggregate—a good QOL which is indistinguishable from healthy individuals. Against expectation, patients with complex CHD scored higher on QOL. However, specific subgroups of patients indicate significant reductions in QOL and may require extra support in their care to cope with challenges associated with their underlying CHD. The negative correlation with age deserves particular attention as it could lead to a decrease in QOL with the growing median age of this patient population.
QOL is regarded as a central target in the treatment of chronically ill patients. This study supports the need to further assess and promote mental well-being in ACHDs to safeguard surgical successes of the past decades which have ensured the survival of patients with CHD into adulthood. Successful treatment implies not only an increased length of survival but also enhanced subjective well-being and QOL.
Supplementary Material
Footnotes
Contributors: Conception and design: CSA, HK and JB. Administrative support: CSA, SF, SA, PE, UG, JH, HK, LP, MW, RCN and JB. Collection and assembly of data: CSA, SF, SA, UG and MW. Data analysis and interpretation: CSA and SF. Manuscript writing: CSA and JB. Final approval of manuscript: CSA, SF, SA, PE, UG, JH, HK, LP, MW, RCN and JB.
Funding: This work was supported by the German Heart Foundation (‘Deutsche Herzstiftung e.V.’) (grant number F-30-15), the patient organisation ‘Herzkind e. V.’, Actelion Pharmaceuticals Germany GmbH (grant number MED-2015-495) and the German healthcare insurance AOK-Bayern.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request. The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
The study was part of the nationwide VEMAH project which was approved on 04/05/2016 by the ethical committee of the Technical University of Munich (157/16S).
References
- 1.GBD 2017 Congenital Heart Disease Collaborators . Global, regional, and national burden of congenital heart disease, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet Child Adolesc Health 2020;4:185–200. 10.1016/S2352-4642(19)30402-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kovacs AH, Sears SF, Saidi AS. Biopsychosocial experiences of adults with congenital heart disease: review of the literature. Am Heart J 2005;150:193–201. 10.1016/j.ahj.2004.08.025 [DOI] [PubMed] [Google Scholar]
- 3.Hunter AL, Swan L. Quality of life in adults living with congenital heart disease: beyond morbidity and mortality. J Thorac Dis 2016;8:E1632–6. 10.21037/jtd.2016.12.16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moons P, Luyckx K. Quality‐of‐life research in adult patients with congenital heart disease: current status and the way forward. Acta Paediatr 2019;108:1765–72. 10.1111/apa.14876 [DOI] [PubMed] [Google Scholar]
- 5.Bratt E-L, Moons P. Forty years of quality-of-life research in congenital heart disease: temporal trends in conceptual and methodological rigor. Int J Cardiol 2015;195:1–6. 10.1016/j.ijcard.2015.05.070 [DOI] [PubMed] [Google Scholar]
- 6.Neidenbach R, Achenbach S, Andonian C, et al. Systematic assessment of health care perception in adults with congenital heart disease in Germany. Cardiovasc Diagn Ther 2021;11:481–91. 10.21037/cdt-20-825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thiene G, Frescura C. Anatomical and pathophysiological classification of congenital heart disease. Cardiovasc Pathol 2010;19:259–74. 10.1016/j.carpath.2010.02.006 [DOI] [PubMed] [Google Scholar]
- 8.Herdman M, Gudex C, Lloyd A, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Quality of Life Research 2011;20:1727–36. 10.1007/s11136-011-9903-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stout KK, Daniels CJ, Aboulhosn JA, et al. 2018 AHA/ACC guideline for the management of adults with congenital heart disease: a report of the American College of Cardiology/American heart association Task force on clinical practice guidelines. Circulation 2019;139:e698–800. 10.1161/CIR.0000000000000603 [DOI] [PubMed] [Google Scholar]
- 10.Grochtdreis T, Dams J, König H-H, et al. Health-related quality of life measured with the EQ-5D-5L: estimation of normative index values based on a representative German population sample and value set. Eur J Health Econ 2019;20:933–44. 10.1007/s10198-019-01054-1 [DOI] [PubMed] [Google Scholar]
- 11.Boczor S, Daubmann A, Eisele M, et al. Quality of life assessment in patients with heart failure: validity of the German version of the generic EQ-5D-5L™. BMC Public Health 2019;19:1464. 10.1186/s12889-019-7623-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Warnes CA, Liberthson R, Danielson GK, et al. Task force 1: the changing profile of congenital heart disease in adult life. J Am Coll Cardiol 2001;37:1170–5. 10.1016/S0735-1097(01)01272-4 [DOI] [PubMed] [Google Scholar]
- 13.Dyer MTD, Goldsmith KA, Sharples LS, et al. A review of health utilities using the EQ-5D in studies of cardiovascular disease. Health Qual Life Outcomes 2010;8:13. 10.1186/1477-7525-8-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Apers S, Kovacs AH, Luyckx K, et al. Quality of life of adults with congenital heart disease in 15 countries: evaluating country-specific characteristics. J Am Coll Cardiol 2016;67:2237–45. 10.1016/j.jacc.2016.03.477 [DOI] [PubMed] [Google Scholar]
- 15.Huber MB, Reitmeir P, Vogelmann M, et al. EQ-5D-5L in the general German population: comparison and evaluation of three yearly cross-section surveys. Int J Environ Res Public Health 2016;13:343. 10.3390/ijerph13030343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moons P, Van Deyk K, De Bleser L, et al. Quality of life and health status in adults with congenital heart disease: a direct comparison with healthy counterparts. Eur J Cardiovasc Prev Rehabil 2006;13:407–13. 10.1097/01.hjr.0000221864.19415.a0 [DOI] [PubMed] [Google Scholar]
- 17.Berghammer M, Karlsson J, Ekman I, et al. Self-reported health status (EQ-5D) in adults with congenital heart disease. Int J Cardiol 2013;165:537–43. 10.1016/j.ijcard.2011.10.002 [DOI] [PubMed] [Google Scholar]
- 18.Andonian C, Beckmann J, Biber S, et al. Current research status on the psychological situation of adults with congenital heart disease. Cardiovasc Diagn Ther 2018;8:799–804. 10.21037/cdt.2018.12.06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vigl M, Niggemeyer E, Hager A, et al. The importance of socio-demographic factors for the quality of life of adults with congenital heart disease. Qual Life Res 2011;20:169–77. 10.1007/s11136-010-9741-2 [DOI] [PubMed] [Google Scholar]
- 20.Moons P, Norekvål TM. Is sense of coherence a pathway for improving the quality of life of patients who grow up with chronic diseases? A hypothesis. Eur J Cardiovasc Nurs 2006;5:16–20. 10.1016/j.ejcnurse.2005.10.009 [DOI] [PubMed] [Google Scholar]
- 21.Moreland P, Santacroce SJ. Illness uncertainty and posttraumatic stress in young adults with congenital heart disease. J Cardiovasc Nurs 2018;33:356–62. 10.1097/JCN.0000000000000471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moons P, Apers S, Kovacs AH, et al. Sense of coherence in adults with congenital heart disease in 15 countries: patient characteristics, cultural dimensions and quality of life. Eur J Cardiovasc Nurs 2021;20:48–55. 10.1177/1474515120930496 [DOI] [PubMed] [Google Scholar]
- 23.Antonovsky A. Unraveling the mystery of health: how people manage stress and stay well. Jossey-bass, 1987. [Google Scholar]
- 24.Saliba Z, Butera G, Bonnet D, et al. Quality of life and perceived health status in surviving adults with univentricular heart. Heart 2001;86:69–73. 10.1136/heart.86.1.69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen C-A, Liao S-C, Wang J-K, et al. Quality of life in adults with congenital heart disease: biopsychosocial determinants and sex-related differences. Heart 2011;97:38–43. 10.1136/hrt.2010.200709 [DOI] [PubMed] [Google Scholar]
- 26.Barsky AJ, Peekna HM, Borus JF. Somatic symptom reporting in women and men. J Gen Intern Med 2001;16:266–75. 10.1046/j.1525-1497.2001.016004266.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ford ES, Mokdad AH, Li C, et al. Gender differences in coronary heart disease and health-related quality of life: findings from 10 states from the 2004 behavioral risk factor surveillance system. J Womens Health 2008;17:757–68. 10.1089/jwh.2007.0468 [DOI] [PubMed] [Google Scholar]
- 28.Engelfriet P, Boersma E, Oechslin E, et al. The spectrum of adult congenital heart disease in Europe: morbidity and mortality in a 5 year follow-up period. The Euro heart survey on adult congenital heart disease. Eur Heart J 2005;26:2325–33. 10.1093/eurheartj/ehi396 [DOI] [PubMed] [Google Scholar]
- 29.Olsson IN, Runnamo R, Engfeldt P. Medication quality and quality of life in the elderly, a cohort study. Health Qual Life Outcomes 2011;9:95. 10.1186/1477-7525-9-95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Perloff JK, Warnes CA. Challenges posed by adults with repaired congenital heart disease. Circulation 2001;103:2637–43. 10.1161/01.CIR.103.21.2637 [DOI] [PubMed] [Google Scholar]
- 31.Neidenbach RC, Lummert E, Vigl M, et al. Non-Cardiac comorbidities in adults with inherited and congenital heart disease: report from a single center experience of more than 800 consecutive patients. Cardiovasc Diagn Ther 2018;8:423–31. 10.21037/cdt.2018.03.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Keyes CLM. The mental health continuum: from languishing to flourishing in life. J Health Soc Behav 2002;43:207–22. 10.2307/3090197 [DOI] [PubMed] [Google Scholar]
- 33.Albrecht GL, Devlieger PJ. The disability paradox: high quality of life against all odds. Soc Sci Med 1999;48:977–88. 10.1016/S0277-9536(98)00411-0 [DOI] [PubMed] [Google Scholar]
- 34.Rapkin BD, Schwartz CE. Toward a theoretical model of quality-of-life appraisal: implications of findings from studies of response shift. Health Qual Life Outcomes 2004;2:14. 10.1186/1477-7525-2-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sprangers MA, Schwartz CE. Integrating response shift into health-related quality of life research: a theoretical model. Soc Sci Med 1999;48:1507–15. 10.1016/S0277-9536(99)00045-3 [DOI] [PubMed] [Google Scholar]
- 36.Feng Y, Parkin D, Devlin NJ. Assessing the performance of the EQ-VAS in the NHS PROMs programme. Qual Life Res 2014;23:977–89. 10.1007/s11136-013-0537-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Leidl R, Reitmeir P. An experience-based value set for the EQ-5D-5L in Germany. Value Health 2017;20:1150–6. 10.1016/j.jval.2017.04.019 [DOI] [PubMed] [Google Scholar]
- 38.Bauer GR, Braimoh J, Scheim AI, et al. Transgender-inclusive measures of sex/gender for population surveys: mixed-methods evaluation and recommendations. PLoS One 2017;12:e0178043. 10.1371/journal.pone.0178043 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request. The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.


