Abstract
Introduction
Liposarcoma is the most common sarcoma entity and accounts for 17% to 30% of soft tissue sarcomas. There are several histological types including well-differentiated liposarcoma. This paper aims to underline the interest of immunohistochemical and cytogenetic studies to diagnose well-differentiated liposarcoma and to show the delicacy of performing a surgical procedure in the cheek area.
Case presentation
The authors report the case of a 48-year-old female patient who presented with the recurrence of a right jugal mass initially diagnosed as a lipoma on the resection specimen. The patient was reoperated 5 years later and further immunohistochemical and cytogenetic studies confirmed the diagnosis of well-differentiated jugal liposarcoma.
Discussion
Sarcomas are rare malignant tumors of mesenchymal origin, arising from connective and supporting tissues. It should be noted that certain MRI features can distinguish liposarcoma from lipoma. Conventional histology and immunohistochemistry are the basic means for the diagnosis and classification of liposarcomas. However, molecular biology can add to the pathologist's analysis and rule out differential diagnoses Liposarcoma of the maxillofacial region has a better prognosis compared to other parts of the human body.
Conclusion
This paper underlines the interest of complementary immunohistochemical and cytogenetic studies to differentiate well-differentiated liposarcoma from lipoma as well as the potential for local recurrence of liposarcomas.
Keywords: Liposarcoma, Lipoma, Cheek, Recurrence
Highlights
-
•
Liposarcoma of the maxillofacial region is rare.
-
•
Histologicaly the diagnosis is done by research of the expression of MDM 2 and CDK4 in immunohistochemistry and of the amplification of these two genes by FISH.
-
•
The main treatment of liposarcoma is surgical excision.
-
•
Liposarcoma has a good prognosis in the maxillofacial region.
1. Introduction
This work has been reported in line with the SCARE 2020 criteria [1].
Sarcomas are rare malignant tumors of mesenchymal origin developed from connective and supporting tissues. Soft tissue sarcomas (STS) represent about 1% of adult cancers, of which liposarcoma is the most frequent entity in adults [2]. The criteria for histological diagnosis according to the classification of Enzinger and Weis can be difficult, in particular, to differentiate a lipoma from well-differentiated liposarcoma [3,4]. The pathologist uses classical histopathology, immunohistochemistry, and in some cases molecular biology techniques, mainly FISH (fluorescence in situ hybridization) and RT-PCR (reverse transcription polymerase chain reaction), to confirm the diagnosis [5].
The main treatment is surgical and may be associated with radiotherapy.
The prognosis is relatively favorable and depends mainly on the histological grade.
2. Case presentation
A 48-year-old female patient with a history of penicillin allergy; and an excision of a mass in the soft tissues of the right cheek 5 years ago in another hospital. The histology of the mass was in favor of a lipoma with no signs of malignancy. The evolution was marked 8 months after the removal by the recurrence of a mass of the same clinical characteristics. It had increased progressively in size responsible for discomfort for the patient for which she consulted.
The clinical examination revealed an asymmetry of the 1/3 lower of the face due to a right lower jugal mass with the healthy skin opposite. This mass was firm, rounded, and well limited, measuring about 4.5 cm on the long axis, mobile with concerning the superficial plane, not painful, and not pulsatile (Fig. 1). Examination of the oral cavity revealed a good oral condition with a lower vestibular bulge and the mucosa opposite the mass was normal. On bi-digital palpation, the mass can be easily individualized. No regional lymph nodes were found on examination.
Fig. 1.
Images showing the clinical aspect of the mass in the right cheek.
The facial CT scan showed a well-limited oval fatty mass of the jugal soft tissues with fat density crossed by linear structures measuring 44 × 20 mm, extending over 48 mm, arriving externally in contact with the superficial cervical fascia without extension to the subcutaneous soft tissues and arriving medially in contact with the right masseter without invading it (Fig. 2).
Fig. 2.

CT image of the face in axial section showing a well-limited fatty mass of the soft parts of the right cheek.
After getting informed and written consent from the patient, she underwent removal of the mass under general anesthesia by a cervical skin incision about 4 cm from the mandibular margin. Intraoperatively, an encapsulated yellowish mass was found under the platysma and was removed in monobloc without any incident (Fig. 3). The specimen was sent for histological study (Fig. 4). The immediate postoperative course was favorable. The patient received daily antibiotics with amoxicillin/clavulanic acid 1 g × 2 for 8 days and paracetamol 1 g × 3 for 5 days. The examination of the specimen showed a well-differentiated adipose proliferation, the immunohistochemical study showed the absence of marking of the tumor cells by anti MDM2 antibodies; however, the search for the amplification of the MDM2 gene by FISH showed that there was an amplification concluding in a grade 1 atypical adipose tumor (well-differentiated liposarcoma).
Fig. 3.
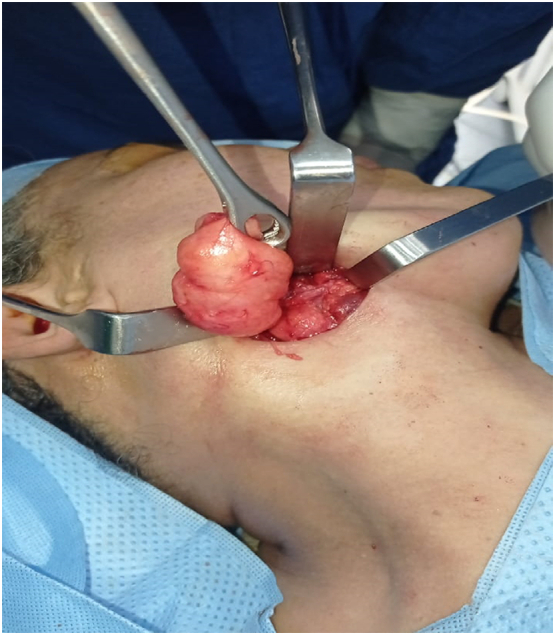
Intraoperative appearance of the tumor.
Fig. 4.

Image of excisional specimen.
After a multidisciplinary consultation with oncologists, and radiologists an adjuvant radiotherapy was decided. The patient was referred to the oncology department. The patient was followed up at the consultation every 3 months for one year, and then every 6 months with no complications, or after-effects or metastases.
3. Discussion
Les Liposarcomas are malignant lipomatous tumors that arise from adipose tissue. There represent 17% to 30% of soft tissue sarcomas, and are the most common entity. Most liposarcomas arise in the deep tissues of the extremities and retroperitoneum. Their prevalence in the head, and neck region represents only 2–9% of all malignant mesenchymal tumors [6,7]. In the oral and maxillofacial area, the sites of predilection of liposarcoma in order of frequency are respectively, the buccal mucosa, the tongue, the parotid and the mandibular soft tissue location [17]. Cases on the floor of the mouth and palate are also reported [19].
These tumors occur in adults with a slight male predominance depending on the literature, in people aged 51–64 years [8]. The neck is most frequently affected and the localization in the face is rarer. This tumor presents clinically as a firm mass relatively fixed to the surrounding tissues, of relatively progressive growth. In general, patients do not have lymph nodes or distant metastases at the time of diagnosis [6].
Imaging (ultrasound, CT scan, and MRI) is essential for a good characterization of the tumor, its adipocytic nature, its location, size, limits, extension to the surrounding tissues, and its relationship with the neurovascular structures as well as for the detection of metastases [9].
It should be noted that certain MRI features can distinguish liposarcoma from lipoma. These are, the presence of thickened septa greater than 2 mm, nodular and/or globular areas of nonadipose tissue within the lesion or associated with the mass, and a total amount of non-adipose tissue comprising more than 25% of the lesion [19].
In histology, we distinguish four subtypes of liposarcoma: atypical lipomatous, tumor/well differentiated liposarcoma (ALT/WDLPS), myxoid liposarcoma (MLPS), pleomorphic liposarcoma (PLPS) de-differentiated liposarcoma (DDLPS) [9,10].
Well-differentiated liposarcoma is the most common entity of all head and neck sarcomas and accounts for 30–40% of liposarcomas. It is locally aggressive and may recur if excision was not complete with a very low tendency to metastasis [9].
Conventional histology and immunohistochemistry remain the basic tools for the diagnosis and classification of sarcomas. However, molecular biology can enrich the pathologist's analysis: the identification of a specific molecular anomaly can confirm the diagnosis, rule out a differential diagnosis, and sometimes provide prognostic information [5]. It is now well established that atypical lipomatous tumor/well differentiated liposarcoma and dedifferentiated liposarcomas are characterized in cytogenetics by MDM2 and CDK4 amplification. Therefore, the search for MDM2 and CDK4 expression by immunohistochemistry and the amplification of these two genes by FISH are essential tools for this diagnosis [9,11,12].
Histopathologically, differential diagnoses must be made with intramuscular myxoma, spindle cell or pleomorphic lipoma, lipogranuloma and glioblastoma [19].
Not performing an immunohistochemical study initially in our patient case was responsible for a misdiagnosis. This is justified by the fact that it is not systematically performed in cases of benign tumors. The occurrence of local recurrence motivated us to perform this study.
Some authors advocate fine-needle aspiration biopsy as an aid to diagnosis in deep locations [18].
Solitary lipoma does not degenerate and atypical lipomatous tumor/well-differentiated liposarcoma in no case from the degeneration of a lipoma [13,14]. Although the excision was not enlarged at the previous excision, the recurrence was explained by immunohistochemistry.
Despite its proximity to the noble structures of the head and neck, the basic treatment is surgical excision. It must be carcinologic, consisting of a wide, monobloc resection in healthy margins. Complete excision is generally sufficient to cure low-grade tumors (well-differentiated and myxoid) [8,10,15].
For our patient, the fact that there was histological evidence of lipoma for the previous surgery and the presence of an encapsulated mass did not allow a wide excision or an extemporaneous examination. Similarly, a second-stage revision to complete the resection was not considered necessary in view of the benefit/risk balance.
Surgery in this region of the cheek may expose to complications due to the risk of injury to the buccal branch of the facial nerve or the parotid canal but also to aesthetic sequelae due to the scarring of the approach.
The use of postoperative radiotherapy should be considered in patients with high-grade tumors, large size >5 cm in their largest dimension, deep location, or in the presence of positive margins [6]–[8,14,16].
In the case of this patient the option of radiotherapy was justified because of recurrence and the absence of safety margins. However, there is no scientific evidence to date on the usefulness of chemotherapy or radiotherapy on liposarcoma [18].
The most important factor in terms of prognosis is the histological grade. Other factors that may influence the prognosis of liposarcoma are tumor size, location, spread to regional lymph nodes, and distant metastases.
The prognosis is relatively favorable in liposarcomas of the scalp and face. This can be explained by their location in a region that remains accessible to clinical examination and allows early detection of these tumors at a stage that gives a better chance for surgical treatment [8,10].
Liposarcoma of the maxillofacial region has a better prognosis compared to other parts of the human body. To date, no cases of metastasis have been reported for any subtype or histological grade. Most cases of recurrence are associated with the type of well-differentiated liposarcoma with an average size of 5 cm [17].
The prognosis also depended on the treatment modality, patients receiving the only radiotherapy had significantly worse outcomes than patients who received surgical resection or surgery plus adjuvant radiotherapy [7].
4. Conclusion
The distinction between a lipoma or its variants and an atypical lipomatous tumor (TLA)/liposarcoma can be much more complex. When morphological features are insufficient, immunohistochemistry and/or molecular biology can be of great help but remain non-specific in the identification of liposarcoma. Currently, the cytogenetic study is becoming a crucial means for the diagnosis and even for the determination of the histological type of these tumors and thus for a better management.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Funding
The authors declared that this study has received no financial support.
Author contribution
Salissou IRO: Corresponding author writing the paper
Amina MAADANE: writing the paper
Fatema Ez-zahrae Azami Hassani: writing the paper
Mohamed Raiteb: writing the paper
Ouassime Kerdoud: writing the paper
Faiçal SLIMANI: Correction of the paper
Registration of research studies
-
1.
Name of the registry: researchregistry
-
2.
Unique identifying number or registration ID: 6836
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked):
Guarantor
Salissou IRO.
Declaration of competing interest
Authors of this article have no conflict or competing interests. All of the authors approved the final version of the manuscript.
References
- 1.Agha R.A. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 2.Honoré C., Méeus P., Stoeckle E., Bonvalot S. Le sarcome des tissus mous en France en 2015: épidémiologie, classification et structuration de la prise en charge ଝ. J. Chir. (Paris) 2015;152(4):224–232. [Google Scholar]
- 3.Nouri H., Hassani R., Aderdour L., Raji A. Liposarcome bien différencié de l’hypopharynx. Ann. Fr. d’Oto-Rhino-Laryngologie Pathol. Cervico-Faciale. 2011;128(3):162–164. [Google Scholar]
- 4.De Bree E. 2014. Lipomatous Tumours of the Head and Neck: A Spectrum of Biological Behaviour. [DOI] [PubMed] [Google Scholar]
- 5.Chetaille B., Laibe S. Apport des analyses moléculaires à la classification anatomopathologique des sarcomes. Oncologie. 2012;14(9):538–542. [Google Scholar]
- 6.Khamassi K. vol. 37. 2010. Head and Neck Liposarcomas a 32 Years Experience; pp. 347–351. [DOI] [PubMed] [Google Scholar]
- 7.Gerry D., Fox N.F., Spruill L.S., Lentsch E.J. no. March. 2014. Liposarcoma of the Head and Neck: Analysis of 318 Cases With Comparison to Non–head and Neck Sites Study Population; pp. 393–400. [DOI] [PubMed] [Google Scholar]
- 8.Davis E.C. no. January. 2009. Original Article Liposarcoma of the Head and Neck: The University of Texas M. D. Anderson Cancer Center Experience; pp. 28–36. [DOI] [PubMed] [Google Scholar]
- 9.Barisella M., Giannini L., Piazza C. vol. 28, no. 2. 2020. From Head and Neck Lipoma to Liposarcoma: A Wide Spectrum of Differential Diagnoses and Their Therapeutic Implications; pp. 136–143. [DOI] [PubMed] [Google Scholar]
- 10.Golledge J., Fisher C., Rhys-Evans P.H. Head and neck liposarcoma. Cancer. 1995;76(6):1051–1058. doi: 10.1002/1097-0142(19950915)76:6<1051::aid-cncr2820760620>3.0.co;2-4. Sep. [DOI] [PubMed] [Google Scholar]
- 11.Karanian M., Coindre J. Quatrième édition de la classification OMS des tumeurs des tissus mous fourth edition of WHO classification tumours of soft tissue. Ann. Pathol. 2014;35(1):71–85. doi: 10.1016/j.annpat.2014.11.003. [DOI] [PubMed] [Google Scholar]
- 12.Subtypes D.L., Aurias A., Hostein I., Coindre J.M. 2005. MDM2 and CDK4 Immunostainings Are Useful; pp. 1340–1347. [DOI] [PubMed] [Google Scholar]
- 13.“liposarcoma of the cheek.pdf.”.
- 14.Fouque O. Stratégie diagnostique devant une tumeur graisseuse des tissus mous de l’adulte. J. d’imagerie diagnostique Interv. 2018;1(4):265–283. [Google Scholar]
- 15.de Bree R. Prognostic factors in adult soft tissue sarcomas of the head and neck: a single-centre experience. Oral Oncol. 2006;42(7):703–709. doi: 10.1016/j.oraloncology.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 16.Garrel R. Sarcomes des tissus mous de la tête et du cou de l' adulte. Ann. françaises doto-rhino-laryngologie Pathol. cervico-faciale. 2016;133(1):34–39. [Google Scholar]
- 17.Fanburg-Smith J.C., Furlong M.A., Childers E.L. Liposarcoma of the oral and salivary gland region: a clinicopathologic study of 18 cases with emphasis on specific sites, morphologic subtypes, and clinical outcome. Mod. Pathol. 2002;15(10):1020–1031. doi: 10.1097/01.MP.0000027625.79334.F5. Oct. [DOI] [PubMed] [Google Scholar]
- 18.Cheng J., Yu H., Wang L., Wang X., Shen G. Primary oral and maxillofacial liposarcoma: a clinicopathological and immunohistochemical study of eleven cases. Arch. Med. Sci. 2012;8(2):316–323. doi: 10.5114/aoms.2012.28560. May 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim Y.B., Leem D.H., Baek J.A., Ko S.O. Atypical lipomatous tumor/well-differentiated liposarcoma of the gingiva: a case report and review of literature. J. Oral Maxillofac. Surg. 2014;72(2):431–439. doi: 10.1016/j.joms.2013.06.222. Feb. [DOI] [PubMed] [Google Scholar]



