Abstract
Background
Beliefs about gender roles and high-risk sexual behaviours underlie the human immunodeficiency virus (HIV) epidemic in South Africa. Yet, there is limited information on the relationships between beliefs about gender roles and risky sexual behaviours. Few studies have explored the association between beliefs about gender roles, high risk sexual behaviour, and health-seeking behaviour among men.
Methods
We investigated associations between gender beliefs (dichotomised as traditional or progressive) and high-risk sexual behaviour among South African men presenting for medical male circumcision (Apr 2014 to Nov 2015).
Results
Of 2792 enrolled men, 47.4% reported traditional gender beliefs. Participant ages ranged between 18–46 years (median age 26 years; interquartile range, 21–31 years). Most participants had at least one sex partner over the last 12 months (68.2%). Younger men (18–24 years old vs. 25–46 years old) (odds ratio [OR], 1.5 [95% confidence interval (CI) 1.0–2.0]), those with multiple partners ([OR], 1.5 (CI) 1.3–1.8]) and participants unsure of their last partner’s HIV status (OR, 1.4 [95% CI 1.1–1.7]) were more likely to have traditional beliefs on gender roles.
Conclusion
Young men with traditional beliefs on gender roles may be more likely to engage in high-risk sexual behaviour and could be good candidates for HIV prevention programmes. N = 206 (max 350)
Trial registration Name of registry: Clinicaltrials.gov; Trial registration number: NCT02352961; Date of registration: 30 January 2015 “Retrospectively registered”; URL of trial registry record: https://www.clinicaltrials.gov/
Keywords: HIV risk, Men, Beliefs about gender roles, South Africa, Circumcision
Introduction
Beliefs about gender roles and high risk sexual behaviours may underlie the human immunodeficiency virus (HIV) epidemic in South Africa [1–7]. Beliefs about gender roles are dynamic, context-specific [7–11], socially constructed [7, 12] and influence how men interact with their sexual partners. Traditional roles of men are characterized by the beliefs that men are the primary bread-winners [13] and superior to women [13, 14]. Progressive beliefs about gender roles are in support of gender equality [13] and promote participation in HIV prevention for individuals and families [15]. Yet there is limited information on the relationships between beliefs about gender roles and risky sexual behaviours.
According to the 2017 South African national survey, black South African men aged 45–49 years had higher HIV risk [16] than women in the same age group. Men also had lower HIV treatment coverage (41%) than women (52%) and accounted for 58% of AIDS-related deaths [2]. Sexual behaviours that increase HIV risk among men include independent or impulsive sexual decision-making [6, 7, 10, 11, 17, 18], refusal to test for HIV [19, 20], not knowing or denial of partner HIV status [21], inconsistent condom use [22, 23], and having multiple sexual partners [15, 22–27]. Yet few studies have explored the association between beliefs about gender roles, high risk sexual behaviour, and health-seeking behaviour among men.
Medical male circumcision (MMC) reduces the risk of heterosexual transmission of HIV [28]. However, uptake of HIV prevention interventions, including MMC, remains low [29, 30]. The UNAIDS 2017 report showed that 37% of adult men in South Africa are living with HIV [31], and the South African national survey indicated that only 31.8% men aged 15–64 years were circumcised [32]. These statistics highlight the need to identify men at high risk for HIV and involve them in HIV prevention activities, such as MMC.
To help identify men at high risk of HIV, we used a scale on gender roles to determine whether traditional beliefs are associated with high risk sexual behaviour among South African men.
Methods
Description of the study area
The parent study that collected the data for this analysis was conducted at a health clinic in Ekurhuleni North, a peri-urban area in Gauteng Province, South Africa. The clinic provides services to adolescent and adult men. Routine sexual health services include HIV counselling and testing, provision of condoms, screening for sexually transmitted infections (STIs), linkage to treatment for HIV or STIs, and MMC.
Parent study
Retrospective data for this analysis were derived from parent study Imbizo (which is the IsiZulu word for traditional forums where elders discuss important issues with the community. IsiZulu is a language spoken in South Africa) [33], which developed and evaluated an intervention to increase demand for circumcision among HIV-uninfected men aged 25–49 years. During enrolment of the Imbizo study, quantitative behavioural risk data during were collected from participants. In phase one (April 1–September 30, 2014), we identified characteristics of men presenting for MMC. In phase two (June 22–November 30, 2015) we implemented an intervention strategy and determined whether this intervention increased the number of men (aged ≥ 25 years) presenting for MMC at the clinic. The intervention included infrastructure changes that physically separated adult from adolescent males inside the facility, an exclusive health club, adult-specific community awareness materials, and community discussions [33]. Details and outcomes of the intervention are described elsewhere [33]. For this report, we analysed data from all men aged 18–49 years who enrolled during both phases.
Enrolment procedures
For this analysis, we used cross-sectional data from the parent study first visit. We analysed data from the structured behavioural risk questionnaires that were administered during enrolment. Eligibility criteria for our analysis included age 18–49 years at enrolment, enrolment in the parent study, eligible for circumcision at screening, and ability to communicate in English, IsiZulu, or Sepedi. Following informed consent, trained interviewers administered the structured behavioural risk questionnaire to all participants before the circumcision procedure.
Data collection tools
The beliefs about gender roles Likert scale (Table 1) is an eight-item index with four response options, derived and previously validated from research conducted in South Africa, where the estimate of the internal consistency (Cronbach alpha) of the scale was good [34]. In addition we administered a structured behavioural risk questionnaire that included demographic information (e.g., age, employment, and alcohol or drug use), number of partners in the last 12 months, age at sexual debut, sexual partner history, and condom use at last sex act.
Table 1.
Beliefs about gender roles were measured using an eight-item index with four-level response options
| No | Progressive | Traditional | |||
|---|---|---|---|---|---|
| Strongly Disagree | Disagree | Agree | Strongly agree | ||
| 1 | Men have many lovers because it is in their nature to do so | 1 | 2 | 3 | 4 |
| 2 | Men have lovers to get energy to satisfy their primary partners | 1 | 2 | 3 | 4 |
| 3 | Women these days say that they need to have more than one sex partner | 1 | 2 | 3 | 4 |
| 4 | Men feel ashamed of their wives and want young lovers to take around to their friends | 1 | 2 | 3 | 4 |
| 5 | If men do not have lovers their friends laugh at them | 1 | 2 | 3 | 4 |
| 6 | Women who are financially independent do not want to commit themselves to one relationship | 1 | 2 | 3 | 4 |
| 7 | The families of young people who work do not want them to get married because they are afraid to lose their income | 1 | 2 | 3 | 4 |
| 8 | Men often force women in subtle ways to have sex with them even if they do not want to | 1 | 2 | 3 | 4 |
Statistical analysis
STATA (version 14, StataCorp LP, College Station, TX) was used for the analysis. The main independent variable was beliefs on gender roles. To describe the enrolled sample, we used means (± standard deviations) or medians with associated interquartile ranges (IQR) for continuous variables depending on their distribution. We calculated frequencies and proportions for categorical variables with the Fisher exact test or chi-square test for comparisons. For the bivariate analysis we used the Fisher exact test for cell counts of less than 5. For larger cell counts per variable we used chi-square tests. p-values < 0.05 were considered statistically significant.
Factor analysis and Cronbach alpha measures were used to assess the reliability of the gender beliefs scale. For this scale, we summed responses across all eight items for each respondent and calculated a median score. Distribution of the summed scores were normal, suggesting that most of the beliefs on gender roles scores were within expected ranges. We used the median as an index of how progressive (promoting gender equality) or traditional (promoting male dominance) participants were with respect to gender roles. We generated a binary outcome score for each participant by summing scores from the eight-statements on gender beliefs as as progressive (scores of ≤ 16), or traditional (scores of > 16; scale range, 8–24) [34]. Scores for the progressive and traditional beliefs on gender roles were derived from the eight statements listed in Table 1. The binary score of yes or no as categorised using the cut-off point was used as the outcome variable while socio-demographic characteristics at baseline were used as the explanatory variables. A median score of 16 was used as the cut-off.
Multivariable logistic regression modelling was used to assess the main association of participant age and beliefs about gender roles (traditional versus progressive), adjusting for potential confounders. The outcome for the logistic regression model was traditional beliefs on gender roles. Potential confounders were defined a priori from review of the literature for demographics and behaviours that place men at high risk for HIV. Potential confounders included age, number of partners in the last 12 months, belief that last sexual partner was HIV positive and condom use at last sex act.
Results
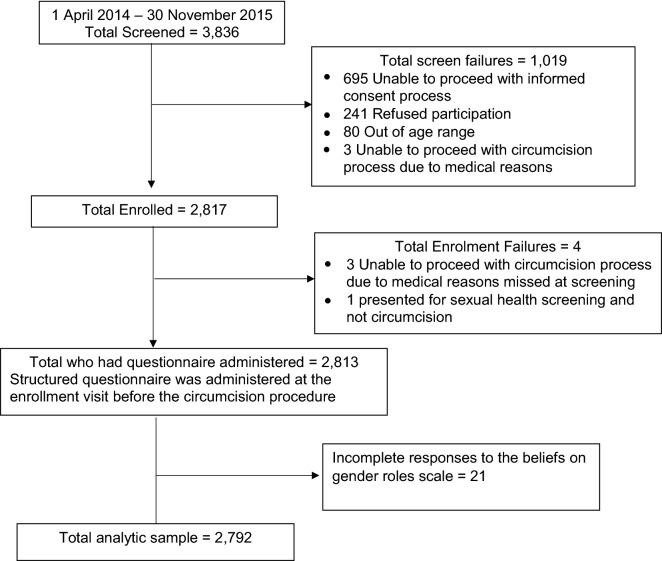
Of the 3836 men screened during the Imbizo, study 1023 screened men were excluded (1019 after screening and 4 after enrolment). More than two-thirds of the screened participants (695 or 67.9%) could not proceed with the informed consent process as they were unable to communicate in any of the three study-supported languages and could not understand the consent form, 241 (23.6%) refused participation, 80 (7.8%) were out of the age range, 6 (0.6%) could not proceed with circumcision process due to medical reasons while one participant (0.1%) only attended the clinic for sexual health screening and not circumcision. The structured questionnaire was administered to 2813 (73.3%) eligible participants. For this analysis, 21 participant records were excluded due to incomplete information on the beliefs of gender roles scale. A total of 2792 participant records were used for this analysis (Fig. 1). The structured behavioural risk questionnaires took approximately 30 min to complete. Reliability for the scale on beliefs about gender roles was 0.6 (Cronbach alpha co-efficient). We observed that the 2792 analysed participants differed from the 21 excluded participants in terms of age. The group excluded were slightly older on average but no other significant difference was observed. Exclusion was mainly related to not being able to respond to all statements required on the beliefs of gender roles scale. Slightly older people were less likely to be able to complete all questions.
Fig. 1.
Enrolment diagram of men (aged 18–49 years) who accessed circumcision services between 2014 and 2015 in Ekurhuleni North, Gauteng Province, South Africa
The overall median age was 26 years (interquartile range, 21–31 years). A total of 1330 (47.6%) participants had traditional beliefs about gender roles. Most participants were enrolled in phase one (1584; 56.7%), aged 25–34 years old (1173; 42.0%), and had steady employment (1259, 45.1%). A high proportion of participants reported a sexual relationship with at least one person over the last 12 months (1903; 68.2%); reported sexual debut at age ≤ 17 years (1579; 56.6%); did not believe that their last partner was HIV positive (2023; 72.4%); and whose last sex partner was ≥ 5 years older than the participant or the same age (1970; 70.6%) when the questionnaire was administered. Refer to Table 2.
Table 2.
Sample characteristics and HIV risk behaviour at baseline and associations with beliefs about gender roles among men aged 18 to 49 years old (n = 2792) (2014–2015)
| Beliefs about gender roles | |||
|---|---|---|---|
| Progressive (n = 1462) | Traditional (n = 1330) | p-value | |
| n (%) | n (%) | ||
| Phase of enrolment | |||
| Phase 1 (1 Apr–30 Sep 2014) | 800 (50.5) | 784 (49.5) | 0.02 |
| Phase 2 (22 Jun–30 Nov 2015) | 662 (54.8) | 546 (45.2) | |
| Age | |||
| 18–24 years | 600 (49.6) | 609 (50.4) | 0.02 |
| 25–39 years | 757 (53.9) | 647 (46.1) | |
| ≥ 40 years | 105 (58.7) | 74 (41.3) | |
| Employment status | |||
| Student | 290 (53.8) | 249 (46.2) | 0.03 |
| Unemployeda | 380 (47.7) | 416 (52.3) | |
| Some employment | 104 (55.9) | 82 (44.1) | |
| Steady employment | 680 (54.0) | 579 (45.9) | |
| Missing | 8 (66.7) | 4 (33.3) | |
| Alcohol use | |||
| Never | 522 (53.3) | 457 (46.7) | 0.31 |
| Occasional (≤ 1 to 3 times a month) | 676 (50.9) | 652 (49.1) | |
| Frequent (Once a week to daily) | 264 (54.4) | 221 (45.6) | |
| Cannabis use | |||
| No | 1198 (52.5) | 1085 (47.5) | 0.19 |
| Yes | 264 (52.2) | 242 (47.8) | |
| Missing | 0 (0.0) | 3 (100.0) | |
| Number of partners in the last 12 months | |||
| 0–1 sexual partner | 1059 (55.7) | 844 (44.4) | |
| > 1 sexual partner | 402 (45.3) | 485 (54.7) | < 0.01 |
| Missing | 1 (50.0) | 1 (50.0) | |
| Age of sexual debut | |||
| ≤ 17 years | 810 (51.3) | 769 (48.7) | 0.77 |
| 18–34 years | 589 (53.6) | 510 (46.4) | |
| Unknown age | 7 (53.9) | 6 (46.2) | |
| Never had sexb | 53 (55.2) | 43 (44.8) | |
| Missing | 3 (60.0) | 2 (40.0) | |
| Believe last partner was HIV positive | |||
| No | 1097 (54.2) | 926 (45.8) | 0.01 |
| Yes | 45 (45.9) | 53 (54.1) | |
| Not surec | 263 (46.2) | 306 (53.8) | |
| Not applicabled | 55 (56.1) | 43 (43.9) | |
| Missing | 2 (50.0) | 2 (50.0) | |
| Age of last sex partner | |||
| > 5 years younger | 387 (53.9) | 331 (46.1) | 0.41 |
| Same age | 981 (51.8) | 914 (48.2) | |
| > 5 years older | 37 (49.3) | 38 (50.7) | |
| Not applicabled | 55 (56.1) | 43 (43.9) | |
| Missing | 0 (0.0) | 2 (100.0) | |
| Condom use at last sex | |||
| No | 727 (53.5) | 632 (46.5) | 0.06 |
| Yes | 680 (51.1) | 650 (48.9) | |
| Missing | 0 (0.0) | 3 (100.0) | |
Row percentages are shown
aIncludes those that reported receiving social grants
bTotal who never had sex is 98. There was 1 missing age and 1 data discrepancy for this variable
cUncertain of partner’s HIV status
dThese participants reported never having sex
Men enrolled in Phase 2 were more likely to have progressive beliefs about gender roles (p = 0.02). Men between 18 to 24 years old (p = 0.02), those with multiple partners (p < 0.01) and unsure of their last partner’s HIV status (p < 0.01) were more likely to have traditional beliefs on gender roles. Beliefs about gender roles were not significantly associated with participant’s age at sexual debut (p = 0.54), age of last sex partner (p = 0.49), or condom use at last sex act (p = 0.35). Although the phase of enrollment seemed relevant in the univariate model, we removed this variable from the multivariable model, as the phase of enrolment was closely correlated with participant age. Condom use at last sex act was not significant (p > 0.05) in the univariate model and was also removed from the multivariable model.
The final multivariable model (Table 3) showed that younger men (18–24 years old) were more likely to have traditional beliefs on gender roles (adjusted odds ratio [aOR], 1.5 [95% confidence interval (CI) 1.0–2.0]; p < 0.01) compared to men who were 40 years and above. Men with multiple partners (aOR, 1.5 (CI) 1.3–1.8]; p < 0.01) were more likely to have traditional beliefs on gender roles compared to men who reported none or only one partner. Those unsure of their last partner’s HIV status (aOR, 1.4 [95% CI 1.1–1.7]; p < 0.01) were more likely to have traditional beliefs on gender roles compared to those who who knew that their last sex partner was not HIV positive. While the aOR for men who knew their last partner was HIV positive was similar, there were few men in this strata and this did not achieve statistical significance.
Table 3.
Logistic regression models of association between traditional beliefs about gender roles and HIV risk behaviour among adult men 18 to 49 years (n = 2783)
| Unadjusted odd ratio (95% CI) | p-value | Adjusted odds ratio (95% CI) | p-value | |
|---|---|---|---|---|
| Phase of enrolment | ||||
| Phase 1 (1 April–30 September 2014) | 1 | |||
| Phase 2 (22 June–30 November 2015) | 0.8 (0.7–0.9) | 0.02 | ||
| Age | ||||
| 18–24 years | 1.4 (1.0–1.9) | 0.02 | 1.5 (1.0–2.0) | 0.01 |
| 25–39 years | 1.2 (0.9–1.7) | 0.23 | 1.2 (0.9–1.6) | |
| ≥ 40 years | 1 | 1 | ||
| Number of partners in the last 12 months | ||||
| 0–1 sexual partner | 1 | 1 | < 0.01 | |
| > 1 sexual partner | 1.5 (1.3–1.8) | < 0.01 | 1.5 (1.3–1.8) | |
| Age of sexual debut | ||||
| ≤ 17 years | 1 | |||
| 18–34 years | 0.9 (0.8–1.1) | 0.24 | ||
| Unknown age | 0.9 (0.3–2.6) | 0.85 | ||
| Never had sexa | 0.9 (0.6–1.3) | 0.45 | ||
| Believe last partner was HIV positive | ||||
| No | 1 | 1 | < 0.01 | |
| Yes | 1.4 (0.9–2.1) | 0.11 | 1.4 (0.9–2.1) | |
| Not sureb | 1.4 (1.1–1.7) | < 0.01 | 1.4 (1.1–1.7) | |
| Not applicablea | 0.9 (0.6–1.4) | 0.71 | 0.9 (0.6–1.4) | |
| Age of last sex partner | ||||
| > 5 years younger | 1 | |||
| Same age | 1.1 (0.9–1.3) | 0.33 | ||
| > 5 years older | 1.2 (0.7–1.9) | 0.45 | ||
| Not applicablea | 0.9 (0.6–1.4) | 0.67 | ||
| Condom use at last sex | ||||
| No | 1 | |||
| Yes | 1.1 (0.9–1.3) | 0.22 | ||
| Not applicablea | 0.9 (0.6–1.4) | 0.61 | ||
Models conducted for non-missing values
aParticipants who never had sex
bUncertain of partner’s HIV status
Discussion
We found that young men with traditional beliefs about gender roles were more likely to report multiple sexual partners and were unsure of their last partner’s HIV status—factors that increase men’s HIV risk. Our findings suggest that MMC demand-creation campaigns and HIV prevention programmes could consider targeting men with traditional beliefs about gender roles who may be more likely to engage in high risk sexual behaviour.
Men aged 25 years and above are at high risk for HIV, yet many do not access HIV prevention services. While societal norms encourage men to have multiple partners [11, 26], this type of behaviour is associated with increased HIV risk [22, 25, 27]. Although our finding of multiple partners being a risk factor to HIV among men with traditional beliefs about gender roles concurs with other studies [15, 22–27], there was no significant association to not using condoms. This is possibly due to self-reporting bias that occurred with the questionnaire was administered. Biological and behavioural surveillance surveys conducted in Cape Town, South Africa, across 3 years (2006, 2008, and 2010), showed that the number of sexual partners reported by men has decreased [23]. Yet, multiple partners remains a driver for HIV infections. In our study, men with traditional beliefs about gender roles were also more likely to be unsure of the HIV status of their last sexual partner. Other studies have reported that when men control the sexual relationship, they often distrust their female sexual partners [7, 35] and deny their partner’s HIV status [21]. It is possible that female partners might not disclose their HIV status to male partners due to fear of discrimination, stigma, gossip, or abandonment [36, 37].
Men aged ≥ 40 years were more likely to have progressive beliefs about gender roles, and we saw a trend of men between the ages of 25–39 years falling between the younger men and the older men in terms of their beliefs. Age and gender role beliefs were also both correlated to the phase of study enrolment. We observed that men enrolled in the second phase of the study tended to be both more progressive and older (25 years and above); recruitment for this second phase put a greater emphasis on older men (25 years and above). The association between more progressive gender beliefs among those in phase two of enrolment may have been due to selection bias. From a societal perspective, it seemed that men who were especially concerned about their health to the point of pursuing MMC at an older age, were somehow also more progressive, forward-thinking, or otherwise different from the norm. This is consistent with diffusion of innovation theory, in which those most likely to try new things (“innovators and early adopters”) are usually a small, different portion of society [38], and from our findings mature men 40 years and above were more likely to have progressive beliefs compared to those who were younger. However, additional studies are needed to interpret this finding. Promoting gender equality behaviours (what we typically recorded as “progressive”), such as taking responsibility to protect partners from HIV [15] and maintaining personal respect [39], could improve health-seeking behaviours among men.
Our study had several limitations. We did not do a formal sample size calculation and our analysis was limited to the available data. Our sample was comprised of only men who participated in the study and were willing to be circumcised at a clinic and was not a random sample of all men from the general population, however we don’t have any reason to believe that these men are different from their demographic and risk behaviour to other men in the community. This study also was conducted in only one sub-district of South Africa, but we believe that it is representative of many other urban settings in South Africa. The internal consistency of the beliefs about gender roles scale in our analysis was modest (Cronbach alpha co-efficient of 0.6) and lower than the household survey that was used to standardise this Likert scale for use in South Africa. One possible reason for the difference in reliability between the studies is that the representative household survey included men and women [34], while our study only included men. Our work is also a cross-sectional study, and with the inherent problems of temporality, we are unable to properly assess whether correlates of gender beliefs are actually causal predictors. Another limitation was possible social desirability bias when responding to questions on sexual behaviour and/or beliefs on gender roles, however many men reported high risk sexual behaviour. Despite these limitations, this study documents the importance of understanding the association of men’s beliefs about gender roles and high risk sexual behaviour.
Our findings suggest that men with traditional beliefs about gender roles, and perhaps with an emphasis on younger (18–24 years old) men, should be targetted for HIV prevention programmes even among a clinic-based sample. Interventions that account for beliefs about gender roles among men who access MMC could help engage men and their partners in HIV prevention programmes and could promote gender equality behaviours.
Conclusions
Our findings suggest that traditional beliefs about gender roles among men could drive the HIV epidemic in South Africa. Past studies have shown that men may change their perceptions on gender roles after circumcision [5, 39]. Future HIV prevention programmes could consider using circumcision clinics to involve men who seek MMC in discussing and developing interventions that promote gender equality. Multi-level interventions should also involve the sexual partners of men who seek MMC and key traditional stakeholders in the community. Awareness could be created in the community by educating men on the long-term negative impact of traditional beliefs about gender roles and associated high risk sexual behaviours. Such interventions could help decrease HIV transmission in South Africa.
Acknowledgements
We would like to acknowledge the University of California, San Francisco (UCSF) International Traineeships in AIDS Prevention Studies (ITAPS) program for providing mentorship to the first author (NIMH, R25MH064). The authors would like to thank all of the participants. We would also like to thank all of the staff at The Aurum Institute Winnie Mandela Male Sexual Health Clinic for ensuring successful implementation of the study.
Abbreviations
- HIV
Human immunodeficiency virus
- MMC
Medical male circumcision
- UNAIDS
The Joint United Nations Programme on HIV/AIDS
- STIs
Sexually transmitted infections
- OR
Odds ratio
- CI
Confidence intervals
- IQR
Interquartile ranges
Authors’ contributions
CMCM, JMG, MHL and SC: Designed the study, conducted the analysis and wrote the first draft of the manuscript. CMCM, MHL and EM: Conducted the data analysis. JMG, EM, MAP, MHL and SC: Reviewed the analysis and draft manuscripts. All authors read and approved the final manuscript.
Funding
This research has been supported by the President’s Emergency Plan for AIDS Relief (PEPFAR) through the US Centers for Disease Control and Prevention (CDC) under the terms of the Cooperative Agreement Number 5U01GH00518. The findings and conclusions in this manuscript are those of the authors and do not necessarily represent the official position of the funding agencies.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Approval was obtained from the University of the Witwatersrand Human Research Ethics Committee (M130711) and the U.S. Centers for Disease Control and Prevention Institutional Review Board (6546) for the parent study and current analysis. Voluntary written informed consent was obtained from all participants, and, in the case of illiterate participants, a thumbprint from the participant was recorded in the presence of a witness to acknowledge understanding and consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Candice M. Chetty-Makkan, Email: cchetty@heroza.org
Jonathan M. Grund, Email: iha3@cdc.gov
Evans Muchiri, Email: EMuchiri@auruminstitute.org.
Matt A. Price, Email: MPrice@iavi.org
Mary H. Latka, Email: mary.latka@gmail.com
Salome Charalambous, Email: SCharalambous@auruminstitute.org.
References
- 1.South African National Department of Health. National Strategic Plan on HIV, STIs and TB 2012-2016.
- 2.HIV/AIDS JUNP on. GLOBAL AIDS UPDATE; 2016. http://unaids.org.
- 3.PEPFAR. South Africa Country Operational Plan 2017 (COP17) Strategic Direction Summary (SDS). Final submission draft 16 March 2017. Vol. 2017. 2017.
- 4.Montgomery ET, Chidanyika A, Chipato T, van der Straten A. Sharing the trousers: gender roles and relationships in an HIV-prevention trial in Zimbabwe. Cult Heal Sex. 2012;14(7):795–810. doi: 10.1080/13691058.2012.697191. [DOI] [PubMed] [Google Scholar]
- 5.Human Science Research Council. The Fifth South African National HIV Prevalence, Incidence, Behaviour and Communication Survey, 2017. 2018;5–8.
- 6.Zeglin RJ. Systematic review to inform HIV risk reduction counseling. Arch Sexual Behav. 2017;44(7):1979–1990. doi: 10.1007/s10508-015-0501-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jacques-Aviñó C, García de Olalla P, González Antelo A, Fernández Quevedo M, Romaní O, Caylà JA. The theory of masculinity in studies on HIV. A systematic review. Glob Public Health. 2018;14(5):1–20. doi: 10.1080/17441692.2018.1493133. [DOI] [PubMed] [Google Scholar]
- 8.Courtenay WH. Constructions of masculinity and their influence on men’s well-being: a theory of gender and health. Soc Sci Med. 2000;50(10):1385–1401. doi: 10.1016/S0277-9536(99)00390-1. [DOI] [PubMed] [Google Scholar]
- 9.Vlassoff C, Moreno CG. Placing gender at the centre of health programming: challenges and limitations. Soc Sci Med. 2002;54(11):1713–1723. doi: 10.1016/S0277-9536(01)00339-2. [DOI] [PubMed] [Google Scholar]
- 10.Baloyi EM. An African view of women as sexual objects as a concern for gender equality: a critical study. Verbum Eccles. 2010;31(1):1–6. doi: 10.4102/ve.v31i1.380. [DOI] [Google Scholar]
- 11.Mswela M. Cultural Practices and HIV in South Africa: A Legal Perspective. Potchefstroom Electronic Law Journal // Potchefstroomse Elektroniese Regsblad. 2009.
- 12.Everitt-Penhale B, Ratele K. Rethinking ‘Traditional Masculinity’ as constructed, multiple, and hegemonic masculinity. S Afr Rev Sociol. 2015;46(2):4–22. doi: 10.1080/21528586.2015.1025826. [DOI] [Google Scholar]
- 13.Calton JM, Heesacker M, Perrin PB. The elusiveness of progressive masculinity: Gender differences in conceptualizations of nontraditional gender roles. J Gend Power. 2014;2(2).
- 14.Wedgwood N. Connell’s theory of masculinity—its origins and influences on the study of gender. J Gend Stud. 2009;18(4):329–339. doi: 10.1080/09589230903260001. [DOI] [Google Scholar]
- 15.Bandali S. Norms and practices within marriage which shape gender roles, HIV/AIDS risk and risk reduction strategies in Cabo Delgado, Mozambique. AIDS Care Psychol Socio-Med Asp AIDS/HIV. 2011;23(9):1171–1176. doi: 10.1080/09540121.2011.554529. [DOI] [PubMed] [Google Scholar]
- 16.Simbayi LC, Zuma K, Zungu N, Moyo S, Marinda E, Jooste S, Mabaso M, Ramlagan S, North A, van Zyl J, Mohlabane N, Dietrich C, Naidoo I and the SABSSM V Team . South African National HIV Prevalence, Incidence, Behaviour and Communication Survey, 2017. Cape Town: HSRC Press; 2019. [Google Scholar]
- 17.Kaufman MR, Shefer T, Crawford M, Simbayi LC, Kalichman SC, Kaufman MR, et al. Gender attitudes, sexual power, HIV risk : a model for understanding HIV risk behavior of South African men. AIDS Care. 2008;20:434–441. doi: 10.1080/09540120701867057. [DOI] [PubMed] [Google Scholar]
- 18.Mtenga SM, Pfeiffer C, Tanner M, Geubbels E, Merten S. Linking gender, extramarital affairs, and HIV: a mixed methods study oncontextual determinants of extramarital affairs in rural Tanzania. AIDS Res Ther. 2018;15(1):1–17. doi: 10.1186/s12981-018-0199-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nanda G, Dal Santo L, Konde JN, de Negri B. Barriers to achieving the first 90%: gender norms and HIV testing among men in the Democratic Republic of the Congo. AIDS Care Psychol Socio-Med Asp AIDS/HIV. 2018;30(10):1231–1238. doi: 10.1080/09540121.2018.1489100. [DOI] [PubMed] [Google Scholar]
- 20.Sileo KM, Fielding-Miller R, Dworkin SL, Fleming PJ. What role do masculine norms play in men’s HIV testing in sub-Saharan Africa?: a scoping review. AIDS Behav. 2018 doi: 10.1007/s10461-018-2160-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moodley Y. The impact of an unknown HIV serostatus on inpatient mortality. Pan Afr Med J. 2017;28:1–7. doi: 10.11604/pamj.2017.28.285.11860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shisana O, Rehle T, Simbayi L, Zuma K, Jooste S, Zungu N, et al. South African National HIV Prevalence, Incidence and Behaviour Survey, 2012. 2014. [DOI] [PubMed]
- 23.Townsend L, Zembe Y, Mathews C. HIV prevalence and risk behaviours from three consecutive surveys among men who have multiple female sexual partners in Cape Town. AIDS Behav. 2013;17(7):2367–2375. doi: 10.1007/s10461-012-0264-4. [DOI] [PubMed] [Google Scholar]
- 24.Schensul JJ, Radda KE, Corbeil C. Sexual culture in low-income older adult housing: norms, behaviours and risks. Cult Heal Sex. 2018;1058:1–15. doi: 10.1080/13691058.2018.1472809. [DOI] [PubMed] [Google Scholar]
- 25.Kenyon CR, Tsoumanis A, Schwartz IS, Maughan-Brown B. Partner concurrency and HIV infection risk in South Africa. Int J Infect Dis. 2016;45:81–87. doi: 10.1016/j.ijid.2016.03.001. [DOI] [PubMed] [Google Scholar]
- 26.Strebel A, Crawford M, Shefer T, Cloete A, Dwadwa-Henda N, Kaufman M, et al. Social constructions of gender roles, gender-based violence and HIV/AIDS in two communities of the Western Cape, South Africa. SAHARA-J J Soc Asp HIV/AIDS. 2006;3(3):516–528. doi: 10.1080/17290376.2006.9724879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gaffoor Z, Wand H, Street RA, Abbai N, Ramjee G. Predictors of perceived male partner concurrency among women at risk for HIV and STI acquisition in Durban. South Africa AIDS Res Ther. 2016;13(1):1–11. doi: 10.1186/s12981-015-0086-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, Sitta R, Puren A. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 trial. PLoS Med. 2005;2(11):1112–1122. doi: 10.1371/journal.pmed.0020298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.WHO . Progress in scaling up voluntary medical male circumcision for HIV prevention in East and Southern Africa Progress in scaling up voluntary medical male circumcision for HIV prevention in East and Southern Africa. Geneva: WHO; 2012. [Google Scholar]
- 30.WHO . Progress in scaling up voluntary medical male circumcision for HIV prevention in East and Southern Africa Progress in scaling up voluntary medical male circumcision for HIV prevention in East and Southern Africa, 2017–8. Geneva: World Health Organisaiton; 2018. [Google Scholar]
- 31.United Nations programme for HIV/AIDS. A snapshot of men and HIV in South africa- unaids. Joint United Nations Programme for HIV/AIDS; 2017. http://www.unaids.org/en/file/111992/download?token=HCocZ_Hh.
- 32.HSRC. Hiv impact assessment summary July 2018 the Fifth South African National Hiv prevalence, incidence , behaviour and communication survey, 2017. 2018;2017(July):5–8.
- 33.Grund JM, Chetty-Makkan CM, Ginindza S, Munyai R, Kisbey-Green H, Maraisane M, et al. Effectiveness of an “Exclusive Intervention Strategy” to increase medical male circumcision uptake among men aged 25–49 years in South Africa. BMC Public Health. 2018;18(1):868. doi: 10.1186/s12889-018-5729-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Geeta Nanda. Compendium of Gender Scales. Washington DC: FHI 360/C-Change; 2011.
- 35.Fleming PJ, Barrington C. Masculinity and HIV: Dimensions of masculine norms that contribute to men’s HIV-related sexual behaviours. AIDS Behav. 2016;20:788–798. doi: 10.1007/s10461-015-1264-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Arrey AE, Bilsen J, Lacor P, Deschepper R. “It’s my secret”: Fear of disclosure among sub-Saharan African migrant women living with HIV/AIDS in Belgium. PLoS ONE. 2015;10(3):1–22. doi: 10.1371/journal.pone.0119653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Obermeyer CM, Baijal P, Pegurri E. Facilitating HIV disclosure across diverse settings: a review. Am J Public Health. 2011;101(6):1011–1023. doi: 10.2105/AJPH.2010.300102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sanson-fisher RW. Diffusion of innovation theory for clinical change. MJA. 2004;180(March):55–56. doi: 10.5694/j.1326-5377.2004.tb05947.x. [DOI] [PubMed] [Google Scholar]
- 39.Grund JM, Hennink MM. A qualitative study of sexual behavior change and risk compensation following adult male circumcision in urban Swaziland. AIDS Care Psychol Socio-Med Asp AIDS/HIV. 2012;24(2):245–251. doi: 10.1080/09540121.2011.596516. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.