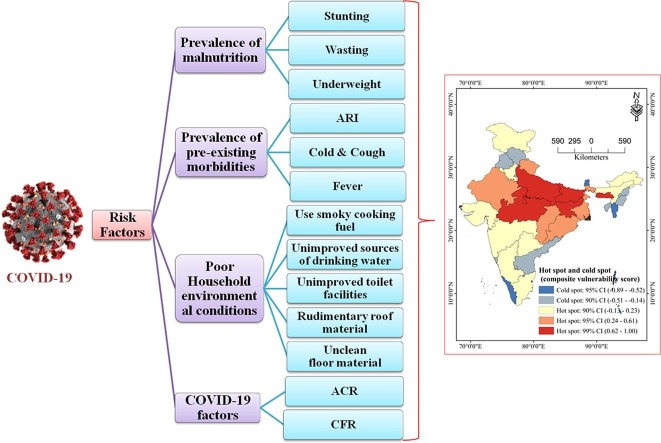
Graphical abstract
Keywords: Malnutrition, Morbidity, CFR, ACR, Risk factor, Hot spot, Under-five children, COVID-19, India
Abstract
Background
The novel Coronavirus disease 2019 (2019-nCoV) outbreak, caused by severe acute respiratory syndrome Coronavirus-2 (SARS-CoV-2), has become the worst serious global risk to humanity in the last century and linked with various risk factors.
Objective
To find out the risk zone associated with Coronavirus disease among children under-five age using malnourished status, pre-existing morbidity conditions, poor household environmental conditions, and also with case fatality rate (CFR) and active case rate (ACR) of COVID-19 in India.
Data sources & methods
Data was collected from the 4th round of the National Family Health Survey (NFHS)-4, 2015–16, and CFR and ACR of COVID-19 related data collected from the Ministry of Health and Family Welfare (MoHFW) on 18th May 2020. Mean, standard deviation, and Z-score statistical methods have been employed to identify the risk factors zone and Hot Spot analysis (Getis-Ord Gi) has been done.
Results
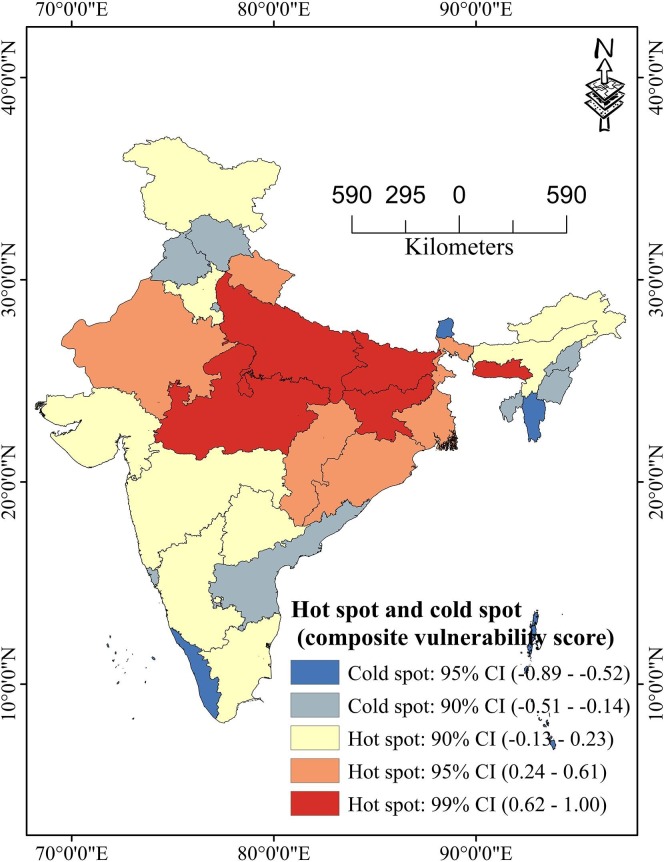
The states and union territories (UTs) which have a high composite vulnerability score (CVS) of COVID-19 among under-five children are in Meghalaya (CVS = 1), Uttar Pradesh (CVS = 0.93), Jharkhand (CVS = 0.86), Bihar (CVS = 0.74), Madhya Pradesh (CVS = 0.74), and Odisha (CVS = 0.55). The states and UTs which have low composite vulnerability score of COVID-19 among under-five children are in Sikkim (CVS = -0.90), Daman & Diu (CVS = -0.76) Lakshadweep (CVS = -0.74), Kerala (CVS = -0.72), Chandigarh (CVS = -0.71). The COVID-19 high-risk zones (hot spot: 99% Confidence interval [CI]) were observed in Madhya Pradesh, Uttar Pradesh, Jharkhand, Bihar, and Meghalaya states of India, which are spatially high clustered and the low-risk zones (cold spot: 95% CI) were observed in Kerala, Mizoram states of India.
Conclusions
Well-built public health measures, including rapidly searching in high focus areas and testing of COVID-19, should be performed in vulnerable regions of COVID-19.
1. Introduction
Globally, at least 1 in 3 under-five children are not growing well due to malnutrition in its more visible forms, i.e. stunting, wasting, underweight, and overweight (UNICEF, 2019a). UNICEF estimated that nearly 2.6 million children, who die each year due to malnutrition, are equivalent to one-third of all registered child deaths globally (UN, 2011). The United Nations International Children's Emergency Fund (UNICEF) has recently published a report on ‘The State of the World’s Children 2019' highlighting the state of children’s health in India and around the world. As per the report, 35%, 17%, 33%, and 2% of children are suffering from stunting, wasting, underweight, and overweight respectively in India (UNICEF, 2019a).
Adequate access to proper health services, safe drinking water supplies, adequate sanitation, and good housing are preconditions for adequate nutrition among under-five children. Inadequate sanitation, unhygiene environment, inappropriate childcare, and poor household environment conditions also directly influence the under-five children’s malnutrition and morbidities (Linnemayr et al., 2008; Masibo, 2013; Poda et al., 2017; Mshida et al., 2018). The most important disease for the cause of the morbidity are acute respiratory infections (ARIs), cold & cough, and fever, etc (Ramani et al., 2016; Rehman and Ishaq, 2018). The acute respiratory infection (ARI) i.e. short and rapid breaths, cold & cough, and fever among human beings are the primary symptoms of Coronavirus disease (Saha & Chouhan, 2020, Cascella et al., 2020) and severe acute respiratory syndrome Coronavirus-2 (SARS-CoV-2) which have widespread effects because it is hazardous or risk factor for under-five children health having a weak immune system (Chan et al., 2020; Jin et al., 2020; Lai et al., 2020; Peeri et al., 2020; Saha & Chouhan, 2020; Singhai, 2020; Velavan and Meyer, 2020). The prevalence of morbidity was found among those under-five children who are malnourished, living in over-crowded and poorly ventilated houses, and those children's families are use unimproved toilet facilities. Several socio-demographics, nutritional, health, and environmental conditions are associated directly and indirectly with the occurrence of disease among under-five children. Household environmental conditions include drinking water quality, sanitation condition, and household dwelling characteristics (Godana and Mengiste, 2013; Mihrete et al., 2014; Adane et al., 2017; Nsabimana et al., 2017; Getachew et al., 2018; Zedie & Kassa, 2018; Workie et al., 2019; Vijayan and Ramanathan, 2020; Abuzerr et al., 2020).
The novel Coronavirus disease 2019 (2019-nCoV) outbreak, epi-centered in Wuhan city, Hubei Province of the People's Republic of China on December 8, 2019 (Saha & Chouhan, 2021), caused by severe acute respiratory syndrome Coronavirus-2 (SARS-CoV-2), has become the worst serious global risk to humanity in the last century (Saha et al., 2020). Pointing to over 118,000 confirmed COVID-19 cases in over 110 countries and territories around the world and the continued threat of further global transmission, the World Health Organization (WHO) declared COVID-19 a pandemic on 11th March 2020 (Saha et al., 2020) and asked all countries to get imperative and aggressive steps against this community health disaster. Globally, as of 31st July 2020, a total of 17,113,205 confirmed cases of Coronavirus disease, including 663,667 deaths have been reported and 216 countries and territories have been affected by the COVID-19 pandemic (WHO, 2020). As of 31 July 2020 as of 08:00 IST (GMT + 5:30), the Ministry of Health and Family Welfare, the Government of India reported, a total of 1,638,870 confirmed cases, and 35,747 deaths have been reported spreaded over 35 states and UTs of India (MoHFW, 2020). Currently, as of July 2020, no vaccine or medicine for COVID-19, prevention of infection is the only tool available, and this is dependent on home isolation, social distancing, mask-wearing, constant hand washing, increasing consciousness, and human being resistance against infection i.e. boost of individual immunity level. Globally, and also in developing countries like India, the under-five children are most vulnerable groups compared to the other age classes, so we considered only the under-five age group and in 2018 an estimated 5.3 million children were died under the age of five years (UNICEF, 2019b), mostly from preventable childhood morbidities. For that very rationale, under-five children with these pre-existing symptoms and areas with poor household environmental conditions are aggravate susceptibility to COVID-19 deaths in the coming days.
This type of study is yet not done, so considering this huge research gap this study also aims to determine the impact of malnutrition and pre-existing morbidities, and poor household environmental conditions aggravate susceptibility to Coronavirus disease among under-five children in the states and UTs of India. So, this very research would be helpful for policymakers, strategy developers, and public health workers to combat and reduce the future pandemic situation.
2. Data & methods
2.1. Data sources
For this study, data was collected from the fourth round of the National Family Health Survey, 2015–16, consisting of nationally representative sample surveys. The purpose of this survey was to gather essential information on family planning, fertility, maternal and child health, under-five nutrition, anemia, infant, child, and maternal mortality indicators, other adult health issues HIV/AIDS-related knowledge, attitudes, and behavior, domestic violence (IIPS & ICF, 2017). A total of 247,743 living children (0–59 months) were utilized from the NFHS-4 in India from different pre-existing morbidities, nutritional status, and environmental characteristics of under-five children. The data used in this study were retrieved from the public domain.
Data on the COVID-19 is collected from the https://www.mohfw.gov.in/ naming ‘COVD-19 state-wise status’, provides the most updated figures on the daily and a total number of confirmed cases, recovered or cured cases, and deaths (MoHFW, 2020) for each affected states and union territories of India. This data was collected from the Ministry of Health and Family Welfare (MoHFW), Government of India website. We have collected data on confirmed cases, the number of death cases, and cured cases as of July 14, 2020, 08:00 IST (GMT + 5:30) of affected states and UTs of India.
2.2. Variables used
For the investigation of the study, pre-existing childhood morbidities, malnutrition status, and poor household environmental conditions among under-five children, and COVID-19 related indicators were included. The prevalence of pre-existing morbidities indicators includes the percentage of children who had symptoms of acute respiratory infection in the last two weeks before the survey, the percentage of children who had cold & cough, and percentage of children who had fever in the last two weeks preceding the survey among under-five children. The nutritional status (based on WHO Multicentre Growth Reference Study of the under-five children) indicators include stunting (children whose height-for-age Z-score is below minus two standard deviations (-2 SD) from the median of the reference population), wasting (children whose weight-for-height Z-score is below minus two standard deviations (-2 SD) from the median of the reference population), and underweight (children whose weight-for-age Z score is below minus two standard deviations (-2 SD) from the median of the reference population) of the states and UTs of India (De Onis et al., 2004). The COVID-19 factors are active case rate and case fatality rate (Table 1 ).
Table 1.
Dimension with their indicators and source of data.
| Dimension | Indicators code | Indicators | Details | Source |
|---|---|---|---|---|
| Prevalence of malnutrition | V1 | Stunting | Children whose height-for-age Z-score is below minus two standard deviations (-2 SD) from the median of the reference population are considered short for their age (stunted), or chronically undernourished. | National Family and Health Survey, 2015-16 (NFHS-4), International Institute for Population Studies (IIPS), Mumbai (IIPS & ICF, 2017). |
| V2 | Wasting | Children whose weight-for-height Z-score is below minus two standard deviations (-2 SD) from the median of the reference population are considered thin (wasted), or acutely undernourished. | ||
| V3 | Underweight | Children whose weight-for-age Z-score is below minus two standard deviations (-2 SD) from the median of the reference population are classified as underweight. | ||
| Prevalence of pre-existing morbidities | V4 | Acute Respiratory Infection (ARI) | Percentage of children had ARI in the last two weeks preceding the survey. | |
| V5 | Cold & Cough | Percentages of children had cold & cough in last two weeks preceding the survey. | ||
| V6 | Fever | Percentage of children who had a fever in the last two weeks preceding the survey. | ||
| Poor household environmental conditions | V7 | Use smoky cooking fuel | Percentage of children's families use smoky cooking fuel or solid biomass. | |
| V8 | Unimproved sources of drinking water | Percentage of children's families use unimproved sources of drinking water. | ||
| V9 | Unimproved toilet facilities | Percentage of children families use unimproved toilet facilities. | ||
| V10 | Rudimentary roof material | Percentage of children families use rudimentary roof material. | ||
| V11 | Unclean floor material | Percentage of children families use unclean floor material. | ||
| COVID-19 factors | V12 | Active Case Rate (ACR) | ACR is calculated as the rate of the total figure of active cases of COVID-19 to the total figure of confirmed cases of COVID-19. | The Ministry of Health and Family Welfare (MoHFW), Government of India, New Delhi (MoHFW, 2020). |
| V13 | Case Fatality Rate (CFR) | CRF is calculated as the rate of the total figure of deaths due to COVD-19 to the total figure of confirmed cases of COVID-19. |
Child’s poor household environmental conditions include smoky cooking fuel (solid fuel for cooking, with virtually all being wood or dung cakes), unimproved sources of drinking water (unimproved [Unprotected (dug) well; unprotected spring, the cart with small tank or drum; tanker truck-provided water, surface water (river, dam, lake, pond, stream, canal, irrigation channel); bottled water (IIPS & ICF, 2017)]), unimproved toilet facilities (Flush or pour-flush to elsewhere, - Pit latrine without a slab or open pit, - Bucket, hanging toilet or hanging latrine and - No facilities or bush or field (open defecation) (IIPS & ICF, 2017)]), rudimentary roof material, and unclean floor material (Table 1).
2.3. Methods
The prevalence of malnutrition (stunting, wasting, and underweight), the prevalence of pre-existing childhood morbidities (ARI, cold & cough, and fever), percentage of children family use smoky cooking fuel or solid biomass, unimproved sources of drinking water, unimproved toilet facilities, rudimentary roof material, and unclean floor material among under-five children were calculated using the Statistical Package and Data Science software STATA version 14.1 (StataCorp LP, College Station, TV, USA).
The case fatality rate is calculated as the rate of the total number of death cases due to COVD-19 to the total number of confirmed cases of the COVID-19. Similarly, the COVID-19 active case rate is calculated as the rate of the total number of cured/ discharged cases of the COVID-19 to the total number of confirmed cases of the COVID-19.
For the identification of the vulnerable/risk zone of the Coronavirus disease, the mean composite vulnerable score (CVS) method has been employed. For each state and UT, all the variables (V1, V2, V3 up to V13) are sum up and the mean was calculated, then standard deviation was calculated as the root mean square deviation from the mean. The composite vulnerable score also be calculated for the identification of the vulnerable zone of COVID-19 using the following formula-
| (1) |
All the Z-score values of all indicators for each state and UT have been calculated the mean was calculated using the total Z-score value divide by the number of variables to get a composite vulnerability score. A high Z-score value indicates the high-risk zone of COVID-19 among under-five children and vice versa.
Hot spot analysis (Getis-Ord Gi*): To identify COVID-19 vulnerable zones, hot spot analysis has been used. The hot spot analysis tool calculates the Getis-Ord Gi* statistic (pronounced G-i-star) for each characteristic in a dataset. Hot spot analysis using spatial statistics produces maps, which show the spatial concentration of events. The resultants Z-scores inform us where features with either high (hot spot) or low values (cold spot) cluster spatially (Nelson & Boots, 2008). This tool works by looking at each feature within the context of neighboring features. A feature with a high value is interesting but may not be a statistically significant hot spot (Prasannakumar et al., 2011). To be a statistically significant hot spot, a feature will have a high value and be enclosed by other features with high values as well (Jana & Sar, 2016). The local sum for a characteristic and its neighbors is compared proportionally to the sum of all features; when the local sum is very different from the expected local sum, and when that difference is too large to be the result of random chance, a statistically significant Z-score result. The Getis-Ord local statistics is given as-
| (2) |
Where, is the attribute value for future j, wi, j is the spatial weight between future i and j, n is equal to the total number of features and the statistics is a z-score, so no additional calculations are required.
3. Results
3.1. Prevalence of malnutrition, pre-existing morbidities, poor household environmental conditions among under-five children, and active case rate and case fatality rate of COVID-19 in India
Table 2 represents the percentage of under-five children with the prevalence of malnutrition, pre-existing morbidities, poor household environmental conditions, and current COVID-19 factors in India. The prevalence of stunting in children under age five is highest in Bihar (48.38%), Uttar Pradesh (46.27%), Jharkhand (45.54%), and Meghalaya (43.94%), and lowest in Kerala (19.99%). Jharkhand has the highest percentage of wasting (28.9%) and underweight (47.85%) under-five children. Symptoms of ARI was higher in the states like Meghalaya (5.8%), Jammu and Kashmir (5.4%), Uttar Pradesh (4.7%), Uttarakhand (4.6%), Punjab (4.1%), West Bengal (3.3%), Jharkhand (3.2%), Haryana (3.2%) compared to other states and UTs of India. The highest prevalence of cold & cough (22.15%) and fever (24.5%) has been observed in Uttrakhand among children under age five.
Table 2.
Percentage of under-five children with the prevalence of malnutrition, pre-existing morbidities, poor household environmental conditions, and COVID-19 factors in India.
| States and union territories |
Prevalence of malnutrition (%) |
Prevalence of pre-existing morbidities (%) |
Poor household environmental conditions (%) |
COVID-19 factors |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Stunting | Wasting | Underweight | ARI | Cold & Cough | Fever | Use smoky cooking fuel | Unimproved sources of drinking water | Unimproved toilet facilities | Rudimentary roof material | Unclean floor material | ACR | CFR | |
| Andaman & Nicobar Islands | 23.27 | 18.98 | 21.11 | 1.50 | 12.89 | 8.62 | 25.83 | 5.75 | 14.09 | 4.91 | 14.34 | 34.34 | 0.00 |
| Andhra Pradesh | 31.44 | 17.35 | 32.19 | 0.50 | 5.38 | 8.33 | 41.02 | 27.69 | 44.57 | 13.17 | 6.87 | 45.89 | 1.17 |
| Arunachal Pradesh | 29.30 | 16.93 | 19.44 | 2.10 | 10.54 | 11.45 | 59.41 | 15.12 | 14.00 | 31.03 | 15.99 | 62.02 | 0.52 |
| Assam | 36.25 | 16.98 | 29.77 | 1.00 | 8.77 | 8.97 | 81.68 | 16.53 | 15.68 | 7.03 | 76.36 | 34.96 | 0.21 |
| Bihar | 48.38 | 20.87 | 43.93 | 2.50 | 10.33 | 12.24 | 88.18 | 1.67 | 74.42 | 23.95 | 77.90 | 30.53 | 0.89 |
| Chandigarh | 29.22 | 9.93 | 24.46 | 2.80 | 10.35 | 9.69 | 10.08 | 1.02 | 4.65 | 2.26 | 5.61 | 26.70 | 1.36 |
| Chhattisgarh | 37.60 | 23.10 | 37.69 | 2.20 | 12.49 | 13.35 | 80.77 | 10.16 | 63.13 | 3.66 | 58.84 | 23.62 | 0.45 |
| Dadra and Nagar Havel | 41.84 | 27.57 | 38.76 | 1.90 | 5.53 | 5.63 | 49.62 | 19.43 | 52.76 | 11.58 | 46.42 | 45.66 | 0.20 |
| Daman and Diu | 23.12 | 24.34 | 26.19 | 0.60 | 5.43 | 6.57 | 11.11 | 8.25 | 6.69 | 1.61 | 1.62 | 45.66 | 0.20 |
| Delhi | 32.11 | 15.48 | 27.30 | 2.40 | 10.80 | 13.40 | 2.77 | 25.06 | 6.14 | 12.44 | 0.60 | 16.72 | 3.00 |
| Goa | 20.00 | 21.83 | 23.66 | 1.40 | 14.07 | 16.20 | 17.39 | 1.59 | 12.33 | 7.22 | 8.52 | 39.72 | 0.66 |
| Gujarat | 38.31 | 26.51 | 39.36 | 1.40 | 9.02 | 8.94 | 55.74 | 10.18 | 38.76 | 3.94 | 22.74 | 25.51 | 4.81 |
| Haryana | 34.00 | 21.23 | 29.53 | 3.20 | 8.87 | 9.24 | 55.69 | 9.91 | 15.14 | 12.98 | 19.47 | 22.76 | 1.41 |
| Himachal Pradesh | 26.40 | 13.90 | 21.56 | 1.60 | 10.78 | 11.84 | 71.87 | 3.47 | 17.07 | 2.98 | 14.57 | 23.49 | 0.88 |
| Jammu and Kashmir | 27.70 | 12.23 | 16.77 | 5.40 | 14.97 | 13.87 | 51.66 | 14.10 | 27.76 | 10.02 | 29.22 | 41.98 | 1.73 |
| Jharkhand | 45.54 | 28.90 | 47.85 | 3.20 | 10.42 | 12.62 | 86.94 | 23.99 | 76.36 | 4.91 | 65.88 | 38.84 | 0.85 |
| Karnataka | 36.28 | 25.89 | 35.08 | 1.20 | 5.76 | 7.05 | 47.57 | 10.44 | 42.55 | 16.89 | 9.55 | 59.10 | 1.82 |
| Kerala | 19.99 | 15.68 | 16.23 | 0.80 | 8.59 | 10.54 | 47.96 | 6.23 | 0.65 | 3.78 | 0.97 | 48.45 | 0.40 |
| Lakshadweep | 26.55 | 14.07 | 23.53 | 0.90 | 12.97 | 13.87 | 59.04 | 9.83 | 0.00 | 1.24 | 0.00 | - | - |
| Madhya Pradesh | 41.94 | 25.81 | 42.83 | 2.10 | 10.45 | 11.36 | 76.03 | 16.92 | 64.59 | 18.11 | 58.35 | 23.82 | 3.64 |
| Maharashtra | 34.23 | 25.52 | 35.91 | 2.40 | 9.24 | 12.62 | 42.53 | 9.44 | 35.67 | 3.66 | 21.88 | 40.60 | 4.02 |
| Manipur | 28.78 | 6.93 | 13.69 | 0.70 | 12.80 | 8.25 | 60.99 | 60.79 | 2.03 | 5.54 | 59.90 | 40.34 | 0.00 |
| Meghalaya | 43.94 | 15.04 | 28.88 | 5.80 | 20.21 | 23.29 | 83.67 | 29.24 | 13.31 | 11.04 | 25.81 | 78.62 | 0.63 |
| Mizoram | 27.86 | 5.96 | 11.91 | 2.20 | 19.46 | 11.42 | 37.69 | 9.22 | 1.40 | 9.77 | 1.99 | 35.19 | 0.00 |
| Nagaland | 28.51 | 11.33 | 16.81 | 1.40 | 8.55 | 7.13 | 75.44 | 20.20 | 2.64 | 17.58 | 56.51 | 59.76 | 0.00 |
| Odisha | 34.08 | 20.39 | 34.30 | 2.40 | 12.73 | 12.86 | 84.10 | 11.93 | 73.66 | 27.04 | 52.87 | 32.12 | 0.51 |
| Puducherry | 23.79 | 23.77 | 22.09 | 3.00 | 14.50 | 11.81 | 13.69 | 5.10 | 30.03 | 15.20 | 4.13 | 45.30 | 1.23 |
| Punjab | 25.75 | 15.69 | 21.65 | 4.10 | 13.18 | 13.36 | 39.31 | 0.82 | 8.34 | 5.81 | 17.88 | 29.20 | 2.49 |
| Rajasthan | 39.08 | 22.97 | 36.57 | 2.10 | 8.53 | 9.82 | 74.61 | 16.28 | 53.62 | 13.93 | 31.39 | 23.18 | 2.11 |
| Sikkim | 29.42 | 14.26 | 14.06 | 0.30 | 3.41 | 3.80 | 46.46 | 2.42 | 0.19 | 2.48 | 14.38 | 55.21 | 0.00 |
| Tamil Nadu | 27.16 | 19.66 | 23.82 | 2.80 | 14.37 | 10.75 | 25.91 | 9.79 | 40.87 | 14.16 | 7.19 | 33.75 | 1.42 |
| Telangana | 27.61 | 17.89 | 27.90 | 2.00 | 13.89 | 16.59 | 30.07 | 21.53 | 32.70 | 5.37 | 12.06 | 33.62 | 1.01 |
| Tripura | 23.98 | 16.72 | 23.98 | 2.60 | 12.88 | 11.67 | 70.76 | 17.76 | 5.92 | 3.99 | 68.12 | 28.99 | 0.10 |
| Uttar Pradesh | 46.27 | 17.93 | 39.49 | 4.70 | 14.26 | 19.67 | 73.48 | 3.27 | 59.55 | 21.11 | 64.62 | 34.02 | 2.50 |
| Uttarakhand | 33.87 | 19.50 | 26.82 | 4.60 | 22.15 | 24.50 | 57.39 | 6.78 | 20.17 | 14.25 | 28.84 | 19.48 | 1.36 |
| West Bengal | 32.72 | 20.18 | 31.56 | 3.30 | 11.00 | 12.57 | 78.09 | 5.63 | 34.63 | 9.78 | 54.38 | 35.87 | 3.04 |
| India | 38.37 | 21.04 | 35.73 | 2.31 | 11.38 | 11.77 | 53.18 | 9.97 | 49.39 | 14.19 | 43.78 | 34.36 | 2.62 |
About 53% of households in India use some type of solid fuel for cooking, with virtually all being wood or dung cakes. In India, 9.97% of households haven’t access to an improved source of drinking water and about half of the Indian households (49.39%) use unimproved toilet facilities, which are non-shared. About 14% of children living in houses having an unclean floor and 43.78% in houses having rudimentary roof material. In Odisha, the highest percentage (27.04%) of children living in houses having rudimentary roof material. In Bihar, the highest percentage (77.9%) of children living in houses having an unclean floor. The case fatality rate of COVID-19 is higher in Gujarat (4.81%), Maharashtra (4.02%), Madhya Pradesh (3.64%), West Bengal (3.04%), Delhi (3%) compared to other states and UTs of India. The active case rate is higher in Meghalaya (78.62%), Arunachal Pradesh (62.02%), Nagaland (59.76%), Karnataka (59.10%) compared to the other states and UTs of India (Table 2).
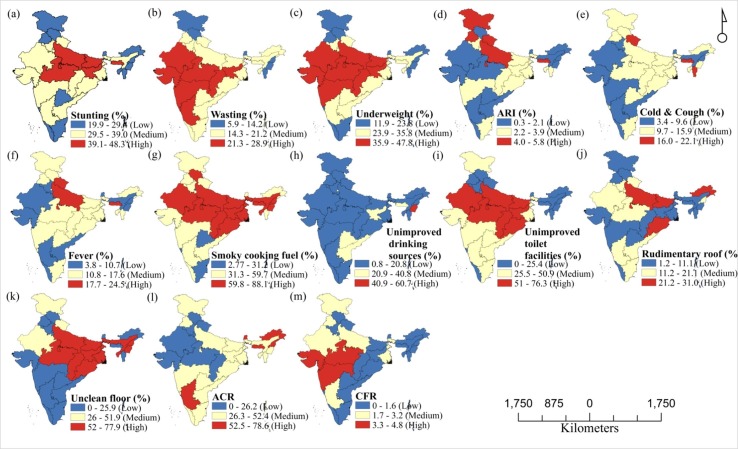
From the above maps, it is clear that in case of stunting the states like Jharkhand, Madhya Pradesh are showing high prevalence, and Jammu and Kashmir, Kerala states are showing low prevalence. In contrast, the states like Gujarat, Rajasthan are showing moderate stunting among under-five children of India. In the case of wasting and underweight, the states like Gujarat, Rajasthan, and Maharashtra are showing high whereas Jammu and Kashmir, Himachal Pradesh states are showing low prevalence. Contradictorily Jammu and Kashmir, Punjab, Uttar Pradesh, and Uttrakhand states are showing high, and Gujarat, Rajasthan are showing low acute respiratory infections. Uttarakhand is showing high, whereas Gujarat, Rajasthan, and Karnataka are showing low both in case of cold & cough and fever among under-five children in India. The use of smoky cooking fuel and unimproved sources of drinking water map states are quite contradictory to each other, states like Rajasthan, Madhya Pradesh, and Jharkhand are showing high percentages in case of use of smoky cooking fuel and a low percentage in case of unimproved sources of drinking water. In the case of unimproved toilet facilities, Rajasthan, Madhya Pradesh and Jharkhand are showing a high percentage, and Himachal Pradesh and Uttarakhand are showing a low percentage. Rudimentary roof materials and unclean floor materials are showing quite similar to each other in Uttar Pradesh and Bihar with a high percentage and Maharashtra and Telangana showing a low percentage. The active case rate is low in Gujarat and Madhya Pradesh, whereas high in Karnataka. In the case of CFR, states like Gujarat and Madhya Pradesh are showing high percentage and states like Kerala, Tamil Nadu, and Andhra Pradesh, etc., are showing a low percentage (Fig. 1 ).
Fig. 1.
Different indicators viz. (a) Stunting; (b) Wasting; (c) Underweight; (d) Acute Respiratory Infections (ARI); (e) Cold & cough; (f) Fever; (g) Use smoky cooking fuel; (h) Unimproved sources of drinking water; (i) Unimproved toilet facilities; (j) Rudimentary roof material; (k) Unclean floor material; (l) Active Case Rate (ACR); and (m) Case Fatality Rate (CFR) for identifying the COVID-19 vulnerable states and UTs of India.
3.2. Composite vulnerability score (CSV) aggravate susceptibility to Coronavirus disease (COVID-19) among under-five children in India
Table 3 represents the composite vulnerability score of various factors of the COVID-19 among under-five children in the states and UTs of India. The states and UTs which have a high composite vulnerability score of the COVID-19 among under-five children are Meghalaya (CVS = 1), Uttar Pradesh (CVS = 0.93), Jharkhand (CVS = 0.86), Bihar, (CVS = 0.74), Madhya Pradesh (CVS = 0.74), and Odisha (CVS = 0.55). The states and UTs which have low composite vulnerability score of the COVID-19 among under-five children are in Sikkim (CVS = -0.90), Daman & Diu (CVS = -0.76) Lakshadweep (CVS = -0.74), Kerala (CVS = -0.72), Chandigarh (CVS = -0.71).
Table 3.
Composite vulnerability score of different indicators of the prevalence of malnutrition, pre-existing childhood morbidities, poor household environmental conditions, and current COVID-19 factors in the states and UTs of India.
| States and union territories | V1 | V2 | V3 | V4 | V5 | V6 | V7 | V8 | V9 | V10 | V11 | V12 | V13 | Composite Vulnerability Score (CVS) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Andaman & Nicobar Islands | −1.18 | 0.06 | −0.74 | −0.60 | 0.37 | −0.73 | −1.12 | −0.64 | −0.57 | −0.73 | −0.60 | −0.24 | −1.02 | −0.60 |
| Andhra Pradesh | −0.09 | −0.23 | 0.46 | −1.34 | −1.47 | −0.79 | −0.50 | 1.30 | 0.69 | 0.37 | −0.90 | 0.61 | −0.08 | −0.15 |
| Arunachal Pradesh | −0.38 | −0.31 | −0.92 | −0.15 | −0.21 | −0.07 | 0.25 | 0.19 | −0.58 | 2.76 | −0.53 | 1.80 | −0.61 | 0.10 |
| Assam | 0.55 | −0.30 | 0.20 | −0.97 | −0.64 | −0.65 | 1.16 | 0.31 | −0.51 | −0.45 | 1.87 | −0.19 | −0.85 | −0.04 |
| Bihar | 2.17 | 0.39 | 1.73 | 0.14 | −0.26 | 0.11 | 1.43 | −1.00 | 1.93 | 1.81 | 1.94 | −0.52 | −0.31 | 0.74 |
| Chandigarh | −0.39 | −1.55 | −0.38 | 0.36 | −0.25 | −0.48 | −1.76 | −1.06 | −0.97 | −1.09 | −0.95 | −0.80 | 0.07 | −0.71 |
| Chhattisgarh | 0.73 | 0.79 | 1.05 | −0.08 | 0.27 | 0.36 | 1.13 | −0.25 | 1.46 | −0.90 | 1.18 | −1.03 | −0.66 | 0.31 |
| Dadra and Nagar Havel | 1.30 | 1.59 | 1.17 | −0.30 | −1.43 | −1.42 | −0.15 | 0.57 | 1.03 | 0.16 | 0.68 | 0.59 | −0.86 | 0.23 |
| Daman and Diu | −1.20 | 1.01 | −0.19 | −1.27 | −1.46 | −1.20 | −1.72 | −0.42 | −0.88 | −1.18 | −1.10 | 0.59 | −0.86 | −0.76 |
| Delhi | 0.00 | −0.56 | −0.07 | 0.07 | −0.14 | 0.37 | −2.06 | 1.07 | −0.90 | 0.27 | −1.15 | −1.53 | 1.38 | −0.25 |
| Goa | −1.62 | 0.57 | −0.47 | −0.67 | 0.66 | 1.02 | −1.46 | −1.01 | −0.65 | −0.43 | −0.83 | 0.16 | −0.49 | −0.40 |
| Gujarat | 0.83 | 1.40 | 1.24 | −0.67 | −0.58 | −0.65 | 0.10 | −0.25 | 0.45 | −0.86 | −0.26 | −0.89 | 2.84 | 0.21 |
| Haryana | 0.25 | 0.46 | 0.17 | 0.66 | −0.62 | −0.58 | 0.10 | −0.27 | −0.53 | 0.35 | −0.39 | −1.09 | 0.11 | −0.11 |
| Himachal Pradesh | −0.76 | −0.84 | −0.69 | −0.53 | −0.15 | 0.02 | 0.76 | −0.84 | −0.45 | −0.99 | −0.59 | −1.03 | −0.31 | −0.49 |
| Jammu and Kashmir | −0.59 | −1.14 | −1.21 | 2.29 | 0.88 | 0.48 | −0.06 | 0.10 | −0.01 | −0.05 | 0.00 | 0.32 | 0.36 | 0.11 |
| Jharkhand | 1.79 | 1.82 | 2.16 | 0.66 | −0.23 | 0.19 | 1.38 | 0.97 | 2.01 | −0.73 | 1.46 | 0.09 | −0.34 | 0.86 |
| Karnataka | 0.56 | 1.29 | 0.77 | −0.82 | −1.38 | −1.09 | −0.23 | −0.23 | 0.61 | 0.87 | −0.79 | 1.58 | 0.44 | 0.12 |
| Kerala | −1.62 | −0.53 | −1.27 | −1.12 | −0.68 | −0.28 | −0.21 | −0.60 | −1.13 | −0.89 | −1.13 | 0.80 | −0.70 | −0.72 |
| Lakshadweep | −0.74 | −0.81 | −0.48 | −1.04 | 0.39 | 0.48 | 0.24 | −0.28 | −1.16 | −1.23 | −1.17 | −2.76 | −1.02 | −0.74 |
| Madhya Pradesh | 1.31 | 1.27 | 1.61 | −0.15 | −0.23 | −0.10 | 0.93 | 0.35 | 1.52 | 1.03 | 1.16 | −1.01 | 1.90 | 0.74 |
| Maharashtra | 0.28 | 1.22 | 0.86 | 0.07 | −0.52 | 0.19 | −0.43 | −0.31 | 0.32 | −0.90 | −0.30 | 0.22 | 2.20 | 0.22 |
| Manipur | −0.45 | −2.08 | −1.55 | −1.19 | 0.35 | −0.81 | 0.32 | 4.23 | −1.07 | −0.65 | 1.22 | 0.20 | −1.02 | −0.19 |
| Meghalaya | 1.58 | −0.64 | 0.10 | 2.59 | 2.17 | 2.65 | 1.24 | 1.44 | −0.61 | 0.09 | −0.14 | 3.02 | −0.52 | 1.00 |
| Mizoram | −0.57 | −2.25 | −1.74 | −0.08 | 1.98 | −0.08 | −0.63 | −0.33 | −1.10 | −0.08 | −1.09 | −0.17 | −1.02 | −0.55 |
| Nagaland | −0.48 | −1.30 | −1.21 | −0.67 | −0.69 | −1.07 | 0.91 | 0.64 | −1.05 | 0.96 | 1.08 | 1.63 | −1.02 | −0.18 |
| Odisha | 0.26 | 0.31 | 0.69 | 0.07 | 0.33 | 0.25 | 1.26 | −0.09 | 1.90 | 2.23 | 0.94 | −0.40 | −0.61 | 0.55 |
| Puducherry | −1.11 | 0.91 | −0.64 | 0.51 | 0.77 | 0.01 | −1.61 | −0.70 | 0.09 | 0.64 | −1.00 | 0.57 | −0.04 | −0.12 |
| Punjab | −0.85 | −0.53 | −0.68 | 1.33 | 0.44 | 0.37 | −0.57 | −1.08 | −0.81 | −0.61 | −0.46 | −0.62 | 0.98 | −0.24 |
| Rajasthan | 0.93 | 0.77 | 0.93 | −0.15 | −0.70 | −0.45 | 0.87 | 0.29 | 1.06 | 0.47 | 0.08 | −1.06 | 0.67 | 0.29 |
| Sikkim | −0.36 | −0.78 | −1.51 | −1.49 | −1.95 | −1.84 | −0.27 | −0.94 | −1.15 | −1.06 | −0.60 | 1.30 | −1.02 | −0.90 |
| Tamil Nadu | −0.66 | 0.18 | −0.45 | 0.36 | 0.73 | −0.24 | −1.11 | −0.28 | 0.54 | 0.50 | −0.88 | −0.28 | 0.12 | −0.11 |
| Telangana | −0.60 | −0.13 | −0.01 | −0.23 | 0.62 | 1.11 | −0.94 | 0.76 | 0.20 | −0.67 | −0.69 | −0.29 | −0.21 | −0.08 |
| Tripura | −1.09 | −0.34 | −0.43 | 0.22 | 0.37 | −0.02 | 0.72 | 0.42 | −0.91 | −0.86 | 1.55 | −0.63 | −0.95 | −0.15 |
| Uttar Pradesh | 1.89 | −0.13 | 1.25 | 1.77 | 0.71 | 1.82 | 0.83 | −0.86 | 1.31 | 1.43 | 1.41 | −0.26 | 0.99 | 0.93 |
| Uttarakhand | 0.23 | 0.15 | −0.12 | 1.70 | 2.64 | 2.93 | 0.17 | −0.55 | −0.32 | 0.52 | −0.02 | −1.33 | 0.07 | 0.47 |
| West Bengal | 0.08 | 0.27 | 0.39 | 0.74 | −0.09 | 0.18 | 1.02 | −0.65 | 0.28 | −0.08 | 1.00 | −0.13 | 1.42 | 0.34 |
| Mean | 32.12 | 18.65 | 27.96 | 2.31 | 11.38 | 11.77 | 53.18 | 12.99 | 27.95 | 10.40 | 29.33 | 37.57 | 1.27 | |
| Standard deviation (σ) | 7.49 | 5.63 | 9.22 | 1.35 | 4.08 | 4.34 | 24.50 | 11.30 | 24.11 | 7.47 | 25.09 | 13.61 | 1.25 | |
V1= Stunting;V2= Wasting;V3= Underweight;V4= Acute Respiratory Infections (ARI);V5= Cold & cough;V6= Fever;V7= Use smoky cooking fuel;V8= Unimproved sources of drinking water;V9= Unimproved toilet facilities;V10= Rudimentary roof material;V11= Unclean floor material;V12= Active case rate (ACR); andV13= Case fatality rate (CFR).
The results of the analysis are shown in Fig. 2 which depicts state and union territory wise hot spot (vulnerable) and cold spot zone of COVID-19 among under-five children in India. Here, hot spots shown in red are statistically significant high clusters of events, random events are shown in yellow color and cold spots shown in blue color are statistically significant low clusters of events. The COVID-19 vulnerable/ risk zones (hot spot: 99% Confidence interval [CI]) were observed in Madhya Pradesh, Uttar Pradesh, Jharkhand, Bihar, and Meghalaya states of India, which are spatially high clustered, while comparatively high rates (hot spot: 95% CI) of COVID-19 vulnerable zones were observed in Chhattisgarh, Odisha, and West Bengal. The less vulnerable zones (cold spot: 95% CI) were observed in Kerala, Mizoram, and Sikkim, and comparatively less vulnerable zones (cold spot: 90% CI) were observed in Himachal Pradesh, Punjab, Delhi, Manipur, Nagaland, Tripura, Goa, and Andhra Pradesh.
Fig. 2.
State and union territory wise hot spot (vulnerable) and cold spot areas of COVID-19 among under-five children in India.
4. Discussion
Globally, stunting, wasting, and underweight are health risks for various diseases also the COVID-19. This study has identified the risk zones of COVID-19 among children under age five in India. As the Coronavirus has been associated with malnutrition, so, there has a relationship between malnutrition and COVID-19 (Fore et al., 2020; Headey et al., 2020). Children’s malnutrition in vulnerable zones could intensify the effects of COVID-19 among children under age five. In the same way, more children under age five are becoming undernourished due to the weakening of health systems, disrupting routine services, interruptions in nutrition and supplementary necessary services, and the socio-economic alter happened by the COVID-19 pandemic in India. Our finding showed that children under age five with high malnutrition have a moderate to high risk of COVID-19 and these states and UTs are susceptible to COVID-19 in India.
Pre-existing morbidities like acute respiratory infection, cold & cough, and fever among children under age five in India have risk factors of the COVID-19. In previous studies, it is found that pre-existing co-morbidities among children under age five are risk factors of the COVID-19 death and these zones are vulnerable to COVID-19 (Saha & Chouhan, 2020, Shekerdemian et al., 2020, Sinha et al., 2020). This finding is in agreement with another study conducted in India (Saha & Chouhan, 2020).
Uses of smoky cooking fuel or solid biomass gas are the risk factors of health disease among under-five children. The use of smoky cooking fuel directly associated with the respiratory health system of living children and dependence on hard biomass for cooking and burning or heating exposes respiratory health problems of under-five children in India. Those people living in an area with extremely high amounts of pollutants are, therefore, more likely to develop severe respiratory infections and also aggravate susceptibility to COVID-19 (Conticini et al., 2020; Tobías et al., 2020). For its likelihood to increase the vulnerability of COVID-19 through smoky cooking fuel-related health effects among children under-five age and from the household air pollutants as such, the accessible public health challenge of indoor air pollution (IAP) in India (Saha & Chouhan, 2020) warrants concern and demands immediate and specific measures.
The spread of COVID-19 is directly related to the unimproved water and sanitation conditions of households. In developing countries, many people have lack of access to improved sources of drinking water and sanitation facilities at present (Cox & Piccolo, 2020). In India, the risk of developing the COVID-19 was higher among those under-five children who are using unimproved drinking water sources and unimproved toilet facilities compared to those children who are using improved sources of drinking water and sanitation. The risk of developing the COVID-19 was higher in children from poor household environment having rudimentary roof materials and unclean floor materials than those from households having metal or concrete roof materials and clean floor materials. This could be because the unclean floor and rudimentary roof materials of the dwelling cause the transmission of the virus, which may aggravate susceptibility to Coronavirus disease. The states and UTs with high case fatality rates are vulnerable areas of the COVID-19 in India. This study is consistent with the study in the People’s Republic of China (Cui et al., 2003) and Northern Italy (Conticini et al., 2020).
5. Limitations
The measurement of CFR amid the COVID-19 outbreak is very difficult, due to to under-reporting. In some places, patients might even die being tested. A major challenge with the exact calculation of the CFR is the denominator: the number of COVID-19 positive people. Asymptomatic cases of COVID-19, patients with mild symptoms, or individuals who are misdiagnosed could be left out of the denominator, leading to its underestimation and overestimation of the CFR. Surveyed women have self-reported about their children’s pre-existing childhood morbidities, so there is a possibility of recall bias during the collection of information about children.
6. Conclusion
In the vulnerable states and UTs of India, under-five children being underprivileged of nutrition sustain, and also to a load of families because of not capable to meet ends due to loss of job and wages and alarming poverty due to the COVID-19 lockdown in India. So, there is a requirement to make stronger the existing food availability and supply along with ample counselling on mask wearing, hand-washing, and social isolation. If don’t this, there is a likelihood of an increase in the number of malnourished under-five children who are susceptible to Coronavirus due to be deficient in immunity level. This possibly will have a negative boost in long-lasting health among under-five children and socio-economic and demographic impact in the vulnerable states and UTs of India. Access to clean drinking water and toilet facilities is key for public health and dropping the transmission of infectious diseases like COVID-19 in the vulnerable zones. For developing countries like India improving access to these facilities be supposed to be a top main concern to reduce this infectious disease.
CRediT authorship contribution statement
Jay Saha: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Supervision, Validation, Visualization, Writing - original draft, Writing - review & editing. Pradip Chouhan: Conceptualization, Formal analysis, Investigation, Supervision, Validation, Visualization, Writing - original draft.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.childyouth.2021.105962.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Abuzerr S., Nasseri S., Yunesian M., Hadi M., Zinszer K., Mahvi A.H.…Mohammed S.H. Water, sanitation, and hygiene risk factors of acute diarrhea among children under five years in the Gaza Strip. Journal of Water, Sanitation and Hygiene for Development. 2020;10(1):111–123. doi: 10.2166/washdev.2019.072. [DOI] [Google Scholar]
- Adane M., Mengistie B., Kloos H., Medhin G., Mulat W. Sanitation facilities, hygienic conditions, and prevalence of acute diarrhea among under-five children in slums of Addis Ababa, Ethiopia: Baseline survey of a longitudinal study. PloS one. 2017;12(8) doi: 10.1371/journal.pone.0182783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cascella, M., Rajnik, M., Cuomo, A., Dulebohn, S. C., & Di Napoli, R. (2020). Features, evaluation and treatment coronavirus (COVID-19). In Statpearls [internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK554776/. [PubMed]
- Chan J.F.W., Yuan S., Kok K.H., To K.K.W., Chu H., Yang J.…Yuen K.Y. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster. The Lancet. 2020;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conticini E., Frediani B., Caro D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environmental pollution. 2020;114465 doi: 10.1016/j.envpol.2020.114465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox, A., & Piccolo, A. (2020). Environmental health and strengthening resilience to pandemics. http://www.oecd.org/coronavirus/policy-responses/environmental- health-and-strengthening-resilience-to-pandemics-73784e04/#biblio-d1e862.
- Cui Y., Zhang Z.F., Froines J., Zhao J., Wang H., Yu S.Z., Detels R. Air pollution and case fatality of SARS in the People's Republic of China: An ecologic study. Environmental Health. 2003;2(1):1–5. doi: 10.1186/1476-069X-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Onis M., Garza C., Victora C.G., Onyango A.W., Frongillo E.A., Martines J. The WHO Multicentre Growth Reference Study: planning, study design, and methodology. Food and nutrition bulletin. 2004;25(1_suppl_1):S15–S26. doi: 10.1177/15648265040251S103. [DOI] [PubMed] [Google Scholar]
- Fore H.H., Dongyu Q., Beasley D.M., Ghebreyesus T.A. Child malnutrition and COVID-19: The time to act is now. The Lancet. 2020;396(10250):517–518. doi: 10.1016/S0140-6736(20)31648-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Getachew A., Guadu T., Tadie A., Gizaw Z., Gebrehiwot M., Cherkos D.H.…Gebrecherkos T. Diarrhea prevalence and sociodemographic factors among under-five children in rural areas of North Gondar Zone, Northwest Ethiopia. International Journal of Pediatrics. 2018;2018 doi: 10.1155/2018/6031594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IIPS & ICF. (2017). National Family Health Survey (NFHS-4), 2015–16. International Institute for Population Sciences (IIPS), Mumbai, India. http://rchiips.org/nfhs/NFHS-4Reports/India.pdf.
- Godana, W., & Mengiste, B. (2013). Environmental factors associated with acute diarrhea among children under five years of age in derashe district, Southern Ethiopia. Sci J Public Health, 1(3), 119-124. https://doi.org/10.11648/j.sjph.20130103.12. [PubMed]
- Headey D., Heidkamp R., Osendarp S., Ruel M., Scott N., Black R.…Walker N. Impacts of COVID-19 on childhood malnutrition and nutrition-related mortality. The Lancet. 2020;396(10250):519–521. doi: 10.1016/S0140-6736(20)31647-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jana M., Sar N. Modeling of hotspot detection using cluster outlier analysis and Getis-Ord Gi* statistic of educational development in upper-primary level, India. Modeling Earth Systems and Environment. 2016;2(2):60. doi: 10.1007/s40808-016-0122-x. [DOI] [Google Scholar]
- Jin Y., Yang H., Ji W., Wu W., Chen S., Zhang W., Duan G. Virology, epidemiology, pathogenesis, and control of COVID-19. Viruses. 2020;12(4):372. doi: 10.3390/v12040372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai C.C., Shih T.P., Ko W.C., Tang H.J., Hsueh P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and corona virus disease- 2019 (COVID-19): The epidemic and the challenges. International journal of antimicrobial agents. 2020;105924 doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masibo, P. K. (2013). Trends and determinants of malnutrition among children Age 0-59 months in Kenya (KDHS 1993, 1998, 2003, and 2008-09). https://doi.org/10.1017/S1368980012002856.
- Linnemayr S., Alderman H., Ka A. Determinants of malnutrition in Senegal: Individual, household, community variables, and their interaction. Economics & Human Biology. 2008;6(2):252–263. doi: 10.1016/j.ehb.2008.04.003. [DOI] [PubMed] [Google Scholar]
- Mihrete T.S., Alemie G.A., Teferra A.S. Determinants of childhood diarrhea among underfive children in Benishangul Gumuz regional state, north West Ethiopia. BMC pediatrics. 2014;14(1):102. doi: 10.1186/1471-2431-14-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MoHFW . COVID-19 State-wise Status. Government of India; New Delhi: 2020. https://www.mohfw.gov.in/ [Google Scholar]
- Mshida H.A., Kassim N., Mpolya E., Kimanya M. Water, sanitation, and hygiene practices associated with nutritional status of under-five children in semi- pastoral communities Tanzania. The American journal of tropical medicine and hygiene. 2018;98(5):1242–1249. doi: 10.4269/ajtmh.17-0399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson T.A., Boots B. Detecting spatial hot spots in landscape ecology. Ecography. 2008;31(5):556–566. [Google Scholar]
- Nsabimana J., Mureithi C., Habtu M. Factors Contributing to Diarrheal Diseases among Children Less than Five Years in Nyarugenge District. Rwanda. 2017 doi: 10.4172/2329-891X.1000238. [DOI] [Google Scholar]
- Peeri N.C., Shrestha N., Rahman M.S., Zaki R., Tan Z., Bibi S.…Haque U. The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: What lessons have we learned? International journal of epidemiology. 2020 doi: 10.1093/ije/dyaa033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poda G.G., Hsu C.Y., Chao J.C.J. Factors associated with malnutrition among children< 5 years old in Burkina Faso: Evidence from the Demographic and Health Surveys IV 2010. International Journal for Quality in Health Care. 2017;29(7):901–908. doi: 10.1093/intqhc/mzx129. [DOI] [PubMed] [Google Scholar]
- Prasannakumar V., Vijith H., Charutha R., Geetha N. Spatio-temporal clustering of road accidents: GIS based analysis and assessment. Procedia-Social and Behavioral Sciences. 2011;21:317–325. doi: 10.1016/j.sbspro.2011.07.020. [DOI] [Google Scholar]
- Ramani V.K., Pattankar J., Puttahonnappa S.K. Acute respiratory infections among under-five age group children at urban slums of gulbarga city: A longitudinal study. Journal of clinical and diagnostic research: JCDR. 2016;10(5):LC08. doi: 10.7860/JCDR/2016/15509.7779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehman M.U., Ishaq M. Prevalence of acute respiratory infections (ARI) and its risk factors in under five children in urban and rural areas of Matta, district Swat. International Journal of Infectious Diseases. 2018;73:230. doi: 10.1016/j.ijid.2018.04.3937. [DOI] [Google Scholar]
- Saha J., Barman B., Chouhan P. Lockdown for COVID-19 and its impact on community mobility in India: An analysis of the COVID-19 Community Mobility Reports, 2020. Children and Youth Services Review. 2020;105160 doi: 10.1016/j.childyouth.2020.105160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha J., Chouhan P. Indoor air pollution (IAP) and pre-existing morbidities among under-5 children in India: are risk factors of coronavirus disease (COVID-19)? Environmental Pollution. 2020;266:115250. doi: 10.1016/j.envpol.2020.115250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha J., Chouhan P. Lockdown and unlock for the COVID-19 pandemic and associated residential mobility in India. International Journal of Infectious Diseases. 2021;104:382–389. doi: 10.1016/j.ijid.2020.11.187. [DOI] [PubMed] [Google Scholar]
- Shekerdemian L.S., Mahmood N.R., Wolfe K.K., Riggs B.J., Ross C.E., McKiernan C.A.…Burns J.P. Characteristics and outcomes of children with coronavirus disease 2019 (COVID-19) infection admitted to US and Canadian pediatric intensive care units. JAMA pediatrics. 2020 doi: 10.1001/jamapediatrics.2020.1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singhai T. A review of the coronavirus disease-2019. Indian J Pediatr. 2020;87:281–286. doi: 10.1007/s12098-020-03263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha I.P., Harwood R., Semple M.G., Hawcutt D.B., Thursfield R., Narayan O.…Southern K.W. COVID-19 infection in children. The Lancet Respiratory Medicine. 2020 doi: 10.1016/S2213-2600(20)30152-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobías A., Carnerero C., Reche C., Massagué J., Via M., Minguillón M.C.…Querol X. Changes in air quality during the lockdown in Barcelona (Spain) one month into the SARS-CoV-2 epidemic. Science of the Total Environment. 2020;138540 doi: 10.1016/j.scitotenv.2020.138540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UN Inter-agency Group for Child Mortality Estimation. (2011). Levels & Trends in Child Mortality: Report 2011, New York: UNICEF. https://data.unicef.org/resources/levels-and-trends-in-child-mortality-report- 2011/.
- UNICEF . Food and Nutrition – Growing Well in a Changing World; UNICEF: 2019. The State of the World’s Children 2019: Children. https://www.unicef.org/reports/state-of-worlds-children-2019. [Google Scholar]
- UNICEF. (2019b). Children: Reducing Mortality, Key Facts. https://www.who.int/newsroom/fact-sheets/detail/children-reducing-mortality.
- Velavan T.P., Meyer C.G. The COVID-19 epidemic. Tropical medicine & international health. 2020;25(3):278. doi: 10.1111/tmi.13383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vijayan B., Ramanathan M. Prevalence and clustering of diarrhoea within households in India: Some evidence from NFHS-4, 2015–16. Journal of Biosocial Science. 2020;1–13 doi: 10.1017/S0021932020000073. [DOI] [PubMed] [Google Scholar]
- WHO . World Health Organization; World Health Organization: 2020. WHO Coronavirus Disease (COVID-19) Dashboard. https://www.who.int/ [Google Scholar]
- Workie G.Y., Akalu T.Y., Baraki A.G. Environmental factors affecting childhood diarrheal disease among under-five children in Jamma district, South Wello zone, Northeast Ethiopia. BMC infectious diseases. 2019;19(1):804. doi: 10.1186/s12879-019-4445-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zedie, F. B., & Kassa, D. H. (2018). Socio-economic, behavioral and environmental factors associated with diarrhea among under five children in health development and non-health development army member mothers in Wondogenet, south Ethiopia. Health Educ Care, 3(3), 1-8. https://doi.org/10.15761/HEC.1000144.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.