Abstract
Background
The COVID-19 pandemic has shifted the dynamics of health care and neurosurgical practice. Elective surgeries were suspended for 8 weeks in Kentucky. Our objective was to determine if telehealth (TH) visits could be sustained as an alternative to in-person visits.
Methods
Deidentified data on TH usage, in-person clinic visits, and inpatient and neurosurgical case volumes from March 2, 2020 to June 26, 2020 were obtained for retrospective analysis.
Results
TH use increased soon after the case suspension started and then decreased to little usage. The number of in-person visits were significantly lower during elective case suspension compared with when cases were resumed. Twenty-five percent of all visits during the suspension were conducted using TH. Thirty-nine percent of TH-visit patients were new patients, 11% were preoperative, 10% were postoperative, and 39% were other existing patients. Forty-eight percent of TH visits resulted in a later in-person clinic visit. After the suspension, in-person visits rebounded to 98% of the prepandemic numbers and TH visits were low.
Conclusions
TH visits were challenging due to the need for in-person physical examinations in neurosurgery. TH temporarily accommodated patient needs during the pandemic but could not totally replace in-person visits and was not sustained after 3.5 months of use. Video TH visits worked well for nonurgent issues, such as minor visual examinations. Our findings could help guide the implementation of TH should similar circumstances arise again.
Key words: COVID-19, Neurosurgery, Telehealth, Telemedicine
Abbreviations and Acronyms: APP, Advanced practice provider; ICU, Intensive care unit; TH, Telehealth
Introduction
As the COVID-19 pandemic spread to the United States in March 2020, health care providers worldwide were forced to rapidly adapt how they saw and evaluated patients.1, 2, 3 Quarantining, social distancing, and limiting in-person contact quickly became the fundamental approach to limiting the spread of the virus and greatly impacted the delivery of medical and surgical care. At the beginning of the pandemic, limitations in resources, such as personal protective equipment, testing kits, and ventilators reduced the ability to treat patients throughout the health care system. In many U.S. states including Kentucky, the government shutdown elective surgical procedures, which dramatically reduced patient flow, altered the distribution of human resources, and negatively impacted financial reimbursements. Taken together, these changes created considerable challenges to providing the appropriate care for the needs of patients, which continued throughout the pandemic.
One of the most seemingly practical solutions to this problem was to use telehealth (TH), also known as telemedicine, to maintain patient throughput while keeping hospital staff and patients safe with social distancing. Previously, providers and patients were limited in using TH due to several factors including the lack of access to the required technology, a lack of need, limited reimbursements, and concerns about patient confidentiality and liability.4, 5, 6 The COVID-19 pandemic left providers feeling that they had no choice but to use TH; however, the barriers previously faced had evolved during the pandemic making TH more accessible. TH had rapidly expanded primarily because Medicare, Medicaid, and commercial health insurance plans had approved home-based telehealth as a reimbursable service. Providers were able to connect from their home or office via computer, tablet, or smartphone to the patient's computer, tablet, or smartphone. Many institutions had rapidly adopted TH since the emergence of the pandemic1; however, its use in neurosurgery had not been widely reported until the pandemic.7 , 8 Understanding the benefits and challenges of using TH in a university hospital setting can provide other institutions with a practical view of whether or not to implement it.
TH clinical visits were quickly implemented for the first time in the Department of Neurosurgery at the University of Kentucky. The state of Kentucky suspended elective surgical cases from March 18 to May 11, 2020. Surgical cases were considered to be elective if the patient had a chronic or non−life-threatening issue and had no to minimal risk for progression or additional functional loss by waiting. Nonelective surgeries included life-threatening cases, those at high risk for additional loss of function such as candidates for spinal surgeries, device battery replacements, and those with severe myelopathy. TH was considered to be a safer alternative to in-person visits at the time. This unique window of 8 weeks allowed us to analyze the impact of the COVID-19 restrictions on our patient flow and evaluate the overall utility of TH in our academic neurosurgery setting.
Our goal with these analyses was to see if TH could be sustainable in a neurosurgical practice. We conducted a detailed retrospective analysis of the impact of the pandemic on our inpatient and outpatient neurosurgical workflows including inpatient volumes, consult volumes, surgical volumes, and clinic volumes. We also present an in-depth analysis of TH implementation in neurosurgery broken down by type of provider and outcomes following the TH visit.
Materials and Methods
Institution Profile: Neurosurgery Department at the University of Kentucky
The University of Kentucky is the largest university in Kentucky. It is a public research university with a major teaching hospital and the only level 1 trauma center serving central and eastern Kentucky. All aspects of neurosurgical care including emergent, urgent, and elective consultations and procedural interventions are carried out on the same campus in Lexington, Kentucky. Points of service occur in the hospital (emergency department, operating room, interventional suites, intensive care unit [ICU], and patient floors) and in the Kentucky Neuroscience Institute clinic space.
Telehealth Patients
Elective cases were suspended in the state of Kentucky from March 18 to May 11, 2020. Patients were offered a TH visit if they had a nonemergent issue or if they were at high risk for COVID-19 based on medical history. If a patient had a significant deficit or possible malignant findings on magnetic resonance imaging, they would be recommended for in-person evaluation. Specific medical conditions that were suitable for TH were chronic conditions (including spinal stenosis, chronic radiculopathy), new onset of symptoms in patients who did not have conservative treatment, and initial evaluations for movement disorders, such as Parkinson disease and essential tremor. Typically, patients were scheduled with an advanced practice provided (APP) if they did not appear to need immediate surgery after screening their referral information or had yet to undergo conservative treatment. Otherwise, a physician would see the patient. TH patients needed to reside in the state of Kentucky and have imaging that could be sent to the provider before the TH visit. They also needed Internet access to sign onto the Zoom conferencing platform and an e-mail address.
Medicare and Medicaid and commercial health plans had approved home-based telehealth as a reimbursable service. Providers connected from their home or office via computer, tablet, or smartphone to the patient's computer, tablet, or smartphone using UK's Zoom video conferencing platform. Zoom is a HIPAA (Health Insurance Portability and Accountability Act)−compliant third-party videoconference platform that uses any web-enabled communication device to facilitate a telehealth visit. Patients benefitted from this service because of the convenience of not leaving home and not being exposed to COVID-19 by traveling to a health care facility.
Data Collection
Data were obtained as part of a retrospective analysis of TH usage. All of the data for this report was deidentified data; thus it did not fall into the category of human research and did not require an IRB approval. TH, in-person clinic visits, inpatient, and surgical cases data from March 2, 2020 to June 26, 2020 were retrieved from Allscripts practice management, Allscripts electronic health record, and Picis OR manager system with no identifying information.
Deidentified inpatient and surgical cases data were collected from a retrospective review of the daily census that was printed out every morning around 5:30 a.m. for checkout (saved on a secured server with University of Kentucky Healthcare Sharepoint). Data were collected from January 1 to June 30 of 2020 to capture transitioning from before the pandemic to after elective cases were suspended. Data from the same time in the previous year were used as a comparison with prepandemic numbers (January 1 to June 30 of 2019). The data reflect all ICU and floor patients on the neurosurgery service, total consults (includes new consults), admits, and postoperative elective surgeries over the previous 24 hours (i.e., census on Tuesday morning reflects new patients from Monday). Weekly data were summed or averaged from Tuesday census to Monday census, reflecting Monday through Sunday. Authors obtained, graphed, and analyzed the data.
Cerebral angiogram case volume data were collected and sent to the authors with no identifying information from an internal surgical log in the interventional radiology department. Data were shared with the authors in an Excel sheet format and analyzed. Data were retrieved about patient type (new or existing), TH visit outcome (return for in-person clinic, TH, PRN, OR, or TBD), provider type (advanced practice providers or physician), and mode of TH visit (phone or video call). APPs consist of nurse practitioners and physician assistants.
Statistical Analyses
The mean number of neurosurgical cases during the window of suspension in 2020 was compared with cases during this window in 2019 using Student's t-test. The number of ICU and floor patients and consults before, during, and after elective case suspension were compared using 1-way analysis of variance, and multiple comparisons were made using the Tukey test. Comparisons of means between in-person and TH visits during and after the window of elective case suspension were made using 2-way analysis of variance and multiple comparisons using the Sidak test. In all statistical tests, significance was defined as P < 0.05.
Results
Effect of Suspending Elective Cases on Neurosurgery Cases
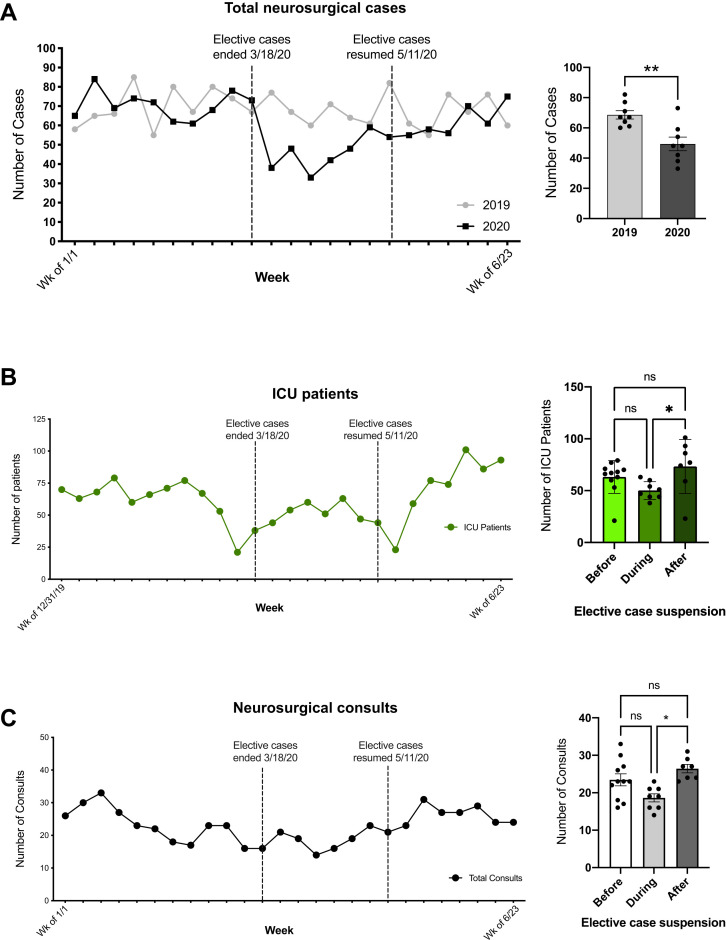
The total number of neurosurgical cases in 2020 dropped to 38 cases (55% of baseline) the week immediately after elective cases were suspended and then dropped to a low of 33 cases (48%) during the third week of the suspension (Figure 1A ). The baseline for weekly number of cases (69) was defined by averaging January−June 2019 cases and January−March 2020 cases (see Figure 1A). The number of cases during the window of suspension was significantly lower in 2020 compared with the same timeframe in 2019 (p = 0.0025; see Figure 1A). By the end of the suspension, neurosurgical cases rose to 54 weekly cases (78%) and reached 75 cases (109% of baseline) 6 weeks after elective cases resumed (see Figure 1A). The neurosurgical cases shown in Figure 1A include surgeries from spine, cerebrovascular, pediatric, epilepsy, tumor, endovascular, and functional neurosurgical practices.
Figure 1.
Neurosurgery cases decreased after elective cases were suspended. (A) Total number of neurosurgical cases shown from January 1 to June 23 of 2019 and 2020. During elective case suspension, neurosurgical cases dropped to 48% of baseline cases. The number of cases during the window of suspension was significantly lower in 2020 compared with the same timeframe in 2019 (P = 0.0025). (B) There were significantly fewer (non-COVID-19) intensive care unit patients during the window of suspension compared with after the suspension (P = 0.045). (C) There were significantly fewer neurosurgical consults during the window of suspension compared with after the suspension (P = 0.04).
There were decreases in ICU patients around the times when elective cases were suspended and resumed. There were significantly fewer (non−COVID-19) ICU patients during the window of suspension compared with after the suspension (P = 0.045; see Figure 1B). Similarly, there were significantly fewer neurosurgical consults during the window of suspension compared with after the suspension (P = 0.04; Figure 1C).
Using Telehealth During Suspension of Elective Cases
In-Person Visits
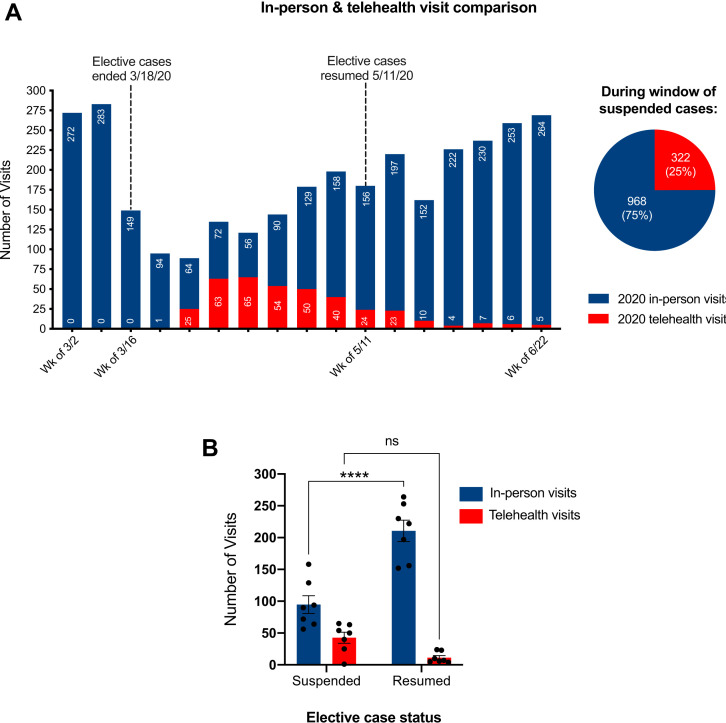
The numbers of in-person visits 2 weeks before the suspension (March 2−13, 2020) and in the same 2 weeks in the year prior (2019) were averaged and used as a baseline for comparisons (268.5 in-person visits). Approximately 4 weeks after elective cases were suspended, the number of in-person visits reached a low of 56 visits for the week (21% of baseline) but increased to 56% (156 visits) by the time elective cases resumed (Figure 2A ). Six weeks after elective cases resumed, in-person visits were at 98% (264 visits for the week) of baseline (see Figure 2A). The number of in-person visits per week was lower during elective case suspension compared with when cases were resumed (P < 0.0001; see Figure 2B).
Figure 2.
In-person and telehealth (TH) visit comparison. (A) TH visits increased starting from 0 visits to a high of 65 visits 4 weeks after elective cases were suspended. This peak of TH visits (65 visits) coincided with the nadir of in-person visits (56 visits). TH visits steadily decreased to 5 visits after elective cases resumed. During the window of suspended cases, TH visits comprised 25% (322) of all visits and in-person visits comprised 75% (968 visits). The average total visits (in-person and TH combined) per week was 137 (95% confidence interval, 100–175) or 51% of baseline levels. (B) The number of in-person visits were lower during elective case suspension compared with when cases were resumed (P < 0.0001).
Telehealth Visits
Before the pandemic, no TH visits had occurred in our neurosurgery department. When cases were suspended, TH visits increased starting from 0 visits to a high of 65 visits 4 weeks after (see Figure 2A). This peak of TH visits (65 visits in a week) coincided with the nadir of in-person visits (56 visits in a week). TH visits steadily decreased to 5 visits 6 weeks after elective cases resumed (see Figure 2). During the window of suspended cases, TH visits comprised 25% (322) of all visits and in-person visits comprised 75% (968 visits). During this period, the average total visits (in-person and TH combined) per week was 137 (95% confidence interval, 100−175) or 51% of baseline levels (see Figure 2).
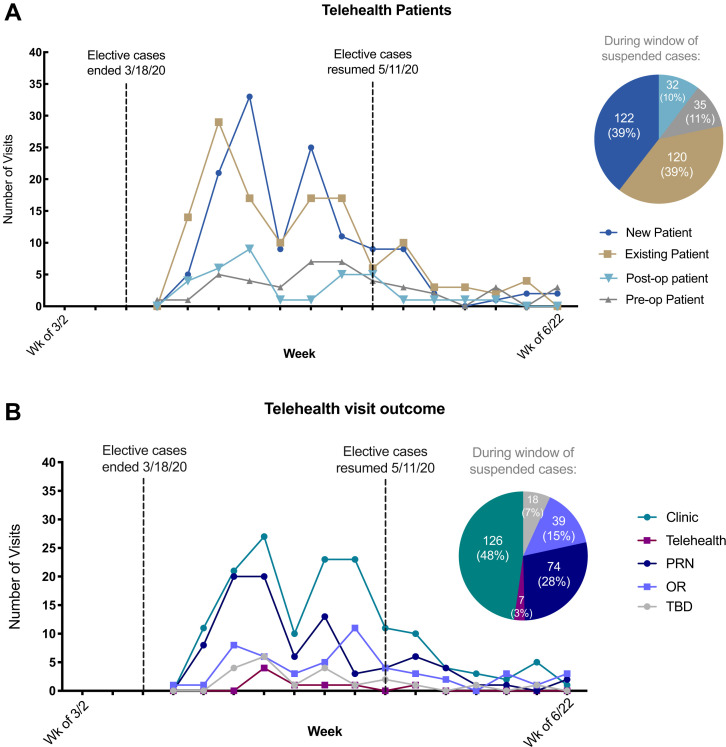
Telehealth Patient Type
TH patients were categorized into new patient, existing patient, postoperative patient, and preoperative patient. Existing patients were those who had TH visits that did not directly relate to preoperative or postoperative care. Existing patients were seen for nonurgent issues including a return of symptoms, follow-up after imaging, follow-up after a hospitalization, and evaluation to be a surgical candidate. The number of new patient TH visits peaked at 33 visits 3.5 weeks after cases were suspended (Figure 3A ). The number of existing patient TH visits peaked at 29 visits 2.5 weeks after cases were suspended. Postoperative patient visits peaked at 9 visits 3.5 weeks after cases were suspended. Preoperative patient visits peaked at 7 visits 5.5 weeks and 6.5 weeks after cases were suspended. TH visits of all types had decreased after the elective cases resumed eventually reaching 5 TH visits total 6 weeks after elective cases resumed. When elective cases were suspended, 39% (122) of TH visits were with new patients and 39% (120) were with existing patients. Eleven percent (35) were for preoperative visits, and 10% (32) were postoperative visits (Figure 3A).
Figure 3.
Breakdown of telehealth (TH) patient types and their visit outcomes. (A) New patient TH visits peaked at 33 visits, and existing patient TH visits peaked at 29 visits when cases were suspended. Postoperative patient visits peaked at 9 visits, and preoperative patient visits peaked at 7 visits after cases were suspended. TH visits of all types had decreased after the elective cases resumed. During case suspension, 39% (122) of TH visits were with new patients and 39% (120) were with existing patients. Eleven percent (35) were for preoperative visits, and 10% (32) were postoperative visits. (B) After a TH visit, 48% (126) of patients were referred to an in-person clinic visit, 28% (74) were PRN (no scheduled follow-up, could be seen on an as-needed basis), 15% (39) to the OR (scheduled for surgery), 7% (18) were to be determined (TBD), and 3% (7) were scheduled to have another TH visit.
Telehealth Visit Outcome
After a TH visit, 48% (126) of patients were referred to an in-person clinic visit, 28% (74) were PRN (no scheduled follow-up, could be seen on an as-needed basis), 15% (39) to the OR (scheduled for surgery), 7% (18) were to be determined (TBD), and 3% (7) were scheduled to have another TH visit (see Figure 3B). The pie chart reflects the window of time of elective case suspension (see Figure 3B).
Telehealth by Provider
Sixty-two percent (237) of TH visits were conducted by APPs and 37% (140) were physician visits (Figure 4A ). The neurosurgery department has 5 APPs who address nonurgent issues and follow-ups. There are 9 physicians in the subspecialties of spine, cerebrovascular, pediatrics, tumor, and functional neurosurgery.
Figure 4.
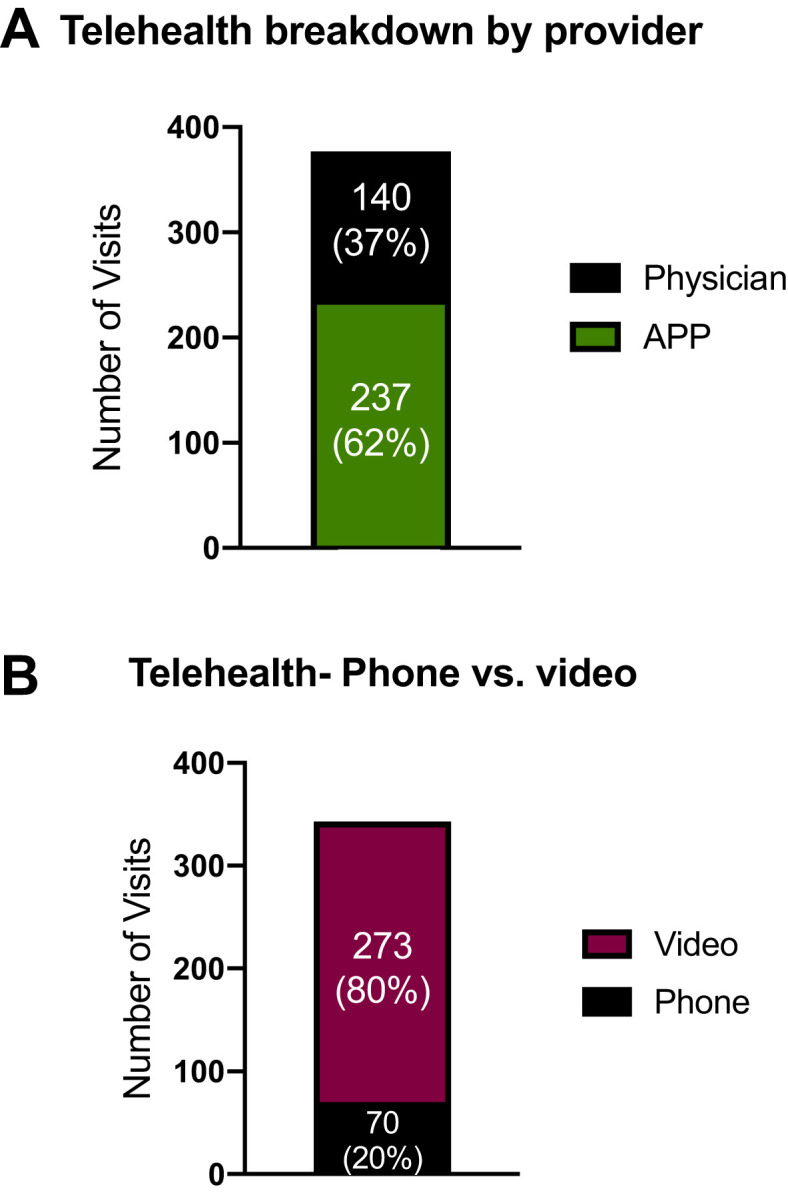
Breakdown of telehealth (TH) visits by provider and mode of visit. (A) TH by provider: Sixty-two percent (237) of TH visits were conducted by advanced practice providers and 37% (140) were by physicians. (B) Mode of TH visit: The vast majority of TH visits were through video (273, 80%).
Mode of Telehealth Visit
As we rapidly transitioned from no existing TH to greater TH use, we incorporated both phone-based and video-based options. The majority of TH visits were through video (273, 80%) (see Figure 4B). The greatest number of phone visits during a week was 22 visits, and the greatest number of video visits during a week was 50 visits (data not shown). Initially, phone calls were a prominent and straightforward means of providing TH, but as TH implementation advanced, video visits became the nearly exclusive means of providing TH, in part because of insurance reimbursement requirements.
Discussion
Our retrospective analyses show that neurosurgical case numbers dropped sharply due to the suspension of elective surgical cases and then steadily increased back to prepandemic levels after elective cases resumed 8 weeks after. In-person visits also decreased quickly in response to the suspension, and TH visits rose rapidly, then gradually decreased. TH visits continued to stay low as elective surgical cases resumed and volumes rebounded. Further evaluation revealed that almost half of all TH visits resulted in a recommendation for an in-person follow-up visit. Reasons for these follow-up visits included meeting the surgeon for a preoperative assessment, getting an updated neurologic examination, or following up after obtaining imaging or pain management procedures. After hospital restrictions were lifted, in-person visits resumed as the default mode of visit. By June 2020, in-person visits rebounded back to 98% of prepandemic baseline numbers and TH visits were minimally used in the neurosurgery department. Interestingly, the number of COVID-19 cases continued to increase in Kentucky9 and nationwide10 during this time. Surgical cases and in-person visits were back at baseline levels amid the pandemic, suggesting that patient concern about COVID-19 did affect in-person visits or surgery at this time.
The decline in surgical and clinic volumes was not surprising; however, we did not expect to see the rapid rise and fall of TH visits to such low levels following successful implementation and use. TH served as a temporary bridge when social distancing and quarantining was in effect. The finding that TH did not transform into a major mode of patient care stands in contrast to our university's neurology and psychiatry departments, where TH has been implemented and continues to play a substantial role in patient care. To explain the lack of sustained TH implementation in our department, we review some of the challenges of incorporating TH into clinical practice (Table 1 ).
Table 1.
Comparison of Telehealth and In-Person Visits
| In-Person Visit | Telehealth Visit | |
|---|---|---|
| Information conveyed | Results, full and minor assessments, medication, patient education Nonverbal cues easier to assess |
Results, minor assessments, visual assessments, medication, patient education Nonverbal cues may be limited or obscured, difficult to assess |
| Clinic workflow | Team effort is streamlined. Can meet in-person and consult with colleagues, trainees, support staff, advanced practice providers |
Team effort and consultation with colleagues less accessible |
This table summarizes the types of information conveyed in visits and clinic workflow.
For patients using TH, benefits include lessened travel time and time taken away from work to consult a health care provider. Many of our patients who live in rural parts of Kentucky drive at least 2 hours to be seen in person at our clinics. In a survey of patients using TH in pediatric surgery in which 97% of patients lived more than 200 km (124 miles) away from the surgical site, 48% of patients reported that the use of TH had a cost savings of $500–$70,000.11 These factors are especially important for increasing access for rural and underserved communities.12 Other benefits of TH include the ability to address time-sensitive medical issues quickly and fewer expensive follow-up visits and routine postoperative care.4 , 13 , 14 A pilot study demonstrated that telemedicine can be effective in elective neurosurgery.14 There was no difference in the rates of readmission and emergency department visits between those who had in-person versus TH visits 30 and 90 days postoperatively.14 In our experience, TH worked well for nonurgent and nonsurgical issues, such as prescribing or adjusting medication, physical therapy recommendations, and pain management. Sixty-three percent of providers for our TH visits during the window of suspension were APPs, who played a major role in addressing the nonurgent and follow-up needs for patients.
We recognized several obstacles in using TH in neurosurgery. Certain aspects of in-person clinic visits were difficult to replicate in video TH. For some neurosurgical subspecialties, such as movement disorders, the neurologic examination is relatively reliable in the video format. For other subspecialties, such as spine surgery, an in-person examination is necessary (e.g., to test strength). In contrast, in other neuroscience-based practices, such as neurology and psychiatry, there is not a great need to physically manipulate the patient with the exception of a specific set of neurologic maneuvers.15 Two studies in these fields show no significant differences in the diagnosis of dementia and no significant differences in scores from the Mini-Mental State Examination when comparing TH visits with in-person visits.16 , 17
Our physicians were more accustomed to running in-person clinics. Physicians stated that running an in-person clinic concurrently with TH visits was cumbersome and required additional planning for integration. During in-person clinics, providers can access several patients in different rooms, whereas with TH visits, 1 patient was attended to at a time sequentially. In-person clinics also provide a teamwork environment in which clinical staff could easily collaborate and consult with others, whereas with TH visits, the visit was often solely the physician or APP on the call. We found this also had a negative impact for learning opportunities for students and trainees.
From a scheduling and preparation standpoint, TH visits required extra communication with the staff related to verifying and facilitating computer and video capabilities, and for obtaining and uploading relevant imaging before the visit. Other neurosurgery practices during the pandemic experienced similar technical challenges.1
The challenges faced by patients with TH is that not all patients have a computer, tablet, or smartphone, or they may not have appropriate broadband for videoconferencing. Some patients also may not have the cognitive or technical skills to use their technology for a video call. Our experience has been that the vast majority of patients are able to make the TH video call, and those that report they cannot will often have a family member who lives close by who can assist them. Public health emergency assistance has also allowed limited use of audio-only phone calls aiding those who cannot do video calls.
Different institutions have different experiences with TH.7 Even subspecialties within neurosurgery have reported nuanced differences and successes in TH usage.18 Similar to our experience, TH was a convenient bridge during the pandemic but may not be desirable or sustainable in the long term. In 1 study, 88% percent of patient survey respondents agreed that the “telehealth visit was more convenient for them than an in-person visit,” but a smaller percentage (36%) would prefer a future TH visit.7 Some have proposed that it may be here to stay in the future and were more hopeful in implementing it.8 Viable long-term integration of TH will most likely involve the dedication of resources for the training of both providers and patients to reach its full potential.19
Overall, during the onset of the pandemic, we experienced substantial changes to our typical inpatient and outpatient workflows. Despite a rapid implementation of TH in an effort to continue to serve as many patients as possible, our neurosurgery practice eventually settled into the most efficient, default mode of practice, reverting back to almost all in-person clinic visits. In general, we found that TH was limited compared with in-person visits. This became even more evident as restrictions were lifted and our workflow began to normalize close to prepandemic numbers.
Conclusion
As we have now passed the third wave of COVID-19 cases, our practice continues to use TH on some occasions for patients, mostly to review imaging or initial postoperative or preoperative appointments where a physical examination is not necessary to make recommendations. However, most neurosurgery patients need a physical examination and imaging review to make recommendations on care, which is why our practice has reverted to almost all in-person visits.
CRediT authorship contribution statement
Monica J. Chau: Conceptualization, Data curation, Formal analysis, Writing - original draft, Visualization. Jorge E. Quintero: Conceptualization, Data curation. Ashley Guiliani: Data curation. Tripp Hines: Data curation, Formal analysis. Christopher Samaan: Data curation, Formal analysis, Visualization. Katie Seybold: Data curation. Matthew Stowe: Data curation, Writing - review & editing. Dean Hanlon: Data curation. Greg A. Gerhardth: Conceptualization, Supervision. Craig G. van Horne: Conceptualization, Supervision, Data curation.
Acknowledgments
We would like to acknowledge Brandon Miller for his manuscript feedback and Ryan Pennington and Elizabeth Means for their assistance in data retrieval.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Basil G.W., Eichberg D.G., Perez-Dickens M., et al. Letter: implementation of a neurosurgery telehealth program amid the COVID-19 crisis—challenges, lessons learned, and a way forward. Neurosurgery. 2020;87:E260–E262. doi: 10.1093/neuros/nyaa215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arnaout O., Patel A., Carter B., Chiocca E.A. Letter: adaptation under fire: two harvard neurosurgical services during the COVID-19 pandemic. Neurosurgery. 2020;87:E173–E177. doi: 10.1093/neuros/nyaa146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mouchtouris N., Lavergne P., Montenegro T.S., et al. Telemedicine in neurosurgery: lessons learned and transformation of care during the COVID-19 pandemic. World Neurosurg. 2020;140:e387–e394. doi: 10.1016/j.wneu.2020.05.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kahn E.N., La Marca F., Mazzola C.A. Neurosurgery and telemedicine in the United States: assessment of the risks and opportunities. World Neurosurg. 2016;89:133–138. doi: 10.1016/j.wneu.2016.01.075. [DOI] [PubMed] [Google Scholar]
- 5.Hall J.L., McGraw D. For telehealth to succeed, privacy and security risks must be identified and addressed. Health Aff (Millwood) 2014;33:216–221. doi: 10.1377/hlthaff.2013.0997. [DOI] [PubMed] [Google Scholar]
- 6.Tuckson R.V., Edmunds M., Hodgkins M.L. Telehealth. N Engl J Med. 2017;377:1585–1592. doi: 10.1056/NEJMsr1503323. [DOI] [PubMed] [Google Scholar]
- 7.Mohanty A., Srinivasan V.M., Burkhardt J.K., et al. Ambulatory neurosurgery in the COVID-19 era: patient and provider satisfaction with telemedicine. Neurosurg Focus. 2020;49:E13. doi: 10.3171/2020.9.FOCUS20596. [DOI] [PubMed] [Google Scholar]
- 8.De Biase G., Freeman W.D., Bydon M., et al. Telemedicine utilization in neurosurgery during the COVID-19 pandemic: a glimpse into the future? Mayo Clin Proc Innov Qual Outcomes. 2020;4:736–744. doi: 10.1016/j.mayocpiqo.2020.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.COVID-19 daily reports. 2020. https://chfs.ky.gov/Pages/cvdaily.aspx Available at:
- 10.Cases in the U.S. 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html Available at:
- 11.Shivji S., Metcalfe P., Khan A., Bratu I. Pediatric surgery telehealth: patient and clinician satisfaction. Pediatr Surg Int. 2011;27:523–526. doi: 10.1007/s00383-010-2823-y. [DOI] [PubMed] [Google Scholar]
- 12.Le S., Aggarwal A. The application of telehealth to remote and rural Australians with chronic neurological conditions. https://doi.org/10.1111/imj.14841 [e-pub ahead of print]. Intern Med J. [DOI] [PubMed]
- 13.Thakar S., Rajagopal N., Mani S., et al. Comparison of telemedicine with in-person care for follow-up after elective neurosurgery: results of a cost-effectiveness analysis of 1200 patients using patient-perceived utility scores. Neurosurg Focus. 2018;44:E17. doi: 10.3171/2018.2.FOCUS17543. [DOI] [PubMed] [Google Scholar]
- 14.Reider-Demer M., Raja P., Martin N., Schwinger M., Babayan D. Prospective and retrospective study of videoconference telemedicine follow-up after elective neurosurgery: results of a pilot program. Neurosurg Rev. 2018;41:497–501. doi: 10.1007/s10143-017-0878-0. [DOI] [PubMed] [Google Scholar]
- 15.Timpano F., Bonanno L., Bramanti A., et al. Tele-Health and neurology: what is possible? Neurol Sci. 2013;34:2263–2270. doi: 10.1007/s10072-012-1285-5. [DOI] [PubMed] [Google Scholar]
- 16.Cullum C.M., Weiner M.F., Gehrmann H.R., Hynan L.S. Feasibility of telecognitive assessment in dementia. Assessment. 2006;13:385–390. doi: 10.1177/1073191106289065. [DOI] [PubMed] [Google Scholar]
- 17.Ball C.J., Scott N., McLaren P.M., Watson J.P. Preliminary evaluation of a Low-Cost VideoConferencing (LCVC) system for remote cognitive testing of adult psychiatric patients. Br J Clin Psychol. 1993;32:303–307. doi: 10.1111/j.2044-8260.1993.tb01060.x. [DOI] [PubMed] [Google Scholar]
- 18.Basil G.W., Eichberg D.G., Perez-Dickens M., et al. Differences between neurosurgical subspecialties in telehealth adoption. World Neurosurg. 2021;146:e323–e327. doi: 10.1016/j.wneu.2020.10.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smith W.R., Atala A.J., Terlecki R.P., Kelly E.E., Matthews C.A. Implementation guide for rapid integration of an outpatient telemedicine program during the COVID-19 pandemic. J Am Coll Surg. 2020;231:216–222. doi: 10.1016/j.jamcollsurg.2020.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]