Abstract
Objective:
While guidelines recommend outpatient management of patients with low-risk pulmonary embolism (PE), little is known about the disposition of patients with PE diagnosed in United States emergency departments (EDs). We sought to determine disposition practices and subsequent health care utilization in patients with acute PE in U.S. EDs.
Methods:
This was a retrospective cohort study of adult ED patients with a new diagnosis of acute PE treated at 740 U.S. acute care hospitals from July 1, 2016, through June 30, 2018. The primary outcome was the initial disposition following an ED visit for acute PE. Additional measures included hospital cost and 30-day revisit rate to the ED.
Results:
A total of 61,070 cases were included in the overall cohort, of which 4.1% of new cases of PE were discharged from the ED. The median hospital-specific proportion of patients discharged was 3.1% (interquartile range = 0.8%–6.8%). The median odds ratio, representing the importance of the hospital in initial disposition decisions, was 2.21 (95% confidence interval = 2.05 to 2.37), which was greater than any patient-level factor with the exception of concurrent ED diagnosis of hypoxemia/respiratory failure, shock, or hypotension. Within 30 days of discharge, 17.9% of discharged cases had an ED return visit to the ED only and 10.3% of patients were hospitalized. Of the 30-day ED return visits in patients initially managed as outpatients, 1.3% had a bleeding-associated diagnosis.
Conclusion:
Despite guidelines promoting outpatient management, few patients are currently discharged home in the United States; however, practice varies widely across hospitals. Return visit rates were high but most did not result in hospitalization.
Pulmonary emboli (PEs) are commonly encountered in the emergency department (ED). Of the 145.6 million ED visits in the United States in 2016, over 180,000 ED patients received a diagnosis of PE in 2016.1,2 Although patients with PE have historically been admitted to the hospital for initial treatment, clinical trials have demonstrated the safety of treating carefully selected patients with acute PE as outpatients.3–8 Protocols to manage patients with acute PE as outpatients were introduced in the late 1990s and over the past 6 years, an increasing number of international society guidelines recommended outpatient treatment of ED patients with low-risk PEs.9–12 Low-risk PEs are typically characterized by hemodynamic stability, lack of significant cardiopulmonary comorbidities, and no evidence of cardiac strain or damage.13,14 This recommendation stems from the safety profile found in two randomized controlled trials and several observational studies, coupled with the concern about the cost of inpatient care and its associated risks.3–8,15,16
On the basis of prior studies, it has been estimated that 30% to 51% of patients diagnosed with acute PE may be suitable for outpatient management.17,18 These patients are generally those with low-risk PE who lack contraindications to anticoagulation and are able to reliably take anticoagulants and follow-up with outpatient clinicians.17 However, the reported prevalence of home discharge in the literature from the United States ranges from 1% to 8%, with some centers reporting rates of 25% to 50% following interventions intended to increase outpatient treatment.15,16,18 Further, while earlier trials have suggested that outpatient management of low-risk PE is safe, it is unclear whether similar results are being achieved in routine clinical practice.
Taking advantage of data from a large consortium of U.S. hospitals, we sought to describe current disposition practices and outcomes for adult patients presenting with acute PE. Additionally, we aimed to identify patient and hospital factors associated with the decision to discharge patients home with acute PE. We hypothesized that the rate of discharge from ED would be low and that the hospital a patient presented to would be a powerful determinant of disposition.
METHODS
Study Design and Setting
We conducted a retrospective cohort study using data from 740 acute care hospitals in the United States that contribute to the Premier Healthcare Database (PHD; Premier Inc.). The PHD is a product of Premier, Inc., a publicly traded company that is an alliance of more than 4,100 hospitals. The PHD is a comprehensive, voluntary database containing approximately 20% of all U.S. hospitalizations in a given year. In addition to the elements found in Uniform Billing 04 form, the PHD contains an itemized, day-stamped log of all items and services charged to the patient or the insurer, including medications, diagnostic and therapeutic services, and laboratory tests. Participating hospitals are drawn from all regions of the United States and compared with the overall makeup of U.S. hospitals, contributors are on average somewhat larger, are more often located in urban centers, and are more frequently engaged in teaching. Premier performs an iterative data validation and audit process, returning missing or invalid data to source hospitals for correction prior to final data validation and release; missing data are minimal.19,20 Access to the PHD was obtained by author PKL using funds from a grant from the National Heart, Lung, and Blood Institute (1K24HL132008–01). The institutional review board at Baystate Medical Center approved the study, which was not considered human subjects research because the data set does not contain any identifiable patient information. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.21
Selection of Participants
Patients were included in the overall cohort if they were 18 years or older, had an ED encounter between July 2016 and June 2018, and received a principal diagnosis of PE (International Classification of Diseases-10 [ICD-10] codes I26.01, I26.02, I26.09, I26.90, I26.92, I26.99). We implemented additional inclusion and exclusion criteria to overcome recognized limitations of administrative claims data. To increase the probability that patients included in the study represented those with acute PE, we restricted the cohort to cases that carried a Current Procedural Terminology code for diagnostic imaging for PE (computed tomographic pulmonary angiogram or ventilation–perfusion scan) as well as a pharmacy charge or ICD code indicating treatment of PE with anticoagulation or an inferior vena cava filter (Data Supplement S1, Table S2, available as supporting information in the online version of this paper, which is available at http://onlinelibrary.wiley.com/doi/10.1111/acem.14181/full).22–24 To restrict the cohort to individuals with a new diagnosis of PE, we excluded patients with PE-related visits in the 90 days prior to the index ED visit. Finally, because our study was focused on disposition decisions, we excluded a small number of patients (n = 25) who expired in the ED. For each patient, we recorded age, sex, race/ethnicity, primary payer, and concurrent diagnoses (Data Supplement S1, Table S3). Comorbidities were assessed using software developed by the Healthcare Cost and Utilization Project of the Agency for Healthcare Research and Quality (AHRQ). Additionally, we characterized hospitals according to size, teaching status, urban or rural population served, and census region.
Outcomes
Our primary outcome was the initial disposition from the ED. Patients were considered to be managed as an outpatient if the discharge location was home or a nursing/rehabilitation facility. We considered a patient to be hospitalized if they were admitted under observation or inpatient status or if they were transferred to an acute care hospital. Additional outcomes included costs and return visits to the ED or rehospitalization within 30 days. We used AHRQ Clinical Classification Software Diagnoses to categorize diagnoses associated with return visits to the ED and rehospitalization.25 Further, we used ICD-10 codes to identify return visits for chest pain, dyspnea, and bleeding (Data Supplement S1, Table S4). We used pharmacy charges to identify use of anticoagulant medications, excluding doses for prophylaxis of venous thromboembolism (Data Supplement S1, Table S5). Hospital costs were determined using the PHD charge master.
Data Analysis
Descriptive statistics including frequencies and percentiles for categorical factors and means and percentile distributions or medians and interquartile range (IQR) for continuous factors were used to examine the distribution of variables at the patient and hospital level and to describe the study population. We compared the characteristics of patients discharged with those patients admitted using absolute standardized differences; a difference greater than 10% is considered meaningful.26 A generalized linear mixed model with hospital-level random effects to account for patient clustering within hospitals was used to model PE discharge. Patient and hospital characteristics were included as fixed effects and were selected based on clinical grounds and prior literature and included patient demographics, comorbidities, concurrent diagnoses that would indicate severity of illness, and recent hospitalizations. For this analysis, we excluded patients treated at a hospital in which 0% of patients were discharged from the ED due to skew in distribution of random effects when many hospitals had 0% discharge. We assessed for correlation among model predictors using intraclass correlation (ICC). Consistent with multilevel modeling, we report median odds ratios (MOR) and 80% interval odds ratios (IOR-80%). The MOR quantifies the relative contribution of individual hospital practice patterns on outpatient management of PE in a manner allowing direct comparison to the impact of patient-level covariates.27,28 The IOR compares all pairs of individuals with the same admission covariates from hospitals with different characteristics. The IOR-80% reports the range of the central 80% of these paired ORs.28,29 For our study, the IOR-80% was calculated to show the impact of the predefined hospital variables on ED discharge by incorporating fixed-effect hospital factors.
In a separate analysis, we calculated hospital-specific discharge-home proportions for each institution, restricting this analysis to hospitals contributing at least 20 cases of acute PE during the study period, which provides more stable rate estimates. All analyses were conducted using SAS 9.4 (SAS Institute Inc.).
RESULTS
Characteristics of Study Subjects
A total of 61,070 cases met our inclusion criteria and were included in the analysis (Figure 1). Patient and hospital characteristics appear in Table 1. The most common comorbidities were hypertension (36,616 [60%]), chronic lung disease (15,497 [25.4%]), and obesity (15,077 [24.7%]). Overall 4.1% of cases were discharged from the ED to the outpatient setting. Of the patients discharged from the ED, 3.2% (n = 82) left against medical advice.
Figure 1.
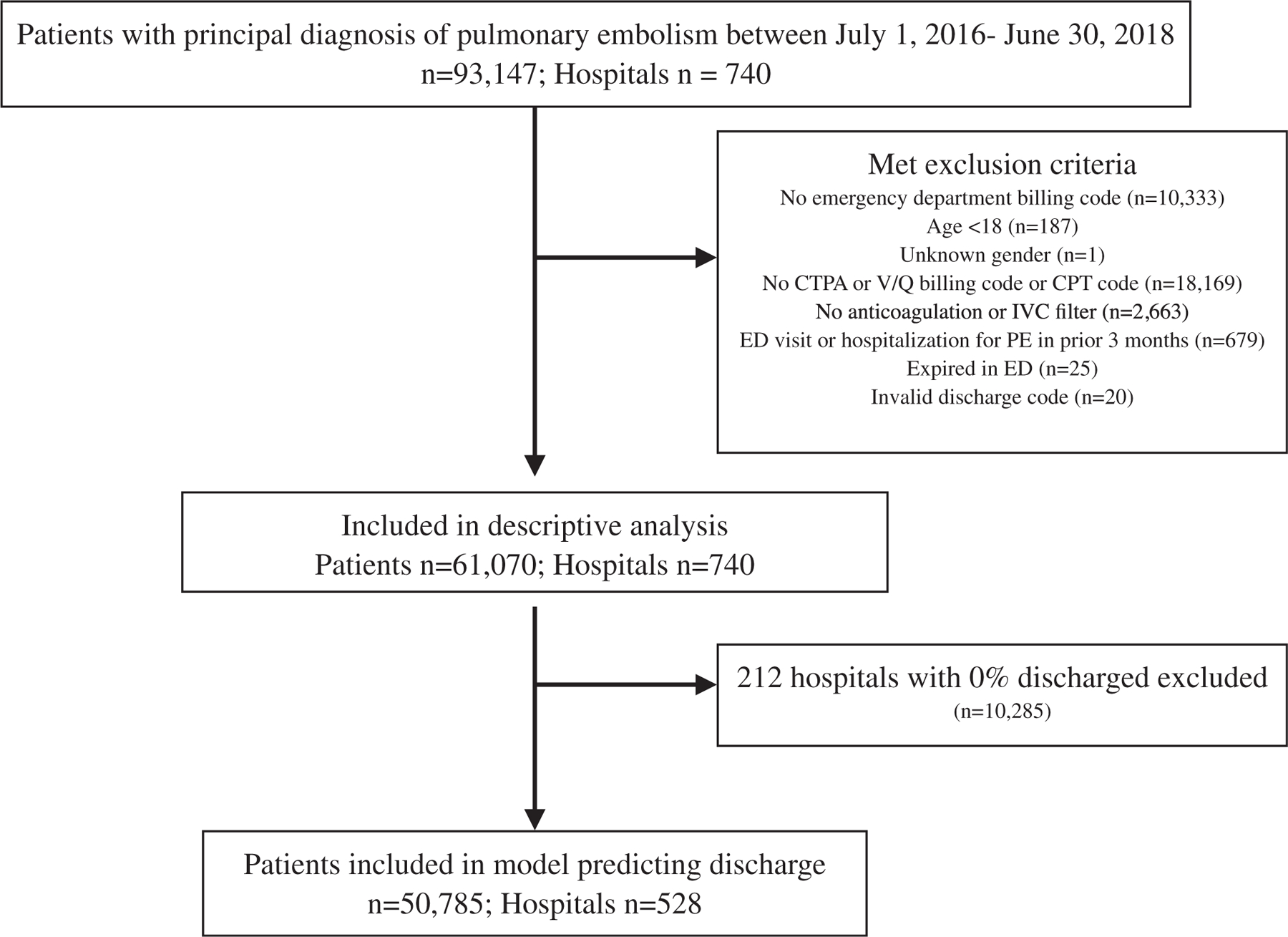
Study cohort flow. CPT = Current Procedural Terminology; CTPA = computed tomographic pulmonary angiogram; IVC = inferior vena cava; PE = pulmonary embolism; V/Q = ventilation–perfusion.
Table 1.
Characteristics of Patients Treated for Acute PE According to Initial Disposition
| Patient Characteristics | All Patients. N = 61,070 |
Outpatient Management, n = 2,530 (4.1%) |
Hospital Admission, n = 58,540 (95.9%) |
Absolute Standardized Difference |
|---|---|---|---|---|
| Age (years) | 61.6 (±16.8) | 53.7 (±16.8) | 62 (±16.7) | 0.495 |
| Female sex | 32,064 (52.5) | 1,320 (52.2) | 30,744 (52.5) | 0.007 |
| Race/ethnicity | ||||
| White | 44,021 (72.1) | 1,840 (72.7) | 42,181 (72.1) | 0.082 |
| Black | 10,393 (17) | 448 (17.7) | 9,945 (17) | |
| Other or unknown | 4,236 (6.9) | 177 (7) | 4,059 (6.9) | |
| Hispanic | 2,420 (4) | 65 (2.6) | 2,355 (4) | |
| Insurance status | ||||
| Medicare | 31,000 (50.8) | 811 (32.1) | 30,189 (51.6) | 0.406 |
| Private | 17,779 (29.1) | 1,055 (41.7) | 16,724 (28.6) | |
| Medicaid | 7,325 (12) | 387 (15.3) | 6,938 (11.9) | |
| Uninsured | 2,890 (4.7) | 164 (6.5) | 2,726 (4.7) | |
| Other/unknown | 2,076 (3.4) | 113 (4.5) | 1,963 (3.4) | |
| Comorbidities | ||||
| Chronic hypertension | 36,616 (60) | 810 (32) | 35,806 (61.2) | 0.611 |
| Chronic pulmonary disease | 15,497 (25.4) | 287 (11.3) | 15,210 (26) | 0.38.3 |
| Obesity | 15,077 (24.7) | 105 (4.2) | 14,972 (25.6) | 0.632 |
| Anemia | 10,303 (16.9) | 47 (1.9) | 10,256 (17.5) | 0.549 |
| Congestive heart failure | 8,601 (14.1) | 69 (2.7) | 8,532 (14.6) | 0.431 |
| Diabetes mellitus | 7,300 (12) | 197 (7.8) | 7,103 (12.1) | 0.146 |
| Diabetes mellitus with chronic complications | 6,526 (10.7) | 40 (1.6) | 6,486 (11.1) | 0.398 |
| Renal failure | 6,536 (10.7) | 58 (2.3) | 6,478 (11.1) | 0.357 |
| Coagulopathy | 3,865 (6.3) | 14 (0.6) | 3,851 (6.6) | 0.329 |
| Metastatic cancer | 3,762 (6.2) | 45 (1.8) | 3,717 (6.4) | 0.233 |
| Solid tumor without metastasis | 3,163 (5.2) | 71 (2.8) | 3,092 (5.3) | 0.126 |
| Liver disease | 2,341 (3.8) | 30 (1.2) | 211 (4) | 0.175 |
| Secondary diagnoses | ||||
| Hypoxemia or respiratory failure | 14,750 (24.2) | 38 (1.5) | 14,712 (25.1) | 0.742 |
| Anticoagulant use | 8,845 (14.5) | 316 (12.5) | 8,529 (14.6) | 0.061 |
| Heart failure | 8,499 (13.9) | 66 (2.6) | 8,433 (14.3) | 0.433 |
| Malignancy | 7,871 (12.9) | 127 (5) | 7,744 (13.2) | 0.288 |
| Hypotension | 2,353 (3.9) | 2 (0.1) | 2,351 (4) | 0.281 |
| Shock | 775 (1.3) | 0 (0) | 775 (1.3) | 0.164 |
| Hospitalization in past 30 days | 14,647 (24) | 524 (20.7) | 14,123 (24) | 0.081 |
| Imaging | ||||
| Computed tomographic pulmonary angiogram | 57,331 (93.9) | 2,444 (96.6) | 54,887 (93.8) | 0.133 |
| Ventilation–perfusion scan | 4,670 (7.7) | 91 (3.6) | 4,579 (7.8) | 0.183 |
| Treatment | ||||
| Anticoagulation | 61,062 (99.9) | 2529 (99.96) | 58,533 (99.99) | 0.017 |
| Enoxaparin | 36,342 (59.5) | 987 (39) | 35,355 (60.4) | 0.438 |
| Heparin | 32,846 (53.8) | 200 (7.9) | 32,646 (55.8) | 1.20 |
| Apixaban | 17,447 (28.6) | 576 (22.8) | 16,871 (28.8) | 0.139 |
| Warfarin | 15,000 (24.6) | 132 (5.2) | 14,868 (25.4) | 0.584 |
| Rivaroxaban | 14,957 (24.5) | 913 (36.1) | 14,044 (24) | 0.286 |
| IVC filter | 148 (0.2) | 3 (0.1) | 145 (0.3) | 0.048 |
Data are reported as mean (±SD) or n (%).
IVC = inferior vena cava; PE = pulmonary embolism.
Predictors of Disposition
Compared to patients who were admitted to the hospital, those managed as outpatients were more likely to be younger and privately insured and less likely to have had a hospitalization in the prior 30 days. The factors most strongly associated with the decision to not discharge patients with acute PE were a concurrent diagnosis of respiratory failure/hypoxia (OR = 0.06, 95% CI = 0.04 to 0.07), shock (OR = 0.17, 95% CI = 0.00 to 0.48), hypotension (OR = 0.07, 95% CI = 0.00 to 0.14), heart failure (OR = 0.24, 95% CI = 0.18 to 0.34), or malignancy (OR = 0.45, 95% CI = 0.36 to 0.53; Table 2). The overall ICC for the model was low, 0.21, suggesting that model factors were not highly correlated. Including patient- and hospital-level cofactors, the MOR for outpatient management computed from the model was 2.21 (95% CI = 2.05 to 2.37), greater than any patient-level factor with the exception of hypoxemia/respiratory failure, shock, and hypotension.
Table 2.
Factors Associated with Outpatient Treatment of Acute PE Among Patients Presenting to the ED
| Variable | Characteristic | OR (95% CI) |
|---|---|---|
| Age (every 10 years) | 0.84 (0.82–0.87) | |
| Sex | Female | Reference |
| Male | 1.00 (0.92–1.12) | |
| Race | White | Reference |
| Black | 1.0 (0.87–1.12) | |
| Hispanic | 0.71 (0.50–0.92) | |
| Other | 0.83 (0.67–0.99) | |
| Insurance | Medicare | Reference |
| Private | 1.27 (1.11–1.42) | |
| Uninsured | 1.09 (0.86–1.31) | |
| Other/unknown | 1.22 (1.00–1.47) | |
| Medicaid | 1.10 (0.92–1.27) | |
| Concurrent ED visit diagnoses | Hypoxemia or respiratory failure | 0.06 (0.04–0.07) |
| Shock | 0.17 (0.14–0.48) | |
| Hypotension | 0.07 (0.00–0.14) | |
| Syncope | 0.54 (0.34–0.74) | |
| Arrhythmia | 2.70 (0.50–4.90) | |
| Heart failure | 0.24 (0.18–0.30) | |
| Anticoagulant use | 0.87 (0.75–0.98) | |
| Malignancy | 0.45 (0.36–0.53) | |
| Admission in prior month, excluding PE | Yes | 0.90 (0.81–1.0) |
PE = pulmonary embolism.
Hospital-level Analysis
In the analysis of the 568 hospitals that had 20 or more cases of PE, the median proportion of patients discharged from the ED was 3.1%; however, the proportions varied from 0% to 13.0% at 10th and 90th percentiles (Figure 2). Hospital characteristics were not a strong predictor of the proportion of patients discharged from the ED (Table 3). The median proportion discharged at small hospitals was 7.5% (IQR = 3.2%–14.3%), higher than the proportion observed at medium (4%) and large-sized (3.1%) hospitals. In addition, the proportion of patients discharged from the ED was higher at rural hospitals (6.7%) compared with urban hospitals (4.4%). The proportion of patients managed as outpatients was highest in hospitals in the west (7.1%).
Figure 2.
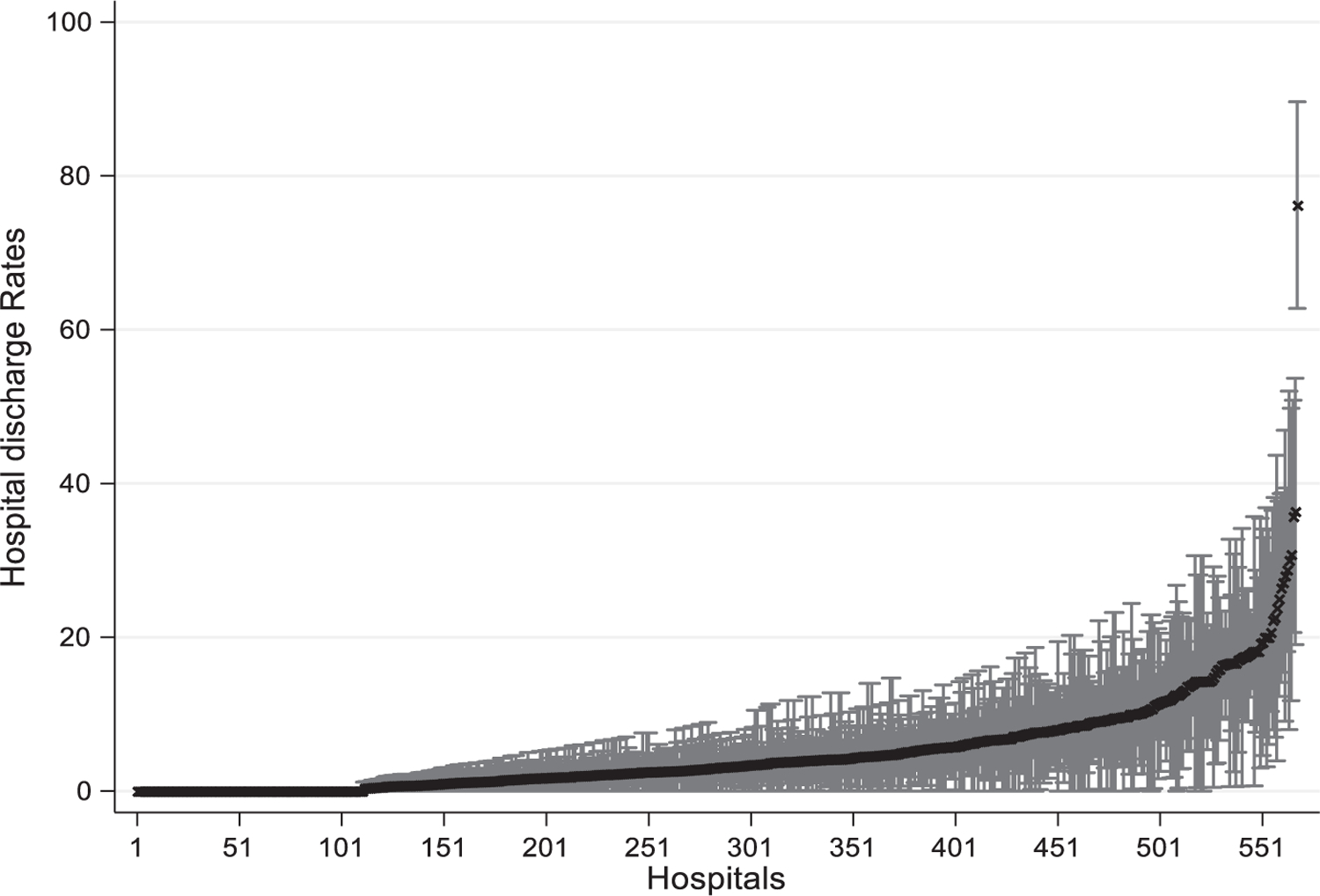
Point estimates represent the proportion of patients with acute PE discharged from the ED for the 568 individual hospitals with at least 20 cases of PE with error bars denoting 95% CIs. PE = pulmonary embolism.
Table 3.
Rates of Outpatient Treatment According to Hospital Characteristics
| Hospital Characteristic | Number of Hospitals (N = 528) | Median Outpatient Management Rate (IQR) | IOR-80% | |
|---|---|---|---|---|
| Lower | Upper | |||
| West | 115 | 7.1 (3.2–14.3) | Reference | |
| Midwest | 128 | 4.9 (2.4–10) | 0.15 | 3.02 |
| South | 223 | 4.4 (2.1–8.6) | 0.15 | 3.04 |
| Northeast | 62 | 4.2 (2.4–9.1) | 0.13 | 2.59 |
| Small (<200 beds) | 241 | 7.5 (4.2–14.3) | 0.53 | 11 |
| Medium (200–400 beds) | 160 | 4 (2–8.1) | 0.33 | 6.82 |
| Large (>400 beds) | 127 | 3.1 (1.6–5.1) | Reference | |
| Nonteaching hospital | 379 | 5.6 (2.5–11.1) | 0.19 | 3.86 |
| Teaching hospital | 149 | 4 (2.2–6.8) | Reference | |
| Rural | 129 | 6.7 (3.6–13) | 0.25 | 5.15 |
| Urban | 399 | 4.4 (2.2–9) | Reference | |
IQR = interquartile ratio; IOR-80% = 80% interval odds ratio.
Secondary Outcomes
The median hospital cost was $986 (IQR = $735–1,359) among patients discharged from the ED and $6,130 (IQR = $3,637–11,078) in admitted patients (Table 4). All-cause in-hospital mortality was 1.9% in admitted patients. Overall, 28.3% of patients discharged from the ED experienced a return visit to the ED or a hospital admission within 30 days of the index encounter. The most common reason for ED revisits among patients initially discharged from the ED were nonspecific chest pain (20.2%); pulmonary heart disease, which includes the diagnosis of PE (18.4%); and other lower respiratory tract diagnoses (12.6%). Among those initially discharged from the ED, 17.9% had an ED-only visit within 30 days and 10.3% were hospitalized. Among the 261 cases with a subsequent 30-day hospitalization, the most common diagnoses were related to PE (36.4%), nonspecific chest pain (3.8%), and gastrointestinal hemorrhage (3.8%). Overall, 1.3% of all patients discharged from the ED had a 30-day ED return visit with a diagnosis of bleeding and 1.2% resulted in hospitalization (Table 4).
Table 4.
Outcomes Among Patients with Acute PE Discharged From the ED
| Total Cohort N = 61,070 |
ED Discharge N = 2530 |
|
|---|---|---|
| Hospital charges in U.S. dollars (SD) | $9,225 ($12,634) | $1,214 ($1,186) |
| All-cause 30-day return visits to ED or hospitalizations among survivors (%) | 15,127 (25.2) | 715 (28.3) |
| ED revisit only | 7,217 (12.0) | 454 (17.9) |
| Hospital admission | 7,910 (13.2) | 261 (10.3) |
| Most common primary diagnoses for ED 30-day return visits | N = 9,065 | N = 555 |
| Nonspecific chest pain | 1,557 (17.2) | 112 (20.2) |
| Pulmonary heart disease (includes PE) | 853 (9.4) | 102 (18.4) |
| Other lower respiratory disease | 981 (10.8) | 70 (12.6) |
| Abdominal pain | 397 (4.4) | 24 (4.3) |
| Other connective tissue disease | 505 (5.6) | 41 (4.7) |
| 30-day ED return visits for select diagnoses | N = 9,065 | N = 555 |
| Chest pain | 2,293 (25.3) | 160 (28.8) |
| Shortness of breath | 2,342 (25.8) | 127 (22.9) |
| Bleeding | 762 (8.4) | 32 (5.8) |
| Most common primary diagnoses for 30-day hospitalizations | N = 7,910 | N = 261 |
| Pulmonary heart disease (includes PE) | 887 (11.2) | 95 (36.4) |
| Sepsis | 720 (9.1) | 9 (3.5) |
| Gastrointestinal hemorrhage | 309 (3.9) | 10 (3.8) |
| Nonspecific chest pain | 531 (6.7) | 10 (3.8) |
| Hypertension | 356 (4.5) | 7 (2.7) |
| Pneumonia | 317 (4.0) | 7 (2.7) |
| 30-day hospitalization for select diagnoses | N = 7,910 | N = 261 |
| Shortness of breath | 3,507 (44.3) | 83 (31.8) |
| Bleeding | 1,273 (16.1) | 30 (11.5) |
| Chest pain | 923 (11.7) | 34 (13.0) |
PE = pulmonary embolism.
DISCUSSION
In the overall cohort of more than 60,000 cases of acute PE from more than 700 U.S. EDs, we found that fewer than 5% were managed in the outpatient setting. As would be expected, the strongest predictors of admission versus discharge were the presence of concurrent diagnoses indicating severity of illness including hypoxemia, hypotension, heart failure, and syncope as well as the hospital to which a patient initially presented. However, outpatient management rates varied widely between institutions; indeed, the hospital where a patient presented was a strong predictor of a patient’s chance of being admitted versus discharged home. Similar to the figures reported in recent studies, just over one in four patients managed as an outpatient returned to the hospital within 30 days of the index encounter, and 10% of patients were ultimately admitted to the hospital.30 These findings emphasize the need for additional research to identify predictors for readmission as well as strategies to overcome barriers to outpatient management.
The evidence underpinning the management of low-risk PE in the outpatient setting is centered on two randomized controlled trials and several cohort studies.31 Based on these data, professional societies have recommended outpatient management of PE for these select patients.11,12,32,33 A study examining disposition of ED patients with a diagnosis of PE between 2006 and 2010 found that approximately 10% of patients in the United States were discharged home to be managed in the outpatient, rather than inpatient, setting; however, this analysis did not restrict the cohort to acute PEs.18 Interestingly, during this same time period in a Canadian province, just under 50% of patients with PE were managed as outpatients.34 Since then, several small studies examining disposition of PE in a total of four health care delivery systems have found that rates of discharge vary among individual EDs, but continue to average 8% to 10%.30,35
Our results confirm and extend these findings by examining disposition of acute PE in a much larger, more representative sample. Similar to earlier studies in the Unites States, we found that fewer than one in 20 patients with acute PE in the ED are managed as outpatients. These results are especially striking because prior investigators have estimated that some 30% to 51% of all patients with acute PE meet criteria for outpatient treatment.12,17,18 Like prior studies, we found that patients discharged from the ED had lower hospital costs.36 In addition to reduced cost burden for patients, increased discharge of patients with PE could help preserve hospital capacity for those patients who will truly benefit from hospitalization. These findings highlight a large opportunity to improve the value of care for patients with PE, while at the same time sparing patients unnecessary, costly, and oftentimes harmful hospital admissions.3,37
Unlike some prior studies that were limited to describing the experiences of individual hospital systems, we analyzed practices across more than 700 acute care hospitals spread across the United States. After adjusting for differences in case mix, we found that the hospital where a patient received care was one of the strongest predictors of whether they were managed in the outpatient setting. Institutional and regional factors such as local protocols and ability to establish outpatient follow-up may contribute to the geographic and hospital-level variation found in this analysis. These findings suggest that local context may play a role in disposition, signaling an area for future investigation. The low proportion of patients discharged with acute PE from the ED and variation in practices between hospitals calls attention to a potential gap in guideline implementation. Further implementation research, including understanding of the barriers and facilitators to the outpatient management of acute PE, is needed to address any potential gap.
Consistent with prior studies, we observed that only 1.3% of patients managed as outpatients experienced return visits for bleeding.31 This was reassuring because the outcomes achieved in clinical trials do not always translate into routine practice. We found that over 25% of patients discharged from the ED had an ED revisit or hospital admission within 30 days, which is only slightly higher than what has been reported in prior studies.6,38 Although high, relatively few of these visits resulted in hospital admission. Further, PE-related diagnosis represented the largest proportion of ED revisits and possible explanations for the high number of return visits include inadequate analgesia, persistent or worsening symptoms, patient fear or anxiety, or difficulties obtaining adequate follow-up. These findings may reflect a gap in the management of symptoms, follow-up, and the understanding of the expected course of PE and underscore the need for future research to understand the drivers of return visits and gaps in outpatient management.
LIMITATIONS
Our results should be interpreted in light of several limitations. First, we used ICD-10 codes to identify patients with acute PE. This approach may not be completely sensitive or specific but has been used by other investigators and shown to have acceptable sensitivity. To improve the specificity of acute PE diagnosis, we restricted the cohort to those who received diagnostic imaging and treatment. Second, because we did not have access to physiologic information, we were unable to determine whether an individual patient met low-risk criteria for outpatient management. However, we aimed to describe real-world patterns because eligibility for outpatient management may vary, depending on patient and clinician preferences and situations, from the criteria used in trials. Additionally, we only included patients with a principal diagnosis of PE. It is possible that some patients could have presented with an acute PE but received an alternative principal diagnosis, such as shock or respiratory failure. To the extent that we overlooked such cases, our estimates may have overestimated the true proportion of patient’s initially receiving outpatient management. A further limitation is that while we assessed hospitalization in the 30 days prior to the index encounter, we did not have information about hospital care received at other institutions. As such, we may have inadvertently included some patients in the study who had prior diagnoses of acute PE. Similarly, we were only able to measure 30-day return visits to the index hospital. Our retrospective study design can only identify associations and cannot account for unmeasured confounders and contributors. Finally, comorbidities are more likely to be coded in admitted patients rather than those discharged, which would cause the discharged patient to appear healthier. As a result, we were unable to incorporate a comorbidity score into the model.
CONCLUSIONS
In a large sample of U.S. hospitals, fewer than 5% of patients with an ED diagnosis of acute pulmonary embolism were discharged from the ED, a proportion that has not changed significantly in more than a decade, despite the publication of multiple guidelines endorsing discharge of patients with low-risk pulmonary embolism.18 Given the significant variation in discharge proportions between hospitals, these findings demonstrate a need to understand the organizational and contextual factors that contribute to this variability and to develop and test strategies to increase the outpatient management of low-risk PE in eligible patients.
Supplementary Material
Data Supplement S1. Supplemental material.
Acknowledgments
The project described was supported by the National Heart, Lung, and Blood Institute through grant 1K12HL138049-01. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. PKL is supported by K24 HL132008: Research and Mentoring in Comparative Effectiveness and Implementation Science.
Footnotes
Accepted for presentation at Society for Academic Emergency Medicine Annual Meeting, Denver, CO, May 2020. Conference canceled due to COVID-19 pandemic.
The authors have no potential conflicts to disclose.
Supporting Information
The following supporting information is available in the online version of this paper available at http://onlinelibrary.wiley.com/doi/10.1111/acem.14181/full
References
- 1.HCUPnet, Healthcare Cost and Utilization Project. Rockville, MD: Agency for Healthcare Research and Quality, c2020. Available at: https://hcupnet.ahrq.gov/#setup. Accessed Jul 20, 2020. [PubMed] [Google Scholar]
- 2.Rui P, Kang K, Ashman J. National Hospital Ambulatory Medical Care Survey: 2016 Emergency Department Summary Tables. 2016. Available at: https://www.cdc.gov/nchs/data/nhamcs/web_tables/2016_ed_web_tables.pdf. Accessed Jul 20, 2020.
- 3.Aujesky D, Roy PM, Verschuren F, et al. Outpatient versus inpatient treatment for patients with acute pulmonary embolism: an international, open-label, randomised, non-inferiority trial. Lancet 2011;378:41–8. [DOI] [PubMed] [Google Scholar]
- 4.Peacock W, Coleman CI, Diercks DB, et al. Emergency department discharge of pulmonary embolus patients. Acad Emerg Med 2018;25:995–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Piran S, Le Gal G, Wells PS, et al. Outpatient treatment of symptomatic pulmonary embolism: a systematic review and meta-analysis. Thromb Res 2013;132:515–9. [DOI] [PubMed] [Google Scholar]
- 6.Bledsoe JR, Woller SC, Stevens SM, et al. Management of low-risk pulmonary embolism patients without hospitalization: the Low-Risk Pulmonary Embolism Prospective Management Study. Chest 2018;154:249–56. [DOI] [PubMed] [Google Scholar]
- 7.Vlasveld LT, Eijsvogel M, Faber LM, et al. Efficacy and safety of outpatient treatment based on the hestia clinical decision rule with or without N-terminal pro–brain natriuretic peptide testing in patients with acute pulmonary embolism. A randomized clinical trial. Am J Respir Crit Care Med 2016;194:998–1006. [DOI] [PubMed] [Google Scholar]
- 8.Malfante PC, Di Micco P, Jiménez D, et al. Identification of low-risk patients with acute symptomatic pulmonary embolism for outpatient therapy. Ann Am Thorac Soc 2015;12:1122–9. [DOI] [PubMed] [Google Scholar]
- 9.Wells PS, Ginsberg JS, Anderson DR, et al. Use of a clinical model for safe management of patients with suspected pulmonary embolism. Ann Intern Med 1998;129:997–1005. [DOI] [PubMed] [Google Scholar]
- 10.Howard LS, Barden S, Condliffe R, et al. British Thoracic Society guideline for the initial outpatient management of pulmonary embolism. BMJ Open Respir Res 2018;5: e000281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Konstantinides SV, Torbicki A, Agnelli G, et al. 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J 2014;35:3033–80. [DOI] [PubMed] [Google Scholar]
- 12.Wolf SJ, Hahn SA, Nentwich LM, Raja AS, Silvers SM, Brown MD. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with suspected acute venous thromboembolic disease. Ann Emerg Med 2018;71:e59–109. [DOI] [PubMed] [Google Scholar]
- 13.Aujesky D, Obrosky DS, Stone RA, et al. Derivation and validation of a prognostic model for pulmonary embolism. Am J Respir Crit Care Med 2005;172:1041–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jiménez D Simplification of the pulmonary embolism severity index for prognostication in patients with acute symptomatic pulmonary embolism. Arch Intern Med 2010;170:1383. [DOI] [PubMed] [Google Scholar]
- 15.Vinson DR, Mark DG, Chettipally UK, et al. Increasing safe outpatient management of emergency department patients with pulmonary embolism. Ann Intern Med 2018;169:855–65. [DOI] [PubMed] [Google Scholar]
- 16.Vinson DR, Ballard DW, Huang J, et al. Outpatient management of emergency department patients with acute pulmonary embolism: variation, patient characteristics, and outcomes. Ann Emerg Med 2018;72:62–72.e3. [DOI] [PubMed] [Google Scholar]
- 17.Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest 2016;149:315–52. [DOI] [PubMed] [Google Scholar]
- 18.Singer AJ, Thode HC, Peacock W. Admission rates for emergency department patients with venous thromboembolism and estimation of the proportion of low risk pulmonary embolism patients: a US perspective. Clin Exp Emerg Med 2016;3:126–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Premier Healthcare Database White Paper: Data That Informs and Performs. 2020. Available at: https://products.premierinc.com/downloads/PremierHealthcareDatabaseWhitepaper.pdf. Accessed Jul 20, 2020.
- 20.Schneeweiss S, Seeger JD, Landon J, Walker AM. Aprotinin during coronary-artery bypass grafting and risk of death. N Engl J Med 2008;358:771–83. [DOI] [PubMed] [Google Scholar]
- 21.von Elm E, Altman DG, Egger M. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE). Ann Intern Med 2007;147:573–7. [DOI] [PubMed] [Google Scholar]
- 22.Casez P, Labarère J, Sevestre MA, et al. ICD-10 hospital discharge diagnosis codes were sensitive for identifying pulmonary embolism but not deep vein thrombosis. J Clin Epidemiol 2010;63:790–7. [DOI] [PubMed] [Google Scholar]
- 23.Alotaibi GS, Wu C, Senthilselvan A, McMurtry MS. The validity of ICD codes coupled with imaging procedure codes for identifying acute venous thromboembolism using administrative data. Vasc Med 2015;20:364–8. [DOI] [PubMed] [Google Scholar]
- 24.Öhman L, Johansson M, Jansson JH, Lind M, Johansson L. Positive predictive value and misclassification of diagnosis of pulmonary embolism and deep vein thrombosis in Swedish patient registries. Clin Epidemiol 2018;10: 1215–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Clinical Classifications Software (CCS) for ICD-10-PCS (beta version). Rockville, MD: Agency Healthcare Research and Quality, 2019. Available at: https://www.hcup-us.ahrq.gov/toolssoftware/ccs10/ccs10.jsp. Accessed Jul 25, 2019. [Google Scholar]
- 26.Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput 2009;38:1228–34. [Google Scholar]
- 27.Merlo J, Chaix B, Ohlsson H, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epidemiol Community Health 2006;60:290–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sanagou M, Wolfe R, Forbes A, Reid C. Hospital-level associations with 30-day patient mortality after cardiac surgery: a tutorial on the application and interpretation of marginal and multilevel logistic regression. BMC Med Res Methodol 2012;12:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Merlo J, Chaix B, Ohlsson H, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: Using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epidemiol Community Health 2006;60:290–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fang MC, Fan D, Sung SH, et al. Outcomes in adults with acute pulmonary embolism who are discharged from emergency departments. JAMA Intern Med 2015;175: 1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Maughan BC, Frueh L, McDonagh MS, Casciere B, Kline JA. Outpatient treatment of low-risk pulmonary embolism in the era of direct oral anticoagulants: a systematic review. Acad Emerg Med 2020;53:xxx–xx. [DOI] [PubMed] [Google Scholar]
- 32.Raja AS, Greenberg JO, Qaseem A, Denberg TD, Fitterman N, Schuur JD. Evaluation of patients with suspected acute pulmonary embolism: best practice advice from the Clinical Guidelines Committee of the American College of Physicians. Ann Intern Med 2015;163:701–11. [DOI] [PubMed] [Google Scholar]
- 33.Konstantinides SV, Meyer G, Becattini C, et al. 2019 ESC guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Respir J 2019;54:1901647. [DOI] [PubMed] [Google Scholar]
- 34.Mansour S, Alotaibi G, Wu C, McMurtry MS. Trends in admission rates and in-hospital stay for venous thromboembolism. Thromb Res 2017;156:149–54. [DOI] [PubMed] [Google Scholar]
- 35.Vinson DR, Ballard DW, Huang J, et al. Outpatient management of emergency department patients with acute pulmonary embolism: variation, patient characteristics, and outcomes. Ann Emerg Med 2018;72:62–72.e3. [DOI] [PubMed] [Google Scholar]
- 36.Fanikos J, Rao A, Seger AC, Carter D, Piazza G, Goldhaber SZ. Hospital costs of acute pulmonary embolism. Am J Med 2013;126:127–32. [DOI] [PubMed] [Google Scholar]
- 37.Zongdag W, Mos IC, Creemers-Schild D, et al. Outpatient treatment in patients with acute pulmonary embolism: the Hestia Study. J Thromb Haemost 2011;9:1500–7. [DOI] [PubMed] [Google Scholar]
- 38.Fang MC, Fan D, Sung SH, et al. Treatment and outcomes of acute pulmonary embolism and deep venous thrombosis: the Cardiovascular Research Network Venous Thromboembolism (CVRN VTE) Study. Am J Med 2019;132:1450–7.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Supplement S1. Supplemental material.


