ABSTRACT
Novel Coronavirus disease (COVID-19) has been widely described as the cause for a proinflammatory and hypercoagulable state.
The inflammatory process involving the alveolar vascular endothelium in the respiratory system, is a determining factor for the onset of primary Pulmonary Artery Thrombosis (PAT) even in patients with heparin prophylactic treatment.
Little is known about the efficacy of the anticoagulant therapy during the course of PAT caused by COVID-19.
In this paper we describe the results obtained in patients with moderate COVID-19 disease, previously threated with prophylactic enoxaparin, who then received full Anticoagulant treatment after diagnosis of PAT.
After three months Computed Tomography Pulmonary Angiography demonstrated a complete resolution of the vascular obstructive lesions in all patients, while all the coagulation tests were normal.
Dear Editor,
since the winter of 2019, there has been a rapid spread of the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2 virus) leading to a global pandemic [1].
Novel Coronavirus (COVID-19) has been well described as the cause of a proinflammatory and hypercoagulable state [2]. The direct viral cytopathic effect in conjunction with its ability to overcome the immune responses causes the disease severity. On the other hand, the aberrant host immune response determines an enhanced inflammatory response [3].
Inflammation promotes thrombosis through the activation of the lympho-monocytes, the alteration of the endothelium and the anticoagulant pathways. The Cytokine Storm (CS) is an uncontrolled release of cytokines (Interleukins IL, Interferons IFN, Tumor Necrosis Factor TNF, Colony Stimulating Factors CSF, chemokines CK, and growth factors GF), with systemic hyper-inflammation and coagulation activation [4]. Coagulation’s disorders in patients with Covid19- are frequent, and characterized by a platelets (PLT) reduction, prolonged prothrombin time (PT) and increased D-Dimer. Patients with a severe disease, as those who were admitted to the Intensive Care Unit (ICU) or died, showed the most important alterations [5].
In the respiratory system there is a lung-specific coagulation system, called broncho-alveolar hemostasis. In healthy subjects, the coagulation-fibrinolysis balance is shifted towards fibrinolysis, while in patients with COVID-19 this is shifted towards a procoagulant effect in order to limit the viral invasion [6]. Dolhnikof et al. showed a high frequency of pulmonary microthrombosis in patients who underwent minimally invasive autopsies [7].
In the lung, even in the early stages, inflammation involves the alveolar vascular endothelium, causing the formation of pulmonary micro-thrombosis which worsen the respiratory failure. These microthrombi are not detected by Computed Tomography Pulmonary Angiography (CTPA) due to their small dimensions and their distal location. As the underlying diseases worsen, the thrombotic process become extensive and systemic as to determine Deep Vein Thrombosis (DVT) or Pulmonary Embolism (PE) [8]. It is possible that conventional heparin prophylaxis may not be sufficient to prevent those thrombotic manifestations that are mostly related to an excessive inflammatory response. [9,10]
In a previous paper, we described nine of 138 patients admitted to our Institution between March 2020 and May 2020, with COVID 19 and Pulmonary Artery Thrombosis (PAT) without DVT [11].
All the patients received thrombosis prophylaxis with enoxaparin 4000 U/day (6000 U/day for patients with a Body Weight > 100 kg). After the diagnosis of PAT, all of them received enoxaparin at anticoagulant dose. During the follow up, six patients started Direct Oral Anticoagulant treatment (DOAC) while three maintained enoxaparin.
After three months, we prescribed laboratory examination and radiological investigations for all patients to evaluate the resolution of the PAT.
All the coagulation tests (D Dimer, PLT, PTT, PT, fibrinogen) were normal (Table 1). Lower limbs Doppler Ultrasound (DU) did not demonstrate any signs of DVT, while CTPA documented the complete resolution of the arterial thrombotic lesions in all patients (Figure 1(a,b)).
Table 1.
Laboratory exams during the admission and after three months
| At admission | After 5 days | After 10 days | After three months (*) | |
|---|---|---|---|---|
| C-reactive proteine (mg/l) | 54.6±58.1 | 54.6±58.1 | 49.5± 27.6 | 23.7 ± 9.2 |
| Lymphocite (MMC) | 1260 ± 414.5 | 1075 ± 219.2 | 1290 ± 336.7 | 1319 ± 276.1 |
| Platelets (MMC) | 263,000 ± 147,000 | 252,800 ± 52,900 | 289,000 ± 113,000 | 388,000 ± 34,700 |
| Fibrinogen (mg/dl) | 530 ± 121.6 | 426,0 ± 14.1 | 466,1 ± 142.1 | 567,3 ± 97.5 |
| Ldh (u/l) | 326.2 ± 121.9 | 314.5 ± 37.5 | 309 ± 63.7 | 275.1 ± 38.2 |
| Inr | 1.1 ± 0.01 | 1.05 ± 0.1 | 1.1 ± 0.1 | 1.02/- 0.1 |
| D-dimer ug/l | 627.4 ± 178.6 | 2143.6 ± 327.5 | 1764.9 ± 227.5 | 236 ± 68.3 |
Figure 1.
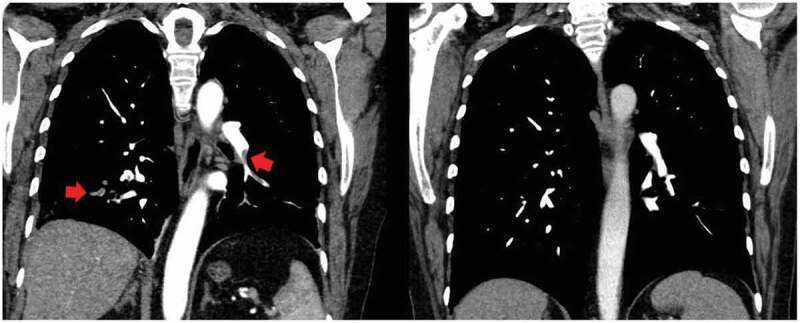
(a) Pulmonary artery thrombosis (red arrows). (b) complete resolution of the thrombosisCTPA documented the complete resolution of the arterial thrombotic lesions in all patients
Regarding PE unrelated to COVID 19, much is known about risk factors, pathophysiology, and appropriate diagnostic strategies. Nevertheless, the evidence about the subsequent changes in clot burden that occur in pulmonary arteries after diagnosis and during treatment is scant [12]. The rate of clot resolution observed in studies using CTPA was: 47–56.7% at 14–21 days, 77–78%% at 22–90 days and 84–94% after 90 days [13,14]. The major predictor of incomplete resolution was a larger artery involvement. Peripheral clots tend to resolve completely and earlier compared to central clots at follow-up with Computed Tomography, reaching a 92.8% resolution rate at the 15–28 days interval in one study [15].
PAT in COVID 19 represents a condition strictly related to the inflammatory process involving the alveolar vascular endothelium and can occur also in patients on prophylactic therapy with heparin. After the diagnosis patients are treated with full dose of anticoagulants with the intention of reducing the extent of the thrombotic lesion and facilitating vascular reperfusion. Unlike non COVID 19 PE, little is known about the efficacy of anticoagulant therapy in patients with vascular thrombosis and in PAT in particular. In this paper we re-evaluated after three months six COVID 19 patients with PAT treated with anticoagulant therapy: CTPA demonstrated a complete resolution of the vascular obstructive lesions. To the best of our knowledge this is the first report evaluating this condition. Further studies with larger numbers of patients will be needed to better define this first observation
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- [1].Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Connors JM, Levy JH.. Thromboinflammation and the hypercoagulability of COVID‐19. J Thromb Haemost. 2020;18(7):1559–1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Terpos E, Ntanasis-Stathopoulos I, Elalamy I, et al. Ematological findings and complications of COVID-19. Am J Ematol. 2020;95(7):834–847. 10.1002/ajh.25829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Resp Med. 2020;8(4):420–422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Tang N, Bai H, Chen X, et al. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019. patients with coagulopathy. J Thromb Haemost. 2020;18(5):1094–1099. DOI: 10.1111/jth.14817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Glas GJ, Van Der Sluijs KF, Schultz MJ, et al. Bronchoalveolar hemostasis in lung injury and acute respiratory distress syndrome. J Thromb Haemost. 2013;11:17–25. [DOI] [PubMed] [Google Scholar]
- [7].Dolhnikoff M, Duarte-Neto AN, De Almeida Monteiro RA, et al. Pathological evidence of pulmonary thrombotic phenomena in severe COVID-19. J Thromb Haemost. 2020. DOI: 10.1111/jth.14844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Thachil J, Cushman M, Srivastava A. A proposal for staging COVID-19 coagulopathy. Res Pract Thromb Haemost. 2020;4:731–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Cattaneo M, Bertinato EM, Birocchi S, et al. Pulmonary embolism or pulmonary thrombosis in COVID-19? Is the recommendation to use high-dose heparin for thromboprophylaxis justified? Thromb Haemost. 2020. [in press]. DOI: 10.1055/s-0040-1712097Fogarty [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Maatman TK, Jalali FC, Douglas A, et al. Routine venous thromboembolism prophylaxis may be inadequate in the hypercoagulable state of severe coronavirus disease 2019. Crit Care Med. 2020;48(9):e783–e790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Graziani A, Domenicali M, Zanframundo G, et al. Pulmonary artery thrombosis in patients with COVID 19. Pulmonol. 2020. DOI: 10.1016/j.pulmoe.2020.07.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Nijkeuter M, Hovens MC, Davidson BL, et al. Resolution of thromboemboli in patients with acute pulmonary embolism: a systematic review. Chest. 2006;129(1):192–197. [DOI] [PubMed] [Google Scholar]
- [13].Aghayev A, Furlan A, Patil A, et al. The rate of resolution of clot burden measured by pulmonary CT angiography in patients with acute pulmonary embolism. AJR Am J Roentgenol. 2013;200(4):791–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Den Exter PL, Van Es J, Ljm K, et al. Prometheus follow-up investigators. Thromboembolic resolution assessed by CT pulmonary angiography after treatment for acute pulmonary embolism. Thromb Haemost. 2015;114(1):26–34. . [DOI] [PubMed] [Google Scholar]
- [15].Choi KJ, Cha SI, Shin KM, et al. Factors determining clot resolution in patients with acute pulmonary embolism. Blood Coagul Fibrinolysis. 2016;27(3):294–300. [DOI] [PubMed] [Google Scholar]


