Abstract
Background:
India has one of the largest numbers of doctors in the world. It is estimated that more than 1 million doctors are in India. Every year more than 80,000 medical students graduate as doctors from 529 medical colleges in India. Medical profession is considered as more stressful, but mental health is still a subject of taboo in medical profession in Indian context. Doctors have higher suicide risk, 2.5 times more than the general population. In the United Kingdom, 430 doctors committed suicide between the years 2011 and 2015. Even though suicide among doctors is reported in Indian media, there is hardly any scientific study that has looked into the suicide among Indian doctors because of many hurdles in the collection of information.
Materials and Methods:
All the Indian newspaper that are published in English and are available in the online platform were scrutinized on doctors suicide report from the year 2016 March to 2019 March.
Results:
Thirty suicides were reported between 2016 March and 2019 March, out of which 18 were female and 12 male. More than 80% were younger than 40 years. Twenty-two were from medical education institutions. Seventeen were from south India and 13 from North India. Eight were MBBS students and ten were postgraduate students. Among subspecialties, six doctors were from Anesthesia. Seventeen used hanging as a method for suicide, eight used medications, and five jumped from building to end life. Nineteen of suicide reports about doctors mentioned that they were depressed.
Conclusion:
Suicide among Indian doctors is concern. Majority are young undergraduate and postgraduate medical students. Female doctors were more than male doctors. Most doctors were reported to be depressed and used lethal method such as hanging and medications.
Keywords: Doctors suicide, Indian doctors, mental health, suicide
INTRODUCTION
India has one of the largest numbers of doctors in the world. It is estimated that more than 1 million doctors are in India.[1] Every year more than 80,000 medical students graduate as doctors from 529 medical colleges in India. The new medical curriculum like the earlier has not incorporated single skill in psychiatry as mandatory in examinations for MBBS graduates to become doctors in India.[2] This adversely affects mental health awareness among budding doctors. Medical profession is considered as more stressful, but mental health issues continue to be a subject of taboo in medical profession in the Indian context. Doctors have higher suicide risk, 2.5 times more than the general population. In the United Kingdom, 430 doctors committed suicide between the years 2011 and 2015.[3] In China, 51 doctors committed suicide between the years 2008 and 2016.[4] Even though suicide among doctors is reported in Indian media, there is hardly any scientific study that has looked into the suicide among Indian doctors because of many hurdles in the collection of information, particularly stigma associated with suicide and lack of centralized information collection either by professional bodies such as Indian Medical Association (IMA) or Medical Council of India (or current National Medical Commission).
Mental disorders are among leading cause of nonfatal disease burden in India with over 197 million people affected of varying severity in 2017, out of which more than 45 million had depressive disorders and another 44 million had anxiety disorders.[5] Suicide is major concern in India, in the year 2018, the number of suicides was 134,516.[6] It is important to consider these factors in Indian scenario; because doctors as human beings are not immune from mental health issues or suicide. As an occupation, doctors have 80% lower risk of suicide compared to other occupation such as farmers but higher risk compared to teachers.[7] However, suicidal ideation among medical students is high and ranges from 1.8% to 53.6%.[8] Some of the issues that increase the risk for doctors are substance use, poor coping skills, burnout, financial debts, litigations, and perceived stigma associated with seeking help. There has been some studies that have looked at personalities of doctors that might increase the risk for mental health issues such as doubt, guilt feeling, exaggerated sense of responsibility, perfectionism, excessive devotion to work, and unable to take leisure time.[9,10] Considering the vulnerability of the profession, some countries have annual assessment and report from the medical trainees and trainers on many issues including mental health.[11] They also have confidential service for general practitioners and trainees. The mental health issue of doctors also has been taken up at annual international practitioner health summit conference; in the year 2018 at London, with the theme was “The wounded healer.”[12] However, such efforts in India are nonexistent. The serious issue of suicide among Indian doctors needs research for preventive measures; hence, this study is one such effort.
MATERIALS AND METHODS
After obtaining institution ethics committee, all the Indian newspaper published in English that are available in the online platform were scrutinized by four authors independently for suicide reports among doctors from the year March 2016 to March 2019. The key words used were Suicide, Doctor, Resident, Medico, and Death. Only those completed suicides of individuals belonging to allopathic medicine were included. Parasuicide or deliberate self-harms were excluded. The ethics committee was informed that the confidentiality shall be maintained about name of individual doctor and the specific institution or workplace of the individual. Furthermore, the city where the suicide act was committed shall not be disclosed.
RESULTS
In thirty suicides that were reported, 18 (60%) were female doctors and 12 (40%) were male doctors [Figure 1]. Age ranged from 19 years to 57 years and 20 (67%) were aged <30 years [Figure 2]. Between March 2016 and March 2019, 12 suicides reported each in 2017–2018 and 2018–2019. Six suicides in 2016–2017 [Figure 3], the regional distribution of suicides was near equal, 17 (57%) were south India, and 13 (43%) from North India [Figure 4]. Twenty-two (73%) were from medical education institutions. Eight (26%) were MBBS students, Ten (33%) were postgraduate students, and 12 working doctors [Figure 5]. Seventeen (57%) used hanging as a method for suicide, 8 (26%) used medications as lethal injections, 5 (17%) jumped from building to end life, and one killed in front of train [Figure 6]. Nineteen (63%) of suicide reports about doctors mentioned that they were depressed. Reports mention two doctors had written suicide note and two others were taking treatment for depression, one of the doctors had attempted twice. Marital discord was reported as reason for six suicides and in three; harassment was mentioned as the reason [Figure 7]. Among different subspecialties; six doctors belonged to anesthesia, three from dermatology, two from radiology [Figure 8].
Figure 1.
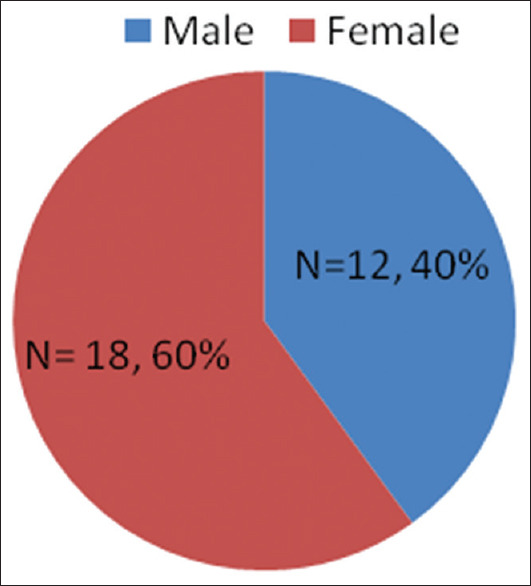
Gender distribution of doctors who committed suicide
Figure 2.
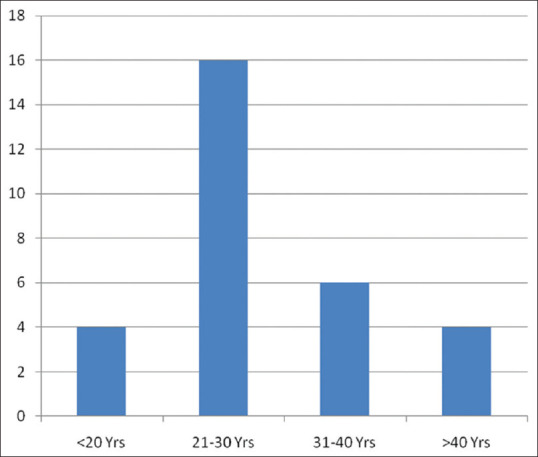
Age distribution of doctors who committed suicide
Figure 3.
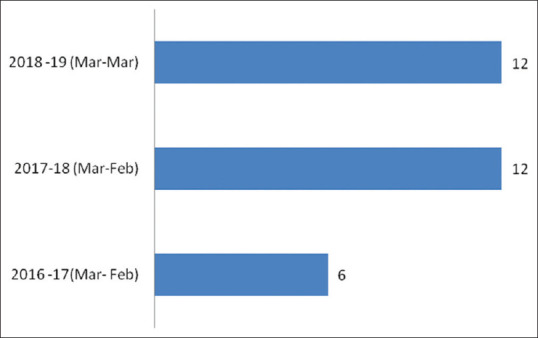
Number of suicide among doctors reported between 2016 and 2019 (March to March)
Figure 4.
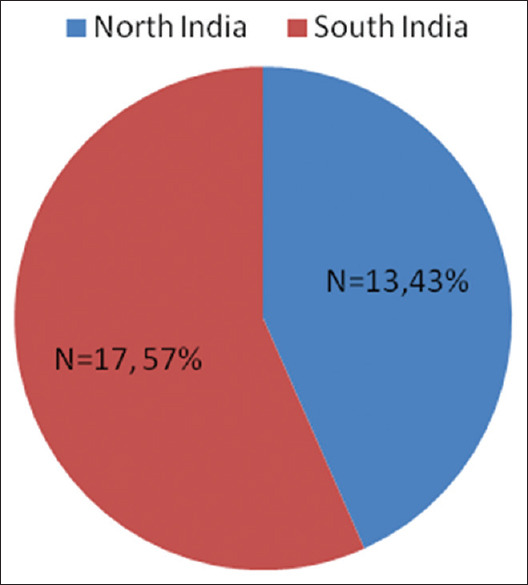
Regional distribution of doctors who committed suicide
Figure 5.
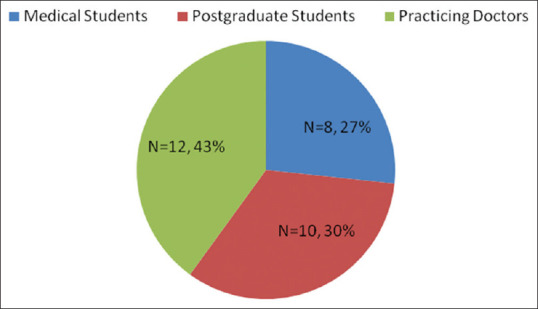
Distribution of medical students, postgraduate students, and practicing doctors among those who committed suicide
Figure 6.
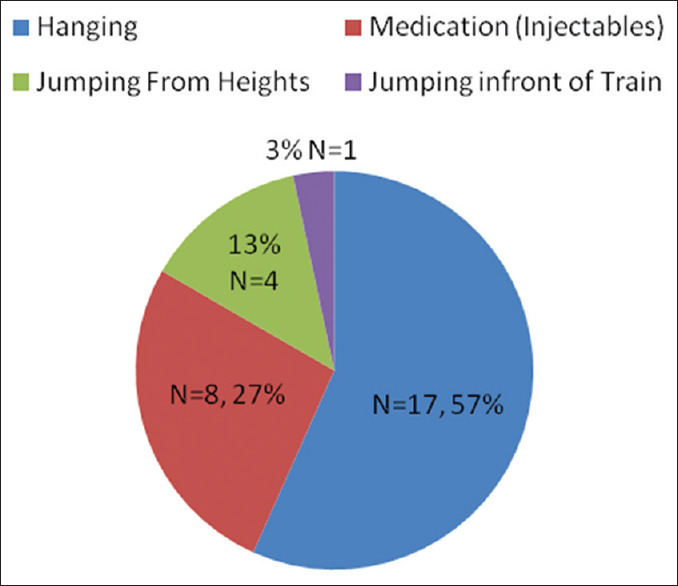
Method used by doctors who committed suicide
Figure 7.
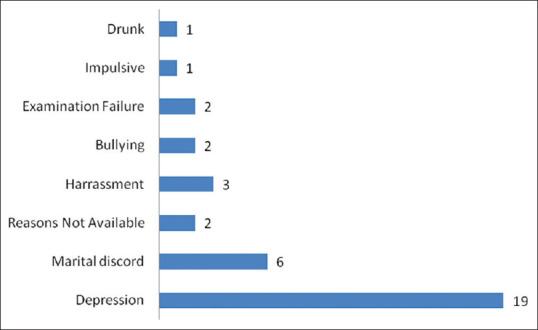
Frequency of reported reasons for the act of suicide among doctors
Figure 8.
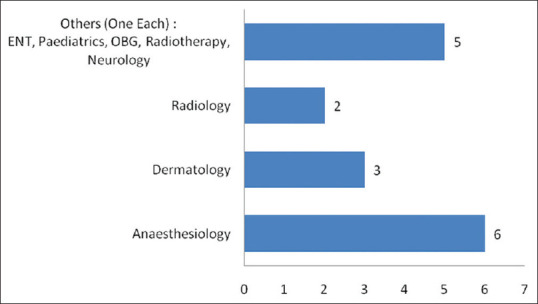
Subspecialty frequency of those doctors who committed suicide
DISCUSSION
Suicide among Indian doctors has been least studied, to our knowledge, this is the first study from India. The only available mode of scientific study is from the information that is available from the newspaper reports, more so from the online edition of the English newspapers. Our study from India found thirty suicides of doctors between the years March 2016 and March 2019. In the United Kingdom, 430 doctors committed suicide between the years 2011 and 2015 and in China 51 doctors ended their lives between years 2008 and 2016.[3,4] The lower deaths in India compared to the United Kingdom and higher deaths compared to China needs further evaluation apart from the methodology used for data collection. The United Kingdom has more robust data collection system about doctors' suicide and hence may have more accurate numbers, which is indeed alarming. The Chinese study and our data largely rely on the information from public domains which inherently has bias. Suicide, in India perceived as stigma to individual and family, it may be more so among doctors and hence may be underreported. The authors had earlier presented a study of suicides from three medical institutions between the year 2015 and 2018, the number of doctors death was ten.[13] Hence, the possible number that was projected, around 150–300 suicides in 4–5 year period, considering that India has more than 500 medical institutions, where more than 80,000 MBBS students, more 30,000 MD/MS students pass out annually, and minimum of 100,000 doctors are employed as teaching faculty apart from other doctors not associated with medical institutions. In order to accurately record suicide among Indian doctors, it should be noted here that India urgently needs a robust system to collect information and such process may happen only if IMA or Indian psychiatric society in association with IMA and/or the National Medical Commission initiate documentation and research on doctors suicide, thereby save precious lives right from undergraduate phase of medical profession.
Female doctors (60%) had higher suicide compared to male doctors in our study which is comparable to United Kingdom data. It may be possible that women doctors may face more challenges compared to men in Indian scenario that may be related to gender issues in the sociocultural context. However, in one study, suicide rate of women doctors in the United States was twice that of other working women.[14] In another study that looked medical students in India, more female students than male had suicidal ideation.[15] These findings may be more important to address the risk factors at earliest among female doctors and consider preventive strategies.
Regional studies about suicide in India have shown that south has higher suicide rates than the north India.[16] Our study also had higher suicide among doctors from south India (57%) compared to north India (43%).
The age group at risk of suicide globally has been in the younger age group.[17] Our study correlates with global findings, 67% of Indian doctors who committed suicides were young and below the age of 30 years.
Medical profession begins from MBBS phase, they are budding doctors and they should be included in any study that is targeted at the profession apart from the postgraduate medical student and practicing doctors. In our study, one-fourth of suicides were MBBS students, one-third were postgraduate medical students and rest were practicing doctors. There are many studies in India about depression and suicidal ideation among medical students because of multiple stressors.[18,19] Our findings corroborate with data that the budding doctors who are depressed may end life if preventing strategies are not put in place at earliest period. There are some novel preventive strategies which are as simple as concept book that guides medical students to navigate the early phase of professional life. Students led group approach to cope with sadness can also be model to emulate.[20,21]
Postgraduate medical students constituted more than 30% of doctor's suicide in our study. Postgraduation may also have additional stressors for individuals such as financial burden, more professional responsibility, and many get married to start their families. Our study from newspaper reports has limited information on such stressors, but in another study from India, residents in general had more depression and suicidal ideation compared to faculty.[22] It is important to engage postgraduates in medical colleges in mental health awareness programs as soon as they join the course.
In our study, 40% of doctors who committed suicides were practicing doctors. Reports mention that, among this section of doctors, more than one-third had MBBS degree and two-third had MD/MS degree. Although our study from available doctors' suicide news reports is small, anesthesia doctors are notable in numbers. Indian and Western studies have consistently highlighted risk of suicide in this specialty, and our study substantiates the findings.[23,24] Identifying higher risk can help in designing focused approach for suicide prevention in respective subspecialty. Strategies can be focused, for mitigation of stress to the particular profession at earliest phase by bringing out concept book.[25]
Method utilized for suicide attempt determines the lethality of the act; in our study, hanging was the most common method of suicide among Indian doctors and more than half used this method. One-fourth of doctors used medication as injections to end their life, reports mention all most all used anesthetic drugs, and one used potassium chloride to end life. One-fifth used violent method to end their life by jumping from the buildings and one of them jumped in front of train. Our study ascertains that doctors use lethal methods to end life, those methods make the attempts certain of death such as hanging or using anesthetic drugs and revival almost difficult in cases of jumping from heights.
Depression has been considered one of the important reasons for suicide, and in our study on Indian doctor's suicide, more than 60% of news reports mention depression as the reason. Reports mention two were taking treatment. Many studies on doctors have looked into burnout and depression; the findings are indeed matter of concern, and our study substantiates the concern.[26,27]
In our study, among medical students, depression appears as the reason commonly mentioned in news reports with some specific reasons that differs. Reasons mentioned were “not interested in MBBS” “ragging” “bullying” “exam anxiety” “exam failure.” These findings are consistent with other study which has systematically reviewed mental health issues among medical students in India.[28] In our study, 20% of doctor's suicide, marital discord was mentioned as reason. Three reports mentioned about harassment as reason for suicide. In some cases, the reason for suicide may never be identified; in our study, from the online news reports on doctor's suicide also had two deaths, in which the reasons were not known.
This study has limitations because of information that is from the 12 English newspapers published in India and that has online presence. News media which do not have print edition were excluded. Many vernacular newspapers online in India may have reported suicide in doctors but not included in the study. The study has not compared suicide of allopathic doctors with those from other system of medicine or other profession to further understand factors unique to the profession. The study has considered only retrospective 3-year period data. There is a need for prospective and methodologically robust studies in this area. The news reports are not rigorously scrutinized and analyzed in scientific manner for publication in media; hence, the use of such data for the study should be considered with caution.
CONCLUSION
Suicide among Indian doctors is a concern. Majority are young undergraduate and postgraduate medical students. Suicide among female doctors is more than male doctors. Most doctors were reported to be depressed, not seeking help and used lethal method such as hanging and injectable medications to end their lives. There is an urgent need for preventive strategies to be initiated both at institutions and professional organization.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kumar R, Pal R. India achieves WHO recommended doctor population ratio: A call for paradigm shift in public health discourse! J Family Med Prim Care. 2018;7:841–4. doi: 10.4103/jfmpc.jfmpc_218_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jacob KS. Medical council of India's new competency-based curriculum for medical graduates: A critical appraisal. Indian J Psychol Med. 2019;41:203–9. doi: 10.4103/IJPSYM.IJPSYM_166_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Suicide by Occupation, England – Office for National Statistics. [Last accessed on 2020 Feb 18]. Available from: https://www.ons.gov.uk/peopepopulationandcommunity/birthdeathandmarriages/deaths/artilces/suicidebyoccupation/england2011to2015 .
- 4.Jin HM, Guo LL. Suicide in medical doctors: A review from Mainland China, 2008-2016. Neuropsychiatry (London) 2018;8:970–6. [Google Scholar]
- 5.India State-Level Disease Burden Initiative Mental Disorders Collaborators. The burden of mental disorders across the states of India: The Global Burden of Disease Study 1990-2017. Lancet Psychiatry. 2020;7:148–61. doi: 10.1016/S2215-0366(19)30475-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Accidental Deaths and Suicide in India 2018. NCRB Report. [Last accessed on 2020 Feb 18]. Available from: https://ncrb.gov.in/StatPublications/ADSI/ADSI2018/chapter-2%20suicides.pdf .
- 7.National Center for Health Statistics. Health, United States, 2012: With Special Feature on Emergency Care. Hyattsville, MD: National Center for Health Statistics; 2013. [Last accessed on 2020 Feb 18]. Available from: https://www.cdc.gov/nchs/data/hus/hus12.pdf . [PubMed] [Google Scholar]
- 8.Coentre R, Góis C. Suicidal ideation in medical students: Recent insights. Adv Med Educ Pract. 2018;9:873–80. doi: 10.2147/AMEP.S162626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gabbard GO. The role of compulsiveness in the normal physician. JAMA. 1985;254:2926–9. [PubMed] [Google Scholar]
- 10.Krakowski AJ. Stress and the practice of medicine – The myth and reality. J Psychosom Res. 1982;26:91–8. doi: 10.1016/0022-3999(82)90068-x. [DOI] [PubMed] [Google Scholar]
- 11.General Medical Council. United Kingdom. National Training Surveys Reports. [Last accessed on 2020 Feb 18]. Available from: https://www.gmc-uk.org/about/what-we-do-andwhy/data-and-research/nationnal-training-surveys-reports .
- 12.The Wounded Healer 2018. International Practitioner Health Summit. London. United Kingdom: [Last accessed on2019 Dec 24]. Available from: http://gphealth.nhs.uk/wp-content/uploads/sites/37/2018/10/The-Wounded-Healer-2018-1.pdf . [Google Scholar]
- 13.Kishor M, Chandran S, Vinay HR, Dushadram D. India: Sneha Foundation Trust; 2019. Suicide among Indian doctors-emerging challenge. In: Poster Session Presented At: Suicide Update. Chennai. [Google Scholar]
- 14.Dobson R. Suicide rate of women doctors in US is twice that of other working women. BMJ. 2007;335:961. [Google Scholar]
- 15.Goyal A, Kishor J, Anand T, Rathi A. Suicidal ideation among medical students of Delhi. J Ment Health Behav. 2012;17:60–70. [Google Scholar]
- 16.Patel V, Ramasundarahettige C, Vijayakumar L, Thakur JS, Gajalakshmi V, Gururaj G, et al. Suicide mortality in India: A nationally representative survey. Lancet. 2012;379:2343–51. doi: 10.1016/S0140-6736(12)60606-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bilsen J. Suicide and youth: Risk factors. Front Psychiatry. 2018;9:540. doi: 10.3389/fpsyt.2018.00540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kumar SG, Kattimani S, Sarkar S, Kar SS. Prevalence of depression and its relation to stress level among medical students in Puducherry, India. Ind Psychiatry J. 2017;26:86–90. doi: 10.4103/ipj.ipj_45_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jain A, Jain R, Menezes R, Subba SH, Kotian MS, Nagesh KR. Suicide ideation among medical students: A cross sectional study from south India. Injury Prev. 2012;18:A166. [Google Scholar]
- 20.Chandran S, Kishor M, Bhargava S, Jayaram R, Sundararajan R, Prabhu P, et al. An innovative concept book guide for MBBS students. Indian J Psychiatry. 2017;59:525–6. doi: 10.4103/psychiatry.IndianJPsychiatry_419_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kishor M, Prabhu P, Bhargava S, Jayaram R, Sundarrajan R. Adopted group therapy approach for coping with sadness among medical students. Int J Health Allied Sci. 2019;9:84–5. [Google Scholar]
- 22.Grover S, Sahoo S, Bhalla A, Avasthi A. Psychological problems and burnout among medical professionals of a tertiary care hospital of North India: A cross-sectional study. Indian J Psychiatry. 2018;60:175–88. doi: 10.4103/psychiatry.IndianJPsychiatry_254_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shinde S, Yentis SM, Asanati K, Coetzee RH, Cole-King A, Gerada C, et al. Guidelines on suicide amongst anaesthetists 2019. Anaesthesia. 2020;75:96–108. doi: 10.1111/anae.14890. [DOI] [PubMed] [Google Scholar]
- 24.Rajaleelan W, Chandramouleeswaran S, Kuppuswamy B. Assesment of mental health status of trainee anaesthesiologists in southern India tertiary care hospital. Astrocyte. 2015;1:292–4. [Google Scholar]
- 25.Ghiya M, Chandran S, Kishor M. The art of healing, emergency minds – A concept book. J Emerg Trauma Shock. 2019;12:163–4. doi: 10.4103/JETS.JETS_142_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dewa CS, Loong D, Bonato S, Thanh NX, Jacobs P. How does burnout affect physician productivity. A systematic literature review? BMC Health Serv Res. 2014;14:325. doi: 10.1186/1472-6963-14-325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Banerjee A. Physician Heal Thysels: Perspectives on burnout among doctors. Perspect Med Res. 2019;7:3–9. [Google Scholar]
- 28.Sarkar S, Gupta R, Menon V. A systematic study of depression, anxiety, and stress among medical students in India. J Ment Health Hum Behav. 2017;22:88–96. [Google Scholar]


