Abstract
Background:
Chronic, heavy alcohol use is associated with multiple health problems, including premature death. Further, the clinical presentation of alcohol dependence may differentially affect and predict the long-term health consequences of affected individuals. Subtypes of alcohol dependence based upon treatment intake information can help identify homogenous groups of patients for treatment purposes, but have not been used to predict long-term outcomes. The current study examined mortality in a 36-year posttreatment interval among 4 subtypes of alcohol-dependent patients based upon their initial intake data.
Methods:
Extensive baseline data were collected from n = 316 male and female patients receiving inpatient treatment for alcohol dependence between 1980 and 1982. Four alcohol dependent subtypes (Del Boca & Hesselbrock, Alcohol Health Res World, 20:56, 1996) derived from the baseline data were used to examine the 1-year posttreatment drinking status and the risk of death 36 years postdischarge. Public records were used to determine patient deaths in the 36 years since discharge.
Results:
At the 36-year follow-up interval since discharge, 68.4% of the sample had died. The 4 subtypes were found to be associated with different rates of resumption of regular drinking in the first year posttreatment and a differential risk of mortality. An increased risk for returning to regular drinking (once a week or more) and early death were associated with subtypes defined, in part, by conduct problems and externalizing disorders. Regardless of subtype membership, women had the highest risk of death following treatment.
Conclusions:
This study demonstrates the clinical usefulness of subtypes of alcohol dependence for examining different alcohol use outcomes, including predicting mortality. The increased risks for returning to regular drinking once a week or more and early death posttreatment among subtypes associated with conduct problems and externalizing disorders suggest the need for continued monitoring and possible additional intervention postdischarge.
Keywords: Alcohol Dependence, Typology, Mortality, Follow-Up
EPIDEMIOLOGICAL AND CLINICAL studies conducted in the United States and Europe have consistently documented strong associations between chronic heavy drinking and negative health consequences, including high rates of premature death. The Centers for Disease Control and Prevention (CDC) reported that 35,823 persons (25,911 males and 9,912 females) died of an alcohol-induced cause in 2017, a 16% increase from 2000 (Kochanek, et al., 2019). Similarly, the age-adjusted death rate for alcohol-induced causes of death for the total population increased significantly from 7.0 in 2000 to 11.0 in 2017. While light and moderate alcohol consumption was associated with a reduced risk for all-cause mortality and cardiovascular disease, a significant increase in risk for all-cause mortality, including cancer, was found among heavy drinkers (Xi et al., 2017). Similar results have been reported for large sample studies of males and females from the United States, Australia, and Europe (Almeida et al., 2015; Breslow and Graubard, 2008; Stahre, et al., 2014; Tverdal, et al., 2017; White et al., 2020), concluding that heavy alcohol consumption was responsible for 14.6 % of all premature adult deaths (Rehm, et al., 2007).
Similarly, studies of mortality among clinical samples of alcohol-dependent persons have consistently reported more health problems and higher mortality rates compared to non-alcohol-dependent groups (Dawson, 2000; O’Brien et al., 2007). Further, a Danish cohort study of patients treated for alcohol dependence found a significantly higher risk for not only alcohol-related diseases, but also dementia, psoriasis, and breast cancer in men (Holst et al., 2017). Accordingly, mortality risk was also higher relative to the general population. A meta-analysis of 81 studies of clinical samples by Roerecke and Rehm (2013) reported a relative risk of all-cause mortality of 3.38 for men and 4.57 for women. They also reported that age-groups under 40 years old and people in treatment for alcohol dependence showed a substantially higher mortality risk than others in that sample. Roerecke and Rehm (2014), in a meta-analyses of cause-specific mortality risk of 17 studies using a 10-year follow-up interval, found elevated cause-specific mortality among alcohol-abusing and alcohol-dependent (AUD) patients across all major categories of diseases. The pooled standard mortality ratio (SMR) was 14.8 for liver cirrhosis, 18.0 for mental disorders, 6.6 for injuries, and 2.0 for cancer and cardiovascular diseases. Consistent with other studies of AUD, the pooled SMR for women was much higher than for men.
In summary, the current literature consistently reports a higher mortality rate across the range of severity of alcohol problems reported by heavy drinkers and alcohol-dependent persons compared to the general population. This finding holds regardless of sample size, sample origin (general population or clinical samples), measurement of alcohol use, and duration of the follow-up period. Women, compared to men, are consistently at higher risk for experiencing serious medical consequences from chronic heavy drinking and alcohol dependence. However, very few studies have investigated possible predictors of mortality among persons with alcohol dependence, other than alcohol use and demographic variables. John and colleagues (2013) found that being female, the severity of alcohol-related problems reported a poor self-rating of health, and the utilization of inpatient detoxification treatment services predicted mortality in a 4-year follow-up of a general population sample. Further, data from alcohol-dependent clinical samples remain scant and are mostly cross-sectional. While higher death rates resulting from alcohol dependence are associated with a genetic predisposition/family history of alcohol use disorder and other personal factors in early life, the direct effects of alcohol dependence on mortality risk increase across the life span (Kendler et al., 2016).
The apparent failure to identify consistent sturdy predictors of mortality among alcohol-dependent persons could be due to the retrospective and/or cross-sectional nature of most existing studies and the primary focus on current drinking variables. The heterogeneity of nonbiological factors including drinking histories and other comorbid psychiatric conditions (including other drug use/abuse) among alcohol-dependent persons is often ignored. Thus, a host of non-drinking factors may also significantly contribute to the increased mortality rate of alcohol-dependent persons over time. One method that could be used to efficiently incorporate this information into prediction models is through classifying alcohol-dependent affected individuals into typologies or subtypes. Available typologies of alcohol dependence typically include a variety of clinical and other factors that begin to address these limitations. Alcohol dependence typologies derived from different populations have produced homogeneous subtypes based upon different clinical features and/or a variety of data reduction procedures. While the resulting subtypes of alcohol dependence have been useful for treatment planning purposes, their utility for predicting long-term outcomes (including mortality) has not been well investigated.
Empirically derived multidimensional typologies typically identify 2 to 5 meaningful alcohol dependent subtypes. While earlier typologies usually identified 2 groups (Babor, et al., 1992; Cloninger et al., 1996), more recent studies indicate that dichotomous subtypes fail to adequately capture the complex clinical nature of alcohol dependence and may mask important sex differences (Del Boca and Hesselbrock, 1996; Epstein, et al., 2002; Leggio, et al., 2009). Some studies have suggested 3 subtypes (Hauser and Rybakowski, 1997; Hill, 1992), 4 subtypes (Bucholz, et al., 1996; Del Boca and Hesselbrock, 1996; Lesch and Walter, 1996; Windle and Scheidt, 2004), or even 5 subtypes (Cardoso, et al., 2006; Moss et al., 2007; Zucker, 1987). Most classification schemas are based on cross-sectional and/or retrospective data typically collected at treatment intake, but have not been examined longitudinally. Thus, the predictive utility of these typological classifications has typically not been determined. A lone exception is a study by Moss and colleagues (2010) that found different clinical outcomes among 5 subtypes of alcohol-dependent persons 3 years after their initial assessment. As expected, Moss et al.’s chronic and severe subtype of alcohol dependence was associated with the continuation of alcohol dependence during the 3-year follow-up interval.
The question of the optimal number of alcohol dependent subtypes has been examined in considerable detail by us (Del Boca and Hesselbrock, 1996) and several others (cf., Bucholz et al., 1996; Epstein et al, 2002; Windle and Scheidt, 2004). While 2 alcohol dependence subtypes are conceptually elegant and statistically efficient, 2 subtypes have been found to overlap, sharing many of the same symptoms, suggesting poor construct validity. Our previous work found that sex differences can be masked when analyses are constrained to using only 2 subtypes, but become evident when 4 subtypes are examined (Del Boca and Hesselbrock, 1996). The use of 4 subtypes also allows for the identification of unique subtype precursors when examining developmental pathways. This, in turn, may help identify critical time points for clinical intervention and help guide treatment planning. Multiple alcohol dependence subtypes, when used in genetic research, are typically more informative and homogeneous phenotypes, offering clear advantages for studies of gene identification and gene function. In the current study, we examined 4 alcohol dependence subtypes based upon clinical intake data as predictors of relapse to drinking in the first year posttreatment and mortality over the 36 years following discharge.
MATERIALS AND METHODS
The initial study was designed as a prospective study and included a 1-year posttreatment follow-up interview reported elsewhere (Babor et al., 1992). The University of Connecticut Health Center Institutional Review Board approved the initial study and its follow-up assessments, including the longer term death record review. Written informed consent was obtained from each participant at intake, including permission for follow-up contacts.
Subjects
Participants included 232 men and 84 women (n = 316) who completed a 21-day inpatient treatment program for alcohol dependence at either a university-affiliated hospital, an innercity substance abuse treatment center, or a Veterans Administration Medical Center (VAMC) from 1980 to 1982. All programs were based in Central Connecticut. At baseline, extensive information was collected via in-person interviews. This included demographic information, lifetime alcohol use patterns and related health problems, current and past history of psychiatric disorders, social and psychological consequences of drinking, and a family history of alcohol use disorders. Axis I lifetime psychiatric disorders were assessed according to DSM-III using a structured and standardized psychiatric interview (Diagnostic Interview Schedule (NIMH-DIS)) (Robins, et al., 1979; Robins, et al., 1981) administered by trained interviewers. Direct interview follow-up assessments of drinking status were also completed on all available subjects (n = 259; 82% of surviving subjects) at 1 year posttreatment. Three subjects died prior to completing the first-year follow-up assessment.
Alcohol Dependence Subtypes
Typological classifications of the participating subjects were previously derived from 17 baseline clinical features via cluster analysis and are described elsewhere (Del Boca and Hesselbrock, 1996). The subtype defining characteristics included the following: (i) premorbid risk factors—familial alcoholism, conduct disorder, and onset of prealcoholic drinking events including age of first drink, age of first intoxication, and age of first symptom; (ii) pathological use of alcohol and other drugs—typical amount of alcohol used/drinks per occasion and polydrug use (including benzodiazepine use); (iii) chronicity and consequences of drinking—health status at intake, physical and social consequences of drinking, dependence severity, and years of heavy drinking; and (iv) psychiatric symptoms (current and lifetime)—depression, antisocial personality, and anxiety.
The first cluster, “High Risk, High Severity” (HR/HS) (n = 70), contained equal proportions of men and women (~22% of the sample) and was the youngest (mean age = 27.23 ± 5.13) at intake. Clinically, they were characterized by a high-risk, early-onset alcohol dependence. HR/HS subjects reported moderate-to-high alcohol involvement and high levels of psychiatric comorbidity, including both major depressive disorder and antisocial personality disorder. The second cluster, “Low Risk, Low Severity” (LR/LS) (n = 99), contained 28% of the males and 39% of the females and was the oldest subtype (mean age = 44.65 ± 11.16). They were characterized by having low-risk, late-onset alcohol dependence, low alcohol involvement, and little or no psychiatric comorbidity. The third cluster, “Internalizers” (n = 53), had a mean age of 40.02 years (±10.96) and was mostly female, with high alcohol involvement and high levels of internalizing disorder (depression, anxiety disorder), but low levels of externalizing behavior/disorder. The fourth cluster, “Externalizers” (n = 94), was similar in age to the “Internalizer” subtype (mean age = 40.49 ± 10.07), but were mostly male. They reported moderate-to-high alcohol involvement and high levels of externalizing behaviors (many had antisocial personality disorder), but few or no depressive or anxiety symptoms.
Alcohol Dependence Subtypes and Drinking History Milestones
The drinking history of each subject from age of first drink to baseline admission to treatment was examined at intake and provides a context for the mortality data. As expected, the age of onset of drinking-related milestones leading to the development of alcohol dependence differed across the 4 subtypes of alcohol dependence (see Fig. 1). The ages of onset of the ten different drinking milestones for the HR/HS and Externalizer subtypes were similar and occurred earlier than for the LR/LS and Internalizer subtypes, with 2 exceptions. The HR/HS subjects entered treatment for the first time earlier than the Externalizers and also had an earlier average age of death. The Internalizer subtype experienced each drinking milestone later than the Externalizer and HR/HR subtypes, but earlier than the LR/RS subtype.
Fig. 1.
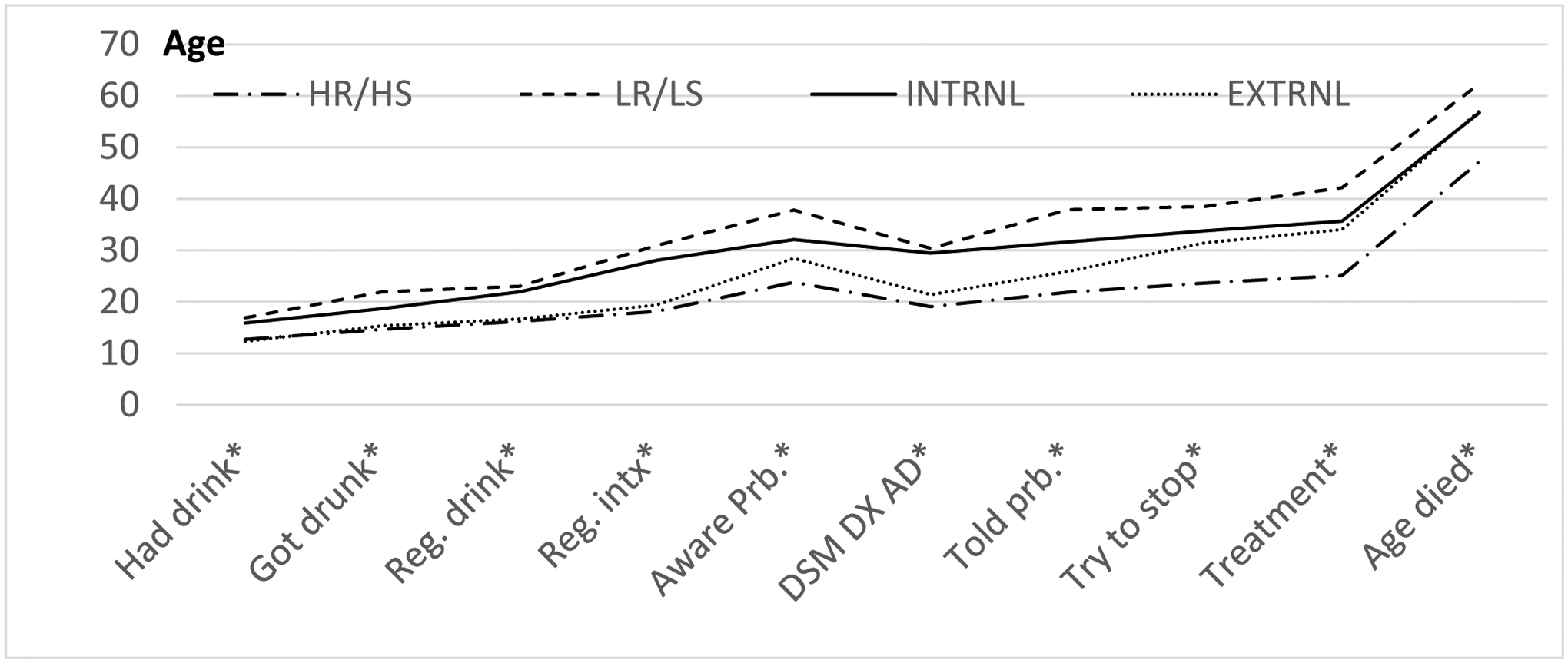
Drinking milestones for alcohol dependence and mortality by subtypes.
Mortality Over Time.
Mortality over the 36-year interval from initial baseline to 2018 was determined for each subject through several information sources including the Social Security Death Index, the CDC’s National Death Index, State of Connecticut Department of Public Health death records/certificates, and other publicly available information sources such as obituaries from local newspapers.
Data Analyses
Drinking status at 1 year postdischarge—All available former patients were reinterviewed 1 year postdischarge. Patients were classified into 1 of 3 categories:
(i) abstinent; (ii) regular drinking (weekly or more) but did not receive treatment; and (iii) regular drinkers who received either inpatient or outpatient treatment.
Standard mortality ratio (SMR)—Mortality rates over the 36-year follow-up interval were examined using a SMR approach. A standardized mortality ratio (SMR) is a ratio between the observed number of deaths in a study population and the number of expected deaths, based on the age- and sex-specific rates in a standard population. Chronological age is known to be a significant predictor of mortality, and in this study, the subject’s age at baseline was highly correlated with subtype membership. Consequently, standard mortality ratios were computed using the State of Connecticut 2016 population data as the standard (CDC WONDER, https://wonder.cdc.gov/). Connecticut death rates were derived from the gender-specific data and divided into 8 age-groups (15 to 24, 25 to 34, 35 to 44, 45 to 54, 55 to 64, 65 to 74, 75 to 84, and 85 + years of age) by 4 calendar periods (1980 to 1989, 1990 to 1999, 2000 to 2009, and 2010 to 2016). The corresponding observed death rates for the same age-groups and calendar periods were calculated for each subtype. Using R programming software, customized R code was used to compute standard mortality ratios, point estimates, and 95% confidence intervals for each subtype.
Survival probability over the 36-year follow-up interval—Kaplan–Meier curves by 1-year postdischarge drinking status and by subtypes were used to visualize survival probability as a function of age. The log-rank test and Cox proportional hazards models were used to determine significant differences by drinking status and between the subtypes.
Predictors of mortality—Stepwise logistic regression analysis was conducted to examine subtypes, gender, and other baseline variables and 1-year postdischarge drinking status as predictors of mortality over the 36-year follow-up interval.
RESULTS
Sample Description
Alcohol-dependent persons (n = 316) receiving inpatient treatment in the greater Hartford area between 1980 and 1982 who volunteered for the study were enrolled and assessed at baseline. The sample included 232 males and 84 females, with an average age of 38.8 years (Table 1). Most began regular drinking during late adolescence. At baseline, on average, men were older than women (39.5 ±11.7 vs.36.7 ± 11.5 years old). More than two-thirds of subjects were high school graduates. Approximately one-third of subjects were married and employed full-time. Male subjects, compared to female subjects, reported a longer period of alcohol dependence (17.7 ± 18.2 vs. 11.6 ± 22.5 years).
Table 1.
Demography at Admission
| Male (n = 232) | Female (n = 84) | Total (N = 316) | |
|---|---|---|---|
| Mean age | 39.5 (±11.7) | 36.7 (±11.5) | 38.8 (±11.7) |
| Age first regular drink | 18.4 (±5.4) | 22.3 (±8.4) | 19.4 (±6.4)* |
| # years of AD | 14.7 (±10.1) | 6.3 (±5.4) | 12.4 (±9.8)* |
| Age of onset of AD | 25.0 (±10.2) | 30.4 (±11.4) | 26.4 (±10.8)* |
| % HS graduate | 65.8 | 75.0 | 68.3 |
| % Married | 26.8 | 35.7 | 29.2 |
| % Divorced/separated | 43.3 | 41.7 | 42.9 |
| % Single | 29.9 | 22.6 | 27.9 |
| % Employed full-time | 34.5 | 29.8 | 33.2 |
| Part-time | 6.6 | 4.8 | 6.1 |
AD, alcohol dependence; HS, high school.
Gender difference, p < 0.01.
Causes of Death
Causes of death were extracted from official death certificates provided by the State of Connecticut Department of Public Health. The most frequently reported acute and chronic causes of death included cardiac/heart diseases and cancers (each 23%), liver disease (13%), overdose (due to alcohol or any drug) (7%), and suicide and respiratory diseases (both 6%). Other less frequently reported causes of death included stroke, diabetes, pneumonia, gastrointestinal problems, kidney diseases, HIV, acute infections, and accidents. Unfortunately, the available death certificates did not consistently document whether the cause of death was directly related to alcohol, smoking, or both. In general, the more common causes of death reported for this sample mimic those reported for the general populations of both Connecticut and the United States (White et al., 2020).
Alcohol Dependence Subtypes and Drinking Status at 1 Year Postdischarge
The 4 subtypes of alcohol dependence were examined in association with drinking status at the 1-year posttreatment follow-up (see Table 2). Patients were classified into 1 of 3 categories: (i) abstinent, (ii) regular drinking (weekly or more) but did not receive treatment, and (iii) regular drinkers who received treatment. The majority of subjects, regardless of subtype, resumed regular drinking (once a week or more) sometime in the first year posttreatment. Further, once they began regular drinking, they tended to be readmitted for treatment (50.8%/ 74.% = 68%). Each subtype was associated with a differential risk for resuming drinking and for treatment readmission. Externalizers were associated with the poorest outcome—with the highest rate of return to drinking and readmission (12.8% + 74.4% = 88.5%). HR/HS subjects reported high rates of drinking (35.1% + 43.9% = 79%), but fewer (43.9%) received additional treatment in the first year postdischarge than the Externalizers (74.4%). A lower proportion of LR/LS and Internalizers reported resuming regular drinking (66.7% vs 63%) and treatment readmission (34.6% vs 47.8 %).
Table 2.
One-Year Postdischarge Drinking Status by Subtypes
| Drinking Frequency | HR/HS (n = 56) % | LR/LS (n = 80) % | INT (n = 46) % | EXT (n = 78) % | Total (N = 259) % |
|---|---|---|---|---|---|
| Abstinent/occasional. | 19.3 | 32.1 | 37.0 | 11.5 | 24.0 |
| Regulara, no treatment | 35.1 | 32.1 | 15.2 | 12.8 | 24.0 |
| Regulara + treated | 43.9 | 34.6 | 47.8 | 74.4 | 50.8 |
HR/HS, High Risk/High Severity; LR/LS, Low Risk/Low Severity; INT, Internalizer; EXT, Externalizer.
χ2 = 35.7 df (9), p < 0.001; 3 subjects died within 1 year of discharge.
Regular drinking (once a week or more).
Alcohol Dependence Subtypes and 36-Year Postdischarge Mortality
As indicated above, mortality was examined using publicly available, mostly governmental, data sources. As of April 2018, 216 subjects (including 162 men and 54 women) were known to be deceased. Three subjects died within the first year following discharge, with an increasing rate over time. First, crude death rates were calculated as the ratio of the number of deaths in the sample divided by the total sample size. The crude death rate over the 36-year follow-up interval was 68.4% (men 69.8% and women 64.3%). The highest crude death rate occurred in the Externalizer subtype (78.7%) followed by the LR/RS subtype (72.7%). Even though similar in age at intake, over the follow-up interval the crude death rate was much lower among Internalizers (62.3%) than among Externalizers. The lowest crude death rate was found for the HR/HS subtype (31.4%), who were also significantly younger than other 3 subtypes at baseline. Although the HR/HS subtype had the lowest crude mortality rate, they had the earliest average age of death among the 4 subtypes (47.2 ± 13.0 years). The mean age of death for Externalizers and for Internalizers was similar (57.0 ± 12.9 vs. 56.7 ± 16.7 years). The LR/LS subtype had the oldest average age at death at 62.3 (±12.0) years old. There were no significant differences in death rates between those subjects followed at 1 year postdischarge versus those not followed.
Since mortality is generally highly correlated with chronological age and the average age at admission significantly differed across the 4 subtypes, the resulting crude death rates can be misleading. In order to adjust for baseline age differences between subtypes, standard mortality ratios (SMRs) were computed. The age-adjusted SMR varied across the 4 subtypes, ranging from 1.56 to 4.81 for men and from 3.53 to 7.74 for women (see Table 3). The significantly higher SMRs across all subtypes (except for male Internalizers) indicate that the alcohol-dependent individuals were at higher risk of death compared to similar-aged individuals in the general population of the State of Connecticut.
Table 3.
Standard Mortality Ratio (SMR) by Subtypes at 36 Years Postdischarge
| Subtypes | High risk high severity | Low risk low severity | Internalizer | Externalizer | Total |
|---|---|---|---|---|---|
| Male | |||||
| SMR | 4.81* | 2.13* | 1.56 | 3.81* | 2.81* |
| (95% CI) | (3.17, 7.00) | (1.57, 2.83) | (0.93, 2.47) | (2.97, 4.81) | (2.40, 3.28) |
| Female | |||||
| SMR | 7.74* | 3.53* | 3.84* | 7.65* | 4.22* |
| (95% CI) | (3.70, 4.23) | (2.28, 5.21) | (2.15, 6.34) | (2.06, 9.58) | (3.17, 5.50) |
SMR, standard mortality ratio.
p < 0.05.
Important sex differences in relation to risk of death were also found. Overall, the resulting SMR was much higher for women (4.2) than for men (2.8), a finding consistent across all subtypes. Among men, unlike the crude mortality rate, the highest SMR was associated with the HR/HS subtype whose age at baseline was the youngest, followed by the Externalizer subtype. Despite being the oldest subtype at baseline, the SMR was lowest for the LR/LS subtype. Similar findings held for the female subjects. The SMR was also highest among women in the HR/HS subtype followed by the Externalizer, Internalizer, and LR/LS subtypes.
Survival Analyses Over the 36-Year Follow-Up Interval
Mortality was also examined using the 1-year postdischarge drinking status and alcohol dependence subtypes as predictors. Figure 2 presents the Kaplan–Meier survival analysis by 1-year follow-up drinking status. First, Kaplan–Meier survival curves were examined for 3 categories of 1-year drinking status: abstinent, regular drinking (weekly or more) but did not receive treatment, and regular drinkers who received treatment. A higher rate of survival was found for abstinent subjects vs. subjects who resumed regular drinking with or without returning to treatment within the first year following treatment. However, a return to treatment did not distinguish among those who resumed regular drinking. Consequently, the 1-year postdischarge drinking statuses were combined into 2 categories: abstinence vs. resumption of regular drinking. Subjects who remained abstinent in the first year posttreatment compared to those who resumed regular drinking showed significantly higher rates of survival over the 36-year follow-up period (log-rank test: chi-square = 10.38, df = 1, p = 0.001). Thus, a higher mortality rate over the 36-year follow-up interval was associated with a return to regular drinking within the first year following discharge from treatment compared to those who remained abstinent (hazard ratio = 0.558 (95% CI = 0.387 to 0.804)).
Fig. 2.
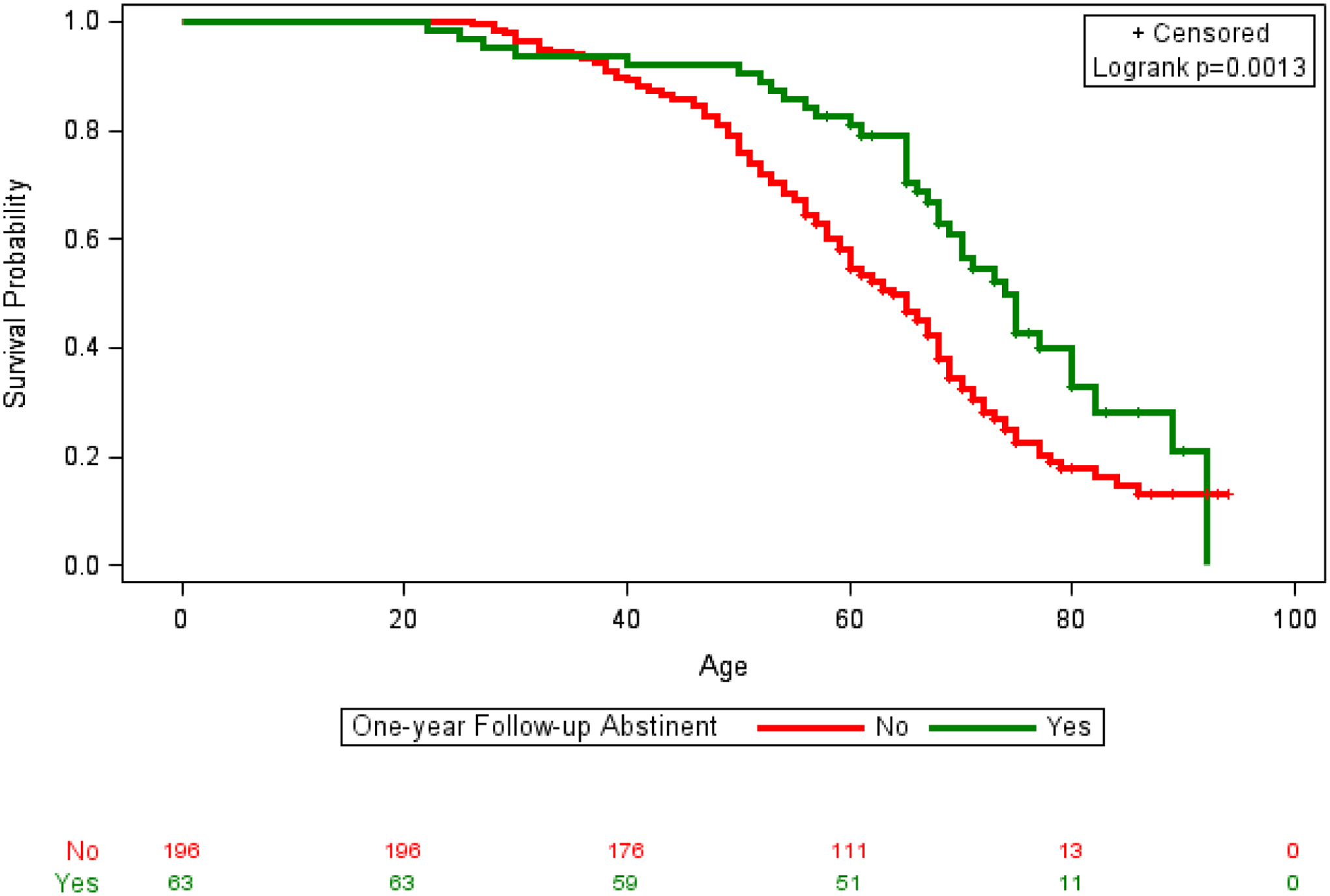
36-Year mortality by 1-year follow-up status: Kaplan–Meier curves.
A Kaplan–Meier survival analysis was also conducted to compare the 4 alcohol dependence subtypes across the 36-year follow-up period. The results were consistent with the findings of the SMR analyses reported above and identified significant subtype differences over time (log-rank test: chi-square = 8.82, df = 3, p = 0.032) (see Fig. 3). The Cox proportional hazards model indicated that the Externalizer subtype was associated with a higher mortality rate compared to the Internalizer subtype (hazard ratio = 1.64 (95% CI = 1.09, 2.48)) and to the LR/LS subtype (hazard ratio = 1.42 (95% CI = 1.03, 1.97)). While the HR/HS subtype and the Externalizer subtype had similar survival curves, the HR/HS subtype had a much earlier average age of death, in fact, the earliest age of death among the 4 subtypes.
Fig. 3.
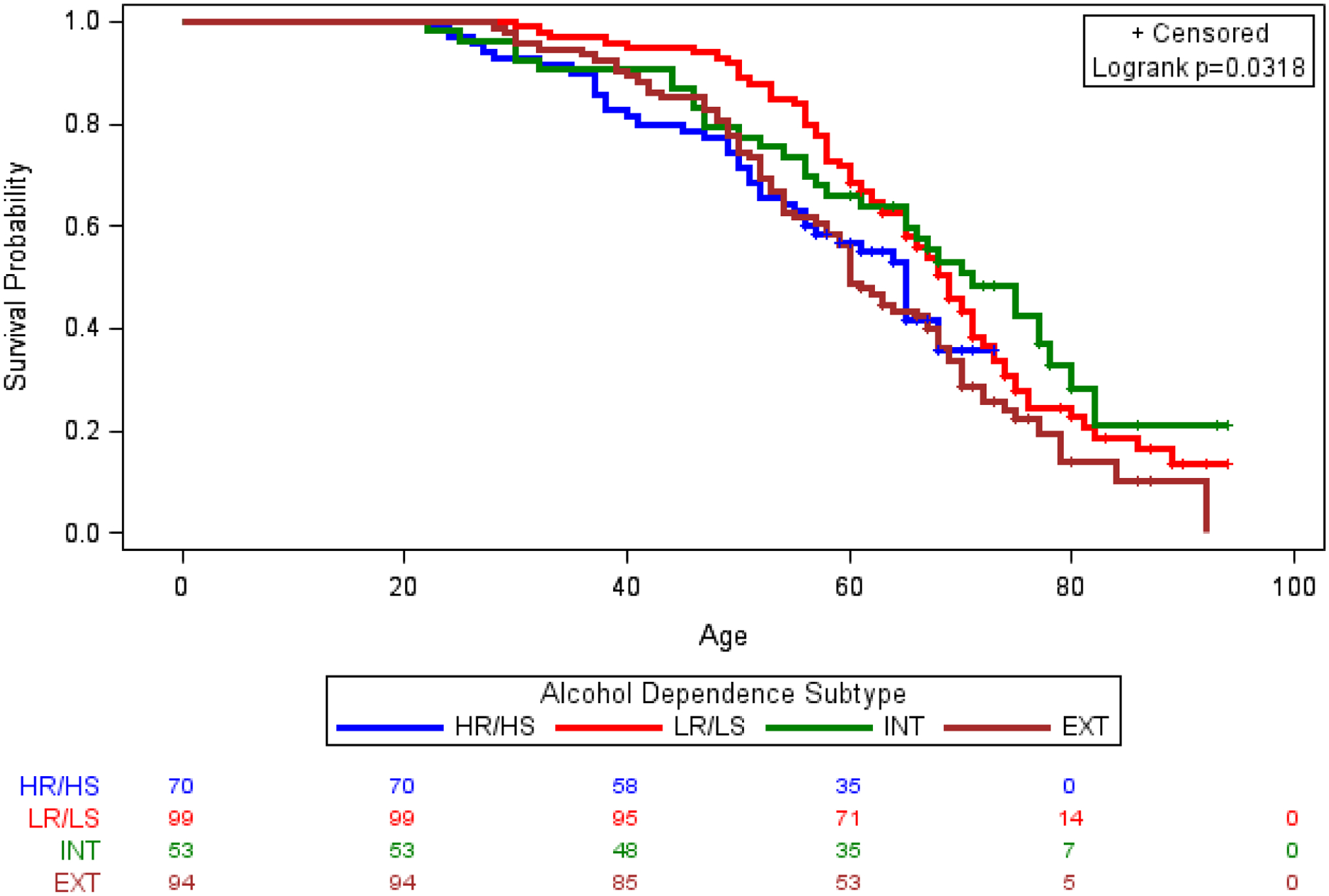
36-Year mortality by alcohol dependence subtypes: Kaplan–Meier curves.
Predictors of Mortality Over Time
Stepwise logistic regression analyses were conducted to examine baseline and 1-year postdischarge drinking status as predictors of long-term mortality. Several other baseline predictors were examined. The initial set of predictors entered into the regression model included employment status, years of regular drinking and years of problem drinking, psychiatric comorbidity, number of DSM-III alcohol dependence symptoms, the age of first treatment for alcohol dependence, other comorbid drug dependence, and a family history of alcohol dependence. Several possible baseline predictors of mortality were dropped from the model at each iteration due to their lack of statistical significance. In the final regression model, age at baseline was a significant predictor of mortality at the 36-year follow-up interval, but the subject’s sex did not add to the equation. Because the subject’s age at baseline and subtype membership were highly correlated, subtype membership was no longer significant after removing the effects of subject’s age at baseline. Within the subtypes, Externalizers versus Internalizers were more likely to be deceased, despite having similar baseline ages (odds ratio = 2.94, 95% CI = 1.18 to 7.32).
DISCUSSION
This study reports on the mortality of a well-characterized clinical sample over the 36 years following their inpatient treatment for alcohol dependence. The sample was obtained from public, Veterans Administration, and academic health center alcohol treatment centers. More than two-thirds of the sample died in the 36-year interval since enrolling in the study. Our mortality findings are consistent with many other studies of alcohol use and mortality (cf., Breslow and Graubard, 2008; Dawson, 2000; O’Brien et al., 2007; White et al., 2020; Xi et al., 2017), indicating that alcohol-dependent persons are at much higher risk of early death compared to the general population (cf., Rehm et al., 2007). Further, our results also show that alcohol-dependent women are at higher risk of death compared to alcohol-dependent men (cf. Roerecke and Rehm, 2014; White et al., 2020). The 4 alcohol dependence subtypes (derived according to the method of Del Boca and Hesselbrock (1996)) followed different developmental pathways toward alcohol dependence, but also displayed a differential risk of death over the longer term. Together, these findings support the clinical relevance of the 4 alcohol dependence subtypes studied.
Overall, the SMRs reported here were consistent with other studies (Roerecke and Rehm, 2013), and this approach emphasizes the importance of standardizing for subject’s age and sex when examining predictors of mortality. The SMR analysis clearly differentiated the 4 alcohol dependence subtypes in relation to all-cause mortality. Our findings also indicate that chronological age alone can be misleading, and when used alone as a predictor ignores the importance of considering individual patient characteristics. Compared to the age-equivalent general population, the HR/HS and Externalizer subtypes were at much higher risk of death at a younger age, a finding similar to Roerecke and Rehm (2013). While the crude mortality risks were lower among the LR/LS and Internalizer subtypes compared to the general population, the SMRs for these subtypes were higher. Our results support the usefulness of 4 subtypes of alcohol dependence for characterizing the longitudinal course of alcohol use disorders, including mortality. While both the Externalizer and HR/HS subtypes were characterized by significant conduct disorder behaviors, the HR/HS subtype was also likely to have comorbid internalizing disorders such as anxiety and/or depression. Internalizing disorders were generally absent among the Externalizer subtype. The LR/LS and Internalizer subtypes had a similar course of their alcohol dependence, but the LR/LS subjects had a lower prevalence of comorbid internalizing disorders. The use of 4 alcohol dependence subtypes also allows for the identification of unique subtype precursors such as the appearance of different clinically important drinking behaviors/milestones over time. This, in turn, may help clinicians recognize critical time points for clinical intervention and help guide treatment planning that is more specific to each subtype.
Consistent with studies by John and colleagues (2013) and Kendler and colleagues (2016), many of the clinical, drinking, and psychiatric variables assessed at entry into treatment lost their ability to predict mortality across the 36-year follow-up interval. Instead, they were replaced by the predictive value of a return to regular drinking during the first-year posttreatment interval. In this study, relapse to regular drinking (either with or without additional treatment) in the first year following discharge from alcohol treatment was a significant predictor of mortality in the 36-year follow-up interval. It may be that an early return to regular drinking following treatment was a proxy for several other factors and may reflect many other patient characteristics such as the severity of alcohol dependence, additional comorbidities, treatment noncompliance, and demographic and contextual factors (e.g., marital status, drinking partners, and alcohol availability). Further, the exact nature of each deceased subject’s drinking behavior during the 36-year follow-up interval is not known. However, it is likely that those subjects who relapsed relatively soon after discharge from treatment continued to drink heavily, a probable important contributor to their death, often prematurely.
The causes of death reported for this sample are consistent with those reported by White and colleagues (2020) based upon US epidemiological data. As in the White et al. study, the leading causes of death were cardiovascular diseases, liver diseases, and cancers, not surprising in an aging sample. Similarly, the rate of overdose deaths due to alcohol alone or in combination with other drugs was also consistent with White et al. Many older adults are also likely using a variety of prescriptions for medical conditions, and these prescriptions often include benzodiazepines and opioid medications. Further, chronic alcohol abusers often consume nonprescription benzodiazepines and opioids when drinking and this can lead to an unintentional overdose, including death. As with other studies using records, our data may be limited due to reporting biases and errors across different recorders of death, the lack of autopsy and toxicological data, and an underreporting of the frequency of alcohol-related death, including possible overdose deaths.
Our study is one of the few that has both mortality data and extensive baseline phenotypic data collected at entry to treatment. However, this study’s sample size was relatively small and included a small number of women as few women sought inpatient treatment for alcoholism during the early 1980s. Even with this limited sample, our results are consistent with findings from more recent alcohol use studies of larger samples of females and support the importance of examining sex differences in alcohol use and outcome studies. Another limitation of the current study is the lack of detailed drinking data over the 36-year posttreatment follow-up interval. Consequently, the exact nature of the subjects’ course of alcohol use over time is unknown. Further, the health and drinking status of the surviving patients was not available for examination. Despite these limitations, findings from the current study provide important information regarding the clinical and theoretical usefulness of alcohol dependence subtypes for examining the longitudinal course of alcohol dependence, the importance of following patients for an extended period postdischarge, and the need for standardized chronological age adjustments in data analysis when examining mortality and other long-term outcome variables.
ACKNOWLEDGEMENTS
Funding for this study was provided by NIH/NIAAA grants 5P60-AA03510 University of Connecticut Alcohol Research Center and NIH/NIAAA U-10-AA08403 Collaborative Study on the Genetics of Alcoholism.
Footnotes
CONFLICT OF INTEREST
None of the authors report an actual or perceived financial or otherwise conflict of interest related to this manuscript.
REFERENCES
- Almeida OP, McCaul K, Hankey GJ, Yeap BB, Golledge J, Flicker L (2015) Excessive alcohol consumption increases mortality in later life: a genetic analysis of the health in men cohort study. Addict Biol 22:570–578. [DOI] [PubMed] [Google Scholar]
- Babor T, Hoffman M, Del Boca F, Hesselbrock V, Meyer R, Dolinsky Z, Rounsaville B (1992) Types of alcoholics, I. Evidence for an empirically derived typology based on indicators of vulnerability and severity. Arch Gen Psychiat 49:599–608. [DOI] [PubMed] [Google Scholar]
- Breslow R, Graubard B (2008) Prospective study of alcohol consumption in the United States: quantity, frequency, and cause specific mortality. Alcohol Clin Exp Res 32:513–521. [DOI] [PubMed] [Google Scholar]
- Bucholz K, Heath A, Reich T, Hesselbrock V, Kramer J, Nurnberger J, Schuckit M (1996) Can we subtype alcoholism? A latent class analysis of data from relatives of alcoholics in a multicenter family study of alcoholism. Alcohol Clin Exp Res 20:1462–1471. [DOI] [PubMed] [Google Scholar]
- Cardoso JM, Barbosa A, Ismail F, Pombo S (2006) NETER alcoholic typology (NAT). Alcohol Alcohol 41:133–139. [DOI] [PubMed] [Google Scholar]
- Cloninger C, Sigvardsson S, Bohman M (1996) Type I and Type II alcoholism: an update. Alcohol Health Res World 20:18–23. [PMC free article] [PubMed] [Google Scholar]
- Dawson D (2000) Alcohol consumption, alcohol dependence, and all-cause mortality. Alcohol Clin Exp Res 24:72–81. [PubMed] [Google Scholar]
- Del Boca F, Hesselbrock M (1996) Gender and alcoholic subtypes. Alcohol Health Res World 20:56–62. [PMC free article] [PubMed] [Google Scholar]
- Epstein E, Labouvie E, McCrady B, Jensen N, Hayaki J (2002) A multi-site study of alcohol subtypes: classification and overlap of unidimensional and multi-dimensional typologies. Addiction 97:1041–1053. [DOI] [PubMed] [Google Scholar]
- Hauser T, Rybakowski T (1997) Three clusters of male alcoholics. Drug Alcohol Depend 48:243–250. [DOI] [PubMed] [Google Scholar]
- Hill S (1992) Absence of paternal sociopathy in the etiology of severe alcoholism: Is there a Type III alcoholism? J Stud Alcohol 53:161–169. [DOI] [PubMed] [Google Scholar]
- Holst C, Tolstrud J, Sorensen H, Becker U (2017) Alcohol dependence and risk of somatic diseases and mortality: a cohort study in 19002 men and women attending alcohol treatment. Addiction 112:1358–1366. [DOI] [PubMed] [Google Scholar]
- John U, Rumpf H-J, Bischoff G, Hapke U, Hanke M, Meyer C (2013) Excess mortality of alcohol dependent individuals after 14 years and mortality predictors based on treatment participation and severity of alcohol dependence. Alcohol Clin Exp Res 37:156–163. [DOI] [PubMed] [Google Scholar]
- Kendler K, Ohisson H, Sundquist J, Sundquist K (2016) Alcohol use disorder and mortality across the lifespan: a longitudinal cohort and co-relative analysis. JAMA Psychiatry 73:575–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochanek K, Murphy S, Xu J, Arias E (2019) National vital statistics reports death: final data for 2017. CDC National Vital Statistics Reports. 68:12–13. [PubMed] [Google Scholar]
- Leggio L, Kenna G, Fenton M, Bonenfant E, Swift R (2009) Typologies of alcohol dependence, from Jellinek to genetics and beyond. Neuropsychol Rev 19:115–129. [DOI] [PubMed] [Google Scholar]
- Lesch O, Walter H (1996) Subtypes of alcoholism and their role in therapy. Alcohol Alcohol 31(supp1):63–67. [PubMed] [Google Scholar]
- Moss H, Chen C, Yi H-Y (2007) Subtypes of alcohol dependence in a nationally representative sample. Drug Alcohol Depend 91:149–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss H, Chen C, Yi H-Y (2010) Prospective follow-up of empirically derived alcohol dependence subtypes in Wave 2 of National Epidemiologic Survey on Alcohol and Related Conditions (NESARC): recovery status, alcohol use disorders and diagnostic criteria, alcohol consumption behavior, health status, and treatment seeking. Alcohol Clin Exp Res 34:1073–1083. [DOI] [PubMed] [Google Scholar]
- O’Brien J, Lu B, Ali N, Martin G, Aberegg S, Marsh C, Lemeshow S, Douglas I (2007) Alcohol dependence is independently associated with sepsis, septic shock, and hospital mortality among adult intensive care unit patients. Crit Care Med 35:626–628. [DOI] [PubMed] [Google Scholar]
- Rehm J, Sulkowska U, Manczuk M, Boffetta P, Powles J, Popova S, Zatonski W (2007) Alcohol accounts for a high proportion of premature mortality in central and eastern Europe. Int J Epidemiol 36:468–469. [DOI] [PubMed] [Google Scholar]
- Robins L, Helzer J, Croughan J (1979) National Institute of Mental Health Diagnostic Interview Schedule. National Institute of Mental Health, Rockville, MD. [DOI] [PubMed] [Google Scholar]
- Robins L, Helzer J, Croughan J, Ratcliff K (1981) National Institute of Mental Health Diagnostic Interview Schedule. Arch Gen Psychiat 38:381–389. [DOI] [PubMed] [Google Scholar]
- Roerecke M, Rehm J (2013) Alcohol use disorders and mortality: a systematic review and meta-analysis. Addiction 108:1562–1578. [DOI] [PubMed] [Google Scholar]
- Roerecke M, Rehm J (2014) Cause-specific mortality risk in alcohol use disorder treatment patients: a systematic review and meta-analysis. Int J Epidemiol 43:906–918. [DOI] [PubMed] [Google Scholar]
- Stahre M, Roeber J, Kanny D, Brewer R, Zhang X (2014) Contribution of excessive alcohol consumption to deaths and years of potential life lost in the United States. CDC Prev. Chronic Dis. 2014:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tverdal A, Magnus P, Selmer R, Thelle D (2017) Consumption of alcohol and cardiovascular disease mortality: a 16-year follow-up of 115,592 Norwegian men and women aged 40–44 years. Eur J Epidemiol 32:775–783. [DOI] [PubMed] [Google Scholar]
- White A, Castle I-J, Hingson R, Powell PA (2020) Using death certificates to explore changes in alcohol-related mortality in the United States. Alcohol Clin Exp Res 44:178–187. [DOI] [PubMed] [Google Scholar]
- Windle M, Scheidt D (2004) Alcoholism subtypes: are two sufficient? Addiction 99:1508–1519. [DOI] [PubMed] [Google Scholar]
- Xi B, Veeranki S, Zhao M, Chuamwei M, Yan Y, Mi J (2017) Relationship of alcohol consumption to all-cause, cardiovascular, and cancer-related mortality in U.S. adults. J Am Coll Cardiology 70:913–922. [DOI] [PubMed] [Google Scholar]
- Zucker R (1987) The four alcoholisms: a developmental account of etiological process, in Nebraska Symposium on Motivation, Alcohol and Addictive Behaviors. (Rivers P ed.) pp. 27–83, University of Nebraska Press, Lincoln, NE. [PubMed] [Google Scholar]


