Abstract
There is a lack of consensus around optimal surgical management for Legg–Calvé–Perthes Disease (LCPD). This case report discusses the benefits of combining arthroscopic femoral neck osteochondroplasty and labral repair with Morscher’s Osteotomy (MO) for LCPD. S.A. is a 17-year-old female diagnosed with LCPD at the age of 6 years and has long-standing right hip symptoms. An arthroscopic femoral neck osteochondroplasty and labral repair followed by MO was performed. The pre-operative and 8 months post-operative International Hip Outcome Tool (iHOT-12) scores were 16.3 and 79.8 out of 100, respectively, indicating better quality-of-life. Also, the femoral neck-shaft-angle (NSA) changed from 120 pre-operative to 138.7 post-operative to represent the correction of coxa vara. The literature review revealed no published reports describing combined MO with hip arthroscopic interventions in managing LCPD. Combined arthroscopic femoral neck osteochondroplasty (with labral repair) and MO provides high patient satisfaction and improves radiographic parameters in patients with LCPD.
INTRODUCTION
Legg–Calvé–Perthes Disease (LCPD) is a congenital hip deformity affecting approximately 29 in 100 000 children, most commonly boys between 4 and 8 years old [1]. LCPD is associated with abnormal development of the femoral head vasculature, causing premature closure of epiphyseal plates. This leads to femoral neck shortening and femoral head enlargement with loss of spherical congruity [2]. The greater trochanter (GT), unaffected by the closure of the epiphyseal plates, continues to grow. These deformities reduce the lever arm of the hip abductor muscles, abductor muscle tension, causing impingement during abduction. Symptoms include reduced hip range-of-motion and anterior thigh pain [3]. Risk factors include familial history, thrombophilias, second-hand smoking, low birth-weight and short stature [4].
There is a lack of consensus for optimal surgical management for LCPD [2]. Surgery aims to restore the anatomy of the hip joint, delaying the onset of osteoarthritis and need for a total hip arthroplasty. One surgical approach for LCPD is the Morscher osteotomy, a femoral neck lengthening procedure that corrects coxa breva and GT overgrowth. This improves lower limb length discrepancy and improves gait, abductor force and range of motion [3]. Arthroscopic labral repair and osteochondroplasty are options for correcting intra-articular abnormalities [5]. Indications for arthroscopy for LCPD include recalcitrant hip pain, intra-articular pathology including loose bodies, labral tears and cartilage lesions [6].
This report presents a 17-year-old with LCPD who underwent Morscher osteotomy for femoral neck lengthening and concomitant arthroscopic femoral neck osteochondroplasty and labral repair. A literature review was performed for reports using the same approach.
CASE DESCRIPTION
A 17-year-old, otherwise healthy, female patient presented with right groin pain radiating to the knee. She was diagnosed with LCPD at the age of 6, and a salter osteotomy was previously performed to relieve her symptoms. Other past surgical history includes a right knee medial patellofemoral ligament reconstruction at the age of 14 for patellar instability. She was able to resume normal daily activity after these two procedures and did not require any follow-up appointments after starting physiotherapy.
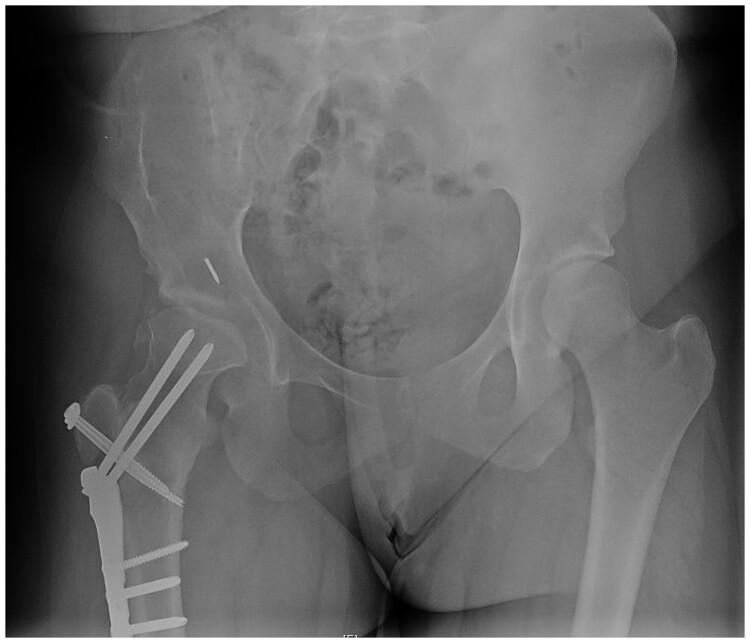
On examination, the patient had a limping gait, a positive Trendelenburg sign, and a positive anterior and posterior impingement test. She had full and symmetrical flexion and extension, 30° of internal rotation, and 45° of external rotation. Strength was normal in all muscles. Anteroposterior and lateral plain radiographs of the right hip showed mature Perthes disease, trochanteric overgrowth, coxa breva and coxa magna (Fig. 1). A scanogram and full leg-length X-rays showed that the right lower limb had an 11 degree of valgus deformity and a 3-cm length discrepancy caused by proximal femur abnormality. MRI of the right hip demonstrated patchy areas of avascular necrosis of the femoral head, posterior labral tear and degenerative changes. A combined open and arthroscopic approach was discussed. Patient decided to proceed with the surgical management and consent was obtained.
Fig. 1.
AP Pelvis, pre-operative.
We choose to evaluate this patient post-operatively using the International Hip Outcome Tool-12, a questionnaire designed to assess treatment outcomes in young patients with hip pathology. iHOT 12 focuses on four parameters: (i) patient-reported symptoms and daily function, (ii) recreational and sport activities, (iii) social and job-related concerns and (iv) emotional and lifestyle concerns [7]. The femoral neck-shaft angle (NSA) was used as a radiographic parameter and was within normative values for the Canadian population (range 113–135) [5].
Intra-operative findings and surgical technique
The two procedures were performed in the same setting by two board-certified orthopedic surgeons. After administering a general anesthetic, the patient was positioned in supine position on a radiolucent traction table. A modified anterolateral portal and mid-anterior portal were utilized for the diagnostic arthroscopy, which revealed a partially detached (10- to 3-o'clock) hypertrophic labrum superolaterally. The adjacent cartilage was visibly softened at the superolateral acetabulum, and there was some fraying of the ligamentum teres. The posterior labrum was intact. Two suture anchors at the 10 and 2-o’clock positions were utilized for labral refixation using a vertical mattress technique. Femoral neck osteochondroplasty was completed under fluoroscopy which partially restored the offset and concavity. Capsular re-approximation of the T capsulotomy was completed before wound closure.
The patient was transferred to a fracture table to proceed with the Morscher’s osteotomy and percutaneous adductor tenotomy. A right hip corrective valgus osteotomy with greater trochanter distalization and fixation of the proximal femur using a 140° plate was completed. Then, a percutaneous adductor tenotomy was done and the wounds were closed.
Post-operative rehabilitation and outcomes
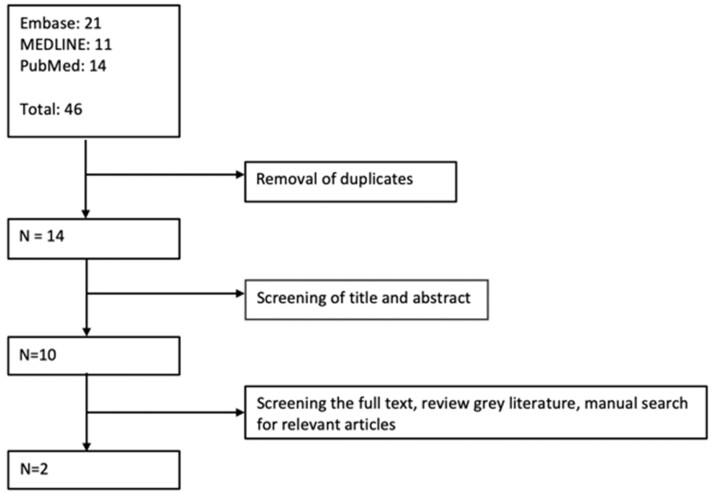
Figure 2 illustrates the radiological characteristics observed after surgery. The International Hip Outcome Tool (iHOT12) was used to evaluate the patient’s ability to perform daily tasks. The pre-operative score was 16.3; the 8-month post-operative score was 79.8. The patient denied taking any pain medications or using walking aids. The femoral neck-shaft angle (NSA) was measured to report radiologic results since other imaging parameters of the proximal femur were difficult to deduce due to hardware interference. The pre- and post-operative NSA was 120 and 138.7, respectively, indicating correction of coxa vara. Also, the offset increased post-operatively when measured radiographically and the femoral head-neck convexity also improved. Figure 2 illustrates the radiological characteristics after surgery.
Fig. 2.
AP Pelvis, post-operative.
LITERATURE SEARCH
Broad search terms were used to capture all relevant articles in the literature using three search engines: Medline, Embase and Pubmed. A total of 46 articles were found. Our inclusion criteria are any paper that discusses individual and simultaneous osteotomy of the hip or pelvis with arthroscopic management in pediatrics as a management of LCPD. Ten relevant articles were included after the title and abstract screening phase and removal of duplicates. After the full-text review, two articles discussing management with surgical hip dislocation and femoral neck lengthening met the inclusion criteria. Furthermore, manual search was done on related journals but did not reveal any articles (Fig. 3).
Fig. 3.
Search strategy flow chart.
The first study by Faure et al. [8] demonstrated the effects of true femoral neck lengthening with great trochanter transposition through surgical dislocation in 15 patients with LCPD and Developmental Dislocation of the Hip. The authors reported an improvement in articular-trochanteric distance, horizontal femoral offset and limb-length discrepancy in all patients. Complications included progression of OA, decreased joint space and pulmonary embolism [8]. Isolated relative femoral neck lengthening through surgical hip dislocation was reported by Anderson et al. [9]. This study demonstrated a mean Harris Hip score improvement of 21 points in 14 patients. Four of the fourteen patients, however, also demonstrated progression of OA [9].
Another search was performed focusing on the indications for proximal femoral osteotomies. Leunig et al. [10] categorized this based on the procedure’s location. The most common, intertrochanteric osteotomy, is indicated for femoral neck malunion and non-union, LCPD, dysplasia and SCFE [10]. A varus positioned ITO can be used for cases of excessive coxa valga, caput valgum with a high fovea, segmental osteonecrosis or rarely in cases of concentric osteoarthritis; a valgus ITO can be useful for coxa vara, post-traumatic varus malunion or femoral neck nonunion and rarely for the isolated medial SCFE [10]. A subtrochanteric osteotomy allows for de-rotation of the femur in patients with isolated lower extremity torsional abnormalities; it is ideal for improving pain and biomechanical function in patients with dislocations but is only recommended in adults due to frequent loss of correction in younger patients [10]. Unlike intertrochanteric osteotomies, this does not interfere with growth plates of the greater or lesser trochanter [10]. Femoral neck osteotomy, which delays degenerative arthrosis, is employed for reduction and physeal fixation in patients with SCFE [10]. Moreover, this procedure facilitates intraoperative assessment of joint pathology and secondary procedures (e.g. chondroplasty, labral repair, and joint debridement) to be performed concomitantly [10].
DISCUSSION
Surgical management of LCPD varies and sometimes depends on surgeon preference and expertise. A triple pelvic osteotomy (TPO) is one surgical option. Pailhé et al. [11] found that TOP significantly improves Oxford Hip Score and may delay the onset of osteoarthritis. However, altered pelvic anatomy after TOP can make a future THA challenging [11]. Acetabular dysplasia caused by LCPD can be corrected with periacetabular osteotomy, retroversion with periacetabular osteotomy and rim trimming, and incongruity with a femoral osteotomy alone or with simultaneous acetabular osteotomy [5].
In patients with significant articular erosion, a THA may be necessary once skeletally mature. Since hip deformity can be asymptomatic in childhood and young adulthood, there may already be significant damages and degeneration to the hip articular cartilage by the time a patient is diagnosed with LCPD. Due to this insidious onset, more than half of patients with LCPD gradually develop OA and eventually need a THA. The average age of LCPD patients undergoing a THA is 37.5 years old, which is significantly younger than non-LCPD patients this will put them at higher risk of needing a revision surgery in the future [12].
In this case report, a novel technique that combines arthroscopic hip arthroscopy with Morscher’s osteotomy was presented. Arthroscopic osteochondroplasty reshapes the femoral head, reducing incongruity and correcting hip impingement. In addition, the damaged labrum is repaired. Morscher’s osteotomy improves abduction by transferring the greater trochanter and subperiosteal trimming of the proximal stable trochanter distally [13]. This lateralizes the femoral shaft via a double oblique osteotomy, increasing the lever arm of abductor muscles and helps to lengthen the femoral shaft and neck as well due to the angle of the osteotomy. In our patient, the Morscher Osteotomy corrected the femoral neck-shaft angle significantly. Eidelman et al. [3] found that a Morscher Osteotomy reduced length discrepancy by an average of 0.8 cm in patients with LCPD. A 17 points increase in HHS score, improved gait pattern and function as well as high patient satisfaction. Also, there were fewer complications.
Arthroscopic osteochondroplasty and Morscher’s osteotomy have been separately described in the literature for the management of LCPD, but have not been studied as a simultaneous procedure as per the findings of this publication. Risto et al. [13] discussed combining open osteochondroplasty and femoral neck lengthening for LCPD patients and reported that 74% of patients experienced functional improvements. Results from that study, however, did not recommend combining these two procedures for cases of severe deformity and patients younger than 28-years-old [13]. Baraka et al. [14] performed a combined Imhauser osteotomy with osteochondroplasty through the surgical hip dislocation approach on adolescent patients with moderate and severe stable slipped capital epiphysis. This involved surgical dislocation and osteochondroplasty followed by an intertrochanteric osteotomy and trochanteric transfer [14]. The mean preoperative HHS improved from 65.39 to 93.3 (27.91 points difference); the mean lower limb length discrepancy improved from 1.99 cm to 0.27 cm (1.72 cm) [14]. More recently, Faure et al. [8] reported on 15 patients who underwent undergoing open Morscher’s osteotomy through surgical dislocation approach. All patients showed horizontal femoral offset improvement by a mean of 32.3 mm (4–46.4 mm), articular–trochanteric distance increased by >5 mm and limb length improved by a median of 11.5 mm (3–30 mm) [8].
Optimal management for LCPD is evolving. Combining hip arthroscopy with Morscher’s osteotomy comes with its own set of possible complications. First, the two surgeries were conducted on the same day, prolonging anesthesia time which has inherent risks. A high degree of expertise is needed to tackle this condition with two unique approaches given the anatomical challenges. For example, the Morscher osteotomy may cause femoral shaft fractures or injure the superior gluteal, femoral and sciatic nerve or nearby tendons. Likewise, hip arthroscopy in the setting of altered anatomy (LCPD) can cause labral injury, over-resection of the deformity, transient pudendal nerve palsy and instrument breakage [15]. Since this is a novel case report, it has limited generalizability of findings and lack of standardized outcome metrics to facilitate comparison to other publications. More prospective cohort studies with longer-term follow-up will help define which approach leads to the best clinical outcomes.
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.
CONCLUSION
In conclusion, combining arthroscopic hip osteochondroplasty with morscher can restore functional anatomy, provide symptomatic relief and improve function for LCPD patients.
CONFLICT OF INTEREST STATEMENT
There is no conflict of interest to disclose.
FUNDING
This paper was published as part of a supplement financially supported by the European Society for Sports Traumatology, Knee Surgery and Arthroscopy (ESSKA) www.esska.org.
REFERENCES
- 1. Perry DC. The epidemiology of Perthes’ disease. Orthopaedic Proceedings. Available at: https://online.boneandjoint.org.uk/doi/abs/10.1302/1358-992X.95BSUPP_6.BSCOS2012-001 Accessed: 29 June 2020.
- 2. Wenger DR, Pandya NK.. A brief history of Legg-Calvé-Perthes disease. J Pediatr Orthop 2011; 31: S130–6. [DOI] [PubMed] [Google Scholar]
- 3. Eidelman M, Keshet D, Nelson S, Bor N.. Intermediate to long-term results of femoral neck lengthening (Morscher osteotomy). J Pediatr Orthop 2019; 39: 181–6. [DOI] [PubMed] [Google Scholar]
- 4. Loder RT, Skopelja EN.. The epidemiology and demographics of Legg-Calvé-Perthes’ disease. ISRN Orthop 2011; 2011: 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tannast M, MacIntyre N, Steppacher SD. et al. A systematic approach to analyse the sequelae of LCPD. HIP Int. 2013; 23: 61–70. [DOI] [PubMed] [Google Scholar]
- 6. Awad MAH, Bajwa AK, Slaunwhite E. et al. Indications for hip arthroscopy in pediatric patients a systematic review. J Hip Preserv Surg 2019; 6: 304–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Griffin DR, Parsons N, Mohtadi NGH, Safran MR, Multicenter Arthroscopy of the Hip Outcomes Research Network. A short version of the International Hip Outcome Tool (iHOT-12) for use in routine clinical practice. Arthrosc J Arthrosc Relat Surg 2012; 28: 611–8. [DOI] [PubMed] [Google Scholar]
- 8. Faure P-A, Zaltz I, Côté K. et al. Morscher osteotomy through surgical dislocation approach for true femoral neck lengthening with greater trochanter transposition. J Bone Jt Surg 2020; 102: 66–72. [DOI] [PubMed] [Google Scholar]
- 9. Anderson LA, Erickson JA, Severson EP, Peters CL.. Sequelae of Perthes disease: treatment with surgical hip dislocation and relative femoral neck lengthening. J Pediatr Orthop 2010; 30: 758–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Leunig M, Puloski S, Beck M. et al. Proximal femoral osteotomy: current indications and techniques. Semin Arthropl 2005; 16: 53–62. [Google Scholar]
- 11. Pailhé R, Cavaignac E, Murgier J. et al. Triple osteotomy of the pelvis for Legg-Calve-Perthes disease: a mean fifteen year follow-up. Int Orthop 2016; 40: 115–22. [DOI] [PubMed] [Google Scholar]
- 12. Masrouha KZ, Callaghan JJ, Morcuende JA.. Primary total hip arthroplasty for Legg-Calvé-Perthes syndrome: 20 year follow-up study. Iowa Orthop J 2018; 38: 197–202. [PMC free article] [PubMed] [Google Scholar]
- 13. Risto O, Sandquist S, Lind S, Madan S.. Outcome after osteochondroplasty and relative neck lengthening for patients with healed Legg-Calvé-Perthes disease: a retrospective cohort study of patients with hip-deformities treated with osteochondroplasty and relative neck lengthening. HIP Int 2019; 112070001989676. [DOI] [PubMed] [Google Scholar]
- 14. Baraka MM, Hefny HM, Thakeb MF, Fayyad TA. et al. Combined Imhauser osteotomy and osteochondroplasty in slipped capital femoral epiphysis through surgical hip dislocation approach. J Child Orthop 2020; 14: 190–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Nwachukwu BU, McFeely ED, Nasreddine AY. et al. Complications of hip arthroscopy in children and adolescents. J Pediatr Orthop 2011; 31: 227–31. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.