Abstract
The medial collateral ligament (MCL) is a major stabilizer of the knee joint, providing support against rotatory and valgus forces; moreover, it is the most common ligament injured during knee trauma. The MCL injury results in valgus instability of the knee and makes the patient susceptible to degenerative knee osteoarthritis. Although it has been nearly a dogma to manage MCL injury nonoperatively, recent literature has suggested operative MCL management as a suitable option for specific patient populations. The present review aimed to assess the current literature on the management of MCL injuries of the knee. In this regard, we go over the anatomy, physical examination, and MCL imaging.
Key Words: MCL, MCL reconstruction, MCL repair, POL, PMC
Introduction
The medial collateral ligament (MCL) is the most common knee ligament to be injured during knee trauma (1). The annual incidence of MCL injury has been reported as 0.24-7.3 per 1,000 people with a male to female ratio of 2:1 (1, 2). A ten-year observational study demonstrated that the injury occurs in 7.9% of all athletic knee injuries (3). It is a common injury during popular sports, such as soccer, skiing, or ice hockey, as a result of either a direct valgus force to players’ knees or cutting maneuvers, when athletes plant a foot and suddenly shift their direction or speed (1, 4, 5). The injury may result in knee instability against the rotational or valgus force. In their study, Memarzadeh et al. indicated that MCL injury often presents as an isolated injury; nonetheless, it may occur in combination with other ligament injuries, mostly anterior cruciate ligament injury (1). Since the MCL is an extra-articular ligament with a high healing ability, most of its injuries can be treated nonoperatively; however, the surgery may be indicated in certain instances (5). In this review, we discuss this concept with the aim of delineating the management principles of the MCL injury.
Anatomy and biomechanics
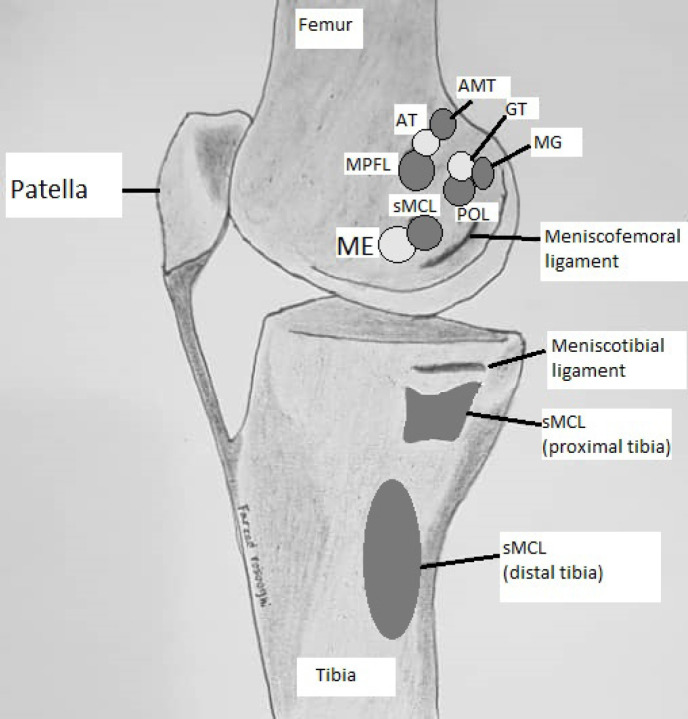
The MCL consists of superficial and deep parts, and superficial MCL (sMCL) is one of the most important stabilizing structures of the medial knee. It originates from 3.2mm proximal and 4.8mm posterior to the medial femoral epicondyle [Figure 1]. It has two insertions on the tibia: the proximal division attaches 12mm distal to the plateau articular surface, and the distal division inserts on a point 6 cm distal to the joint line (6). The recent studies pointed out that the proximal division is the primary knee stabilizer against valgus stress, while the distal division is a primary stabilizer against both internal and external rotation moments. In other words, the proximal and distal divisions of the sMCL perform different roles in knee stabilization. Therefore, in any surgical reconstruction of the MCL injury, it has been proposed to fix the applied graft distally to the tibia at both proximal and distal anatomical insertion zone of the sMCL (7, 8).
Figure 1.
Attachment sites of the medial knee stabilizers. Abbreviations: AMT: Adductor Magnus tendon, AT: adductor tubercle, MPFL: medial patellofemoral ligament, ME: medial epicondyle, sMCL: superficial MCL, POL: posterior oblique ligament, GT: gastrocnemius tubercle, MG: medial head of the gastrocnemius muscle
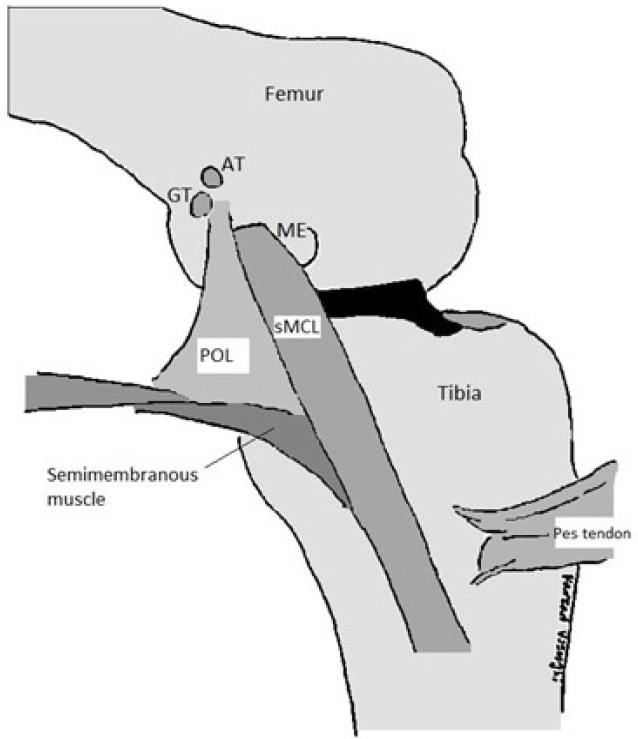
The deep part of the MCL (dMCL) is the thick part of the middle third of the medial knee capsule. It has two arms, namely meniscofemoral and meniscotibial, and attaches the medial meniscus to the joint capsule (6). The structures of the medial knee posterior to the MCL known as the Posteromedial corner (PMC) are another important stabilizer of the medial knee. They consist of Posterior Oblique Ligament (POL), semimembranous insertion, Oblique Popliteal Ligament (OPL), medial joint capsule, and posterior horn of the medial meniscus. POL is a capsular thickening of the knee joint attaching to the semimembranosus muscle (7). Its proximal attachment is on the distal femur near the insertion site of the medial head of the gastrocnemius muscle, and its distal attachment is on the posteromedial side of the tibia [Figure 2] (6).
Figure 2.
Posteromedial corner structure, POL is a continuation of the semimembranous insertion on the medial joint capsule, distal femur, and the medial meniscus. Abbreviations: POL: posterior oblique ligament, AT: Adductor Magnus Tubercle, GT: gastrocnemius tubercle, ME: medial epicondyle, sMCL: Ssuperficial Medial Collateral Ligament
During knee joint flexion, the semimembranosus muscle contracts and tightens the posteromedial knee capsule and the POL. It also pulls the medial meniscus posteriorly and prevents the anterior subluxation of the tibia. Another important role of the semimembranosus muscle is internal rotation of the tibia. Therefore, PMC injuries may lead to anterior tibial subluxation by damaging the function of the semimembranosus muscle and results in external tibial rotation. The anterior subluxation of the medial tibial condyle observed by the flexion of the injured knee is known as anteromedial rotatory instability (AMRI) and may be caused by PMC injuries (9).
History and Physical examination
Acute isolated MCL injury may present by local swelling, ecchymosis, and tenderness in the medial knee. Incomplete MCL injuries might be more painful than a complete tear of the MCL (5). Joint effusion within 2 hours after the injury is in favor of hemarthrosis and suggests intraarticular pathology, such as cruciate ligaments injury (5, 9). The best time for physical examination is the first hours after the injury before the occurrence of muscle spasms. Nevertheless, in the event of muscle spasticity, it may be suitable to examine the patient after 24 hours of immobilization when the spasm has subsided (5, 10). Special attention should be paid to lower limb alignment since valgus malalignment puts more pressure on the medial knee, and its correction should be considered.
During the physical examination, medial laxity of the knee in 30° flexion while abducted by a valgus force is indicative of MCL injury. However, if valgus instability is still observed at 0 degrees knee flexion, the injury is more extensive, and either cruciate ligaments or PMC may be also injured (1). The examination should also include the evaluation of the Anterior Cruciate Ligament (ACL) and Posterior Cruciate Ligament (PCL) by the anterior and posterior drawer test, respectively, in addition to the assessment of menisci and posterolateral corner (PLC) status. Anterior subluxation of the leg at 90 degrees of knee flexion suggests ACL injury or AMRI. However, anterior subluxation of the medial tibial condyle while the knee is 15 degrees externally rotated and 90 degrees flexed is specific for AMRI (Slocum test) (9, 11). Assiduous attention is needed in the interpretation of the Pivot shift test since it may have higher false-negative results in the presence of MCL injury (5).
The dial test is one of the useful tests for the examination of the PLC; however, it is very important to differentiate the reason for the positive dial test. A positive dial test may indicate PMC injury as well. In the dial test, the amount of foot external rotation is evaluated, in comparison with the contralateral side while the patient is in the supine or prone position and is performed in 30- and 90-degrees of knee flexion. A foot external rotation of at least 15 degrees more than the other side both in 30 and 90 degrees of knee flexion may indicate either combined PCL and PLC injury or PMC injury (1). If external rotation is accompanied by anterior subluxation of the medial tibial plateau, PMC injury will be the probable cause. On the contrary, posterior subluxation of the lateral tibial plateau increases the likelihood of combined PCL and PLC injury.
Classification of medial collateral ligament injury
The American Medical Association classified the MCL injury into three grades. Grade I injuries indicate only some minimal torn fibers without any loss of ligamentous integrity (stretch injury). In grade II, there is a partial tear of the MCL. Grade III injuries show severe complete disruption of a ligament. By performing a valgus stress test in 30 degrees of knee flexion, patients with grade III MCL injury experience valgus knee laxity (5). In their study, Hughston et al. subdivided grade III injuries into categories of 3-5 mm, 5-10 mm, and ≥10mm based on the amount of increased medial knee space during the knee abduction stress test (3). Nonetheless, the clinical classifications proposed for the MCL injury are relatively based on subjective opinions; moreover, to the best of our knowledge, their validity and reliability have not been assessed and approved (5).
Diagnosis
AnteroPosterior (AP) weight-bearing, lateral, sunrise view, and valgus stress radiographs of the knee can be used for primary evaluation of MCL injury (10). Since lateral plateau fracture may cause knee valgus instability, plain knee radiographies are of great help to distinguish between medial knee ligamentous and bony instability due to a depressed lateral plateau in acute knee trauma. Ossification of the proximal part of the MCL (Pellegrini-Stieda sign) is suggestive of chronic MCL injury. Moreover, bone avulsion in peripheral rim of the medial tibial plateau (reverse Segond sign) may point to MCL injury (3).
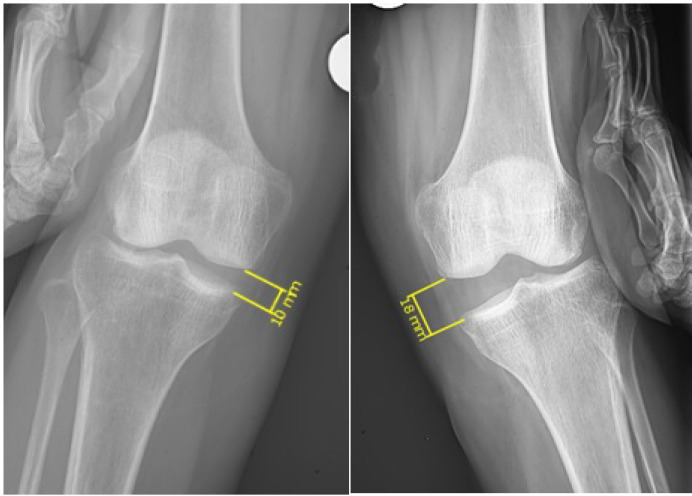
During the valgus stress radiography, while the knee is flexed to 30 degrees, medial knee gap side-to-side difference of at least 3.2mm is suggestive of complete sMCL injury, and if this difference is higher than 9.8mm, it indicates combined MCL/PMC injury. Side-to-side difference of less than 3.2 mm denotes either intact or partially injured sMCL [Figure 3] (12). Stress radiography in a skeletally immature patient can be of great help in the diagnosis of physeal injuries (5).
Figure 3.
Valgus stress radiography, Medial knee gap side to side difference of at least 3.2mm suggests complete sMCL injury. In this case, the difference of medial knee gap between the two sides was 8 mm. During the operation, a complete tear was demonstrated in the sMCL of the left knee. Abbreviations: sMCL: Superficial part of the medial collateral ligament
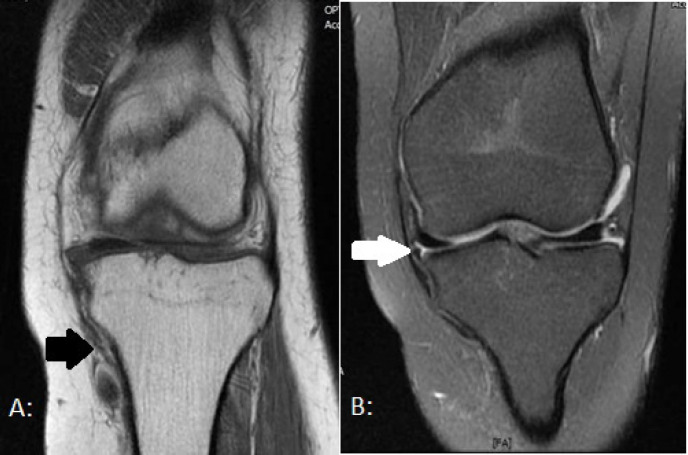
Magnetic Resonance Imaging (MRI) may be indicated in the presence of grade III valgus knee laxity in order to explore the possibility of multi-ligament knee injury (MLKI) (5). Moreover, it localizes the exact site of damage [Figure 4]. On MRI (T2-weighted sequences), grade I MCL injured cases (minor sprain) have increased signal intensity medial (superficial) to the ligament; nonetheless, the MCL itself looks normal. In grade II (severe sprain or partial tear), partial-thickness enhanced MCL signal is observed. Finally, in grade III, complete disruption of the ligament is noted on MRI (1).
Figure 4.
Magnetic resonance imaging (MRI) of a patient with MCL injury, An injury in the sMCL can be detected on T1-weighted MRI (picture A, black arrow), and a tear in deep MCL (dMCL) is marked with a white arrow on T2-MRI view in picture B. Abbreviations: MRI: Magnetic resonance imaging, MCL: Medial collateral ligament, sMCL: Superficial part of the medial collateral ligament, dMCL: Deep part of the medial collateral ligament
The MRI-based grading is not necessarily in accordance with clinical MCL grading. The level of agreement between MRI and clinical grading was obtained at 92% in one study (13). Tiwari et al. have reported two cases with medial knee tenderness and a positive valgus knee stress test that turned out to have grade III MCL injury during open exploration. Nonetheless, the knee MRI for both cases failed to reveal any obvious sign of MCL injury (14). Consequently, high clinical suspicion of MCL injury may merit further examination using arthroscopy or open exploration (3).
Treatment
Non-operative care has been proposed as the mainstay of treatment in the majority of isolated MCL injuries regardless of their injury severity. Previously conducted studies demonstrated that prolonged immobilization culminates in collagen degradation of the MCL and bone resorption at the insertion point of the ligament. This finding highlights the importance of early initiation of Range of Motion (ROM) exercises in nonoperative protocols (1, 5). Grade I injury can be managed without a brace; nonetheless, a hinged knee brace is required for grade II and grade III cases (15). Grade II and III cases usually have to wear the brace for at least three and six weeks, respectively (15). ROM exercises should be initiated at the earliest opportunity with weight-bearing as tolerated. On walking, the brace is locked in full extension till the patient’s extension lag is improved. Straight leg raising test, quadriceps sets, and patella mobilization are started at the beginning of rehabilitation and help patients with MCL injury to increase the strength of their quadriceps and mobilize their knee joint. Closed chain exercises will be practiced after full weight-bearing (15).
The indications for surgical management are presented in Table 1 (5, 16). In cases of femoral avulsion of the MCL, the free end of the injured MCL stays near its previous attachment site. Consequently, the healing potential of the ligament is often retained and it may be healed by conservative management. On the contrary, the tibial avulsion of the MCL may results in the interposition of the pes anserine muscles between the tibia and the injured MCL, preventing the ligament from healing on its own. This situation which is called Stener-type lesion mandates surgical management [Figure 5] (1, 2). Acute cases (≤3weeks since injury) with planned surgery are mostly managed by direct MCL repair. However, cases with subacute (from three weeks to six weeks from the trauma), chronic MCL injury (time since the injury of more than six weeks), or patients with poor ligament quality may be scheduled for ligament reconstruction (1, 11, 17).
Table 1.
Clues in favor of operative management of the MCL injury during patients’ evaluation
| History and physical examination | Open MCL injury |
| Medial knee laxity when a valgus stress is inserted to the fully-extended knee | |
| AMRI | |
| Examination suggestive of MLKI | |
| Chronic symptomatic MCL injury despite being conservatively treated for at least 6 weeks | |
| Radiologic studies | Valgus malalignment of the injured knee |
| Associated tibial plateau fracture | |
| Large bone avulsion | |
| Stener type lesion | |
| Work up suggestive of MLKI | |
| Entrapment of the MCL under the medial meniscus |
Abbreviations: MCL: Medial collateral ligament, AMRI: Anteromedial rotatory instability, MLKI: Multiligament knee injury
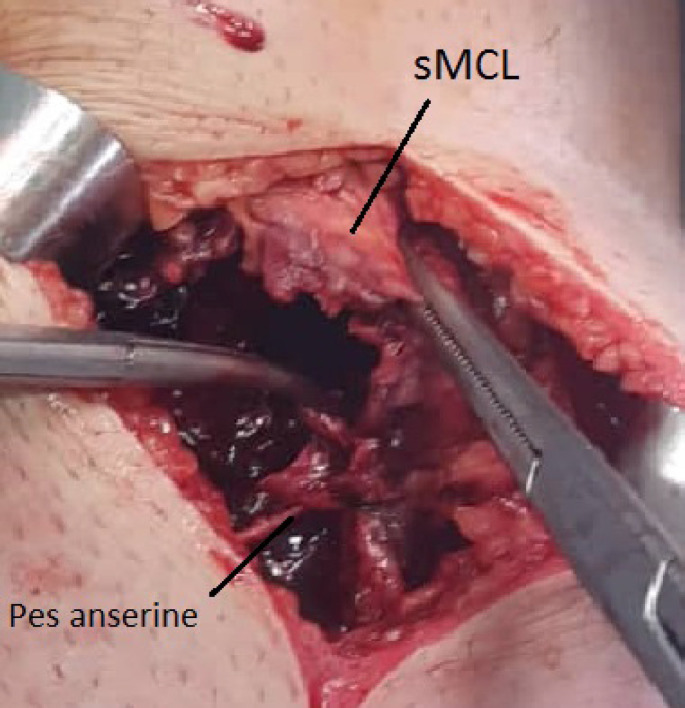
Figure 5.
Stener-type lesion, This is an intraoperative photo of a patient with Stener-type lesion. The MCL was avulsed from the tibia, and the distal end of the MCL was moved from its original place (deep to the Pes anserine tendons) and positioned superficial to the Pes anserine tendons. Abbreviations: MCL: Medial collateral ligament, sMCL: superficial part of the medial collateral ligament
As already mentioned, MLKI is an indication for surgery; nonetheless, the timing of the surgery is controversial. Surgeries scheduled later result in less inflammation and swelling during the operation. In addition, delayed surgical management of the injured ligament is associated with fewer incidences of post-surgical arthrofibrosis. On the contrary, as time passes, more scar tissues are grown in the area complicating the procedure. Some surgeons conduct the extra-articular soft tissue surgical management within two weeks post-surgery, followed by delayed cruciate reconstruction after the patient regains the knee ROM (18). In a systematic review, Jiang et al. demonstrated that staged management is associated with a higher excellent/good result, compared to either early or delayed operative management of MLKI (19). Surgical repair versus the reconstruction of PMC and MCL in MLKI is another important question. Stannard et al. showed that in MLKI following knee dislocation, surgical repair of the PMC is associated with a higher failure rate, as compared to PMC reconstruction (20).
Numerous management options have been proposed in the literature for the combined ACL-MCL injury cases [Table 2]. It is a well-established practice to reconstruct the ACL and manage MCL conservatively(21). However, in the presence of other operative indications for MCL (as depicted in Table 1), combined ACL-MCL injury may be managed with early ACL reconstruction and MCL exploration. The timing for ACL reconstruction for cases with combined ACL-MCL injury is still open to debate. Grant recommended treating MCL injury conservatively and postpone ACL reconstruction until six weeks post-trauma (22). After ACL reconstruction, valgus stress radiography can be performed intraoperatively. Exploration and surgical management of the MCL should be considered in the presence of persistent valgus laxity. Dong et al. compared the outcomes of direct repair with the reconstruction of the MCL in cases with combined ACL-MCL injury. They indicated that reconstruction provides the knees with more rotational stability (11). However, with the introduction of internal brace augmentation techniques using high-strength sutures, more studies may be required to further determine the MCL management of choice in the MLKI cases. Moreover, a biomechanical study revealed that the moment needed to disrupt the internal brace was not significantly different from the force required to fail the anatomical MCL reconstruction (23).
Table 2.
Different management options proposed in the literature for combined ACL-MCL injury
| Study | ACL management | MCL management | Outcome |
|---|---|---|---|
| Jokl et al. (1984) (34) | Nonop. | Nonop. | 68% of cases returned to their activity. |
| frolke et. al (1998)(35) | Nonop. | operative | 68% of participants returned to their activity. |
| Halinen et al. (2006) (36) | Recons. | Nonop. vs operative | MCL Nonop. management was associated with knee stability and reoperation rates similar to those undergoing MCL Recons. in 96% of cases. |
| Halinen et al. (2009) (37) | Recons. | Nonop. vs operative | MCL Nonop. management was associated with better knee flexion in the first 9 month postoperatively. |
Abbreviations: ACL, anterior cruciate ligament, MCL: Medial collateral ligament, Nonop: Nonoperative, Recons: reconstruction, vs: versus
Surgical Technique
Direct repair is recommended for acute cases. After incising the skin from the medial femoral condyle to the anteromedial tibia around 6 centimeters distal to the knee joint line, the sartorial fascia is dissected. Care should be taken in order to keep the saphenous nerve intact. Thereafter, the pes anserinus tendon is retracted to reach the MCL. The stabilizing medial knee structures are repaired from deep to superficial layers (24). Firstly, the medial meniscus and its attachment to the dMCL should be explored and managed. Following that, injury to the dMCL, POL, and sMCL can be addressed, respectively (25).
Regarding the POL, its distal attachment should be repaired after the proximal counterpart. Subsequently, after drifting the POL anteriorly, the middle part of the POL’s anterior border should be fixed to the sMCL by pants-over-vest sutures(25). This closes the gap in the medial side of the knee and tightens the PMC, stabilizing the joint further against valgus laxity (26). In addition, the semimembranosus muscle is evaluated. In the presence of any laxity, its capsular arm should be anteriorly advanced and fixed to the POL with pants-over-vests sutures (24, 26). Historically, pants-over-vests sutures have been recommended to fix injured medial knee ligaments (5, 24, 25). However, interlocking Bunnel and Kracków sutures are also utilized for repairing MCL in the literature (27, 28).
Proximal or distal bony avulsions of the medial knee ligaments can be repaired by screw fixation (16). Nowadays, there is a growing interest to repair MCL “peel-off” injuries or small bony MCL avulsions with anchor sutures (29). Mid-substance tears are needed to be sutured and simultaneously augmented since they are more difficult to be repaired. Recently, the advent of ultrahigh Molecular Weight Polyethylene (FiberWire®) Sutures with their strength against abrasion has revolutionized the ligament repairing techniques. The use of ultrahigh-molecular-weight polyethylene/polyester suture tape (FiberTape) further enhances the strength of the ligament repairs (25, 27, 28).
Ligament reconstruction is indicated whenever a chronic MCL injury or failed MCL repair is encountered or whenever the ligament quality is inappropriate (1). It provides the knee with stability against valgus and rotational stress. Nonetheless, similar to surgical MCL repair, it may also be associated with knee stiffness (2, 10). Before the management of patients undergoing MCL reconstruction, it is important to evaluate knee meniscus and ligaments by arthroscopy and examination under anesthesia. Furthermore, any valgus malalignment of the injured knee should be addressed with osteotomy prior to the reconstruction surgery (1, 17).
To date, different types of reconstruction have been proposed which are selected by knee surgeons depending on their experience, the presence of other ligament injuries, and the availability of surgical equipment. Isolated chronic MCL injuries unresponsive to conservative treatment can be managed with isolated MCL augmentation with semitendinous autograft (12). When MLKI simultaneously affects PMC and MCL, more advanced techniques may be selected, including combined MCL reconstruction and posteromedial capsule reefing, or MCL plus POL reconstruction. Van der Wal et al. demonstrated that posteromedial capsule reefing performed simultaneously with MCL reconstruction may have a stabilizing result against valgus knee laxity, similar to the methods reconstructing both MCL and POL(30).
LaPrade’s anatomical reconstruction of sMCL and POL needs more grafts and is more technically demanding. More bone tunnels should be drilled for holding the grafts, and the MCL bone tunnels may risk the other reconstructed ligaments in cases with multiligament injuries. However, it will provide a better biomechanics if performed correctly (31). LaPrade et al. proposed to use two separate ligament grafts for the reconstruction of MCL and POL [Figure 6]. They used two separate tunnels in the femur and two tibial tunnels to fix the grafts at the anatomical attachment points of MCL and POL. They also reported that the use of this technique gives the best biomechanical property to the knee joint. Moreover, they found that 100% of patients had less than 3 mm medial knee gap on valgus stress radiographs during a follow-up period of 18 months (32).
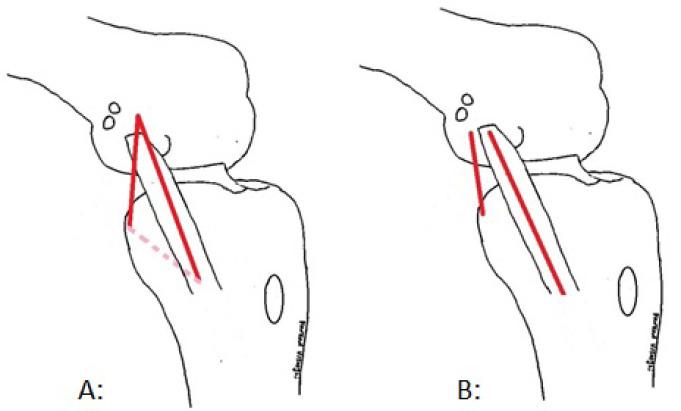
Figure 6.
Schematic pictures of the Triangular vector ligament reconstruction (A) and the Laprade anatomical ligament reconstruction (B). The knee is semi-flexed and the position of the graft (red line) relative to the MCL is shown in the pictures. The circular area in each picture shows the relative insertion site of pes anserine muscles on the tibia. Abbreviations: MCL: medial collateral ligament
Hongtao Xu proposed a method with one femoral tunnel and one tibial tunnel to reconstruct MCL and POL [Figure 6]. In this method called triangular vector ligament reconstruction, the attachment sites of MCL and POL on the femur and tibia are marked. Thereafter, two pins are positioned on the knee joint between the origin and insertion site of each of the two ligaments (POL and MCL) to simulate the relative path of each ligament. The intersection of the two pins on the femur is marked as the best place to position the femoral tunnel. The insertion sites of the two ligaments on the tibia are used as the endpoints of the tibial tunnels. After drilling the femoral tunnel mediolaterally and the tibial tunnel posteroanteriorly, an allograft is inserted through the tibial tunnel. Finally, the endpoints of the graft are fixed at the femoral tunnel. Hongtao found that the medial knee gap on the valgus stress radiographs (with 30 degrees of knee flexion) decreases from 10.32 to 3.13mm using this method (33).
Postoperative rehabilitation
The exact postoperative protocol is still a topic of debate. It is a common practice to give the patient a hinged knee brace postoperatively for at least 4-6 weeks. Jacobson recommended that the brace be set at 45 degrees of flexion in isolated medial knee repair and increment 15 degrees of passive knee extension every 2 weeks. The weight-bearing would be started when a 15 degree of flexion is reached. In the presence of ACL injury; however, he was a proponent of keeping the brace at full extension and following an ACL rehabilitation protocol (9). Nevertheless, delayed initiation of knee motion, as proposed in this approach, makes the patients more prone to arthrofibrosis.
According to LaPrade et al., postoperatively, patients with MCL injury should be encouraged to start knee ROM within the safe zone determined during the operation for the first two weeks, and since then, they can gradually increase their ROM to the normal limits. Moreover, patients are recommended to exercise straight leg raising in braces until they can do this without knee extension lag. After six weeks, MCL-injured individuals are recommended to start weight-bearing as tolerated. Strengthening exercises can be initiated once their gait is normalized, commonly after 4-5 months (32).
It may be possible to begin weight-bearing earlier by augmenting MCL surgical repair with an internal bracing technique using high-strength sutures. Golden et al. proposed to initiate ROM within 0-90 degrees of flexion and partial weight-bearing in the first two weeks postoperatively. After two weeks, the ROM could be increased to 120-degree flexion with a full weight-bearing protocol (28).
The majority of patients with MCL injury can be treated conservatively by hinged knee brace and early ROM. Nonetheless, understanding the surgical indications of the MCL injury, including Stener-type lesion, AMRI, MLKI, and chronic MCL injuries unresponsive to conservative treatment, may help the orthopedic surgeon to decide if the patient benefits from the surgical intervention. Whether operative or conservative therapy is selected, the early initiation of ROM would be a key part of the MCL management in order to prevent arthrofibrosis.
Conflicts of Interest:
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
References
- 1.Memarzadeh A, Melton J. Medial collateral ligament of the knee: anatomy, management and surgical techniques for reconstruction. Orthopaedics and Trauma. 2019;33(2):91–9. [Google Scholar]
- 2.DeLong J, Waterman B. Surgical Techniques for the Reconstruction of Medial Collateral Ligament and Posteromedial Corner Injuries of the Knee: A Systematic Review. Arthroscopy The Journal of Arthroscopic and Related Surgery. 2015;31(11):2258–72. doi: 10.1016/j.arthro.2015.05.011. [DOI] [PubMed] [Google Scholar]
- 3.Andrews Kyle, Lu Alex, McKean L, Nabil E. Review: Medial collateral ligament injuries. Journal of Orthopaedics. 2017;14(4):550–4. doi: 10.1016/j.jor.2017.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Robinson J, Bull A, Thomas R, Amis A. The Role of the Medial Collateral Ligament and Posteromedial Capsule in Controlling Knee Laxity. The American journal of sports medicine. 2006;34(11):1815–23. doi: 10.1177/0363546506289433. [DOI] [PubMed] [Google Scholar]
- 5.Phisitkul P, James S, Wolf B, Amendola A. MCL Injuries of the Knee: Current Concepts Review. The Iowa orthopaedic journal. 2006:26:77–90. [PMC free article] [PubMed] [Google Scholar]
- 6.LaPrade R, Engebretsen A, Ly T, Johansen S, Wentorf F, Engebretsen L. The anatomy of the medial part of the knee. The Journal of bone and joint surgery American volume. 2007;89(9):2000–10. doi: 10.2106/JBJS.F.01176. [DOI] [PubMed] [Google Scholar]
- 7.Wijdicks C, Ewart D, Nuckley D, Johansen S, Engebretsen L, LaPrade R. Structural Properties of the Primary Medial Knee Ligaments. The American journal of sports medicine. 2010;38(8):1638–46. doi: 10.1177/0363546510363465. [DOI] [PubMed] [Google Scholar]
- 8.Griffith C, LaPrade R, Johansen S, Armitage B, Wijdicks C, Engebretsen L. Medial Knee Injury: Part 1, Static Function of the Individual Components of the Main Medial Knee Structures. The American journal of sports medicine. 2009;37(9):1762–70. doi: 10.1177/0363546509333852. [DOI] [PubMed] [Google Scholar]
- 9.Jacobson K, Chi F. Evaluation and Treatment of Medial Collateral Ligament and Medial-sided Injuries of the Knee. Sports medicine and arthroscopy review. 2006;14(2):58–66. doi: 10.1097/01.jsa.0000212305.47323.58. [DOI] [PubMed] [Google Scholar]
- 10.Chen L, Kim P, Ahmad C, Levine W. Medial collateral ligament injuries of the knee: Current treatment concepts. Current reviews in musculoskeletal medicine. 2008;1(2):108–13. doi: 10.1007/s12178-007-9016-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dong J, Wang X, Men X, Zhu J, Walker G, Zheng X, et al. Surgical Treatment of Acute Grade III Medial Collateral Ligament Injury Combined With Anterior Cruciate Ligament Injury: Anatomic Ligament Repair Versus Triangular Ligament Reconstruction. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2015;31(6):1108–16. doi: 10.1016/j.arthro.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 12.Serra Cruz R, Olivetto J, Dean C, Chahla J, LaPrade R. Superficial Medial Collateral Ligament of the Knee: Anatomic Augmentation With Semitendinosus and Gracilis Tendon Autografts. Arthroscopy Techniques. 2016;5(2):e347–e52. doi: 10.1016/j.eats.2016.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lundblad M, Hägglund M, Thomeé C, Hamrin Senorski E, Ekstrand J, Karlsson J, et al. Medial collateral ligament injuries of the knee in male professional football players: a prospective three-season study of 130 cases from the UEFA Elite Club Injury Study. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2019;27(11):3692–8. doi: 10.1007/s00167-019-05491-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tiwari V, Marak D, Muellner M, Resinger C, Muellner T. Grade III Distal Medial Collateral Ligament Tear Missed by Magnetic Resonance Imaging: A Report of Two Cases. Cureus. 2018;10(3):e2251. doi: 10.7759/cureus.2251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Edson C. Conservative and Postoperative Rehabi-litation of Isolated and Combined Injuries of the Medial Collateral Ligament. Sports medicine and arthroscopy review. 2006;14(2):105–10. doi: 10.1097/01.jsa.0000212308.32076.f2. [DOI] [PubMed] [Google Scholar]
- 16.Tandogan R, Kayaalp A. Surgical treatment of medial knee ligament injuries: Current indications and techniques. EFORT Open Reviews. 2016;1(2):27–33. doi: 10.1302/2058-5241.1.000007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Encinas-Ullán CA, Rodríguez-Merchán E. Isolated medial collateral ligament tears: An update on management. EFORT Open Reviews. 2018;3(7):398–407. doi: 10.1302/2058-5241.3.170035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burrus MT, Werner B, Griffin J, Gwathmey F, Miller M. Diagnostic and Management Strategies for Multiligament Knee Injuries A Critical Analysis Review. The Journal of Bone and Joint Surgery. 2016;4(2):e1. doi: 10.2106/JBJS.RVW.O.00020. [DOI] [PubMed] [Google Scholar]
- 19.Jiang W, Yao J, He Y, Sun W, Huang Y, Kong D. The timing of surgical treatment of knee dislocations: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):3108–13. doi: 10.1007/s00167-014-3435-1. [DOI] [PubMed] [Google Scholar]
- 20.Stannard JP, Black BS, Azbell C, Volgas DA. Posteromedial corner injury in knee dislocations. J Knee Surg. 2012;25(5):429–34. doi: 10.1055/s-0032-1322605. [DOI] [PubMed] [Google Scholar]
- 21.Elkin J, Zamora E, Gallo R. Combined Anterior Cruciate Ligament and Medial Collateral Ligament Knee Injuries: Anatomy, Diagnosis, Management Recommendations, and Return to Sport. Current Reviews in Musculoskeletal Medicine. 2019;12(2):239–44. doi: 10.1007/s12178-019-09549-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grant J, Tannenbaum E, Miller B, Bedi A. Treatment of Combined Complete Tears of the Anterior Cruciate and Medial Collateral Ligaments. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2012;28(1):110–22. doi: 10.1016/j.arthro.2011.08.293. [DOI] [PubMed] [Google Scholar]
- 23.Gilmer BB, Crall T, DeLong J, Kubo T, Mackay G, Jani SS. Biomechanical Analysis of Internal Bracing for Treatment of Medial Knee Injuries. Orthopedics. 2016;39(3):e532–7. doi: 10.3928/01477447-20160427-13. [DOI] [PubMed] [Google Scholar]
- 24.Hughston J, Eilers AF. The role of the posterior oblique ligament in repairs of acute medial (collateral) ligament tears of the knee. The Journal of bone and joint surgery American volume. 1973;55(5):923–40. [PubMed] [Google Scholar]
- 25.Lubowitz J, Mackay G, Gilmer B. Knee Medial Collateral Ligament and Posteromedial Corner Anatomic Repair With Internal Bracing. Arthroscopy techniques. 2014;3(4):e505–8. doi: 10.1016/j.eats.2014.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hughston JC. The importance of the posterior oblique ligament in repairs of acute tears of the medial ligaments in knees with and without an associated rupture of the anterior cruciate ligament. Results of long-term follow-up. J Bone Joint Surg Am. 1994;76(9):1328–44. doi: 10.2106/00004623-199409000-00008. [DOI] [PubMed] [Google Scholar]
- 27.Van der List J, Difelice G. Primary Repair of the Medial Collateral Ligament With Internal Bracing. Arthroscopy Techniques. 2017;6(4):e933–e7. doi: 10.1016/j.eats.2017.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Golden T, Friedman A, Jazayeri R, Sanderson B, Levy E. Primary Repair of the Medial Collateral Ligament with a Double Row Suture Technique and Suture Tape Augmentation for Acute Tibial-Sided Injuries. Arthroscopy Techniques. 2019;8(4):e395–e8. doi: 10.1016/j.eats.2018.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Trofa D, Sonnenfeld J, Song D, Lynch TS. Distal Knee Medial Collateral Ligament Repair With Suture Augmentation. Arthroscopy Techniques. 2018;7(9):e921–6. doi: 10.1016/j.eats.2018.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Van der Wal WA, Van Gennip S, Heesterbeek PJ, Busch VJ, Wymenga AB. Anatomical superficial medial collateral ligament reconstruction with posteromedial capsule reefing successfully restores valgus knee laxity. Acta Orthop Belg. 2020;86(1):69–76. [PubMed] [Google Scholar]
- 31.Joshi A, Nagmani S, Thapa S, Pradhan I. Weave Technique for Reconstruction of Medial Collateral Ligament and Posterior Oblique Ligament: An Anatomic Approach Using Semitendinosus Tendon. Arthroscopy Techniques. 2019;8(11):e1417–e23. doi: 10.1016/j.eats.2019.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.LaPrade R, Wijdicks C. Surgical Technique: Develo-pment of an Anatomic Medial Knee Reconstruction. Clinical orthopaedics and related research. 2011;470(3):806–14. doi: 10.1007/s11999-011-2061-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xu H, Kang K, Zhang J, Xin D, Liu W, Jin G, et al. An anatomical-like triangular-vector ligament reconstruction for the medial collateral ligament and the posterior oblique ligament injury with single femoral tunnel: A retrospective study. Journal of Orthopaedic Surgery and Research. 2017;12:6. doi: 10.1186/s13018-017-0602-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jokl P, Kaplan N, Stovell P, Keggi K. Non-Operative Treatment of Severe Injuries to the Medial and Anterior Cruciate Ligaments of the Knee. The Journal of bone and joint surgery American volume. 1984;66(5):741–4. [PubMed] [Google Scholar]
- 35.Frölke JPM, Oskam J, Vierhout P. Primary reconstruction of the medial collateral ligament in combined injury of the medial collateral and anterior cruciate ligaments Short-term results Knee surgery. sports traumatology, arthroscopy : official journal of the ESSKA. 1998;6(2):103–6. doi: 10.1007/s001670050081. [DOI] [PubMed] [Google Scholar]
- 36.Halinen J, Lindahl J, Hirvensalo E. Range of Motion and Quadriceps Muscle Power After Early Surgical Treatment of Acute Combined Anterior Cruciate and Grade-III Medial Collateral Ligament Injuries A Prospective Randomized Study. The Journal of bone and joint surgery American volume. 2009;91(6):1305–12. doi: 10.2106/JBJS.G.01571. [DOI] [PubMed] [Google Scholar]
- 37.Halinen J, Lindahl J, Hirvensalo E, Santavirta S. Operative and Nonoperative Treatments of Medial Collateral Ligament Rupture With Early Anterior Cruciate Ligament Reconstruction: A Prospective Randomized Study. The American journal of sports medicine. 2006;34(7):1134–40. doi: 10.1177/0363546505284889. [DOI] [PubMed] [Google Scholar]