Abstract
Background:
Atypical femoral fractures are the femoral fractures located anywhere between the lesser trochanter and the supracondylar flare of the femur. Long-term bisphosphonates, as the most common preventive and treatment medications for osteoporosis, are thought to have an important role in these fractures. Most of the fractures should be treated surgically, and the complications are considerable.
Methods:
We searched Medline, CENTRAL, Embase, and DART on February 26, 2020. One author reviewed and retrieved citations from these four databases for irrelevant and duplicate studies, and two other authors independently extracted data from the studies and rated their quality.
Patients with surgical treatment of bisphosphonate-related atypical femoral fracture, according to the American Society for Bone and Mineral Research definition, were included. Animal studies, case reports, studies with high-energy trauma, pathological fracture, or malignancy-related fractures were excluded.
Results:
In total, 316 patients (348 fractures) were included in this study. Mean age of patients was 70.47 years, and 97.5% of them were female. Duration of using bisphosphonates was 4.04 to 8.8 years, and Alendronate was the most common type. Moreover, 65.27% and 34.72% of the reported fractures were in diaphyseal and subtrochanteric, respectively. Moreover, the most common fixation type was intramedullary. Rate of complication was 17.52%, and the most frequent one was non-union, followed by implant failure. The main limitation of this research was that most of the studies did not have a high level of evidence.
Conclusion:
An increase in the rate of atypical femoral fracture with its challenging management makes it an important issue to be noted by orthopedic surgeons. Based on the results of this study, subtrochanteric fractures might have more complications post-operatively and are suggested to be operated on by more experienced surgeons. It was also found that extra-medullary fixation increases the risk of complications. Future studies on union time, outcomes of different surgical methods, and teriparatide therapy may help shed more light on the surgical management of these fractures.
Key Words: Atypical femoral fractures, Bisphosphonates, Fracture fixation, Health policy, Osteoporosis, Teriparatide
Introduction
The American Society for Bone and Mineral Research (ASBMR) developed criteria for the diagnosis of atypical femoral fractures (AFFs) in 2013, including five major and four minor features. Nevertheless, only four major features must be evident for the diagnosis of AFF [Appendix 1] (1). Long-term use of bisphosphonates is thought to play a crucial role in the development of these fractures by inhibition of bone resorption and induction of osteoclast apoptosis (2, 3). The incidence of osteoporosis and fragility fractures has increased in the two past decades due to population aging. Therefore, the use of bisphosphonates is grown as they are the most common medications for the prevention and treatment of osteoporosis. This might be why, in recent years, orthopedic surgeons have encountered a growing number of AFFs (3-5).
Management of AFFs is challenging for orthopedic surgeons (6). A concerning issue is fracture healing, which seems to depend on several factors, including fracture type, mal-reduction at the site of the fracture, and suppression of bone turnover (7, 8). The conservative non-surgical treatments usually have poor results and are recommended only for patients with incomplete fractures or severe comorbidities (6). Most of the cases are treated surgically with intramedullary nailing or plating. Regarding biomechanical and biological advantages, intramedullary nailing is supposed to be the treatment of choice in a couple of studies while in some others it is not (9-11). Hence, there is a controversy and lack of knowledge about the standard choice of the treatment (12). Delayed union, non-union, and implant failures are encountered more frequently in intramedullary nailing, in comparison with typical femoral fractures (13, 14).
The present systematic review aimed to evaluate the current evidence for the surgical treatment of bisphosphonate-related AFFs, including different surgical methods and devices, to advance considerations that can be helpful to decrease the rate of complications and/or re-operations in the treatment.
Materials and Methods
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Inclusion criteria for considering studies for this review
This systematic review was performed on patients with surgical treatment of bisphosphonate-related atypical femoral fracture as defined by ASBMR. Studies that had reported neither fracture location nor type of fixation for bisphosphonate-related cases were excluded. There was no limitation in terms of timing, duration, or date of publication, and only the studies that were in English were included. All the clinical trials, cohort studies, or case series that had considered a surgical treatment for all or a group (more than one) of their patients were reviewed. Case reports, studies performed on animal models, and review articles were not included. Besides, studies that included patients with high-energy traumatic femoral fractures, pathologic fractures related to malignancy, or metabolic bone disease, except for osteoporosis, were not included in this systematic review.
Literature search strategy for identification of studies
The primary search process was conducted in Embase, CENTRAL, Medline, and DART databases according to the search strategies described in the protocol on February 26, 2020 [Appendix 2].
One of the authors imported citations from all databases into an Endnote library (version X9, Thomson Reuters, USA), and removed irrelevant studies by screening the title and abstract of the remainders of search results. Afterward, we retrieved full texts of the remainder of the citations for further screening, data collection processes, and quality assessment.
Two independent authors (H.V and R.M) reviewed the identified studies. After screening the abstracts based on the eligibility criteria stated in the protocol, full texts were evaluated based on inclusion and exclusion criteria [Appendix 2]. In case of disagreement, a third author made the final decision.
Data extraction and quality assessment
Two authors independently extracted data, including study title, name of the first author, publication year, population information (sample size, age, and gender of participants), type and level (I to IV) of study based on the American Academy of Orthopaedic Surgeons classification system for the Orthopaedic literature, type of bisphosphonate and duration of treatment, fracture location, fracture fixation method, use of teriparatide or any other concomitant therapy for treatment, inclusion criteria, outcomes, and bias assessment from full texts of articles. Subsequently, they entered this information into pre-designed data extraction forms in Microsoft Excel spreadsheets (version 2019, Microsoft Corporation, USA). It should be noted that no prophylactic nailing was included in the extracted data.
Two reviewers independently evaluated the studies in terms of risk of bias for randomized controlled trials in six domains of random sequence generation (selection bias for controlled trials), allocation concealment (selection bias for controlled trials), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), and selective reporting (reporting bias) according to the Cochrane risk-of-bias tool [Appendix 3]. Afterward, they categorized the domains as “low risk” of bias, “high risk” of bias, or “unclear risk” of bias for each article (15).
Regarding the non-randomized studies, the same reviewers meticulously evaluated the methodologic quality by using the Methodological Index for Non-Randomized Studies (MINORS). Based on the MINORS score, the lowest risk-of-bias global ideal score is 16 for non-comparative studies and 24 for comparative studies (16). Any disagreement between the two authors regarding the quality of studies was resolved through discussion or consultation with a third author.
Evidence synthesis
The inter-reviewer agreement was calculated by using the Kappa (k) statistic. The intra-class correlation coefficient (ICC) was calculated for the MINORS scores quality assessment. Due to the non-uniform nature of the studies in terms of their design, fracture location, type of bisphosphonate, and outcome measures, the results are presented in absolute numbers, mean, and narrative summary fashion.
Results
Description of included studies
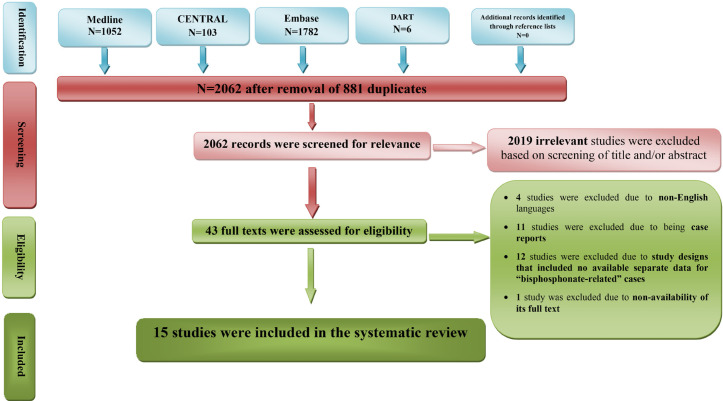
In total, 2943 references were found by applying the above-mentioned search strategy in three databases of journal articles and one database of grey literature. However, 881 duplicate citations were excluded using Endnote software as well as 2019 articles due to apparent irrelevancy of their topics in primary screening [Figure 1]. In the secondary screening of 43 full-text studies, 28 articles were excluded, and finally, 15 studies with 316 patients were included in this systematic review [Table 1] (8, 10, 11, 17-28).
Figure 1.
PRISMA flow diagram showing the systematic review of surgical treatment for Bisphosphonate-related atypical femoral fracture
Table 1.
Patients characteristics, fracture type, fixation type, and outcome in selected studies
| General information of studies and demographic characteristics of patients | Past medical and drug history |
Operative management
(fracture location and fixation type) |
Post-op management and evaluation | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
First Author,
Country, Publication Year |
Level of Evidence
Study design |
Total number of AFF (surgically treated) |
Mean age
---- Female (All patients) |
Risk factors | Type of BP | Duration of BP therapy | Fracture location | Fracture fixation type | Teriparatide medical therapy | Outcome measure | Complications | Follow-up |
| Canbek, Turkey, 2019 |
Level III Retrospective case-control study |
32 | 74±6 ---- 32 (32) |
Diabetes Mellitus | NA | Open Surgery GP: 6.7±1.4 years Close Surgery GP: 7.2±1.5 years |
Femoral Shaft - all | CMN GP1: (n=8) GP2: (n=8) Standard GP1: (n=7) GP2: (n=9) |
- | Primary union Radiologic union time: (months) GP1: 6.8±1.8 GP2: 5.1±1.3 |
Non-union GP1: (n=1) - revision GP2: (n=1) |
Months GP1: 41±10 GP2: 34±8 At least 24 |
| Rajput, Pakistan, 2019 |
Level III Retrospective cohort |
11 | 68.8 ---- 10 (10) |
- | Alendronate (n=4) Ibandronate (n=3) Zoledronic acid (n=3) |
58.3 months | Subtrochanteric (n=9) Femoral shaft (n=2) |
IMN: (n=2) PFNA: (n=9) |
- | Radiologic union time: (months) (9.9) (6-16) |
Delayed union (n=5) - Dynamization:1 Bone grafting:4 |
12 months |
| Greenspan, USA, 2018 |
Level I Randomized clinical trial |
13 | 74.2±2.5 ---- 13 (13) |
- | Alendronate (n=6) Risedronate (n=4) Ibandronate (n=3) |
NA | Femoral shaft - all | Plate/wire/screw Immediate GP: (n=3) Delayed GP: (n=1) IMN Immediate: (n=4) Delayed: (n=5) |
N=13 Immediate GP (20 μg subcutaneous daily for 12 months) vs Delayed GP (initiated 6 months later) |
Radiographic indices Composite score BMD Healing score Quality of life questionnaire Pain assessment Hospitalizations |
Implant failure Delayed GP: (n=1) |
Months Mean: 14.7 Delayed GP: 18 Immediate GP: 12 |
| Rocos, UK, 2018 |
Level III Retrospective cohort |
12 | 71 ---- 9 (10) |
Diabetes Mellitus, Rheumatoid Arthritis, Polymyalgia Rheumatica, Ankylosing Spondylitis, Colitis, gout, Ischemic heart disease |
Alendronate (n=10) Ibandronate (n=1) {One was using both} |
6 months to 8 years | NA | Nail Gamma 3: (n=11) Recon: (n=1) |
- | Prodromal pain Union time: (days) Medial: 144.7 Lateral: 199.8 Position of final reduction |
Nonunion (n=6) – revision Iatrogenic fracture (n=1) - revision |
2 years |
| Eisenstein, UK, 2017 |
Level III Retrospective cohort |
7 | 71.1 ---- 6 (7) |
NA | Alendronate (n=6) Pamidronate (n=1) |
NA | NA | IMN - all | - | Incidence of AFF | - | NA |
| Kayali, Turkey, 2017 |
Level IV Retrospective case series |
26 | 73 ----- 22 (22) |
NA | NA | 7.6 years | Femoral Shaft - all |
IMN Open GP: 21 Close GP: 5 |
- | Femur stress reaction BMD Union time: (months) (7.4) |
Nonunion (n=5) – revision: 3 |
NA |
| Lee, South Korea, 2017 |
Level III Retrospective cohort |
46 | 70.1 ---- 44 (44) |
High BMI | NA | 5.1 years | Subtrochanteric (n=15) Femoral shaft (n=31) |
IMN - all | N=14 | Radiographic union time: (weeks) (24.9) Body mass index |
Delayed union (n=15) Nonunion (n=2) – revision: 2 |
12 months |
| Philips, UK, 2017 |
Level III Retrospective cohort |
12 | 71.6 ---- 12 (12) |
polymyalgia rheumatica, hypothyroidism, nephritic syndrome | Alendronate (n=12) |
8.33 years | Subtrochanteric (n=12) |
Gamma nail -all | - | Radiologic union time: (weeks) (24) |
Broken nail (n=1) – revision Nonunion (n=2) – bone stimulation: 2 |
25.9 weeks for 11 cases |
| Yeh, Taiwan, 2017 |
Level III Retrospective cohort |
16 | 70.15±6.36 ---- 13 (13) |
hypertension, diabetes mellitus, breast cancer |
Alendronate (n=13) |
4.04 years | Subtrochanteric (n=10) Femoral haft (n=6) |
IMN: (n=8) Recon: (n=5) Gamma3 nail: (n=2) PFNA: (n=1) |
N=8 | Radiologic union time: (months) Teriparatide GP: 4.4 Non-Teriparatide GP: 6.2 months |
Nonunion and implant failure in non-teriparatide GP (n=1) – Revision: twice |
1 year |
| Teo, Singapore, 2014 |
Level III Retrospective cohort |
33 | 67.5 ---- 33 (33) |
- | Alendronic acid (n=33) |
4.9 years | Subtrochanteric (n=33) |
IMN; (n=6) PFNA: (n=4) DCS: (n=10) DHS: (n=8) Plate and screw: (n=5) |
N=10 | Rate of failure and revision Radiologic union time: (months) IM: (10) Extramedullary: (10.9) |
Implant failure (n=7) – revisions: 6 Nonunion (n=1) Delayed union (n=4) – Bone graft: 4 |
21.7 months for 30 patients |
| Egol, USA, 2013 |
Level III Retrospective cohort |
41 | 66.8 ---- 31 (33) |
NA | Alendronate (n=33) |
8.8 months | Subtrochanteric (n=25) Femoral shaft (n=16) |
IMN: (n=18) CMN (n=23) |
NA (“small number”) | Union time: (months) (8.3) |
Nonunion & implant failure: (n=1) - revision | 1 year |
| Prasarn, USA, 2012 |
Level III Retrospective cohort |
25 | 71 ---- 25 |
Diabetes Mellitus, Alcohol, Tobacco | NA | 7.6 years | Femoral Shaft - all |
CMN: (n=15) Plate: (n=10) |
N=16 | Radiologic union time: (weeks) (26) |
Iatrogenic fracture (n=5) Implant failure (Post-op) {Plate: (n=3) Nail: (n=1)} Nonunion (n=1) |
29 months At least 5 |
| Shkolnikova, Australia, 2012 |
Level III Retrospective cohort |
18 | 72.64 ---- 11 (14) |
Breast cancer, Hypothyroidism, Gastroesophageal reflux, Paget’s disease, heart failure, smoker, alcohol consumer | Alendronate (n=14) | 6 years | NA | IMN - all | - | Pre- and post-fracture level of function | Nonunion (n=1) - revision Delayed union (n=1) Fat embolism (n=1) |
NA |
| Banffy, USA, 2011 |
Level III Retrospective cohort |
39 | 68.5 ---- 33 (33) |
- | NA | 77 months | Femoral Shaft - all |
CMN (n=39) |
- | Length of hospital stay Nonunion Non-operative treatment outcomes |
Nonunion (n=1) - revision |
36.5 months At least 12 |
| Weil, Israel, 2011 |
Level IV Retrospective cohort |
17 | 73 ---- 14 (15) |
NA | NA | 7.8 years | Subtrochanteric (n=4) Femoral shaft (n=13) |
IMN: (n=12) CMN: (n=4) Plate: (n=1) |
N=3 | bone mineral density Complications |
Dynamization (n=4) Nail exchange (n=2) Plating: (n=1) |
1 year |
AFF: atypical femoral fracture, BP: bisphosphonate, NA: not available, GP: group, CMN: cephalomedullary nail, IM: intramedullary, IMN: intramedullary nail, PFNA: proximal femoral nail antirotation, DHS: dynamic hip screw, DCS: dynamic condylar screw
Overall, 1, 12, 1, and 1 of the studies were randomized clinical trial, retrospective cohort, case-control, and retrospective case series, respectively.
Past medical history, which may affect surgical outcomes, including underlying diseases, type, and duration of used bisphosphonates, was evaluated. Moreover, fracture locations, fixation types, and post-op medications were studied. Clinical outcomes that were investigated in these studies included union time, complications (i.e., non-union, delayed union, implant failure, and infection), and follow-up time.
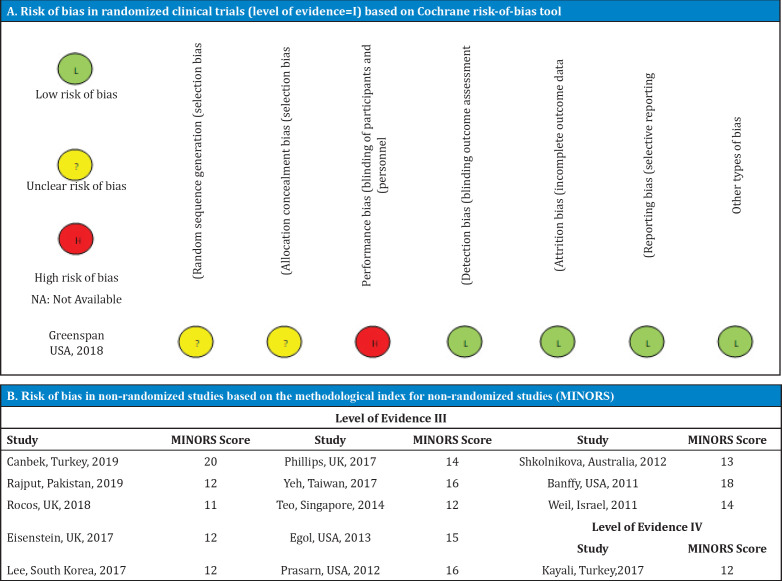
The overall quality of the studies was good. The randomized clinical trial was evaluated for the risk of bias by the Cochrane risk-of-bias tool. It had a high risk of performance bias and unclear bias of allocation concealment and random sequence generation. All non-randomized studies were evaluated using the MINORS score with an ICC of 0.823 (95% CI, 0.809-0.861). The lowest MINORS score was 11 for non-comparative studies. Table 2 summarizes the risk of bias ratings.
Table 2.
Risk of bias in included studies
Pre-operation evaluation
Demographic data and risk factors
In total, 316 patients (348 fractures) who met the criteria were included in the current systematic review. Majority of patients were female, while only 2.5% (n=8) of them were male. The mean age of all patients was 70.47 years, with a mean reported age range of 66.8-74.2 years in different studies.
It should be mentioned that seven studies had reported risk factors or underlying diseases as comorbidities of the patients. These risk factors included diabetes mellitus, rheumatoid arthritis, polymyalgia rheumatica, ankylosing spondylitis, colitis, gout, ischemic heart disease, hypothyroidism, chronic obstructive pulmonary disease, obstructive sleep apnea, nephritic syndrome, hypertension, osteoporosis, breast cancer, gastroesophageal reflux, Paget’s disease, history of corticosteroid and protein pump inhibitors usage, alcohol or tobacco consumption, and high body mass index (BMI) (8, 11, 17, 20, 23, 24, 26). In their study, Lee et al. found that the mean BMI was significantly higher in the delayed AFFs healing group of their study, compared to the normal group (8).
Bisphosphonates
Regarding the study design, all the patients had been under bisphosphonate medication previously. Moreover, 9 and 13 out of the 15 included studies reported the type of bisphosphonate and duration (mean or range) of therapy, respectively.
The type of bisphosphonates was not reported for 171 patients (54.1%) in the included studies.
Among the 145 patients whose bisphosphonates type was reported, 90.3% (n=131), 4.8% (n=7), 2.75% (n=4), 2.06% (n=3), and 0.6% (n=1) used alendronate, ibandronate, risedronate, zoledronic acid, and pamidronate, respectively. One patient was using both alendronate and ibandronate (10, 18-21, 23-26).
In the 12 studies that reported an exact mean duration of bisphosphonate therapy, the reported mean values were within the range of 4.04-8.8 years. The calculated mean of bisphosphonate therapy duration for these patients (n=285) was 5.59 years (8, 10, 11, 17, 18, 22-28).
No specific trial was performed on the effect of bisphosphonates type or duration of usage on the surgical outcomes. However, Prasarn et al. showed that a higher percentage of patients treated with bisphosphonates had confirmed osteoporosis pre-operatively, compared to those who were not treated with bisphosphonates (11).
Operative Management
In total, 12 out of the 15 included studies reported 311 fractures in 285 patients. Based on the acquired data, 65.27% (203 AFFs) and 34.72% (108 AFFs) of these fractures were in diaphyseal and subtrochanteric, respectively (8, 10, 11, 17-19, 22-25, 27, 28).
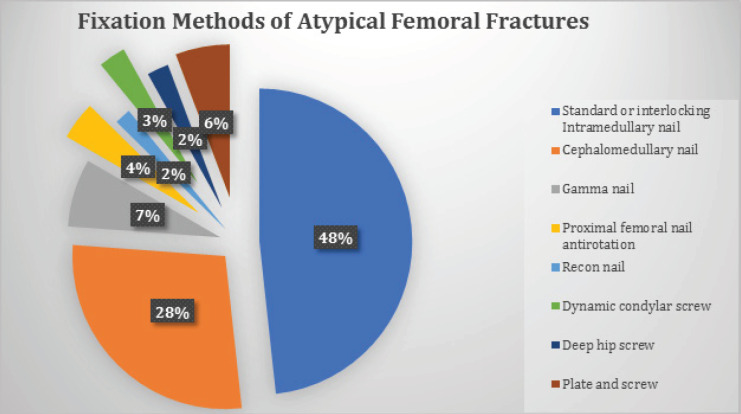
All the reviewed studies have reported the type of fixation. 89.08% of the 348 AFFs had an intramedullary fixation device, and 10.91% had an extramedullary. The details for each group are summarized in [Figure 2].
Figure 2.
Fixation methods frequency for atypical femoral fractures
Intramedullary fixation devices can be inserted with open surgery and drilling of the bone ends, or in a closed manner. Several studies have considered this difference in their patient cohorts (8, 17, 22, 28). Canbek et al. found out that there is no difference between closed and open surgery groups in terms of the union and complication rates. However, they realized that radiologic union time was shorter in the open-intervention group (17). Weil et al. performed 9 out of 17 fixations through an open intervention and took a biopsy in seven cases for ruling out the malignancy (28).
Rocos et al. considered the lateral side of AFFs a primary site of non-union to consider particular approaches for AFFs operation. They advocated undertaking a wedge excision to have a valgus morphology in the bone and stabilizing it with an intramedullary nail and a lateral tension plate (20). Egol et al. also found out that a varus mal-reduction at the site of fracture leads to delayed healing which is mostly returned to self-reported baseline function within a year post-operation (25).
Post-operative evaluation
Follow-up and outcomes
Patients had been followed up with a mean follow-up time of 20.8 months in the studies that have reported an exact mean follow-up time. It should be noted that for 23 patients (7.3%), the follow-up time has been insufficient or they were lost for follow-up.
The top reported outcome measurement in the reviewed study was the union time. Accordingly, 10 out of 15 studies reported the mean union time in their patient groups with a mean range of 4.4-10.9 months (8, 10, 11, 17, 18, 20, 22-25). The minimum was achieved in a group of patients with intramedullary management under teriparatide medication by Yeh et al., while the maximum was obtained in a group with extramedullary fixation by Teo et al. (10, 24).
Complications
Non-union, delayed union, and implant failure during the intervention or post-operative phase, were the most frequently reported complications. Bone Stimulation, bone grafting procedure, dynamization, and other revision surgeries were also performed in a couple of studies. Table 3 summarizes the frequency of these complications and their following performed procedures. There was also a report of post-operative fat embolism by Shkolnikova et al. (26). Among the 61 reported complications in 348 AFFs (complication rate: 17.52%), non-union was the most frequent, followed by implant failure. Half of the patients with these complications underwent significant surgical treatments, while one-third of them did not need any intervention or refused it.
Table 3.
Surgical treatment complications and required interventions in bisphosphonates-related atypical femoral fractures*These cases have both implant failure, and non-union
| Intervention | Complication | |||||
|---|---|---|---|---|---|---|
| Delayed union | Non-union | Implant failure | Not clear | Total | ||
| Intra-operation | Post-operation | |||||
| Bone stimulation | 2 | - | - | - | - | 2 |
| Bone graft | 8 | - | - | - | - | 8 |
| Major revision | 1 | 14 | 1 | 7 (+4*) | 7 | 30 |
| No intervention or unknown | 2 | 7 | 5 | 6 | - | 20 |
| Total | 13 | 21 | 6 | 13 (+4*) | 7 | 60 |
The most commonly reported revision methods were nailing, plating, and dynamization, and the primary reason for reported revisions was non-union with an intramedullary fixation device in most of the cases. Based on the existing reported cases, 6 out of 38 extramedullary fixation devices required a revision (15.7%), while only 20 out of 310 (6.45%) intramedullary cases needed a revision. Among the 29 revised cases, two needed to be revised twice. Table 4 summarizes the major revisions and their characteristics.
Table 4.
Major revisions
|
Study
(first author) |
Revision reason(s) | Primary fixation method | Revision Method | AFF Location | |
|---|---|---|---|---|---|
| 1 | Canbek | Non-union | IMN standard | Long femoral stem | Femoral shaft |
| 2 | Rajput | Delayed union | - | Dynamization | - |
| 3 | Rocos | Non-union and broken nail | Gamma Nail | Nail and lateral tension band plate | - |
| 4 | Rocos | Non-union and broken nail | Gamma Nail | Blade plate | - |
| 5 | Rocos | Non-union and broken nail | Gamma Nail | - | - |
| 6 | Rocos | Non-union | Gamma Nail | Blade plate | - |
| 7 | Rocos | Iatrogenic fracture | Gamma Nail | Plate | Femoral shaft |
| 8 | Kayali | Non-union | IMN Standard | IMN+autografting | Femoral shaft |
| 9 10 | Kayali | Non-union | IMN Standard | Hemiarthroplasty for femoral head fracture | Femoral shaft |
| 11 | Lee | Non-union | - | Plate | - |
| 12 | Lee | Non-union | - | - | - |
| 13 | Phillips | Broken nail | Gamma Nail | Further long gamma nail | Subtrochanteric |
| 15 | Yeh | Non-union and implant failure * | IMN | DCS+all bone grafting | Subtrochanteric |
| 15-20 | Teo | Implant failure | Extramedullary fixation | - | Subtrochanteric |
| 21 | Egol | Non-union | CMN | Blade plate+bone graft | - |
| 22 | Shkolnikova | Non-union | IMN | - | - |
| 23 | Banffy | Non-union | CMN | - | Femoral shaft |
| 24 | Weil | - | CMN | Blade plate | Subtrochanteric |
| 25 | Weil | - | IMN | Nail exchange | Femoral shaft |
| 26 | Weil | - | CMN | Nail exchange | Subtrochanteric |
| 27-29 | Weil | -* | IMN | Dynamization | Femoral shaft |
| 30 | Weil | - | CMN | Dynamization | Subtrochanteric |
AFF: atypical femoral fractures, IMN: intramedullary nail, DCS: dynamic condylar screw, CMN: cephalomedullary nail
* One of the cases was revised twice.
Teriparatide therapy and prophylactic nailing
Teriparatide was part of the post-operative treatment protocol of some AFF patients in seven studies. Teriparatide was given to a total of 64 patients in six studies, and in the study performed by Egol et al., only a small number of patients had used teriparatide post-operatively. Moreover, in four out of these seven studies, the effects of teriparatide on the patients were not evaluated. Greenspan et al. performed a randomized clinical trial on 13 patients and found no significant difference between the effects of the early and delayed start of teriparatide use on surgical outcomes. Lee et al. and Yeh et al. in their studies indicated that although the union or healing time is shorter in teriparatide groups of patients, it is not significant (8, 10, 11, 19, 24, 25, 28).
Prophylactic nailing has not been notably discussed in the reviewed studies. Eisenstein et al. reported that one of their patients had also received prophylactic nailing on the contralateral femur (21). Kayali et al. also reported one case with prophylactic intramedullary nailing (22). Banffy et al. had an experience of six prophylactic cephalomedullary nail fixation in one of their patient cohorts; however, due to their study limitations, they recommended the conduction of a prospective randomized trial study on prophylactic AFFs management (27).
Discussion
We used a comprehensive search strategy in four databases to retrieve studies about surgical treatment of bisphosphonate-related AFFs. Finally, the results of 15 retrieved articles with 316 patients were evaluated comprehensively and systematically. The retrieved studies were heterogeneous regarding the applied surgical approaches, study designs, populations, and level of evidence. Therefore, we collected and presented the details of each study in our systematic review.
What are the risk factors?
The findings revealed that almost all patients with bisphosphonate-related AFFs were elderly females. This finding is inconsistent with that of Shkolnikova et al. which indicated that AFFs occur in younger patients and that this might be due to more susceptibility of the younger patients to the anti-resorptive effects of bisphosphonates (26). The mean values of reported bisphosphonates therapy duration were within the range of 4.04-8.8 years in the reviewed studies.
Bisphosphonate therapy may have some notable adverse effects. Although there is no definite recommendation for the duration of bisphosphonate treatment, studies show that a 3 to 5-year course of treatment is acceptable. However, it must be noted that the risk factors of the patients should be taken into account. Metabolic diseases, rheumatologic diseases, medications, and social history risk factors have been mentioned as the risk factors for bisphosphonate therapy. Among all the risk factors, high BMI has been proven to play a significant role in delayed post-operative healing (8). Therefore, it can be concluded that a decrease in BMI may be helpful for patients under bisphosphonates treatment.
None of the reviewed studies was a trial about the effects of bisphosphonate type and duration usage on surgical outcomes. Nevertheless, it was indicated that bisphosphonates, as an effective therapy for the prevention of osteoporotic fractures, might play a role in inducing atypical femoral fractures in the long term, and surgical treatments are highly recommended in most cases in comparison with medical management (21, 27). The scoping review and comprehensive algorithm for AFFs management used by Toro et al. corroborate this recommendation (6).
Based on the results of this review, most of the fractures were in diaphyseal, and most of the revisions were required by these cases. However, considering the proportion of revisions, they had a better surgical outcome in comparison with subtrochanteric cases. This finding is in line with that of a study performed by Teo et al. which indicated that subtrochanteric fractures lead to considerable morbidity with a significant proportion of patients requiring revision surgery and experiencing implant failure (10). This may indicate that performing the surgery by an experienced senior surgeon would help to prevent failure of the fixation of subtrochanteric AFFs.
Despite the fact that intervention techniques in terms of open or closed reduction and fixation differed in some studies, there cannot be any direct recommendation on the superiority of any approach. Rocos et al. suggested a new strategy for the surgical approach, including valgising wedge osteotomy for correcting the evolved varus morphology and improving the final construct mechanics (20). The rate of failure and required revision of the aforementioned study was higher than that of the other reviewed studies. Since the other studies did not report this strategy, it may not be generally recommended.
Intramedullary nail fixation was the most common method in the reviewed studies. It may be due to its better load-sharing capacity and more rigid fixation with less bending movement at the fracture site (29). However, Weil et al. needed 46% revision surgery for their nailing patients which is considerably more than the overall rate of required revisions in other studies. Moreover, the required revisions of intramedullary fixations are less than half of those of extramedullary fixations in the reviewed studies overall. Lee et al. and Rajput et al. also indicated that the intramedullary fixation method is a reliable one with low complication rates (8, 18).
Egol et al. reported a mean radiological union time of eight months; however, as there is a wide range of reported union times with noticeable confounding factors, a reliable union time cannot be concluded based on this review (25).
Despite the fact that teriparatide had been considered to play a role in healing improvement of AFFs, it was mostly not prescribed or did not play a significant role in the studied cases that were treated surgically.
This also accords with an earlier systematic review about the effect of teriparatide on the healing of AFFs regardless of their management, in which it was declared that a better understanding of its effect might be elucidated with future prospective trials (7, 30). The role of prophylactic fixation before the development of complete AFF was mentioned in some reviewed studies; however, it is controversial and needs to be investigated more.
The aging population size is growing, and we are facing an increase in the elderly female population under longtime bisphosphonates treatment. The AFF is a challenging complication of bisphosphonates which should mostly be treated via a surgical procedure. Results of this study revealed that extra-medullary fixations and subtrochanteric fractures might have more complications post-operatively. However, no firm conclusions can be drawn due to the heterogeneity and level of evidence of the available data.
Future randomized clinical trials on surgical outcomes of different fracture locations and fixation methods, the advent of teriparatide prescription, and prophylactic fixations may help shed a better light on the surgical management of these fractures.
Limitations
The main limitation of the current systematic review was the low quality of available evidence on AFF. Most studies were retrospective case series or cohorts with incomplete data collection, which led to weak recommendation strength. Besides, the external validity of the results is questionable due to the low number of AFFs in most studies. Hence, a high-quality randomized clinical trial with a larger number of patients is needed to investigate multiple aspects of the AFF.
Funding:
Not applicable.
Conflicts of interest:
The authors declare that they have no conflict of interest.
Ethics approval:
Not applicable.
Authors’ Contributions:
All contributed to the study design/data analysis, drafting the manuscript/critical revision, and confirming the final manuscript.
References
- 1.Shane E, Burr D, Abrahamsen B, Adler RA, Brown TD, Cheung AM, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. Journal of bone and mineral research : the official journal of the American Society for Bone and Mineral Research. 2014;29(1):1–23. doi: 10.1002/jbmr.1998. [DOI] [PubMed] [Google Scholar]
- 2.Lenart BA, Neviaser AS, Lyman S, Chang CC, Edobor-Osula F, Steele B, et al. Association of low-energy femoral fractures with prolonged bisphosphonate use: a case control study. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2009;20(8):1353–62. doi: 10.1007/s00198-008-0805-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reyes C, Hitz M, Prieto-Alhambra D, Abrahamsen B. Risks and Benefits of Bisphosphonate Therapies. Journal of cellular biochemistry. 2016;117(1):20–8. doi: 10.1002/jcb.25266. [DOI] [PubMed] [Google Scholar]
- 4.Habib ZA. Bisphosphonates in the treatment of osteoporosis: a review of skeletal safety concerns. Expert review of endocrinology & metabolism. 2017;12(1):59–71. doi: 10.1080/17446651.2017.1256199. [DOI] [PubMed] [Google Scholar]
- 5.Dell RM, Adams AL, Greene DF, Funahashi TT, Silverman SL, Eisemon EO, et al. Incidence of atypical nontraumatic diaphyseal fractures of the femur. Journal of Bone and Mineral Research. 2012;27(12):2544–50. doi: 10.1002/jbmr.1719. [DOI] [PubMed] [Google Scholar]
- 6.Toro G, Ojeda-Thies C, Calabrò G, Toro G, Moretti A, Guerra GM-D, et al. Management of atypical femoral fracture: a scoping review and comprehensive algorithm. BMC musculoskeletal disorders. 2016;17(1) doi: 10.1186/s12891-016-1086-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Im G-I, Lee S-H. Effect of teriparatide on healing of atypical femoral fractures: a systemic review. Journal of bone metabolism. 2015;22(4):183–9. doi: 10.11005/jbm.2015.22.4.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee KJ, Yoo JJ, Oh KJ, Yoo JH, Rhyu KH, Nam KW, et al. Surgical outcome of intramedullary nailing in patients with complete atypical femoral fracture: A multicenter retrospective study. Injury. 2017;48(4):941–5. doi: 10.1016/j.injury.2017.02.036. [DOI] [PubMed] [Google Scholar]
- 9.Shane E, Burr D, Ebeling PR, Abrahamsen B, Adler RA, Brown TD, et al. Atypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the American Society for Bone and Mineral Research. Journal of Bone and Mineral Research. 2010;25(11):2267–94. doi: 10.1002/jbmr.253. [DOI] [PubMed] [Google Scholar]
- 10.Teo BJ, Koh JS, Goh SK, Png MA, Chua DT, Howe TS. Post-operative outcomes of atypical femoral subtrochanteric fracture in patients on bisphosphonate therapy. The bone & joint journal. 2014;96-b(5):658–64. doi: 10.1302/0301-620X.96B5.32887. [DOI] [PubMed] [Google Scholar]
- 11.Prasarn ML, Ahn J, Helfet DL, Lane JM, Lorich DG. Bisphosphonate-associated femur fractures have high complication rates with operative fixation. Clinical orthopaedics and related research. 2012;470(8):2295–301. doi: 10.1007/s11999-012-2412-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Şahin K, Ergin ÖN, Bayram S, Akgül T. Atypical femoral fractures related to bisphosphonate use: A comprehensive review of 19 patients. Ulusal travma ve acil cerrahi dergisi= Turkish journal of trauma & emergency surgery: TJTES. 2019;25(6):603–10. doi: 10.14744/tjtes.2019.46595. [DOI] [PubMed] [Google Scholar]
- 13.Koh A, Guerado E, Giannoudis P. Atypical femoral fractures related to bisphosphonate treatment: issues and controversies related to their surgical management. The bone & joint journal. 2017;99(3):295–302. doi: 10.1302/0301-620X.99B3.BJJ-2016-0276.R2. [DOI] [PubMed] [Google Scholar]
- 14.Schilcher J. High revision rate but good healing capacity of atypical femoral fractures A compa-rison with common shaft fractures. Injury. 2015;46(12):2468–73. doi: 10.1016/j.injury.2015.09.031. [DOI] [PubMed] [Google Scholar]
- 15.Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ (Clinical research ed) 2011:343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ journal of surgery. 2003;73(9):712–6. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 17.Canbek U, Akgun U, Aydogan NH. Efficacy of bone-end intervention on fracture healing in bisphosphonate-related atypical femoral fractures. Orthopaedics & Traumatology: Surgery & Research. 2020;106(1):77–83. doi: 10.1016/j.otsr.2019.07.028. [DOI] [PubMed] [Google Scholar]
- 18.Rajput IM, Kumar J, Siddiqui AA, Jamil M, Soughat M, Ahmed MW. Surgical Fixation of Atypical Femur Fractures in Bisphosphonate-treated Patients. Cureus. 2019;11(5):e4690. doi: 10.7759/cureus.4690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Greenspan SL, Vujevich K, Britton C, Herradura A, Gruen G, Tarkin I, et al. Teriparatide for treatment of patients with bisphosphonate-associated atypical fracture of the femur. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2018;29(2):501–6. doi: 10.1007/s00198-017-4286-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rocos B, Fleming T, Harding K, Acharya M, Riddick A, Kelly M. A Case Series and Discussion on Surgical Treatment Strategy for Atypical Proximal Femoral Fractures Associated with Bisphosphonate Use. Cureus. 2018;10(12):e3670. doi: 10.7759/cureus.3670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eisenstein N, Kasavkar G, Bhavsar D, Khan FS, Paskins Z. Incidence and medical management of bisphosphonate-associated atypical femoral fractures in a major trauma centre: a retrospective observational study. BMC musculoskeletal disorders. 2017;18(1):29. doi: 10.1186/s12891-017-1392-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kayali C, Altay T, Ozan F, Sozkesen S, Yamak K. Atypical femoral shaft fractures secondary to long-term bisphosphonate therapy. Journal of orthopaedics. 2017;14(2):226–30. doi: 10.1016/j.jor.2017.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Phillips HK, Harrison SJ, Akrawi H, Sidhom SA. Retrospective review of patients with atypical bisphosphonate related proximal femoral fractures. Injury. 2017;48(6):1159–64. doi: 10.1016/j.injury.2017.03.025. [DOI] [PubMed] [Google Scholar]
- 24.Yeh WL, Su CY, Chang CW, Chen CH, Fu TS, Chen LH, et al. Surgical outcome of atypical subtrochanteric and femoral fracture related to bisphosphonates use in osteoporotic patients with or without teriparatide treatment. BMC musculoskeletal disorders. 2017;18(1):527. doi: 10.1186/s12891-017-1878-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Egol KA, Park JH, Rosenberg ZS, Peck V, Tejwani NC. Healing delayed but generally reliable after bisphosphonate-associated complete femur fractures treated with IM nails. Clinical Orthopaedics and Related Research®. 2014;472(9):2728–34. doi: 10.1007/s11999-013-2963-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shkolnikova J, Flynn J, Choong P. Burden of bisphosphonate-associated femoral fractures. ANZ journal of surgery. 2013;83(3):175–81. doi: 10.1111/ans.12018. [DOI] [PubMed] [Google Scholar]
- 27.Banffy MB, Vrahas MS, Ready JE, Abraham JA. Nonoperative versus prophylactic treatment of bisphosphonate-associated femoral stress fractures. Clinical orthopaedics and related research. 2011;469(7):2028–34. doi: 10.1007/s11999-011-1828-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weil YA, Rivkin G, Safran O, Liebergall M, Foldes AJ. The outcome of surgically treated femur fractures associated with long-term bisphosphonate use. The Journal of trauma. 2011;71(1):186–90. doi: 10.1097/TA.0b013e31821957e3. [DOI] [PubMed] [Google Scholar]
- 29.Giannoudis PV, Ahmad MA, Mineo GV, Tosounidis TI, Calori GM, Kanakaris NK. Subtrochanteric fracture non-unions with implant failure managed with the “Diamond” concept. Injury. 2013;44 Suppl 1:S76–81. doi: 10.1016/S0020-1383(13)70017-2. [DOI] [PubMed] [Google Scholar]
- 30.Chiang CY, Zebaze RM, Ghasem-Zadeh A, Iuliano-Burns S, Hardidge A, Seeman E. Teriparatide improves bone quality and healing of atypical femoral fractures associated with bisphosphonate therapy. Bone. 2013;52(1):360–5. doi: 10.1016/j.bone.2012.10.006. [DOI] [PubMed] [Google Scholar]