Abstract
Background:
Pilon fractures represent one of the most surgically challenging fractures in orthopaedics. Different techniques exist for their management, with open reduction and internal fixation (ORIF) and External fixation (Ex-Fix) the most widely used. Whilst there is a plethora of data regarding these strategies for Pilon fractures as a whole, very limited data exists solely on the management of open Pilon fractures. This study aimed to elucidate how surgical management options can influence postoperative complications, and if this can influence future management protocols.
Methods:
We conducted a search in PubMed, EMBASE and CENTRAL for postoperative complications and functional outcomes in open pilon fractures in those treated with Ex-Fix vs ORIF (PROSPERO-CRD42020184213). The postoperative complications measured included non-union, mal-union, delayed union, bone grafting, amputation, osteoarthritis, deep infection and superficial infection. Functional outcomes in the form of the AOFAS score was also measured where possible. We were able to carry out a meta-analysis for both deep infections and non-unions.
Results:
The search yielded 309 results and a total of 18 studies consisting of 484 patients were included. All fractures included were open, and consisted of 64 Gustilo-Anderson Type I, 148 Type II, 103 Type IIIa, 90 Type IIIb and 9 Type IIIc. 60 Type III fractures could not be further separated and 12 were ungraded. Both ORIF and Ex-Fix were found to have statistically similar AOFAS scores (P=0.682). For all included studies, the Ex-Fix group had significantly higher rates of superficial infections (P=0.001), non-unions (P=0.001), osteoarthritis (P=0.001) and bone grafting (P=0.001). The meta-analysis found no significant difference in non-union (pooled OR=0.25, 95% CI: 0.03 to 2.24, P=0.44) or deep infection rates (pooled OR=1.35, 95% CI: 0.11 to 16.69, P=0.12) between the ORIF and Ex-fix groups.
Conclusion:
Based on our study, while Ex-Fix and ORIF have similar functional outcomes, Ex-Fix appears to have a significantly higher risk of postoperative complications which must be considered by surgeons when choosing surgical management options. Further research, ideally in a randomised control trial format, is required to definitively demonstrate ORIF superiority in the management of open pilon fractures.
Key Words: External fixation, Open pilon fracture, Open reduction internal fixation
Introduction
Pilon fractures or tibial plafond fractures, referring to intraarticular fractures of the distal tibia, represent one of the most surgically challenging fractures in orthopaedics. The combination of a high energy trauma mechanism, articular comminution and soft tissue damage make management of these fractures particularly difficult. The implosion of the tibial plafond due to axial compression results in significant soft tissue injury and can result in multiple displaced articular fragments (1). Pilon fractures are relatively uncommon, making up only 5-7% of tibial fractures seen; rarer still is the open pilon fracture (2). The objective of surgical intervention in these injuries is the restoration of articular congruency and epiphyseal-metaphyseal alignment which are often tenuous due to the high energy nature of the injury. The timing of surgical intervention varies depending on soft tissue condition, patient factors such as concomitant injuries and the surgeon’s preference. The use of early definitive management in open pilon fractures is complicated, as the incidence of wound dehiscence and deep tissue infection are elevated relative to closed fractures (3).
There is a complex balance to be struck between soft tissue protection via a limited approach, and sufficient exposure of the articular surface for precise restoration via more open techniques. The most commonly used method in treating pilon fractures is open reduction and internal fixation (ORIF), which involves substantial soft tissue dissection for visualisation of the articular surface (4). Other definitive techniques include the use of limited internal fixation in combination with an external fixator (LIFEF) which involves less soft tissue disruption, intramedullary nailing and minimally invasive plate osteosynthesis (5-7). There is a scarcity of studies regarding the outcome of open pilon fractures, with statistics often the result of open and closed fracture outcomes grouped together. The aim of this systematic review is to address this issue and summarise current literature specific to open pilon fractures regarding definitive surgical management and their accompanying functional outcomes and complication rates.
Materials and Methods
In conducting this review, the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guideline was used (8).
A protocol for this systematic review and meta-analysis was prospectively registered in the International Prospective register of systematic reviews (PROSPERO; 2020: CRD42020184213) (9).
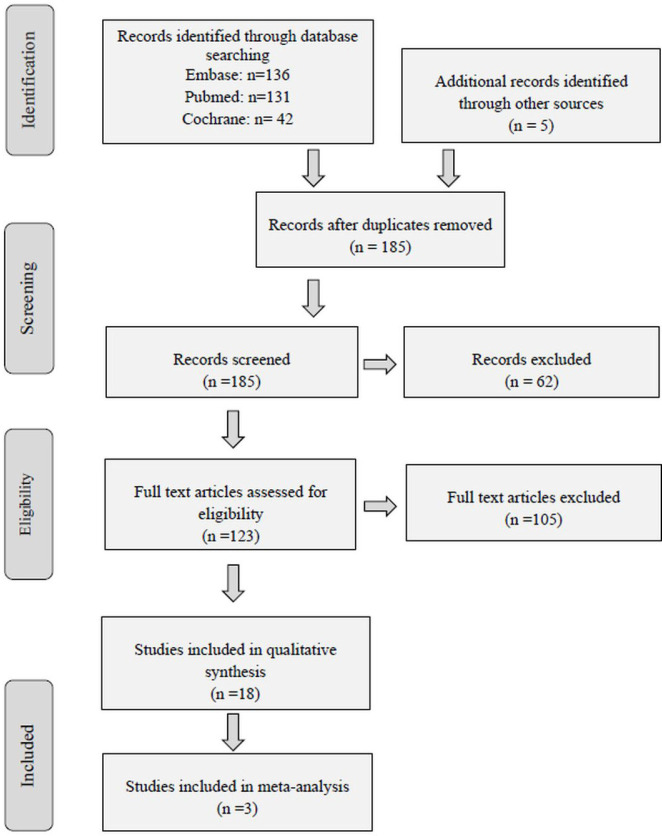
Three researchers identified relevant studies according to inclusion/exclusion criteria via a search of PubMed, EMBASE and Cochrane Central Register of Controlled Trials (CENTRAL) using the keyword search (pilon OR plafond) AND fracture AND open AND management which yielded 309 results. Abstract screening was conducted by all three researchers and exclusion criteria used in screening included case reports, and studies including less than our set minimum of 5 patients. After the screening process limiting studies to open pilon fractures with sufficient data on outcomes including complications and functional status post-surgery, 18 were found to be relevant and the rest were excluded from statistical analysis [Figure 1]. Full text screening exclusion criteria included case reports, papers incorporating both open and closed fractures into final analysis, and papers without data on complication outcomes. Two independent researchers were involved in the full text screening process.
Figure 1.
PRISM Flow diagram summarizing text selection process
Quality Assessment
Quality assessment of the included studies were performed using the GRADE criteria, whilst risk of bias assessments were performed using the RoB2 tool for RCTs and ROBINS-I tool for non-randomised controlled trials [Supplementary Table 1-3] (27) .The included studies included 1 randomised controlled trial (RCT), 1 cohort studies, 13 retrospective studies and 3 prospective studies.
Supplementary Table 1.
GRADE quality
| Author | Study Design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Large Effect | Plausible Confounding | Quality |
|---|---|---|---|---|---|---|---|---|---|
| Hu et al | Retrospecitve Case Series |
Low | Not serious | Not serious | Not serious | Serious | N/A | No | ⊕⊕⊕ ⊕ High |
| Encinas-Ullán et al | Prospective Case Control |
Low | Not serious | Not serious | Serious | Not serious | N/A | No | ⊕⊕⊕ Moderate |
| Choi et al | Retrospective Case Series |
Moderate | Not serious | Not serious | Not serious | Undetected | N/A | No | ⊕⊕⊕ Moderate |
| Boraiah et al | Retrospective Case Series |
Moderate | Not serious | Not serious | Not serious | Undetected | N/A | No | ⊕⊕⊕ Moderate |
| Sirkin et al | Retrospective Case Series |
Moderate | Not serious | Serious | Not serious | Not serious | N/A | No | ⊕⊕⊕ Moderate |
| Bone et al | Prospective Case Series |
Moderate | Serious | Not serious | Serious | Undetected | N/A | No | ⊕⊕ Low |
| Molina et al | Retrospective Case Series |
Moderate | Not serious | Serious | Not serious | Serious | N/A | No | ⊕⊕⊕ Moderate |
| White et al | Cohort | Moderate | Not serious | Not serious | Serious | Undetected | N/A | No | ⊕⊕⊕ Moderate |
| Gardner et al | Retrospective Case Series |
Moderate | Not Serious | Not Serious | Not Serious | Undetected | N/A | No | ⊕⊕⊕ Moderate |
| Gehr et al | Prospective Case Series |
Moderate | Serious | Not Serious | Not Serious | Serious | N/A | No | ⊕⊕ Low |
| Danoff et al | Retrospective Case Series |
Low | Not Serious | Serious | Not Serious | Serious | N/A | No | ⊕⊕⊕ Moderate |
| Silluzio et al | Retrospective Case Series |
Moderate | Not Serious | Not Serious | Serious | Undetected | N/A | No | ⊕⊕⊕ Moderate |
| Zeng et al | Retrospective Case Series |
Moderate | Not Serious | Not Serious | Serious | Not Serious | N/A | No | ⊕⊕⊕ Moderate |
| Conroy et al | Retrospective Case Series |
Moderate | Not Serious | Serious | Serious | Serious | N/A | No | ⊕⊕⊕ Moderate |
| Harris et al | Retrospective Case Series |
Moderate | Not Serious | Serious | Not Serious | Serious | N/A | No | ⊕⊕⊕ Moderate |
| Kapukaya et al | Retrospective Case Series |
Low | Not Serious | Not Serious | Serious | Undetected | N/A | No | ⊕⊕⊕ ⊕ High |
| Yildiz et al | Retrospective Case Series | Moderate | Not Serious | Not Serious | Not Serious | Undetected | N/A | No | ⊕⊕⊕ Moderate |
| Wyrsch et al | Randomised Controlled Trials |
High | Not Serious | Not Serious | Not Serious | Undetected | N/A | No | ⊕⊕⊕ Moderate |
“Very low”; the true effect is probably markedly different from the estimated effect, “Low”; the true effect might be markedly different from the estimated effect, “Moderate”; the authors believe that the true effect is probably close to the estimated effect, “High”; the authors have a lot of confidence that the true effect is similar to the estimated effect
Supplementary Table 3.
Assessing risk of bias: Randomised controlled trials
| Item | Wyrsch et al |
|---|---|
| Random sequence generation | High risk |
| Allocation concealment | High risk |
| Blinding of participants and personnel | High risk |
| Blinding of outcome assessment | High risk |
| Incomplete outcome data | Unclear |
| Selective reporting | Low risk |
| Other sources of bias * | High risk |
| Risk of bias | High |
* Other sources of bias: Important concerns about surgical randomization
The figures for these can be found in the supplementary data section.
Statistical Analysis
We performed the meta-analysis using Review Manager 5.4, using odds ratio (OR) as an effect measure, with a 95% confidence interval (CI). The analysis was performed using the random effect model. Heterogeneity was assessed using I2, where a value of >60% was considered significant.
Complication data and functional outcome scores were collected where possible from each study. Statistical analysis was performed using IBM SPSS Statistics. An independent t-test was carried out to compare AOFAS scores in patients who underwent ORIF compared to External Fixation as their definitive management, whilst a Pearson Chi-Square test was used to compare complication rates. Complications that we decided to include in our study were rate of deep infections, superficial infections, non-unions, delayed unions, malunions, amputations, osteoarthritis and bone grafting. In all cases, statistical significance was set at P<0.05.
Results
The patient demographics from the 18 included studies can be seen below in [Table 1]. A total of 484 open pilon fractures were included in our study for analysis. Open pilon fractures were more commonly found in males (72%) compared to females (28%) and the most common mechanism of injury was via a road traffic collision (48%). Open pilon fractures present quite frequently with associated fibula fractures (77%), while the most common grade of soft-tissue injury was Gustilo-Anderson Type II. Of the 18 studies, there were 10 studies that performed ORIF as a source of definitive management. There were 6 studies which performed both ORIF and Ex-fix while the remaining 2 studies performed only Ex-fix. These results can be seen in [Table 2].
Table 1.
Patient Demographics
| Demographic Variable | Total in Included Studies | Missing Data in Included Studies (n =) |
|---|---|---|
| Age | Mean 42.9 (n = 255) Range: 16-82 |
229 |
| Sex | Female (n = 67) Male (n = 174) |
243 |
| Mechanism of Injury | RTC (n =102) Fall from height (n = 79) Crush injuries (n =11) Gunshot (n = 19) Sports (n = 2) |
271 |
| Gustilo-Anderson Classification | Type I (n = 64) Type II (n = 148) Type IIIa (n = 103) Type IIIb (n = 90) Type IIIc (n = 9) Type III (n = 60) |
10 |
| Fibula Status | Intact (n = 24) Fractured (n = 80) |
380 |
RTC = Road Traffic Collision
Table 2.
Results from Studies
| Author | Article | Definitive Management | Open Fractures | AOFAS Score | Complications | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | Type I | Type II | Type IIIa | Type IIIb | Type IIIc | |||||
| Hu et al10 | Open reduction and internal fixation of Gustilo type-I and type-II open pilon fractures using a lateral approach | ORIF | 35 | 15 | 20 | 0 | 0 | 0 | 89.8 Range: 84-95 |
2 Superficial Infections |
| Encinas-Ullán et al11 | Medial versus lateral plating in distal tibial fractures: a prospective study of 40 fractures | ORIF | 8 | 3 | 4 | 1 | 0 | 0 | 85.75 Range: 69-97 |
1 Deep Infection 1 Non-union 2 Malunions |
| Choi et al12 | Result of Staged Operation in Ruedi-Allgower Type II and III open Tibia Pilon Fractures with Severe Comminution | ORIF | 14 | 3 | 8 | 3 | 0 | 0 | 68 | 1 Deep Infection 4 Superficial Infections 1 Non-union 3 Delayed Unions 1 Amputation 10 Osteoarthritis |
| Boraiah et al13 | Outcomes following open reduction and internal fixation of open pilon fractures | ORIF | 59 | 2 | 3 | 37 | 17 | 0 | n/a | 2 Deep Infections 3 Superficial Infections 5 Delayed Unions 1 Amputation 6 Bone Grafting |
| Sirkin et al14 | A staged protocol for soft tissue management in the treatment of complex pilon fractures | ORIF | 22 | 3 | 6 | 7 | 6 | 0 | n/a | 2 Deep Infections 1 Amputation |
| Bone et al15 | External fixation of severely comminuted and open tibial pilon fractures | ORIF | 10 | 1 | 2 | 3 | 4 | 0 | n/a | None |
| Molina et al16 | Risk factors of deep infection in operatively treated pilon fractures (AO/OTA: 43) | ORIF | 142 | 25 | 64 | 53 | 0 | 0 | n/a | 33 Deep Infections |
| White et al3 | The Results of Early Primary Open Reduction and Internal Fixation for Treatment of OTA 43.C-Type Tibial Pilon Fractures: A Cohort Study | ORIF | 21 | 5 | 7 | 6 | 3 | 0 | n/a | 4 Deep Infections 3 Delayed Unions |
| Gardner et al17 | Treatment Protocol for Open AO/OTA Type C3 Pilon Fractures With Segmental Bone Loss | ORIF | 10 | - | - | - | - | - | n/a | 1 Deep Infection 1 Amputation |
| Gehr et al18 | Minimally invasive management of distal metaphyseal tibial fractures and pilon fractures: Technique and early results with the IP-XS nail | ORIF | 5 | - | - | - | 3 | - | n/a | None |
| Danoff et al19 | Outcome of 28 open pilon fractures with injury severity-based fixation | ORIF | 18 | 0 | 0 | 18 | 0 | 0 | ORIF: 71 Ex-Fix: 75 |
ORIF: 3 Deep Infections 1 Non-union Ex-Fix: 1 Deep Infection 1 Non-union |
| Ex-Fix | 10 | 0 | 0 | 0 | 10 | 0 | ||||
| Siluzio et al20 | Clinical and radiographic outcomes in patients operated for complex open tibial pilon fractures | ORIF | 10 | 0 | 0 | 3 | 7 | 0 | 71.5 Range: 40-95 |
4 Deep Infections 6 Superficial Infections 6 Delayed Unions 5 Osteoarthritis 1 Bone Graft |
| Ex-Fix | 4 | 0 | 0 | 0 | 0 | 4 | ||||
| Zeng et al21 | Surgical treatment of open pilon fractures | ORIF | 7 | 4 | 0 | 2 | 1 | 0 | 85.2 Range: 66-98 |
1 Deep Infection 2 Superficial Infections 2 Delayed Unions 10 Osteoarthritis 5 Bone Grafts |
| Ex-Fix | 21 | 0 | 21 | 0 | 0 | 0 | ||||
| Conroy et al22 | Early internal fixation and soft tissue cover of severe open tibial pilon fractures | ORIF | 28 | 0 | 0 | 0 | 28 | 0 | n/a | 2 Deep Infections 4 Superficial Infections 3 Malunions 2 Amputations 6 Osteoarthritis 7 Bone Grafts |
| Ex-Fix | 4 | 0 | 0 | 0 | 4 | 0 | ||||
| Harris et al23 | Results and outcomes after operative treatment of high-energy tibial plafond fractures | ORIF | 16 | 1 | 3 | 9 | 0 | 3 | n/a | ORIF: None Ex-Fix: 1 Deep Infection 1 Non-union |
| Ex-Fix | 5 | 0 | 0 | 0 | 5 | 0 | ||||
| Kapukaya et al24 | Non-reducible, open tibial plafond fractures treated with a circular external fixator (is the current classification sufficient for identifying fractures in this area?) | Ex-Fix | 12 | 0 | 5 | 5 | 0 | 2 | 58 Range: 28-90 |
1 Deep Infection 5 Superficial Infections 2 Non-union 2 Delayed Union 1 Malunion 10 Osteoarthritis |
| Yildiz et al25 | High-velocity gunshot wounds of the tibial plafond managed with Ilizarov external fixation: a report of 13 cases | Ex-Fix | 13 | 0 | 0 | 11 | 2 | 0 | n/a | 6 Superficial Infections |
| Wyrsch et al26 | Operative treatment of fractures of the tibial plafond. A randomized, prospective study | ORIF | 3 | - | - | - | - | - | n/a | ORIF: 2 Deep Infections 1 Superficial Infection 3 Osteoarthritis 2 Bone Grafts Ex-Fix: 1 Deep Infection 7 Osteoarthritis 6 Bone Grafts |
| Ex-Fix | 7 | 2 | 4 | 4 | - | - | ||||
On analysing the overall complications among the 484 open fractures, deep infection (12.4%) was found to be the most common out of the 8 different complications. For the 355 open fractures treated with ORIF, the most common complication was deep infection (13.8%), whilst the most common complication among the 57 Ex-fix treated patients was osteoarthritis (29.8%). When comparing complication rates between the ORIF group and the Ex-Fix group, a Pearson Chi-Square test was performed. Among all the complications that we looked at, the rate of superficial infection, osteoarthritis, non-union and bone grafting was significantly higher (P=0.001) in the Ex-Fix group. A summary of the overall complication with their significance can be seen in [Table 3].
Table 3.
Overall Complications
| Total (n = 484) | ORIF(n=355) | Ex-Fix (n=57) | p | Unclassified | |
|---|---|---|---|---|---|
| Superficial Infection | 33 (6.8%) | 10 (2.8%) | 11 (19.3%) | 0.001 | 12 |
| Deep Infection | 60 (12.4%) | 49 (13.8%) | 4 (7%) | 0.117 | 7 |
| Osteoarthritis | 51 (10.5%) | 13 (3.7%) | 17 (29.8%) | 0.001 | 21 |
| Non-union | 7 (1.4%) | 3 (0.85%) | 4 (7%) | 0.001 | 0 |
| Mal-union | 6 (1.2%) | 2 (0.56%) | 1 (1.8%) | 0.326 | 3 |
| Delayed union | 21 (4.3%) | 11 (3.1%) | 2 (3.5%) | 0.869 | 8 |
| Bone Grafting | 27 (5.6%) | 8 (2.3%) | 6 (10.5%) | 0.001 | 13 |
| Amputation | 6 (1.2%) | 4 (1.1%) | 0 | 0.421 | 2 |
On comparing functional outcomes via AOFAS scores between the 2 groups, an independent t test was performed. No significant difference was found between patients treated with either approach and this can be seen in [Table 4].
Table 4.
Comparison of functional outcomes
| ORIF (n = 69) | Ex-Fix (n = 20) | p | |
|---|---|---|---|
| AOFAS Score | 81.6 | 64.8 | 0.682 |
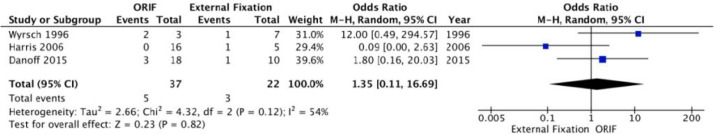
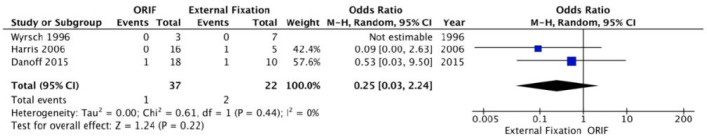
We were able to carry out a meta-analysis for both deep infections and non-unions [Figures 2; 3]. For deep infection, 3 studies with 59 fractures were included. The rate of deep infection was 5 of 37 in the ORIF groups and 3 of 22 in the External Fixation group, respectively. The meta-analysis showed no significant difference in deep infection between 2 groups, the pooled OR was 1.35 (95%CI: 0.11 to 16.69, P=0.12) and the heterogeneity among the studies were substantial (I2 = 54%). For non-unions, 3 studies with 59 fractures reported the results of non-union. The rate of non-union was 1 of 37 in the ORIF group and 2 of 22 in the External Fixation group. The meta-analysis showed no significant difference in non-unions between 2 groups, the pooled OR was 0.25 (95% CI: 0.03 to 2.24, P=0.44) and the heterogeneity among the studies was not significant (I2 = 0%).
Figure 2.
Outcome of deep infection rate in ORIF vs Ex-Fix
Figure 3.
Outcome of non-union in ORIF vs Ex-Fix
Discussion
Historically, pilon fractures were considered unfit for reconstruction with non-operative methods having dire outcomes. However, in 1969 with the innovative use of ORIF by Rüedi and Allgöwer, the use of operative methods for this fracture type has gradually evolved (28). ORIF incorporates four key principles: fibular length restoration, articular surface reconstruction, bone grafting as a means to fill the metaphyseal void and internal plate fixation with generally positive outcomes (29). With the subsequent focus shifting onto soft tissue vulnerability and its preservation, external fixation became a popular method of choice (28). External fixation can either be used temporarily in the staging of tibial pilon fractures, or as the definitive fixation method (30). A delayed approach to fixation is generally used to enable soft tissue recovery to an extent that makes it more amenable to definitive intervention (31).
Careful consideration when choosing an appropriate approach is essential as the high energy nature of pilon fractures and the inevitable soft tissue damage that results makes postoperative infection rates higher. This has prompted less invasive methods of operative management to be innovated (32). The aim of minimising postoperative infection is thus a high priority when deciding on definitive management, and the staging of such surgical procedures. External fixation is deemed to increase soft tissue preservation and theoretically reduce deep infection risk, but at the cost of reduced articular exposure. ORIF on the other hand, whilst getting adequate exposure, results in a greater degree of soft tissue dissection and a deeper conduit in which pathogens can accumulate. It is often thus down to the surgeon’s preference, patient characteristics and the axial CT images at plafond level that decide which method to use (33). Soft tissue swelling evaluation is essential when planning the timing of definitive management, as early internal fixation in severe cases of tissue oedema are associated with poorer infection outcomes (34).
In this study we found that both ORIF and Ex-Fix had statistically similar AOFAS outcomes, but significant differences in the propensity to develop certain infections postoperatively. The Ex-Fix group had an overall greater number of complications associated with it; osteoarthritis, bone grafting, superficial infection and non-union were more prevalent in the Ex-Fix cohort [Table 3]. Whilst the more invasive nature of ORIF and the substantial soft tissue dissection involved in the procedure would be expected to increase deep infection rate, our meta-analysis found no significant difference in deep infection incidence between the two groups with a pooled OR of 1.35 [Figure 2]. It is however important to note that the lack of available socioeconomic and comorbidity data on individual patients makes it impossible to discount other factors such as diabetes which could arguably impact infection outcomes. Additionally, a limitation of our infection data is that our study was not able to separate the ORIF or Ex-Fix procedures by specific approach or staging regimen used, which can influence infection outcomes. The significant heterogeneity between the studies included for deep infection meta-analysis (I2=54%) merits further research into whether this is a true difference.
Whilst deep infection rates were not significantly different between groups, the rate of superficial infections were significantly lower in the ORIF group (19.3% vs 2.8%), which can be explained by the commonly encountered pin site infection. Osteoarthritis was an encountered complication in 29.8% of those patients treated with external fixation, and remains a significant and poorly understood source of morbidity in patients with intra-articular fractures (35). Such progressive articular surface degeneration is an important factor, as it was the second most commonly encountered complication in the patients included and is associated with a later need for realignment surgery or joint replacement [Table 3] (36). It is however important to note that fractures with severe comminution tend to be selected for Ex-Fix, which would impact the osteoarthritis data. In the randomised prospective study included, there was no significant difference in osteoarthritis outcomes between the ORIF and Ex-Fix group which indicates that further research in a randomised format is required before the increased propensity to develop osteoarthritis after Ex-Fix can be considered a true effect.
Open Pilon fractures are associated with a higher rate of nonunion relative to their closed counterparts (37). This was worsened in the Ex-Fix group, which had a significantly higher rate of nonunion relative to the ORIF group (7% vs 0.85%). However our meta-analysis which consisted of three of the included studies did not find a significant difference in non-union outcomes between the two procedures, the pooled OR was 0.25 [Figure 3]. Heterogeneity was not significant, and our non-union findings are concordant with another meta-analysis of pilon fractures which found the difference in non-union between limited internal fixation combined with an external fixator (LIFEF) and ORIF not significant (5). The rate of bone grafting was also higher in the Ex-Fix group, indications for which include delayed unions, malunions and nonunions (38).
Whilst the data suggests that ORIF is superior to Ex-Fix in regards to reducing the risk of postoperative complications, it is important to consider the various limitations of our studies [Table 3]. Firstly, most of the studies included were retrospective case series which are naturally more prone to bias. The risk of bias was assessed using the RoB2 tool for RCTs and ROBINS-I tool for non-randomised controlled trials (27). Whilst many of the included studies had a moderate risk of bias, as is expected for retrospective studies, none were found to have a high risk of bias. The GRADE quality of included studies was moderate in the majority of cases, however two were considered low grade but were not included in the meta-analysis.
Additionally, it is important to consider that the sample size of the Ex-Fix group was significantly smaller and we were unable to adequately separate complications by the specific surgical approaches making up the ORIF and Ex-Fix groups, or the Gustilo grade involved. Other factors such as age and health of the patient could also influence complication outcome irrespective of surgical management used, as demographic and socioeconomic status has been shown to influence outcomes of high-energy pilon fractures (39).
Whilst there are no absolute guidelines as to which definitive surgical approach to use, the foundation of optimal management is nonetheless conserved. Fibular fixation to restore length, articular surface reconstruction, bone grafting and meta-diaphyseal reconstruction are the pillars to successful pilon fracture outcomes (40). Based on our study, while Ex-Fix and ORIF have similar functional outcomes, Ex-Fix appears to have a significantly higher risk of postoperative complications. Given the greater theoretical risk of deep infection with ORIF, the various confounding factors in our studies and the limited number of studies used in the meta-analysis, a firm conclusion of superior technique cannot be made. Further research, ideally in a randomised control trial format, is required to definitively demonstrate ORIF superiority in the management of open pilon fractures.
Supplementary Table 2.
Risk of Bias using ROBINS-I tool
| Study | Confounding | Selection | Intervention Measurement | Missing Data | Outcome Measurement | Reported Results | Overall |
|---|---|---|---|---|---|---|---|
| Hu et al | Low | Low | Moderate | Low | Low | Low | Low |
| Encinas-Ullán et al | Moderate | Low | Moderate | Low | Low | Low | Low |
| Choi et al | Moderate | Moderate | Moderate | Low | Low | Low | Moderate |
| Boraiah et al | Moderate | Moderate | Moderate | Moderate | Low | Low | Moderate |
| Sirkin et al | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate |
| Bone et al | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate |
| Molina et al | Moderate | Low | Moderate | Moderate | Moderate | Moderate | Moderate |
| White et al | Moderate | Moderate | Moderate | Moderate | Low | Moderate | Moderate |
| Gardner et al | Moderate | Moderate | Moderate | Low | Moderate | Low | Moderate |
| Gehr et al | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate |
| Danoff et al | Low | Moderate | Moderate | Low | Low | Low | Low |
| Silluzio et al | Moderate | Moderate | Moderate | Moderate | Moderate | Low | Moderate |
| Zeng et al | Moderate | Moderate | Moderate | Low | Moderate | Low | Moderate |
| Conroy et al | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate |
| Harris et al | Moderate | Moderate | Moderate | Moderate | Low | Moderate | Moderate |
| Kapukaya et al | Moderate | Moderate | Low | Low | Moderate | Low | Low |
| Yildiz et al | Moderate | Moderate | Moderate | Low | Moderate | Low | Moderate |
Note: Moderate = the study is sound for a non-randomised study with regard to this domain but cannot be considered comparable to a well-performed randomised trial; Low = The study is comparable to a well-performed randomised trial with regard to this domain
Availability of data and materials:
The data sets supporting the conclusions of the article are included within the article
Declaration of conflicting interests:
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. No benefits in any form have been, or will be, received from a commercial party related directly or indirectly to the subject of this manuscript
Funding:
No funding was necessary.
References
- 1.Tomás-Hernández J. High-energy pilon fractures management: State of the art. EFORT open reviews. 2016;1(10):354–61. doi: 10.1302/2058-5241.1.000016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mauffrey C, Vasario G, Battiston B, Lewis C, Beazley J, Seligson D. Tibial pilon fractures: A review of incidence, diagnosis, treatment, and complications. Acta Orthopaedica Belgica. 2011;77(4):432. [PubMed] [Google Scholar]
- 3.White TO, Guy P, Cooke CJ, Kennedy SA, Droll KP, Blachut PA, et al. The results of early primary open reduction and internal fixation for treatment of OTA 43 C-type tibial pilon fractures: a cohort study. Journal of orthopaedic trauma. 2010;24(12):757–63. doi: 10.1097/BOT.0b013e3181d04bc0. [DOI] [PubMed] [Google Scholar]
- 4.Grose A, Gardner MJ, Hettrich C, Fishman F, Lorich DG, Asprinio DE, et al. Open reduction and internal fixation of tibial pilon fractures using a lateral approach. Journal of orthopaedic trauma. 2007;21(8):530–7. doi: 10.1097/BOT.0b013e318145a227. [DOI] [PubMed] [Google Scholar]
- 5.Wang D, Xiang JP, Chen XH, Zhu QT. A meta-analysis for postoperative complications in tibial plafond fracture: open reduction and internal fixation versus limited internal fixation combined with external fixator. The Journal of Foot and Ankle Surgery. 2015;54(4):646–51. doi: 10.1053/j.jfas.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 6.Marcus MS, Yoon RS, Langford J, Kubiak EN, Morris AJ, Koval KJ, et al. Is there a role for intramedullary nails in the treatment of simple pilon fractures? Rationale and preliminary results. Injury. 2013;44(8):1107–11. doi: 10.1016/j.injury.2013.02.014. [DOI] [PubMed] [Google Scholar]
- 7.Vidović D, Matejčić A, Ivica M, Jurišić D, Elabjer E, Bakota B. Minimally-invasive plate osteosynthesis in distal tibial fractures: results and complications. Injury. 2015;46:S96–9. doi: 10.1016/j.injury.2015.10.067. [DOI] [PubMed] [Google Scholar]
- 8.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Journal of clinical epidemiology. 2009;62(10):e1–34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 9.Natasha Daniels, Jiang An Lim, Azeem Thahir. Open pilon fracture postoperative outcomes with different definitive surgical management options: a systematic review and meta-analysis. PROSPERO 2020 CRD42020184213. Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020184213. [DOI] [PMC free article] [PubMed]
- 10.Hu C, Zhu W, Chahal K, Zhu N, Fang W, Jing J, et al. Open reduction and internal fixation of Gustilo type-I and type-II open pilon fractures using a lateral approach. Journal of Orthopaedic Surgery. 2019;27(3):2309499019864722. doi: 10.1177/2309499019864722. [DOI] [PubMed] [Google Scholar]
- 11.Encinas-Ullán CA, Fernandez-Fernandez R, Rubio-Suárez JC, Gil-Garay E. Medial versus lateral plating in distal tibial fractures: a prospective study of 40 fractures. Revista Española de Cirugía Ortopédica y Traumatología (English Edition) 2013;57(2):117–22. doi: 10.1016/j.recot.2012.11.004. [DOI] [PubMed] [Google Scholar]
- 12.Choi KY, Lee JY, Jang H, Kim YW. Result of Staged Operation in Ruedi-Allgower Type II and III Open Tibia Pilon Fractures with Severe Comminution. Journal of Korean Foot and Ankle Society. 2019;23(3):110–5. [Google Scholar]
- 13.Boraiah S, Kemp TJ, Erwteman A, Lucas PA, Asprinio DE. Outcome following open reduction and internal fixation of open pilon fractures. JBJS. 2010;92(2):346–52. doi: 10.2106/JBJS.H.01678. [DOI] [PubMed] [Google Scholar]
- 14.Sirkin M, Sanders R, DiPasquale T, Herscovici Jr D. A staged protocol for soft tissue management in the treatment of complex pilon fractures. Journal of orthopaedic trauma. 1999;13(2):78–84. doi: 10.1097/00005131-199902000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Bone LA, Stegemann PH, McNamara KE, Seibel RO. External fixation of severely comminuted and open tibial pilon fractures. Clinical orthopaedics and related research. 1993(292):101–7. [PubMed] [Google Scholar]
- 16.Molina CS, Stinner DJ, Fras AR, Evans JM. Risk factors of deep infection in operatively treated pilon fractures (AO/OTA: 43) Journal of Orthopaedics. 2015;12(Suppl 1):S7–13. doi: 10.1016/j.jor.2015.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gardner MJ, Mehta S, Barei DP, Nork SE. Treatment protocol for open AO/OTA type C3 pilon fractures with segmental bone loss. Journal of orthopaedic trauma. 2008;22(7):451–7. doi: 10.1097/BOT.0b013e318176b8d9. [DOI] [PubMed] [Google Scholar]
- 18.Gehr J, Hilsenbeck F, Arnold T, Friedl W. Minimally invasive management of distal metaphyseal tibial fractures and pilon fractures. European Journal of Trauma. 2004;30(6):378–86. [Google Scholar]
- 19.Danoff JR, Saifi C, Goodspeed DC, Reid JS. Outcome of 28 open pilon fractures with injury severity-based fixation. European Journal of Orthopaedic Surgery & Traumatology. 2015;25(3):569–75. doi: 10.1007/s00590-014-1552-7. [DOI] [PubMed] [Google Scholar]
- 20.Silluzio N, De Santis V, Marzetti E, Piccioli A, Rosa MA, Maccauro G. Clinical and radiographic outcomes in patients operated for complex open tibial pilon fractures. Injury. 2019;50:S24–8. doi: 10.1016/j.injury.2019.01.041. [DOI] [PubMed] [Google Scholar]
- 21.Zeng XT, Pang GG, Ma BT, Mei XL, Sun X, Wang J, et al. Surgical treatment of open pilon fractures. Orthopaedic surgery. 2011;3(1):45–51. doi: 10.1111/j.1757-7861.2010.00113.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Conroy J, Agarwal M, Giannoudis PV, Matthews SJ. Early internal fixation and soft tissue cover of severe open tibial pilon fractures. International orthopaedics. 2003;27(6):343–7. doi: 10.1007/s00264-003-0486-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harris AM, Patterson BM, Sontich JK, Vallier HA. Results and outcomes after operative treatment of high-energy tibial plafond fractures. Foot & ankle international. 2006;27(4):256–65. doi: 10.1177/107110070602700406. [DOI] [PubMed] [Google Scholar]
- 24.Kapukaya A, Subasi M, Arslan H, Tuzuner T. Non-reducible, open tibial plafond fractures treated with a circular external fixator (is the current classification sufficient for identifying fractures in this area?) Injury. 2005;36(12):1480–7. doi: 10.1016/j.injury.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 25.Yildiz C, Atesalp AS, Demiralp B, Gür E. High-velocity gunshot wounds of the tibial plafond managed with Ilizarov external fixation: a report of 13 cases. Journal of orthopaedic trauma. 2003;17(6):421–9. doi: 10.1097/00005131-200307000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Wyrsch B, McFerran MA, McAndrew M, Limbird TJ, Harper MC, Johnson KD, et al. Operative treatment of fractures of the tibial plafond A randomized, prospective study. JBJS. 1996;78(11):1646–57. doi: 10.2106/00004623-199611000-00003. [DOI] [PubMed] [Google Scholar]
- 27.Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. bmj. 2019:366. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 28.Rüedi TP, Allgöwer M. Fractures of the lower end of the tibia into the ankle-joint. Injury. 1969;1(2):92–9. [Google Scholar]
- 29.Zelle BA, Dang KH, Ornell SS. High-energy tibial pilon fractures: an instructional review. International orthopaedics. 2019:1. doi: 10.1007/s00264-019-04344-8. [DOI] [PubMed] [Google Scholar]
- 30.Bear J, Rollick N, Helfet D. Evolution in management of tibial pilon fractures. Current reviews in musculoskeletal medicine. 2018;11(4):537–45. doi: 10.1007/s12178-018-9519-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shah KN, Johnson JP, O’Donnell SW, Gil JA, Born CT, Hayda RA. External Fixation in the Emergency Department for Pilon and Unstable Ankle Fractures. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2019;27(12):e577–84. doi: 10.5435/JAAOS-D-18-00080. [DOI] [PubMed] [Google Scholar]
- 32.Kottmeier SA, Madison RD, Divaris N. Pilon fracture: preventing complications. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2018;26(18):640–51. doi: 10.5435/JAAOS-D-17-00160. [DOI] [PubMed] [Google Scholar]
- 33.Jacob N, Amin A, Giotakis N, Narayan B, Nayagam S, Trompeter AJ. Management of high-energy tibial pilon fractures. Strategies in trauma and limb reconstruction. 2015;10(3):137–47. doi: 10.1007/s11751-015-0231-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Saad BN, Yingling JM, Liporace FA, Yoon RS. Pilon Fractures: Challenges and Solutions. Orthopedic Research and Reviews. 2019;11:149. doi: 10.2147/ORR.S170956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Anderson DD, Marsh JL, Brown TD. The pathomechanical etiology of post-traumatic osteoarthritis following intraarticular fractures. The Iowa orthopaedic journal. 2011;31:1. [PMC free article] [PubMed] [Google Scholar]
- 36.Ewalefo SO, Dombrowski M, Hirase T, Rocha JL, Weaver M, Kline A, et al. Management of posttraumatic ankle arthritis: literature review. Current reviews in musculoskeletal medicine. 2018;11(4):546–57. doi: 10.1007/s12178-018-9525-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rubio-Suarez JC, Carbonell-Escobar R, Rodriguez-Merchan EC, Ibarzabal-Gil A, Gil-Garay E. Fractures of the tibial pilon treated by open reduction and internal fixation (locking compression plate-less invasive stabilising system): Complications and sequelae. Injury. 2018;49:S60–4. doi: 10.1016/j.injury.2018.06.043. [DOI] [PubMed] [Google Scholar]
- 38.Finkemeier CG. Bone-grafting and bone-graft substitutes. JBJS. 2002;84(3):454–64. doi: 10.2106/00004623-200203000-00020. [DOI] [PubMed] [Google Scholar]
- 39.Cutillas-Ybarra MB, Lizaur-Utrilla A, Lopez-Prats FA. Prognostic factors of health-related quality of life in patients after tibial plafond fracture A pilot study. Injury. 2015;46(11):2253–7. doi: 10.1016/j.injury.2015.06.025. [DOI] [PubMed] [Google Scholar]
- 40.Liporace FA, Yoon RS. Decisions and staging leading to definitive open management of pilon fractures: where have we come from and where are we now? Journal of orthopaedic trauma. 2012;26(8):488–98. doi: 10.1097/BOT.0b013e31822fbdbe. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data sets supporting the conclusions of the article are included within the article