Abstract
BACKGROUND
An effective and efficient protocol for delirium identification is needed to improve health outcomes for older adults and reduce health care costs. This study describes the barriers and facilitators related to the implementation of the Ultra-brief Confusion Assessment Method (UB-CAM), a rapid two-step delirium identification protocol (ultra-brief screen, followed by CAM in positives), field tested with hospitalized older adults (70+).
METHODS
Field researchers at two sites (an urban academic medical center and a community teaching hospital) collected observational data from 322 clinical staff (50 physician hospitalists, 189 registered nurses, and 83 nursing assistants [NAs]) as they administered the UB-CAM. Thematic analysis of 767 direct observations of structural, organizational, patient, clinician, and innovations of the protocol was conducted. Field notes and open-ended interviews (n=231) with clinicians, explored the utility, acceptability, and feasibility of the protocol, and supplemented the observations.
RESULTS
The UB-CAM was generally positively received by all three clinician types. Six themes describe barriers and/or facilitators to implementing the UB-CAM: 1) physical setting and milieu; 2) practice environment; 3) integrating into role; 4) adaptive techniques; 5) patient responses; and 6) systematic assessment. The composition and interaction of the six themes determined if the theme was expressed as a barrier or facilitator, affirming the importance of context when implementing system-level delirium screening.
CONCLUSION
One of the first studies to test a two-step process for delirium identification, and to involve NAs in screening, the findings demonstrate overall support from clinicians for delirium identification, and describe the need for a multi-faceted, contextualized, and systemic approach to implementation and evaluation of delirium screening
Keywords: Delirium, hospitalized older adults, observations
INTRODUCTION
Developing a standardized approach for efficiently identifying delirium in hospitalized older adults is a health care imperative. Several tools are available for delirium identification; the efficacy and uptake of these tools vary.1, 2 We designed and field-tested implementation of a protocol for identifying delirium in hospitalized older adults that involves three major innovations.
The first innovation is a two-step process that involves an ultra-brief 2-item screen (the UB-2) as step-one. The UB-2 can effectively rule out delirium in less than 40 seconds, with a 93% sensitivity in persons with and without dementia.3, 4 If the person correctly answers both items in the UB-2, the protocol is complete; if not, the 3D-CAM is administered as step two.3, 4 The 3D-CAM is a validated diagnostic interview for delirium that can be completed in three minutes.5 We refer to this two-step process as the UB-CAM. (See Supplementary file S1, S2, S3)
The second major innovation was development of a mobile application (App) for efficient delivery of the protocol and data collection. Our field team examined protocol implementation in real time to understand the conditions and environments under which delirium assessment occurs, and the challenges associated with implementing the UB-CAM into practice. Our third innovation was to involve nursing assistants in protocol delivery. Despite providing the most direct and sustained interaction with patients, nursing assistants are not typically asked to participate in evaluation of mental status.
The overarching goal driving our innovations was to enhance the acceptability, adoption, and sustainability of the protocol. The purpose of this study was to explore the barriers and facilitators of implementing the UB-CAM in acute care, to inform its implementation.
METHODS
Study Design
This study used a qualitative descriptive design, conducive to research in health care environments.6 Trained field researchers, experienced in acute care data collection, collected observational data about the patient environment and administration of the protocol, and the experiences of consented clinical staff during implementation. Researchers kept field notes of observations on the unit, such as patient emergencies and staffing. Observational data were supplemented with brief semi-structured interviews to elicit the clinician’s views on protocol effectiveness, patient experience, and potential ways to improve the experience for both clinicians and patients.
Settings / Participants
A multistage purposive sampling technique was used at two sites, an urban academic medical center, and a community teaching hospital. A total of 322 clinicians participated, including 50 physician hospitalists, 189 registered nurses, and 83 nursing assistants. All clinicians were trained to administer the UB-2 (step-one); nurses and hospitalists were trained to complete the full 2-step UB-CAM (i.e., the UB-2 and 3D-CAM). Training included didactic and interactive methods and ranged from 15–40 minutes. Patients 70 years or older were recruited into the hybrid type-1 effectiveness-implementation design of the broader study. 7Patients were screened at random times throughout the day, once by each type of clinician.
Theoretical Framework
The study was guided by a modified multi-level framework designed to assist with successful implementation of findings into practice.8 The framework comprises of five causal constructs known to affect implementation: 1) structural factors (physical environment, staffing, and ambience); 2) organizational factors (staff satisfaction and morale); 3) patient factors (patient verbalizations, appearance and response); 4) provider factors (clinician verbalizations or behaviors/actions that reflect beliefs or attitudes, and motivations); and 5) innovation (i.e., the UB-CAM itself and evidence of readiness to implement it). This framework was used to guide data collection, and to organize data for analysis.
Data Collection
Data was collected over 14 months and included protocol observations, field notes, and clinician interviews. Data collection was led at each site by a project director/qualitative researcher. Field staff were trained by experienced qualitative researchers with video-conferenced and in person sessions; weekly field team meetings were used to review data and address questions.
Observation Data
Field researchers conducted direct observation during implementation of the UB-CAM at the patients’ bedside, assuming a non-participant observation stance. Guided by the five-factor model they generated data that included environmental information and details about the patient and clinician behaviors and interactions.9 As soon as possible following the observation, researchers dictated their notes either into a hand-held device, or directly into a computer. If using the hand-held device, researchers downloaded audio onto the laptop, used Dragon Software10 to transcribe the audio, then verified the transcription. Completed observations were uploaded as a document into REDCap.TM11 For quality control, protocol observations were reviewed by the authors (MB, DF, EH, PS) using a continuous, iterative process.
Interviews
Immediately following completion of the UB-CAM, brief interviews (n=231) were conducted with providers, to elicit their views on its usefulness and implementation. Interviews were conducted face-to-face, were recorded and stored in the same fashion as the observations, and ranged in duration from five to 10 minutes. The interview guide was an iterative process and is found in the supplementary material (See Supplementary file S4). Analyses were conducted in parallel with ongoing observations and interviews to evaluate for thematic saturation. Data include a total of 767 observations (Physicians=258; Nurses=255; Nursing Assistants=254) and 231 interviews (Physicians=87; Nurses=91; Nursing Assistants=53). The study was approved by the Institutional Review Boards of the participating sites.
Data Analysis
Thematic analysis was conducted using the six steps of Braun & Clarke.12 De-identified data was downloaded from REDCap and imported into Dedoose13 software for data organization and management. In step one, two researchers (MB and PS) independently read and reread the data to familiarize themselves with the content and note initial ideas. Step two involved collaborative, manual systematic coding of significant features of the data. During this phase, several iterative double-coding meetings were conducted until agreement was reached. During step three, codes were sorted and collated into themes. Step four involved confirming that themes correlated with the codes and the entire dataset. In step five, themes were defined, named, and then refined and validated. In the final step, selected extracts and the analysis were related back to the research question and to the literature. Rigor was supported by the methodological experience of the researchers, the use of a codebook, a detailed audit trail, and participant validation.14
RESULTS
The clinician participants were in their current profession an average of seven years, with an average of five years at their current location. See Table 1 for additional clinician characteristics.
Table 1.
Clinician Demographics and Background
| Hospitalist n=50 |
Nurse n=189 |
Nursing Assistant n=83 | TOTAL N=322 |
|
|---|---|---|---|---|
| n (%) | ||||
| Gender | ||||
| Male | 29 (58) | 16 (8) | 6 (7) | 51 (16) |
| Female | 21 (42) | 173 (92) | 77 (93) | 271 (84) |
| Race | ||||
| American Indian or Alaska Native | 1 (2) | 1 (1) | 1 (1) | 3 (1) |
| Asian | 16 (32) | 7 (4) | 7 (8) | 30 (9) |
| Black or African American | 2 (4) | 8 (4) | 30 (36) | 40 (13) |
| White | 31 (62) | 166 (88) | 37 (45) | 234 (73) |
| Other | 0 | 7 (4) | 7 (8) | 14 (4) |
| Refused | 0 | 0 | 1 (1) | 1(0) |
| Ethnicity | ||||
| Hispanic or Latino | 1 (2) | 13 (7) | 10 (12) | 24 (7) |
| Non-Hispanic or Latino | 49 (98) | 174 (92) | 70 (85) | 293 (91) |
| Other | 0 | 2 (1) | 2 (3) | 4 (2) |
| Native/first language | ||||
| English | 46 (92) | 174 (92) | 54 (65) | 274 (85) |
| Other | 4 (8) | 15 (8) | 29 (35) | 48 (15) |
| Years practicing | ||||
| ≤ 5 years | 37 (74) | 140 (74) | 58 (70) | 235 (73) |
| > 5 years | 13 (26) | 49 (26) | 25 (30) | 87 (27) |
| Geriatrics/Gerontology certified | 1 (2) | 2 (1) | 2 (2) | 5 (1.5) |
The coded interview data and field notes were categorized into six broad themes, each with the potential to act as a barrier or facilitator to delirium screening: 1) physical setting and milieu; 2) practice environment; 3) integration into role; 4) adaptive techniques; 5) patient responses; and 6) systematic assessment. Table 2 provides a summary of barriers and facilitators and illustrative quotes in alignment with the multi-factor implementation framework.8
Table 2.
Quotes, barriers and facilitators, and themes organized by the multi-level framework implementation factors of Chaudoir et al.7
| Factors | Themes | Barriers (−) and facilitators (+) | Quotes |
|---|---|---|---|
| Structural | I. Physical setting and milieu | − Noise − Interruptions/distractions − Limited space, seating /access to patient + Privacy + Adequate lighting + Controlled TV volume +/− Family/visitor presence |
“Two nursing students standing in the hallway near the patient’s room talking loud... I had a bit of difficulty hearing the patient’s responses even after repositioning myself to be on the other side of her bed.” (FR) “patient seemed to be distracted by the television” (FR) |
| Organization | II. Practice environment | − High workload − Low morale |
“No matter how many times you tell them what’s wrong, nothing ever changes.” (NA016) “…nurses appear to be running all over the unit… alarms going off” (FR) “They have a lot of open positions, but they are not filled because physicians get burnt out.” (H004). “Big issues are communication, and …feeling undervalued or underappreciated.” (N005) |
| Clinician | III. Integration into Role | + Efficiency of the protocol + Alignment with role functions + Perception of compatibility with scope of practice |
“Fitting it into my day wouldn’t be hard…. Hey, are you eating, are you using your bowels, hey, let’s talk about this stuff real quick…it would be easy every day…” (N005) “The questions could be asked by either nurses or PCTs [nursing assistants], as they do not require a medical degree to ask.” (H020) “We are the ones that spend real time with them.” (NA004) |
| IV. Adaptive techniques | + Relational communication + Attention to sensory loss + Physical and emotional comfort measures + Adaptation to patient personality − Minimizing the importance of cognitive assessment − Assurances to patient |
“I just have a couple of silly questions to ask you…” (H040) “Could you help me out here, like, you’re doing me a favor, I really need to get these answers” (NA046) |
|
| Patient | V. Patient responses | − Physical symptoms + Humor − Anxiety − Embarrassment − Frustration − Agitation |
She (patient) is challenging, she has made a member of our staff (MD) cry.” (H016) “Those with dementia can get agitated with the questions because they may not be able to do them.” (N182) |
| Innovation | VI. Systematic assessment | + Perceived benefits to patient + Sensitivity of measures + App and measure efficiency − Need for supplementary and serial assessment |
“I used to use a Gestalt approach to delirium assessment…was missing a lot of delirium…(I) like that it is highly sensitive in order to see mental status changes that are not obvious.” (H032) “About 50% of (my) patients would likely benefit from the questions.” (N054). |
H= Hospitalist, N= Nurse, NA= Nursing Assistant, FR= Observation of Field Researcher
Physical Setting and Milieu
Factors in both the patients’ physical and social environment presented barriers to efforts to identify delirium. Distractions, related to equipment and hallway and nursing station conversations, impeded communication. Limited space included lack of room for a chair or for the clinicians to move. Environmental attributes that facilitated the assessment process included privacy, adequate lighting, and noise control.
Visitor presence during the interview could be either a barrier or facilitator. Some visitors interfered by “helping,” the patient with cues and prompts; some explicitly identified a wrong response. In contrast, other visitors remained silent and a few family members recommended the screening and offered words of encouragement.
Practice Environment
All clinician types appeared to be challenged by barriers in the practice environment. related to workload and low morale. A “hectic unit” and the demands of multiple patients were common. It was difficult at certain times of the day to assess delirium. One nurse reported, “this is hard to do at 7am” (change of shift) when “bare minimum seems to be covered and things are missed” (N007).
Integration into Role
All clinician types were willing to screen for delirium and were observed to implement the protocol seamlessly with other role functions. For example, a nurse conducted the screening prior to administering medications; a hospitalist included the questions within her review of symptoms and assessment; a nursing assistant used delirium screening as a preamble to personal care. None of the clinicians, including the nursing assistants, described delirium screening as outside of their scope of practice or role. However, some hospitalists recommended that non-physicians conduct the screening because it was “efficient” and “easy”(Table 2).
Adaptive Techniques
Clinicians generally adapted their approach to promote patient engagement and comfort during screening. Attention to sensory loss (e.g., providing hearing amplifiers) and both physical and emotional comfort were noted as facilitators. In addition, clinician concern and interest, and communication at eye level, appeared to facilitate engagement. Attempts to “normalize” the communication, or “put the patient at ease,” prior to screening was observed including conversations with patients about their background or family.
Nursing assistants described individualized communication approaches demonstrating empathy and adaptation to the patient’s personality, emotional state, and situation. One approach included framing the questions as a favor and asking the patient for help. One nursing assistant described adaptation as being “chameleon” -like, stating, “your personality has to fit the personality of the person” (NA004).
Some clinicians attempted to decrease patient anxiety by minimizing the importance of the cognitive evaluation, potentially posing a barrier to thorough assessment (including follow-up). For example, a hospitalist referred to “a couple of silly questions” (H040); a nurse described the assessment as “not a big deal” (N180). Other clinicians (all disciplines) frequently assured patients that they (the patients) would be successful in correctly responding to questions, potentially offering false assurances.
Patient Responses
Some screenings were declined or interrupted by physical symptoms (e.g., pain, sedation, fatigue, coughing, dyspnea). Other patients demonstrated behavioral and affective responses, such as closing their eyes or furrowing their brow in concentration. Some said responses to themselves before offering responses to the screener, and some counted the months backward using their fingers. Humor commonly accompanied responses, perceived by field researchers as an attempt to deflect anxiety, or normalize the interaction. A few patients expressed frustration when perceiving the protocol questions as irrelevant to their medical condition.
There were patients who expressed anxiety and/or fear of embarrassment in anticipation of the screening. Some patients who were not able to answer questions correctly showed distress.
Systematic Assessment
Clinicians described a need for delirium screening and appreciated the ease of delivering the UB-CAM two-step process with an App; they reported built-in prompts and direct electronic data entry on the iPad simplified the process. The systematic nature of the protocol and its perceived sensitivity was also valued, with one hospitalist noting the UB-CAM had picked up delirium where he had missed it. The need for supplementary assessment was described, including acquiring information on baseline cognition, and distinguishing between hyperactive and hypoactive delirium. Several clinicians reported that more than one evaluation was often required, stating the need for “looking at the patient’s trajectory” (N062). Several nurses described the need to also monitor affect and behavior, especially in patients who have dementia.
DISCUSSION
The purpose of this study was to better understand the conditions under which delirium assessment occurs and explore the barriers and facilitators to delirium detection. The findings underscore the importance of developing a system-level approach that addresses the physical setting and milieu, practice environment, clinician’s integration into role and adaptive techniques, patient responses, and systematic assessment (Figure 1).
Figure 1.
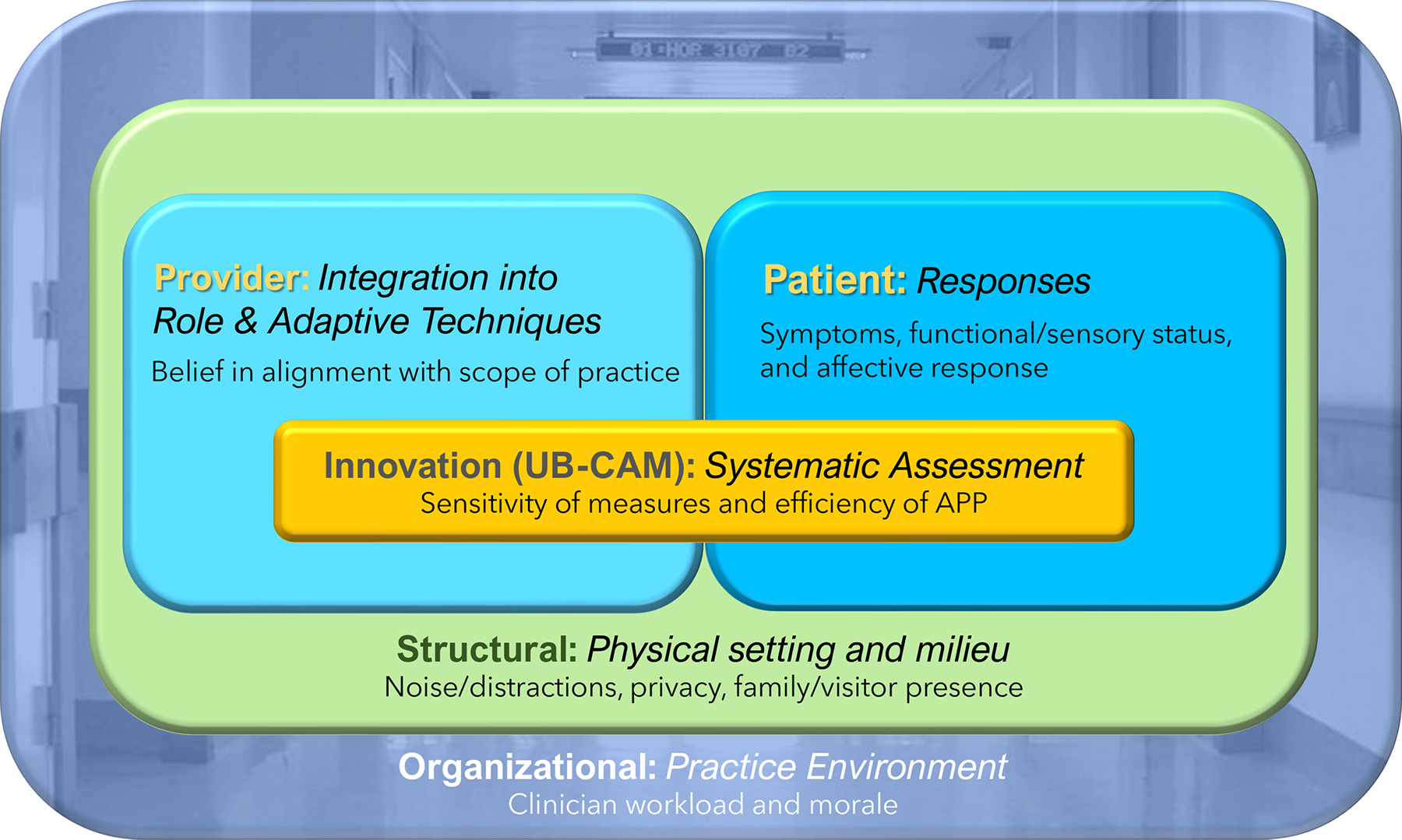
Factors Influencing Implementation of Delirium Detection in Acute Care
The clinicians described structural and organizational factors that promote or constrain delirium screening. Although there is considerable evidence demonstrating the negative effects of noise, limited space and seating upon the hospitalized patient’s function and comfort,15, 16 this study illuminates how the physical setting challenges clinicians’ efforts to conduct accurate assessments, including delirium screening. As the Age-Friendly Health Systems initiative17 expands, environmental policies and tools will be important complements to evidence-based clinical protocols. Findings underscore the role of family. Family caregivers can provide information on baseline cognition - critically important for delirium identification,18 and have shown to be reliable reporters using a standardized delirium assessment.19
Not surprisingly, clinicians described high workload, multiple competing demands, and low morale in the practice environment during protocol implementation. Previous studies have shown that initiatives to implement delirium screening must provide adequate training and a supportive practice environment or sensitivity of the tool falls to unacceptable levels. Thus, initial “readiness” and ongoing appraisal of the practice environment is critical for adoption and sustainability.20–22
All clinician types described the ability to integrate the UB-CAM into their role and routine, without adjustments in workflow, assignments or deployment. These results are corroborated to some extent by the work of Voyer and colleagues,23 which demonstrated feasibility of nurses integrating delirium monitoring into medication administration. Findings associated with this theme warrant future investigation to explore their respective training needs, methods for communicating to other disciplines, and integration of delirium findings into an interdisciplinary plan of care.
The clinicians in our study demonstrated attention to the well-being of patients through consistent use of adaptive techniques to promote the patient’s physical and emotional comfort. Their attempts to establish a positive rapport and normalize the assessment process by showing interest in the patient and engaging in conversation appeared to facilitate evaluation. However, providing assurances that the patient would answer correctly and minimizing the importance of the questions may have the effect of lessening accuracy. A more purposeful approach is to educate patients and families about the brain as a critical organ, and the UB-CAM as a vital sign of brain function.4, 24 This finding corroborates other research that identifies the need for both intellectual and interpersonal skills to attend to the patient’s emotional needs while providing evidence-based care.25
Variable patient responses to the protocol were influenced by mood, medical, and cognitive status. The efficiency of the assessment process facilitated acceptance of the protocol. Some patients who answered questions incorrectly seemed to express agitation, consistent with research in older adults who are depressed and or have dementia.23 These results suggest the importance of observing for subtle cognitive signs that signal need for post- acute follow up for dementia and depression in patients with delirium.26, 27
The enthusiasm for the UB-CAM’s utility, and its facilitation of systematic assessment, promoted clinician engagement in its use. This finding corroborates previous research describing clinicians’ desire for an efficient, sensitive method of identifying delirium.28–30 The clinicians were very positive about the App and found it promoted efficiency and accuracy of documentation. This is the first study to incorporate an interactive electronic platform in delirium screening and the positive response of users warrants additional investigation of utility and efficacy. Clinicians reported that persons with dementia may require additional assessment, and this is an area for future research.
Study results are instructive in identifying the following practical components of a system wide program to support accurate and timely identification of delirium: 1) environmental modification; 2) organizational assessment to evaluate the practice environment and readiness for practice change; 3) policy that supports family engagement; 4) clearly defined policy on communication of positive findings; 5) patient and family education; and 6) staff education and support for addressing the rationale for delirium identification, procedures, and interdisciplinary collaboration to identify and respond to delirium. These components will be important considerations in a larger implementation trial.
This exploratory study was limited in that observations and interviews provide only a snapshot of the protocol implementation and did not consider all patient, clinician, and organizational characteristics that may influence the findings. In particular, administrative and managerial support, organizational culture, the number and deployment of clinicians, and patient characteristics including acuity were not examined in depth. However, the study has several strengths and innovations including the use of observational methods to capture the real world, real-time experiences of clinicians, the inclusion of nursing assistants in identification, and a sample size of more than 700 observed protocols, promoting diversity and breadth to our data.
In conclusion, this study illuminates important factors to consider when planning and evaluating the implementation of a delirium screening protocol. Future research should further examine the patient and caregiver response to assessment, and administrative and leadership facilitators for successful assessment of delirium.
Supplementary Material
Supplementary file S1: UB-2 (Ultra-brief 2-item delirium screening tool)
Supplementary file S2: UB-CAM (2-step delirium identification tool)
Supplementary file S3: 3D-CAM (3 minute- delirium screening tool)
Supplementary file S4: Interview guide
Key points:
This is one of the first studies to test a two-step process for delirium identification in older adults, and to involve Nursing Assistants in delirium screening.
This study illuminates important factors to consider when planning and evaluating the implementation of a delirium screening protocol.
Future research should further examine the patient and caregiver response to assessment, and administrative and leadership facilitators for successful identification of delirium.
Why does this paper matter?
This study provides crucial information for interdisciplinary delirium identification across settings of care. This work has the potential to change the culture of care, policy, and practice by making delirium identification more efficient and accurate, and part of routine care.
ACKNOWLEDGEMENTS
The authors would like to thank Janice Penrod for sharing her methodological expertise, providing theoretical guidance, and for training field researchers on techniques of focused ethnography.
Funding sources: This work was supported by the National Institute on Aging [R01AG030618 to D.M.F. and E.R.M., K24AG035075 to E.R.M., R01AG044518 to S.K.I., R24AG054259 to S.K.I., P01AG031720 to S.K.I.; and the National Institute of Nursing Research [R01NR01104 to D.M.F.].
Sponsor’s role: The opinions, findings, and conclusions or recommendations expressed in this publication are those of the authors and do not necessarily reflect those of the National Institute on Aging and the National Institute of Nursing Research.
Footnotes
Conflict of interest declaration: No conflict of interest to declare from all the authors and c0-authors.
Contributor Information
Erica K. Husser, Penn State College of Nursing, University Park, PA.
Donna M. Fick, Penn State College of Nursing, University Park, PA.
Marie Boltz, Penn State College of Nursing, University Park, PA.
Priyanka Shrestha, Penn State College of Nursing, University Park, PA.
Jonathan Siuta, Mount Nittany Medical Center, State College, PA.
Shannon Malloy, Beth Israel Deaconess Medical Center, Boston, MA.
Abigail Overstreet, Beth Israel Deaconess Medical Center, Boston, MA.
Douglas L. Leslie, Penn State College of Medicine, Hershey, PA.
Long Ngo, Division of General Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA; Department of Biostatistics, Harvard T.H. Chan School of Public Health, Boston, MA.
Yoojin Jung, Division of General Medicine, Beth Israel Deaconess Medical Center, Boston, MA.
Sharon K. Inouye, Hebrew SeniorLife, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA.
Edward R Marcantonio, Divisions of General Medicine and Gerontology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA.
REFERENCES
- 1.Inouye SK, Foreman MD, Mion LC, Katz KH, Cooney LM. Nurses’ recognition of delirium and its symptoms: Comparison of nurse and researcher ratings. Arch Int Med 2001;161(20):2467–2473. 10.1001/archinte.161.20.2467 [DOI] [PubMed] [Google Scholar]
- 2.Inouye SK, Van Dyck C, Alessi C, Balkin S, Siegal A, Horwitz R. Clarifying confusion: The confusion assessment method. Ann Int Med 1990;113(12): 941–948. 10.7326/0003-4819-113-12-941 [DOI] [PubMed] [Google Scholar]
- 3.Fick DM, Inouye SK, Guess J, et al. Preliminary development of an ultrabrief two‐item bedside test for delirium 2015;10(10): 645–650. 10.1002/jhm2418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fick DM, Inouye SK, McDermott C, et al. Pilot study of a two-step delirium detection protocol administered by certified nursing assistants, physicians, and registered nurses. J Gero Nurs 2018;44(5):18–24. 10.3928/00989134-20180302-01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marcantonio E, Ngo L, Jones R, et al. 3D-CAM: Derivation and validation of a 3-minute diagnostic interview for CAM-defined delirium: A cross-sectional diagnostic test study. Ann Int Med 2014;161(8):554–561. 10.7326/M14-0865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Colorafi KJ, Evans B. Qualitative descriptive methods in health science research. HERD 2016;9(4):16–25. 10.1177/1937586715614171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Landes SJ, McBain SA, Curran GM. An introduction to effectiveness-implementation hybrid designs. Psychiatry Research 2019; 280: 112513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chaudoir SR, Dugan AG, Barr CH. Measuring factors affecting implementation of health innovations: A systematic review of structural, organizational, provider, patient, and innovation level measures. Implement Sci 2013;8(1)22. 10.1186/1748-5908-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mack N, Woodsong C, Macqueen K, Guest G, Namey E. Qualitative research methods: A data collector’s field guide. Family Health International 2005. [Google Scholar]
- 10.Dragon Software Website. http://www.nuancesoftwarestore.com.
- 11.REDCap Website. https://projectredcap.org/about/
- 12.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 13.Dedoose Software website. www.softwareadvice.com/collaboration/dedoose-profile.
- 14.Guba EG. ERIC/ECTJ Annual Review Paper: Criteria for assessing the trustworthiness of naturalistic inquiries. ECTJ 1981;29(2):75–91. www.jstor.org/stable/30219811 [Google Scholar]
- 15.Frampton SB. Healthcare and the patient experience: Harmonizing care and environment. HERD 2012;5(2):3–6. 10.1177/193758671200500201 [DOI] [PubMed] [Google Scholar]
- 16.Pope D. Decibel levels and noise generators on four medical/surgical nursing units. J Clin Nurs 2010;19(17‐18):2463–2470. [DOI] [PubMed] [Google Scholar]
- 17.Fulmer T, Mate KS, Berman A. The age‐friendly health system imperative. J Am Geriatr Soc 2018;66(1):22–24. 10.1111/jgs.15076 [DOI] [PubMed] [Google Scholar]
- 18.Roberts AR, Ishler KJ, Adams KB. The predictors of and motivations for increased family involvement in nursing homes. Gerontologist 2018;60(3)535–547. 10.1093/geront/gny158 [DOI] [PubMed] [Google Scholar]
- 19.Rosgen B, Krewulak K, Demiantschuk D, et al. Validation of caregiver-centered delirium detection tools: A systematic review. J Am Geriatr Soc 2018;66(6):1218–1225. 10.1111/jgs.15362 [DOI] [PubMed] [Google Scholar]
- 20.Aiken LH, Sloane DM, Clarke S, et al. Importance of work environments on hospital outcomes in nine countries. Int J Qual Health Care 2011;23(4):357–364. 10.1093/intqhc/mzr022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Helfrich CD, Blevins D, Smith JL, et al. Predicting implementation from organizational readiness for change: A study protocol. Implement Sci 2011;6(1),76. 10.1186/1748-5908-6-76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sharma N, Herrnschmidt J, Claes V, Bachnick S, De Geest S, Simon M. Organizational readiness for implementing change in acute care hospitals: An analysis of a cross‐sectional, multicentre study. J Adv Nurs 2018;74(12):2798–2808. 10.1111/jan.13801 [DOI] [PubMed] [Google Scholar]
- 23.Voyer P, Champoux N, Desrosiers J, et al. Recognizing acute delirium as part of your routine [RADAR]: A validation study. BMC Nurs 2015;14(1):19. 10.1186/s12912-015-0070-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet 2014; 383(9920):911–922. 10.1016/S0140-6736(13)60688-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Scerri A, Innes A, Scerri C. Person-centered dementia care in acute hospital wards–The influence of staff knowledge and attitudes. Geriatr Nurs 2020;41(3):215–221. doi: 10.1016/j.gerinurse.2019.09.001. [DOI] [PubMed] [Google Scholar]
- 26.Landreville P, Voyer P, Carmichael P-H. Relationship between delirium and behavioral symptoms of dementia. Int Psychogeriatr 2013;25(4):635–643. 10.1017/S1041610212002232 [DOI] [PubMed] [Google Scholar]
- 27.Hölttä E, Laakkonen M-L, Laurila JV, et al. The overlap of delirium with neuropsychiatric symptoms among patients with dementia. Am J Geriatr Psychiatry 2011;19(12):1034–1041. 10.1097/JGP.0b013e31820dcbb6 [DOI] [PubMed] [Google Scholar]
- 28.Marcantonio ER. In the clinic: Delirium. Ann Intern Med 2011;154:ITC6–1-ITC6–1. [DOI] [PubMed] [Google Scholar]
- 29.Wong EK-C, Lee JY, Surendran AS, et al. Nursing perspectives on the confusion assessment method: A qualitative focus group study. Age Ageing 2018; 47(6):880–886. 10.1093/ageing/afy107 [DOI] [PubMed] [Google Scholar]
- 30.Morandi A, Davis D, Taylor JK, et al. Consensus and variations in opinions on delirium care: a survey of European delirium specialists. International Psychogeriatrics 2013; 25(12):2067–2075. doi: 10.1017/S1041610213001415 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary file S1: UB-2 (Ultra-brief 2-item delirium screening tool)
Supplementary file S2: UB-CAM (2-step delirium identification tool)
Supplementary file S3: 3D-CAM (3 minute- delirium screening tool)
Supplementary file S4: Interview guide


