Abstract
Aims:
To analyze the prevalence, comorbidities, outcomes and costs of type 2 diabetes mellitus (T2DM) patients with and without coronary artery disease (CAD) or stroke in a population of over 7 million inhabitants.
Methods:
T2DM patients were identified in 2015 (accrual period) from the Ricerca e Salute (ReS) database linking administrative records to demographics. Based on 2013–2015 information, four cohorts were considered: #1 with CAD and/or stroke; #2 without CAD and/or stroke; #3 with chronic CAD but no myocardial infarction or stroke; #4 with chronic CAD undergoing percutaneous coronary interventions (PCI). Hospitalizations, drugs and other outpatient care were assessed from 2015 to 2017.
Results:
The prevalence of T2DM was 6% (441,085/7,365,954). CAD and/or stroke in the previous 3 years affected 7.5% of T2DM patients (33,153); this cohort was generally older, of male sex, with more comorbidities, prescriptions, and hospital admissions (50.5% versus 13.4% during the first follow-up year) compared to cohort #2. Yearly costs were over three-fold for cohort #1 versus #2, main drivers being hospitalizations in the former and drugs in the latter. Two-year cardiovascular events were recorded significantly more commonly in cohort #4 compared to the other cohorts. Guideline-recommended lipid-lowering therapy was <80% in all but cohort #4.
Conclusions:
The present analysis points to three areas of potential improvement in T2DM management: (a) guideline-recommended treatment patterns of T2DM patients; (b) three-fold recurrences and costs in T2DM patients with, compared to those without, prior cardiovascular events; (c) high event rates associated with chronic CAD and PCI, warranting specific studies aimed at improved prevention.
Keywords: big data, coronary artery disease, diabetes mellitus, public health practice
Introduction
In the past decade, there have been improvements in the control of traditional risk factors such as hypertension and hypercholesterolemia. 1 In contrast, the diagnosis of type 2 diabetes mellitus (T2DM) has increased globally and this increase is expected to continue.1,2 Patients with T2DM are prone to vascular complications, both microvascular (such as retinopathy, neuropathy, kidney disease) and macrovascular (such as atherothrombotic events); the most important causes of morbidity and mortality are acute coronary syndromes (ACSs) and/or cerebrovascular diseases, specifically ischemic stroke.3,4 Patients with T2DM who have already suffered a coronary and/or cerebrovascular event are considered at very high risk of recurrences and premature death, as well as those with chronic coronary syndrome (CCS) without prior acute atherothrombotic events. 5 Significant advances have been made in managing the acute and subacute phases of atherothrombotic diseases in T2DM patients. 6 In contrast, chronic T2DM patients at high risk of adverse events, who might benefit from long-term intensification of preventive therapy, remain a challenge.
Diabetes patients included in controlled trials are generally selected on the basis of protocol eligibility and, therefore, do not fully represent the entire population encountered in clinical practice. To describe accurately the demographics and clinical characteristics of diabetes patients, several well designed registries have recently been created;7–9 however, even these patients are selected to a certain extent, being mostly admitted to tertiary specialty wards with high standards of care. Analyses of real world data may be particularly useful in providing a realistic description of the clinical course and healthcare burden of diabetes patients.
The longitudinal Ricerca e Salute (ReS) database10,11 covers more than 7 million inhabitants and links different sources of information (such as demographics) with National Health Service (NHS) administrative data, including drug prescriptions and outpatient diagnostic/therapeutic procedures or hospital records. From this database it is possible to assess the prevalence of diabetes in a contemporary general population and compare, among diabetes patients with or without a prior coronary or cerebrovascular event, the following elements: (a) baseline demographics and clinical characteristics; (b) prescriptions of preventive therapy, as well as rates and types of hospital admissions during follow-up; and (c) annual costs for the NHS.
Methods
Administrative data flows (the same sent to the Italian Health Ministry) were transferred from several local Italian health authorities to the non-profit ReS Foundation, physically located within the CINECA Institution. CINECA is a large consortium of Italian universities, established in 1969, equipped with supercomputing tools that allow ReS to ensure both quality and security of data management at international standards. Five-year longitudinal analyses were retrospectively carried out on the ReS population-based database, linking demographics, drug prescriptions, hospital records, and outpatient specialist exams and procedures.
The study was conducted in conformity with the European law regarding privacy protection [Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC (General Data Protection Regulation) https://eur-lex.europa.eu/legal-content/IT/TXT/?uri=celex%3A32016R0679]. Demographics were made anonymous at the source, with administrative data and results provided in aggregated form; therefore, according to the above regulation, informed consent and ethics approval were not sought. The study was conducted for institutional purposes by specific agreement with regions and local health units of the Italian NHS.
Selection of study population and cohort definitions
Subjects with T2DM were selected in 2015 (accrual period) based on one or more of the following criteria: hospital diagnosis, ‘disease exemption’ code, reimbursed anti-diabetic drug (Supplemental Table 1). In Italy, patients with severe chronic diseases (including T2DM) are relieved from paying a fee for drugs and for out-of-hospital diagnostic/therapeutic procedures (so called ‘disease exemption’). Administrative databases have a disease-related code to identify such patients. Disease exemption codes were gathered from prescriptions or from demographics. The most recent date linked to a patient’s identification criterion was taken as the index date.
Information drawn from the preceding 2 to 3 years (2013–2015) was used to group T2DM subjects into four partially overlapping cohorts:
cohort #1 with T2DM and evidence of coronary artery disease (CAD, including myocardial infarction (MI) or coronary revascularization procedures) or stroke;
cohort #2 with T2DM but not CAD or stroke;
cohort #3 with T2DM and CAD, but no acute atherothrombotic events (chronic CAD subgroup of cohort #1, after excluding patients with MI or stroke);
cohort #4 with T2DM and chronic CAD, with no prior MI or stroke, treated with at least one percutaneous coronary intervention (PCI) procedure (subgroup of cohort #3).
Detailed criteria to identify the above cohorts are listed in Supplemental Table 2.
Demographic and clinical characteristics
The four T2DM cohorts were further characterized during the accrual period by prevalence, sex, age and additional clinical characteristics, namely: hypertension, dyslipidemia, chronic lung diseases, depression, neoplasia, heart failure, chronic kidney disease (CKD), atrial fibrillation, and severe liver disease. The specific criteria to identify the above comorbidities are listed in Supplemental Table 3.
Pharmaceutical data were drawn from free-filled drug prescriptions collected by local and hospital pharmacies; international anatomical therapeutic chemical (ATC) and Italian marketing authorization (AIC) codes were used to classify drugs. Dose, number of packages, dispensing date and cost of medicinal products and generics were also registered. In-hospital diagnoses and invasive procedures were recorded according to the 9th version of the International Classification of Disease – clinical modification (ICD-9-CM) codes from hospital discharge forms, including day hospital records. Outpatient healthcare data consisted of specialist invasive/non-invasive therapeutic and diagnostic procedures performed within ambulatory care facilities of the Italian NHS, and collected using national classifications.
Healthcare resource use
Each T2DM subject was followed over 2 years after the index date for drug prescriptions, outpatient specialist services and hospitalizations. The most commonly prescribed drugs reimbursed by the NHS are reported by therapeutic subgroup (ATC code level II). Antithrombotic agents were identified by active substance (ATC code level V). Drug therapy is expressed as the percentage of treated patients, and drug doses as average defined daily dose (DDD) per patient. Outpatient specialist care, according to the Italian national classification, is expressed as the percentage of users. Finally, the most frequent primary diagnoses leading to at least one overnight hospitalization were identified by ICD-9-CM code, expressed as the percentage of affected patients and average length of stay.
Time-to-hospitalization analysis
For each of the four T2DM cohorts, the estimated percentage who underwent hospitalizations for stroke/transient ischemic attack (TIA), ACS, peripheral artery disease (PAD) or at least one of these events during the 2-year follow-up was estimated. The criteria to identify these diseases are listed in Supplemental Table 4. Censoring criteria were in-hospital death or loss to follow-up owing to transfer to healthcare services not included in the ReS database.
Statistical analyses
When administrative data are analyzed, the number of patients/events is so large that even minimal differences will result in a conventional level of statistical significance (two-sided p < 0.05), often without a corresponding convincing level of clinical significance. For this reason, we have generally avoided the use of detailed p values and have described nominal differences. For those unfamiliar with this approach, conventional p values have been specified in the tables and figures. Continuous values are expressed as mean ± standard deviation (SD). Proportions are expressed as ratios or percentages. The Kaplan–Meier estimator was used to produce cumulative incidence curves for the four T2DM cohorts (monthly percentage of patients in subjects at risk). The curves were compared by log rank test to assess whether differences could be considered statistically significant (p < 0.01) or not. Because this analysis is purely observational, and the catchment area is very broad, a formal sample size was not calculated. All statistical analyses were performed by Oracle SQL Developer version 17.
Results
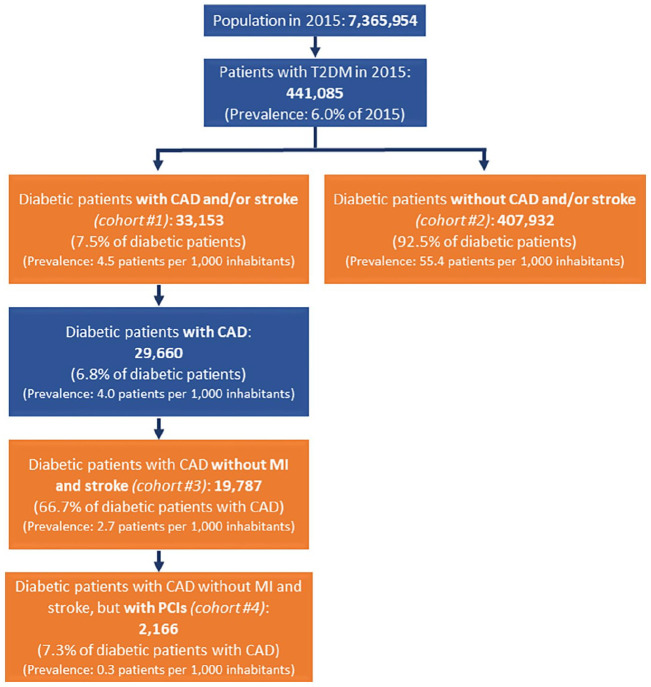
From a general population of 7,365,954 subjects, the present analysis revealed 441,085 affected by T2DM in 2015 (6.0% of the overall population) (Figure 1). Of these, 33,153 T2DM subjects (7.5%) were diagnosed with CAD and/or stroke in the preceding 3 years (cohort #1). The remaining 407,932 T2DM subjects (92.5%) represented cohort #2. Among cohort #1 T2DM patients, those with CAD were 29,660 (6.8% of all T2DM patients and 89.5% of those with CAD or stroke), and those without MI or stroke were 19,787 (4.5% of all T2DM patients, 59.7% of those with CAD or stroke, and 66.7% of those with CAD), representing CCS T2DM patients without acute events in the preceding 3 years – cohort #3. Out of cohort #3, 2166 underwent PCI at least once in the period 2013–2015, representing 7.3% of those T2DM patients who had CAD but no MI or stroke diagnosis in the previous 3 years (cohort #4).
Figure 1.
Flow chart describing the identification of type 2 diabetes mellitus (T2DM) patients in 2015 and the selection of the four cohorts based on 2013–2015 information.
CAD, coronary artery disease; MI, myocardial infarction; PCI, percutaneous coronary intervention.
Demographics and clinical characteristics
Female sex accounted for 51.3% of T2DM subjects without CAD or stroke diagnosis in the previous 3 years (cohort #2) but only approximately one-third of the three other cohorts. T2DM patients with CAD or stroke diagnosis in the previous 3 years were significantly older than those without these events (73 ± 10 versus 67 ± 14 years) and more often had hypertension and dyslipidemia (93.8% and 76.2%, respectively, versus 69.8% and 46.3%) (Table 1). Lung, kidney and other cardiovascular comorbidities, specifically heart failure and atrial fibrillation, were also more frequent in the T2DM cohorts with a prior cardiovascular diagnosis compared to cohort #2 (Table 1). Similar profiles were present in CCS patients without prior atherothrombotic events (cohort #3) and in CCS patients without atherothrombotic events treated with PCI (cohort #4).
Table 1.
Demographic and clinical characteristics of the four T2DM cohorts identified during the accrual period (2015).
| Variable | T2DM patients with CAD and/or stroke (cohort #1) n=33,153 | T2DM patients without CAD or stroke (cohort #2) n=407,932 | T2DM patients with CAD, but no MI or stroke (cohort #3) n=19,787 | T2DM patients with CAD and PCI, but no MI or stroke (cohort #4) n=2166 |
|---|---|---|---|---|
| Age, years (mean ± SD) | 73 ± 10 | 67 ± 14 | 73 ± 10 | 70 ± 9 |
| Women (%) | 35.1 | 51.3 | 33.8 | 26.3 |
| Clinical characteristics (% patients in the cohort) | ||||
| Arterial hypertension | 93.8 | 69.8 | 94.2 | 96.0 |
| Dyslipidemia | 76.2 | 46.3 | 76.1 | 89.1 |
| Chronic lung diseases | 22.1 | 10.4 | 23.1 | 16.3 |
| Depression | 14.4 | 11.2 | 13.4 | 10.3 |
| Heart failure | 13.3 | 1.4 | 12.5 | 10.9 |
| Chronic kidney diseases | 11.5 | 2.2 | 11.0 | 8.4 |
| Neoplasia | 9.2 | 5.9 | 9.8 | 7.7 |
| Atrial fibrillation | 9.2 | 1.2 | 7.9 | 5.2 |
| Severe liver diseases | 2.7 | 1.6 | 2.9 | 2.1 |
p Values for group comparisons <0.001 for all variables.
CAD, coronary artery disease; MI, myocardial infarction; PCI, percutaneous coronary intervention; SD, standard deviation; T2DM, type 2 diabetes mellitus.
Drug prescriptions during follow-up
Table 2 reports drug prescriptions during the 2-year follow-up. Panel A reports drugs recommended for the prevention of atherothrombotic events. In the T2DM patients with cardiovascular disease (cohorts #1, #3 and #4), the percentages of prescriptions of antithrombotic (mainly antiplatelet), lipid lowering (mainly statins), renin angiotensin system inhibitor (RASi) and beta-blocker therapy was 91–97%, 79–92%, 76–84% and 67–79%, respectively, during the first year of follow-up (Table 2). The patient cohort with chronic CAD and at least one PCI-related hospitalization in the previous 3 years (cohort #4) was the most extensively treated with all four types of agents (96.8%, 91.5%, 84.3% and 79.3%, respectively). In the above three cohorts, the percentage of prescriptions decreased in the second year of follow-up for all agents. Conversely, patients with T2DM but without known cardiovascular disease (cohort #2) had the lowest prescription rates: 50.2%, 50.4%, 62.2% and 28.5%, respectively, for the four types of agents, with similar prescription rates in the first and second year of follow-up. Panel B reports anti-diabetic drugs. In 2015 the most prescribed drugs were insulin or analogues, biguanides, and sulfonylureas. The rate of sodium-glucose cotransporter-2 (SGLT2) inhibitor use was very limited given the lack of NHS reimbursement at the time. Panel C reports the most frequent prescriptions of other drug classes. Proton pump inhibitors (PPIs) were the most prescribed non-cardiovascular drugs and diuretics the most prescribed cardiovascular drugs, with lowest prescription rates among T2DM patients without known cardiovascular disease (cohort #2) compared to the other patient cohorts.
Table 2.
Drug prescriptions during the 2-year follow-up in the four T2DM cohorts.
| Therapeutic subgroup | First follow-up year | Second follow-up year | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cohort #1 | Cohort #2 | Cohort #3 | Cohort #4 | Cohort #1 | Cohort #2 | Cohort #3 | Cohort #4 | |||||||||
| % Patients | Mean DDD/patient | % Patients | Mean DDD/patient | % Patients | Mean DDD/patient | % Patients | Mean DDD/patient | % Patients | Mean DDD/patient | % Patients | Mean DDD/patient | % Patients | Mean DDD/patient | % Patients | Mean DDD/patient | |
| Panel A | ||||||||||||||||
| Antithrombotic agents | 91.8 | 338.5 | 50.2 | 258.8 | 91.3 | 324.4 | 96.8 | 419.7 | 88.7 | 336.9 | 51.0 | 270.3 | 88.6 | 325.0 | 95.6 | 385.4 |
| Lipid-lowering agents | 79.2 | 418.5 | 50.4 | 258.5 | 78.9 | 386.0 | 91.5 | 474.7 | 75.5 | 443.9 | 50.6 | 274.4 | 75.9 | 409.9 | 90.1 | 491.8 |
| RASi | 76.4 | 453.6 | 62.2 | 414.9 | 76.1 | 461.9 | 84.3 | 486.1 | 71.3 | 477.0 | 61.6 | 427.6 | 71.8 | 477.8 | 81.3 | 503.9 |
| Beta-blockers | 67.3 | 132.6 | 28.5 | 177.9 | 67.4 | 138.7 | 79.3 | 138.5 | 65.0 | 138.6 | 29.7 | 178.1 | 65.7 | 144.8 | 78.9 | 142.7 |
| Panel B | ||||||||||||||||
| Insulins and analogues | 34.6 | 305.8 | 18.6 | 302.8 | 32.8 | 319.4 | 32.1 | 331.5 | 33.7 | 324.8 | 19.6 | 325.5 | 32.5 | 331.7 | 33.4 | 348.6 |
| Biguanides | 50.3 | 205.3 | 60.4 | 206.5 | 51.8 | 211.9 | 59.1 | 232.1 | 44.6 | 212.9 | 55.9 | 214.2 | 46.6 | 216.4 | 54.3 | 230.4 |
| Sulfonylureas | 14.5 | 302.6 | 16.8 | 332.1 | 14.7 | 309.6 | 17.7 | 332.2 | 12.4 | 325.1 | 15.6 | 340.2 | 13.1 | 327.3 | 15.4 | 347.0 |
| Combinations of oral glucose-lowering drugs | 12.8 | 256.4 | 15.7 | 277.9 | 13.5 | 262.8 | 15.9 | 274.0 | 11.2 | 267.7 | 15.2 | 275.5 | 12.1 | 267.7 | 15.7 | 279.8 |
| Alpha glucosidase inhibitors | 4.2 | 96.9 | 3.7 | 104.3 | 4.2 | 99.1 | 4.4 | 106.1 | 3.6 | 118.9 | 3.3 | 119.3 | 3.6 | 118.8 | 4.1 | 128.5 |
| Thiazolidinediones | 1.0 | 202.8 | 1.7 | 233.7 | 1.0 | 212.1 | 1.0 | 194.7 | 0.7 | 220.0 | 1.5 | 239.7 | 0.8 | 220.9 | 0.7 | 244.5 |
| Dipeptidyl peptidase 4 (DPP-4) inhibitors | 6.0 | 204.7 | 4.8 | 225.4 | 6.1 | 205.2 | 6.3 | 216.1 | 6.6 | 233.5 | 5.3 | 242.4 | 6.6 | 233.1 | 7.1 | 224.7 |
| Glucagon-like peptide-1 (GLP-1) analogues | 1.1 | 249.8 | 1.6 | 274.5 | 1.3 | 255.2 | 1.1 | 252.1 | 1.4 | 271.0 | 2.0 | 279.2 | 1.6 | 269.5 | 1.9 | 237.9 |
| Sodium-glucose cotransporter 2 (SGLT2) inhibitors | 0.5 | 25.2 | 0.5 | 41.6 | 0.5 | 27.0 | 0.6 | 17.3 | 1.3 | 114.4 | 1.3 | 119.8 | 1.4 | 107.3 | 2.0 | 112.7 |
| Panel C | ||||||||||||||||
| PPIs | 86.1 | 206.4 | 54.3 | 159.7 | 85.4 | 208.1 | 91.5 | 217.9 | 79.9 | 220.6 | 51.7 | 173.0 | 79.7 | 218.8 | 87.0 | 224.0 |
| Antibacterial drugs for systemic use | 65.8 | 24.6 | 57.9 | 21.5 | 67.0 | 24.9 | 66.3 | 22.4 | 61.4 | 24.7 | 56.6 | 21.7 | 63.0 | 24.7 | 62.7 | 23.9 |
| Diuretics | 53.3 | 364.3 | 23.1 | 220.4 | 52.4 | 377.6 | 45.8 | 318.6 | 50.5 | 399.9 | 23.9 | 240.3 | 50.1 | 402.7 | 45.4 | 350.4 |
| NSAIDs | 44.9 | 49.3 | 49.2 | 54.7 | 46.8 | 50.8 | 45.8 | 44.6 | 40.9 | 48.0 | 46.8 | 53.4 | 43.2 | 49.7 | 43.3 | 42.9 |
Panel A, recommended drugs for secondary prevention; Panel B, drugs prescribed for type 2 diabetes mellitus (T2DM); Panel C, other most prescribed drugs.
DDD, defined daily dose; NSAIDs, non-steroidal anti-inflammatory drugs; PPIs, proton pump inhibitors; RASi, renin angiotensin system inhibitor.
Hospitalizations during the 2-year follow-up
Hospitalization rates were similar among the three T2DM patient cohorts with CAD. They were elevated during the first year of follow-up, with 50.5% of patients of cohort #1, 45.8% of cohort #3 and 55.0% of cohort #4 being hospitalized at least once; hospitalization rates dropped to about 30% in the second year. In contrast, among T2DM patients without CAD or stroke diagnosis (cohort #2), hospitalization rates were approximately one-third of those in other cohorts, with 13.4% admitted to hospital at least once in the first year and 13.8% in the second year.
The five most important reasons for hospitalization in all cohorts are reported in Table 3. During the first follow-up year, admissions were mostly related to ACS and heart failure in cohort #1, non-ACS CAD and heart failure in cohort #3, and any CAD (both ACS and CCS) in cohort #4. In cohort #2, instead, lung diseases and diabetes were the most frequent causes of admissions. The mean length of hospital stay in each cohort ranged from 8 to 14 days.
Table 3.
Five most important reasons for hospitalization during follow-up.
| Cause of hospitalization | Cohort #1 (n=33,153) | Cohort #2 (n=407,932) | Cohort #3 (n=19,787) | Cohort #4 (n=2166) | ||||
|---|---|---|---|---|---|---|---|---|
| First year % | Second year % | First year % | Second year % | First year % | Second year % | First year % | Second year % | |
| ACS | 7.0 | 1.7 | – | 0.4 | 2.8 | 1.3 | 12.6 | 3.8 |
| Heart failure | 6.4 | 4.0 | 0.6 | 0.7 | 6.4 | 3.9 | 5.2 | 3.3 |
| CCS | 7.7 | 2.6 | – | – | 8.9 | 2.6 | 27.1 | 7.2 |
| Cerebrovascular diseases | 4.1 | – | – | – | – | – | – | – |
| Arrhythmias | – | 1.2 | 0.4 | – | 1.7 | 1.2 | 1.8 | – |
| Lung diseases | 3.5 | 2.8 | 0.7 | 0.9 | 4.0 | 3.0 | 1.7 | 1.9 |
| Diabetes mellitus | – | – | 0.7 | 0.5 | – | – | – | 1.4 |
| Femoral neck fractures | – | – | 0.4 | 0.4 | – | – | – | – |
ACS, acute coronary syndrome; CCS, chronic coronary syndrome.
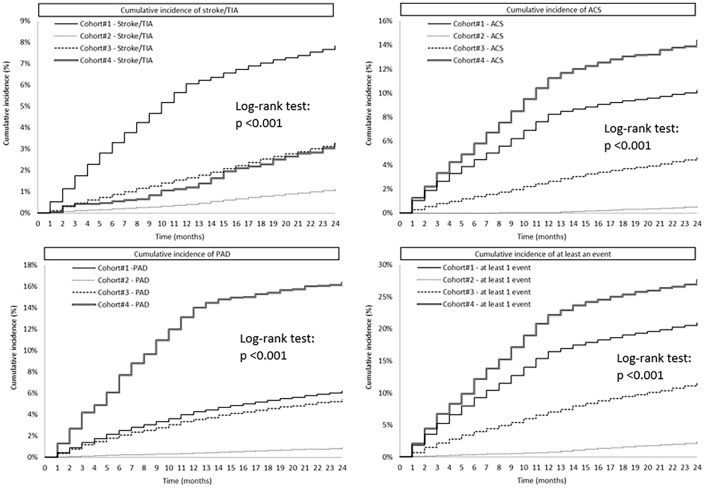
The cumulative incidence curves of hospitalizations for stroke/TIA or ACS or PAD, or any of these three reasons, respectively, are reported in Figure 2. Comparison of the time trends yielded significant differences among all cohorts (p < 0.01), except between cohorts #3 and #4 concerning stroke/TIA. Patients with T2DM but without CAD or stroke diagnosis (cohort #2) had the lowest admission rates for any one of these reasons. The cohort with CAD and/or stroke (#1) had the highest admission rates for stroke/TIA. The cohort with chronic CAD, no prior acute event, and at least one PCI in the previous 3 years (#4) had the highest rates of hospital admissions for any of the analyzed events considered as a whole.
Figure 2.
Kaplan–Meier curves showing the probability (cumulative monthly incidence as percentage of subjects at risk) of hospitalizations due to stroke/transient ischemic attack (TIA) or acute coronary syndrome (ACS) or peripheral artery disease (PAD) or at least one of these events during the 2-year follow-up for each of the four cohorts.
Cost per patient per year
Table 4 reports the integrated yearly NHS costs per patient in the different cohorts. Cohort #2 patients generated the lowest costs, with drugs being the most important determinant. Yearly patient costs were approximately three-fold higher in the other three cohorts, with hospitalizations representing the most important driver.
Table 4.
Integrated costs per patient in the first year of follow-up.
| Administrative flow | Cohort #1 | Cohort #2 | Cohort #3 | Cohort #4 | ||||
|---|---|---|---|---|---|---|---|---|
| Average cost per patient (n=33,153) (€) | % of total cost | Average cost per patient (n=407,932) (€) | % of total cost | Average cost per patient (n=19,787) (€) | % of total cost | Average cost per patient (n=2166) (€) | % of total cost | |
| Total drugs | 1624 | 24.6 | 1037 | 48.8 | 1677 | 28.7 | 1790 | 23.6 |
| Antidiabetic drugs | 289 | 4.4 | 233 | 11.0 | 301 | 5.2 | 321 | 4.2 |
| Cardiovascular | 635 | 9.6 | 272 | 12.8 | 622 | 10.7 | 789 | 10.4 |
| Non-cardiovascular | 700 | 10.6 | 531 | 25.0 | 754 | 12.9 | 680 | 9.0 |
| Hospitalizations | 3991 | 60.6 | 660 | 31.1 | 3230 | 54.4 | 4925 | 65.0 |
| Specialty visits | 978 | 14.8 | 427 | 20.1 | 924 | 15.9 | 865 | 11.4 |
| Total | 6,593 | 100.0 | 2,122 | 100.0 | 5,831 | 100.0 | 7,579 | 100.0 |
p < 0.001 for all total cost comparisons.
Discussion
The main findings of the present ReS database analysis can be summarized as follows. The prevalence of T2DM in a large 2015 sample of over 7 million Italian people was 6%. Approximately one in 13 of these diabetes patients (7.5%) had documented CAD and/or stroke in the previous 3 years. T2DM patients with CAD and/or stroke were generally older, more often male, with more comorbidities and more guideline-recommended prescriptions 12 compared to T2DM patients without documented CAD or stroke. Guideline-recommended treatment was not always optimal, as the prescription rate of several drug classes was below the 80% cut-off, typically used to define adherence, even among those with documented CAD or stroke. T2DM patients with CAD or prior stroke underwent at least one hospital admission during the first year of follow-up in over 50% of cases, versus only 13.4% of those without documented cardio-cerebrovascular disease, with more than three-fold higher yearly costs per patient. The main drivers of costs were hospitalizations for the T2DM cohorts with cardiovascular events versus drug-related costs for T2DM subjects without these events. The highest rates of new hospitalized cardiovascular events during the 2-year follow-up were associated with chronic CAD patients who had no history of acute events but underwent PCI in the previous 3 years.
Prevalence and patient characteristics
The prevalence of T2DM in our analysis (6%) is in line with that reported by the International Diabetes Federation (IDF) for Europe (6.3%). 1 The IDF also estimates that the prevalence of T2DM in Europe will increase in the next two decades by nearly 20%. 1 Although all T2DM complications are relevant in terms of quality of life and outcomes, cardiovascular diseases and, more specifically, coronary and cerebrovascular events are the most significant causes of morbidity and mortality in T2DM patients.13–15 In the ReS database, 7.5% of the overall T2DM population had documented CAD and/or stroke during the previous 3 years (from 2013 to 2015). This percentage is lower than the 15% described by the IDF for cardiovascular diseases in Europe. 1 The difference can be explained by the fact that our evaluation was limited to a relatively brief period of time of 3 years. In addition, carotid artery disease unrelated to stroke and other peripheral artery diseases were not considered in our characterization of the four T2DM cohorts. The contributing role for atherothrombotic events of hypertension and dyslipidemia, more frequently recorded in the T2DM cohorts with documented CAD or stroke, is well described in the current international literature.16–20
As a consequence of CAD, and as a possible cause of stroke, T2DM patients with CAD or stroke in their recent history presented more often with heart failure and atrial fibrillation compared to those without CAD or stroke in their recent clinical history, confirming the well-known association of CAD and stroke with heart failure and atrial fibrillation. Both cardiac conditions can further worsen the quality of life of T2DM patients, while also increasing their morbidity and mortality.21–24 In the T2DM cohorts with prior CAD or stroke, the use of recommended drugs for secondary prevention seemed reasonably adherent to guidelines, but still suboptimal (i.e. <80%): excepting the cohort with recent PCI in whom prescription rates were higher; there appears to be room for improvement in lipid lowering, RASi and maintenance of prescription levels over time. More intensive guideline implementation programmes are probably also necessary for T2DM patients without prior cardiovascular events whose prescriptions of recommended therapies, such as lipid lowering, seemed far from optimal, reaching only approximately 50% of this population.
Clinical outcomes
The need for hospital admission during follow-up was nearly four times more frequent in T2DM patients with CAD and/or prior stroke (cohort #1) than in those without these events. This finding confirms the observation by others1,5,25,26 showing, in different settings, the relevant health burden of T2DM when complicated by a cardiovascular event. The higher rate of events occurring in the first year of follow-up can be explained by the hospitalization criterion used to assign patients to the different cohorts. After a hospitalized event, the likelihood of an early recurrent hospitalization has been demonstrated to be more frequent. 27 As expected, the rate of hospital admissions for stroke was more frequent in the cohort of T2DM patients with a previous cerebrovascular event. However, the most frequent causes of hospitalization were cardiac ones, specifically acute or chronic coronary diseases, and the highest risk of new hospitalized events was in those with chronic CAD and PCI in the previous 3 years (cohort #4). There is limited contemporary population-based data on this group of T2DM patients. 28
A single recent large trial enrolled T2DM patients with chronic CAD but no previous MI or stroke; the presence of chronic CAD was determined by previous PCI or coronary artery bypass or by a documented stenosis of at least 50% in at least one epicardial artery,29,30 resulting in a population quite similar to our cohort #4. Over a median of 3.3 years, long-term treatment with ticagrelor in association with aspirin reduced the relative occurrence of atherothrombotic events by 10% with respect to aspirin alone (from 8.5% to 7.7%), but at the cost of an increased rate of major bleeds (from 1.0% to 2.2%). 29 In a prespecified subgroup who had undergone PCI, but not in those who had not undergone PCI, the net clinical benefit was improved by long-term ticagrelor. 30 In T2DM patients with chronic coronary or peripheral artery disease (62% with previous MI), a prespecified subgroup analysis of another large trial showed a relevant absolute reduction of cardiovascular death, non-fatal MI or stroke (from 6.9% to 5.2%) by adding a low dose of a direct oral anticoagulant to aspirin over 3 years, with a non-significantly different rate of major bleeding as in the non-diabetic treated population (3.2% versus 3.1% over 3 years in diabetes versus non-diabetes patients), compared to aspirin alone. 31 Similar subgroup results by diabetes status have been reported for a large trial testing ticagrelor 60 mg twice daily plus aspirin versus aspirin alone. 32 The results of the above trials, indicating anti-ischemic effects of more aggressive antithrombotic therapy counterbalanced by enhanced risk of major bleeds, stress the importance of preferentially treating patients at very high risk of cardiovascular events. Cardiac rehabilitation has been shown to be another effective option to prevent recurrent atherothrombotic events in patients with T2DM and prior cardiovascular events. 33 Our data indicate that, for all T2DM patients, persistent use of guideline-recommended drugs at the appropriate doses warrants attention.
Strengths and limitations
Some advantages of using administrative data include the breadth of coverage of the population, as well as the ability to evaluate long-term follow-up of prescriptions, outpatient visits and hospitalizations. Administrative records additionally provide important information on routine management of ‘real-life’ patients. Although procedures and/or prescriptions performed outside the NHS coverage were not available, the rate of out-of-pocket services in patients with chronic diseases in Italy is limited. 34 The data were analyzed in a large but limited sample of individuals; the analyzed sample, however, accurately reflected the whole of Italy in terms of demographic characteristics (Supplemental Figure 1).
As in all administrative datasets, the limited type and number of clinical variables precluded a detailed stratification of disease severity; specifically, blood hemoglobin A1c (HbA1c) levels, duration of T2DM, reasons for non-use or discontinuation of recommended drugs were not available. This information would have been useful to define more precisely the true rate of undertreatment. Subjects in the early stages of T2DM, requiring no pharmacotherapy or hospitalization but only diet and lifestyle changes, as well as non-diabetes individuals with similar cardiovascular comorbid characteristics, were not included. These limitations preclude the possibility to assess the generalizability of our conclusions to the whole population of patients with diabetes mellitus, including non-pharmacologically treated patients. The focus of our analysis, however, was on the population of diabetes patients producing the highest clinical/economic burden to the NHS. Because out-of-hospital mortality could not be evaluated from the present data flows, the competitive risk of death for hospitalizations could not be assessed. Finally, patients were characterized by cardiovascular events during the previous 3 years; therefore, the number of patients with an event occurring more than 3 years before inclusion is unknown.
Conclusions
The present study, based on Italian NHS records from a large representative population, provides a contemporary snapshot of patients with T2DM in real-life clinical practice. The risk profile of T2DM patients in general, and particularly of those with cardiovascular comorbidities, has relevant clinical implications. T2DM patients with a prior cardiovascular event warrant close follow-up and care, given the elevated risk of new events and escalating costs for the NHS. On the other hand, up to 50% of T2DM patients without a prior cardiovascular event may be suboptimally treated with drugs recommended by current guidelines; such patients would likely benefit from referral to prevention programmes to improve their adherence to guideline-recommended therapies. Finally, patients with chronic CAD who have undergone a coronary revascularization procedure in the previous 3 years have an unexpectedly high risk of new events, warranting specific studies aimed at defining more effective preventive strategies. Improved management of all T2DM patients described in our analysis could have relevant cost-saving implications for the NHS.
Supplemental Material
Supplemental material, sj-pdf-1-taj-10.1177_20406223211026390 for Prevalence, prescriptions, outcomes and costs of type 2 diabetes patients with or without prior coronary artery disease or stroke: a longitudinal 5-year claims-data analysis of over 7 million inhabitants by Aldo Pietro Maggioni, Letizia Dondi, Felicita Andreotti, Giulia Ronconi, Silvia Calabria, Carlo Piccinni, Antonella Pedrini, Imma Esposito and Nello Martini in Therapeutic Advances in Chronic Disease
Footnotes
Authors’ note: All authors take full responsibility for the reliability and freedom from bias of all aspects of the presented data and their discussed interpretation.
Authors’ contributions: Each author has approved the submitted version and has agreed to be personally accountable for the author’s own contribution and to questions related to the accuracy and integrity of the entire work.
Conflict of interest statement: APM received fees from Astra Zeneca, Bayer, Novartis, Fresenius for participation in study committees, outside the present work. FA reports speaker/consultancy fees from Amgen, Bayer, BMS/Pfizer and Daiichi Sankyo, outside the present work. LD, GR, SC, CP, AP, IE and NM have no conflicts of interest to disclose.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was partially supported by an unconditional grant from Astra Zeneca. Astra Zeneca was not involved in data collection, analysis, interpretation, and writing of the report, nor in the decision to submit the article for publication.
Data availability: The datasets contributing to the current study are not publicly available, as they are anonymized administrative databases owned by the Italian regional and local health facilities; the Fondazione ReS has analyzed them under specific agreements.
ORCID iDs: Aldo Pietro Maggioni  https://orcid.org/0000-0003-2764-6779
https://orcid.org/0000-0003-2764-6779
Carlo Piccinni  https://orcid.org/0000-0002-8648-8961
https://orcid.org/0000-0002-8648-8961
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Aldo Pietro Maggioni, Fondazione Ricerca e Salute (ReS), Rome, Italy ANMCO Research Center, Fondazione per il Tuo cuore – HCF onlus, Via La Marmora 34, Florence, 50121, Italy.
Letizia Dondi, Fondazione Ricerca e Salute (ReS), Rome, Italy.
Felicita Andreotti, Fondazione Policlinico Universitario A. Gemelli IRCCS, Rome, Italy.
Giulia Ronconi, Fondazione Ricerca e Salute (ReS), Rome, Italy.
Silvia Calabria, Fondazione Ricerca e Salute (ReS), Rome, Italy.
Carlo Piccinni, Fondazione Ricerca e Salute (ReS), Rome, Italy.
Antonella Pedrini, Fondazione Ricerca e Salute (ReS), Rome, Italy.
Imma Esposito, Fondazione Ricerca e Salute (ReS), Rome, Italy.
Nello Martini, Fondazione Ricerca e Salute (ReS), Rome, Italy.
References
- 1. International Diabetes Federation. IDF diabetes atlas, 9th ed. https://www.diabetesatlas.org/en/ (2019, accessed June 17, 2020).
- 2. King H, Aubert RE, Herman WH. Global burden of diabetes, 1995–2025: prevalence, numerical estimates, and projections. Diabetes Care 1998; 21: 1414–1431. [DOI] [PubMed] [Google Scholar]
- 3. Nickerson HD, Dutta S. Diabetic complications: current challenges and opportunities. J Cardiovasc Transl Res 2012; 5: 375–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Natali A, Vichi S, Landi P, et al. Coronary atherosclerosis in type II diabetes: angiographic findings and clinical outcome. Diabetologia 2000; 43: 632–641. [DOI] [PubMed] [Google Scholar]
- 5. Nelson AJ, Peterson ED, Pagidipati NJ. Atherosclerotic cardiovascular disease and heart failure: determinants of risk and outcomes in patients with diabetes. Prog Cardiovasc Dis 2019; 62: 306–314. [DOI] [PubMed] [Google Scholar]
- 6. Cosentino F, Grant PJ, Aboyans V, et al. 2019 ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J 2020; 41: 255–323. [DOI] [PubMed] [Google Scholar]
- 7. Kim D, Lee SH, Joon Kim B, et al.; Korean Stroke Registry Investigators. Secondary prevention by stroke subtype: a nationwide follow-up study in 46,108 patients after acute ischemic stroke. Eur Heart J 2013; 34: 2760–2767. [DOI] [PubMed] [Google Scholar]
- 8. Gyberg V, Kotseva K, Dallongeville J, et al.; EUROASPIRE Study Group. Does pharmacologic treatment in patients with established coronary artery disease and diabetes fulfil guideline recommended targets? A report from the EUROASPIRE III cross-sectional study. Eur J Prev Cardiol 2015; 22: 753–761. [DOI] [PubMed] [Google Scholar]
- 9. Andrikopoulos G, Tzeis S, Nikas N, et al. Short-term outcome and attainment of secondary prevention goals in patients with acute coronary syndrome – results from the countrywide TARGET study. Int J Cardiol 2013; 168: 922–927. [DOI] [PubMed] [Google Scholar]
- 10. Maggioni AP, Dondi L, Pedrini A, et al. The use of antiplatelet agents after an acute coronary syndrome in a large community Italian setting of more than 12 million subjects. Eur Heart J Acute Cardiovasc Care 2019; 8: 527–535. [DOI] [PubMed] [Google Scholar]
- 11. Cimminiello C, Dondi L, Pedrini A, et al. Patterns of treatment with antiplatelet therapy after an acute coronary syndrome: data from a large database in a community setting. Eur J Prev Cardiol 2019; 26: 836–846. [DOI] [PubMed] [Google Scholar]
- 12. Arnold SV, Bhatt DL, Barsness GW, et al. Clinical management of stable coronary artery disease in patients with type 2 diabetes mellitus: a scientific statement from the American Heart Association. Circulation 2020; 141: e779–e806. [DOI] [PubMed] [Google Scholar]
- 13. Vijan S. Type 2 diabetes [published correction appears in Ann Intern Med 2020; 172: 708]. Ann Intern Med 2019; 171: ITC65–ITC80. [DOI] [PubMed] [Google Scholar]
- 14. Cavender MA, Steg PG, Smith SC, Jr, et al.; on behalf of the REACH Registry Investigators. Impact of diabetes mellitus on hospitalization for heart failure, cardiovascular events, and death: outcomes at 4 years from the Reduction of Atherothrombosis for Continued Health (REACH) Registry. Circulation 2015; 132: 923–931. [DOI] [PubMed] [Google Scholar]
- 15. Low Wang CC, Hess CN, Hiatt WR, et al. Clinical update: cardiovascular disease in diabetes mellitus atherosclerotic cardiovascular disease and heart failure in type 2 diabetes mellitus – mechanisms, management, and clinical considerations. Circulation 2016; 133: 2459–2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wang CC, Reusch JE. Diabetes and cardiovascular disease: changing the focus from glycemic control to improving longterm survival. Am J Cardiol 2012; 110(9 Suppl.): 58B–68B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study Group. BMJ 1998; 317: 703–713. [PMC free article] [PubMed] [Google Scholar]
- 18. Parhofer KG. Interaction between glucose and lipid metabolism: more than diabetic dyslipidemia. Diabetes Metab J 2015; 39: 353–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wu L, Parhofer KG. Diabetic dyslipidemia. Metabolism 2014; 63: 1469–1479. [DOI] [PubMed] [Google Scholar]
- 20. Nichols GA, Hillier TA, Erbey JR, et al. Congestive heart failure in type 2 diabetes: prevalence, incidence, and risk factors. Diabetes Care 2001; 24: 1614–1619. [DOI] [PubMed] [Google Scholar]
- 21. Dei Cas A, Khan SS, Butler J, et al. Impact of diabetes on epidemiology, treatment, and outcomes of patients with heart failure. JACC Heart Fail 2015; 3: 136–145. [DOI] [PubMed] [Google Scholar]
- 22. Movahed MR, Hashemzadeh M, Jamal MM. Diabetes mellitus is a strong, independent risk for atrial fibrillation and flutter in addition to other cardiovascular disease. Int J Cardiol 2005; 105: 315–318. [DOI] [PubMed] [Google Scholar]
- 23. Dublin S, Glazer NL, Smith NL, et al. Diabetes mellitus, glycemic control, and risk of atrial fibrillation. J Gen Intern Med 2010; 25: 853–858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Erdmann E, Dormandy JA, Charbonnel B, et al.; PROactive Investigators. The effect of pioglitazone on recurrent myocardial infarction in 2,445 patients with type 2 diabetes and previous myocardial infarction: results from the PROactive (PROactive 05) study. J Am Coll Cardiol 2007; 49: 1772–1780. [DOI] [PubMed] [Google Scholar]
- 25. Strandberg TE, Pitkala KH, Berglind S, et al. Multifactorial intervention to prevent recurrent cardiovascular events in patients 75 years or older: the Drugs and Evidence-Based Medicine in the Elderly (DEBATE) study: a randomized, controlled trial. Am Heart J 2006; 152: 585–592. [DOI] [PubMed] [Google Scholar]
- 26. Giorda CB, Avogaro A, Maggini M, et al.; Diabetes and Informatics Study Group. Recurrence of cardiovascular events in patients with type 2 diabetes: epidemiology and risk factors. Diabetes Care 2008; 31: 2154–2159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Krumholz HM, Hsieh A, Dreyer RP, et al. Trajectories of risk for specific readmission diagnoses after hospitalization for heart failure, acute myocardial infarction, or pneumonia. PLoS One 2016; 11: e0160492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jernberg T, Lindholm D, Hasvold LP, et al. Impact of ischemic heart disease severity and age on risk of cardiovascular outcome in diabetes patients in Sweden: a nationwide observational study. BMJ Open 2019. 9: e027199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Steg PG, Bhatt DL, Simon T, et al.; THEMIS Steering Committee and Investigators. Ticagrelor in patients with stable coronary disease and diabetes. N Engl J Med 2019; 381: 1309–1320. [DOI] [PubMed] [Google Scholar]
- 30. Bhatt DL, Steg PG, Mehta SR, et al. Ticagrelor in patients with diabetes and stable coronary artery disease with a history of previous percutaneous coronary intervention (THEMIS-PCI): a phase 3, placebo-controlled, randomised trial. Lancet 2019; 394: 1169–1180. [DOI] [PubMed] [Google Scholar]
- 31. Bhatt DL, Eikelboom JW, Connolly SJ, et al. Role of combination antiplatelet and anticoagulation therapy in diabetes mellitus and cardiovascular disease: insights from the COMPASS trial. Circulation 2020; 141: 1841–1854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bhatt DL, Bonaca MP, Bansilal S, et al. Reduction in ischemic events with ticagrelor in diabetic patients with prior myocardial infarction in PEGASUS-TIMI 54. J Am Coll Cardiol 2016; 67: 2732–2740. [DOI] [PubMed] [Google Scholar]
- 33. Armstrong MJ, Sigal RJ, Arena R, et al. Cardiac rehabilitation completion is associated with reduced mortality in patients with diabetes and coronary artery disease. Diabetologia 2015; 58: 691–698. [DOI] [PubMed] [Google Scholar]
- 34. Gini R, Schuemie MJ, Francesconi P, et al. Can Italian healthcare administrative databases be used to compare regions with respect to compliance with standards of care for chronic disease? PLoS One 2014; 9: e95419. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-taj-10.1177_20406223211026390 for Prevalence, prescriptions, outcomes and costs of type 2 diabetes patients with or without prior coronary artery disease or stroke: a longitudinal 5-year claims-data analysis of over 7 million inhabitants by Aldo Pietro Maggioni, Letizia Dondi, Felicita Andreotti, Giulia Ronconi, Silvia Calabria, Carlo Piccinni, Antonella Pedrini, Imma Esposito and Nello Martini in Therapeutic Advances in Chronic Disease