Supplemental Digital Content is available in the text
Keywords: deaths of despair, healthcare workers, occupational health, opioids, suicide
Objective:
To explore mortality rates and trends according to the occupation of healthcare workers who died from the deaths of despair (DoD).
Methods:
Death certificates for deaths from 2011 to 2015 due to poisonings, suicides, alcholic liver disease and cirrhosis were collected and coded based on the decedent's occupation. Mortality rates and rate ratios were calculated according to occupations for healthcare workers.
Results:
There were 540 DoDs among Massachusetts healthcare workers, accounting for an average annual rate of 32.4 deaths per 100,000 workers. The highest mortality rate for DoDs were among medical assistants; nursing, psychiatric, and home health aides; miscellaneous; health technologists and technicians; emergency medical technicians, and paramedics.
Conclusions:
Further research should examine factors contributing to elevated rates for DoDs among healthcare workers. Interventions targeted for these workers should be developed.
Learning Objectives
Discuss previous findings related to "deaths of despair," including reasons for concern among healthcare workers (HCWs).
Summarize the findings of the new analysis of deaths of despair among Massachusetts HCWs, including job categories associated with higher risk.
Identify additional factors that may lead to an increased risk of deaths of despair among HCWs.
Life expectancy in the United States has generally been decreasing since 2015.1–4 At the same time that these decreases in life expectancy have been occurring, there have been drastic increases in mortality among middle-aged white, non-Hispanics in the United States, which contrasts with generally declining mortality among other racial and ethnic groups in the United States and among those in other countries.5,6 Increasingly research has revealed that midlife mortality is also increasing among American Indians and Alaska Natives, blacks, and Asian, and Pacific Islanders.7 Additionally previous decreases in mortality among Hispanics, Blacks, Asians, and Pacific Islanders ended between 2009 and 2011.7 Midlife deaths of despair have been increasing among these other racial and ethnic groups as well. Much of this increase has been attributable to deaths of despair: drug overdoses (especially opioids), suicides, and alcohol-related liver disease. Deaths from these cases have been disproportionately affecting people with lower education levels,6 suggesting that socioeconomic factors may be playing an important role in these trends.
Exposures related to work and employment may play a large role in determining trends of deaths of despair. For example, Gutin and Hummer8 found that adults not in the labor force had two times the risk of suicide and almost seven times the risk of accidental poisoning risk compared with administrative professional workers. Furthermore, Hawkins et al9 showed that blue collar workers, specifically workers employed in construction and farming, fishing, and forestry occupations, are at a higher risk for death by despair compared with other occupations. These occupational factors may be contributing to the educational disparities described above, because workers with lower educational attainment may be less likely to be in the labor force and/or more likely to be employed in jobs with an elevated risk for deaths of despair.
Previous research exploring the effects of deaths of despair, especially opioid overdoses, on specific occupations has primarily focused on occupations such as construction workers and agriculture fishing workers, who have been shown to have very high mortality rates.10,11 Healthcare workers have not received as much attention. This lack of attention may be due to the fact that, the healthcare industry is extremely diverse with workers from a variety of socioeconomic, racial, and ethnic backgrounds. This diversity may be a challenge for generating interventions meant to prevent deaths of despair among these workers.12,13 However, healthcare workers deserve attention with respect to the deaths of despair. Healthcare workers comprise a large proportion of all workers.13 Furthermore, employment in the healthcare industry is also projected to grow substantially over the next decade.14
Additionally, there are reasons to suspect that healthcare workers may be at an elevated risk for the deaths of despair as well. One study using Massachusetts data from 2011 to 2015 found that healthcare support workers had elevated rates for all categories of deaths of despair and that they had a 7.2% average annual increase in deaths of despair whereas all workers only had a 5.8% increase.9 Another study from Colorado found that the age-adjusted suicide mortality rate among male healthcare practitioners and technicians was 424.1 per 100,000 workers, which was the third highest rate.15 The study also found that healthcare practitioners and technicians had the highest rate of suicide by poisoning at 14.25 per 100,000 workers.15 These elevated rates may be due to the fact that medical professions have easier access to prescription medicine with which to overdose.16 This potential mechanism is supported by a study, which found that physicians used drugs in 57% of suicides whereas the general population used drugs in 26.6% of suicides.17
Occupational injuries may be another factor that contributes to elevated rates of deaths of despair. Healthcare workers are at an increased risk for occupational injuries. The 2018 Bureau of Labor Statistics (BLS) Survey of Occupational Injuries and Illnesses (SOII) showed workers in the healthcare and social assistance industry had the highest rate of nonfatal occupational injuries and illnesses.18 There are a number of factors that may contribute to high injury rates among healthcare workers. The most common sources of injuries among healthcare workers include overexertion, falls, and violent injuries.19 In addition, there is evidence that some of these sources of injuries such as violence may be increasing.20 High physical injury rates may also be compounded by a number of psychosocial stressors and poor working conditions among healthcare workers.21 These injuries and other pain caused by work in healthcare may increase the risk of dying from certain deaths of despair. Kowalski-McGraw et al22 suggested that musculoskeletal disorders (MSDs) caused by completing activities with high ergonomic demands and occupational injuries may be associated with opioids misuse due to the fact that opioids can be used to mitigate pain and therefore make it easier to work. This suggestion is supported by a study using data from Utah, which found that 57% of those who died from opioids had suffered a workplace injury at some point in their lives. A study analyzing worker's compensation data for over 100,000 injured workers in New Mexico found that lost-time injuries were strongly associated with deaths related to drugs and suicide in men and women.23 Another study found similar findings in West Virgina.24 A recent study conducted among home care workers showed that 54.2% of these workers have currently elevated or chronic pain and 4.8% of workers reported prescription opioid use.25 The paper also concludes that financial hardships, injuries, and anxiety were associated with increased risk for opioid misuse.25 Further research has found that occupations with higher injury rates also tend to have higher mortality rates from opioids and other deaths of despair.26,27
Because previous research has suggested that healthcare workers may be at an elevated risk for deaths of despair, this study sought to determine whether workers in certain healthcare occupations have elevated rates of deaths of despair. In addition to this, we also sought to determine whether there is an association between healthcare occupations’ occupational injuries rates and mortality rates due to the deaths of despair.
METHODS
The method used to collect the data for this study have been previously described in detail.9 Data from death certificates for which the International Classification of Diseases-10 code for cause indicated either unintentional or undetermined poisoning, suicide, or alcoholic liver disease and cirrhosis were collected for deaths occurring in Massachusetts from 2011 to 2015 from the MA Registry of Vital Records. Opioid-related deaths were identified based on additional cause of death fields having a code indicative an opioid-related death. Because the unintentional/undetermined poisonings, suicides, or alcoholic liver disease and cirrhosis deaths were identified using the main cause of death field, opioid deaths could fall into the undetermined or unintentional poisonings, suicides, or alcoholic liver categories as well. However, most opioid-related deaths were unintentional or undetermined poisonings.
Occupations were coded to detailed census occupations using the National Institute for Occupational Safety and Health (NIOSH) Industry and Occupation Computerized Coding System (NIOCCS). Using free text occupation and industry information from death certificates, NIOCCS will automatically code industry and occupation titles to census industry and occupation codes. Following automatic coding, occupations that were not automatically coded were reviewed and manually coded if enough data were available.
Deaths included in this study were restricted to MA residents between the ages of 16 and 64 who had information on their death certificate that indicated that they were working in healthcare support or health care practitioners and technical occupations.
Demographic data representing the MA population was obtained from the American Community Survey (ACS) Public Use Micro Dataset (PUMS) for the years 2011 to 2015. We generated denominators representing MA residents according to age groups (16 to 24, 25 to 34, 35 to 44, 45 to 54, and 55 to 64), sex (male, female), race/ethnicity (white, non-Hispanic; black, non-Hispanic; Asian, non-Hispanic; Hispanics of all races; and all others), educational level (high school education or less; some college), and detailed healthcare occupation.
Analysis
For all occupations, we calculated the number of deaths of despair and mortality rates for deaths of despair. We performed the same calculations for individual categories of deaths of despair (poisonings, suicides, alcoholic liver disease and cirrhosis, and opioid-related deaths). For each occupation category, we used generalized linear mixed models in SAS Version 9.3 (SAS Institute, Inc., Cary, NC) to calculate mortality rate ratios (RRs) comparing the mortality rates for all deaths of despair and the individual categories of deaths of despair. For these models, we assumed a Poisson distribution with a log link and modeled the count of deaths with the log of the number of workers employed in the occupations treated as an offset. For each occupation, all other workers were treated as the reference group.
Previous research has suggested demographic factors may affect occupational differences in rates of deaths of despair.5,6 Therefore, we explored the number, percent, and rate of deaths of despair according to age group, sex, race/ethnicity, and education. Controlling for these factors is also important because of the diversity of healthcare workers with respect to these demographic factors.12,13 Additionally, for all deaths of despair, we explored how controlling for these demographic factors impacted the mortality RRs for healthcare occupations. The models used to calculate these mortality RRs had the same components as those described above, but we constructed models controlling for the demographic factors.
Finally, because of our interest into how occupational injury and illness rates may have impacted these findings, we categorized occupations according to their occupational injury and illness rate as published by the BLS SOII. This data was obtained for the years 2011 to 2015. Rates are expressed as the number of injuries per 100,000 full-time workers. We categorized occupations into four categories according to these rates (less than 40; 40 to 69; 70 to 99; or 100 or more injuries per 10,000 full-time workers) according to the injury rate category that the occupation fell for the most years from 2011 to 2015. In cases where there was no category that the occupation fell into for most years, we categorized the occupation according to the average rate over the time period. We calculated mortality RRs for these categories for all deaths of despair and the individual categories of death according to the parameters described above, while treating the less than 100 injury rate category as the reference group. Additionally, we constructed a model in which the imputed injury rates were kept as a continuous variable.
RESULTS
Figure 1 and supplementary Table 1, http://links.lww.com/JOM/A872 show the number, percent, and rate of all deaths of despairs among healthcare workers for all deaths and the individual categories of deaths of despair: poisoning, suicide, alcohol liver disease and cirrhosis, and opioid-related deaths. There was a total of 540 deaths of despair among healthcare workers in MA between 2011 and 2015, accounting for an average annual rate of 32.4 deaths per 100,000 workers (95% confidence interval [CI]: 29.6, 35.1). The highest number of deaths of despair occurred among nursing, psychiatric, and home health aides. The highest mortality rate for all deaths of despair was observed among medical assistants and other healthcare support occupations (75.5 deaths per 100,000 workers). Medical assistants; nursing, psychiatric, and home health aides; miscellaneous; health technologists and technicians; emergency medical technicians, and paramedics had mortality rates due to all deaths of despair significantly higher than that for all other workers (Table 1).
FIGURE 1.
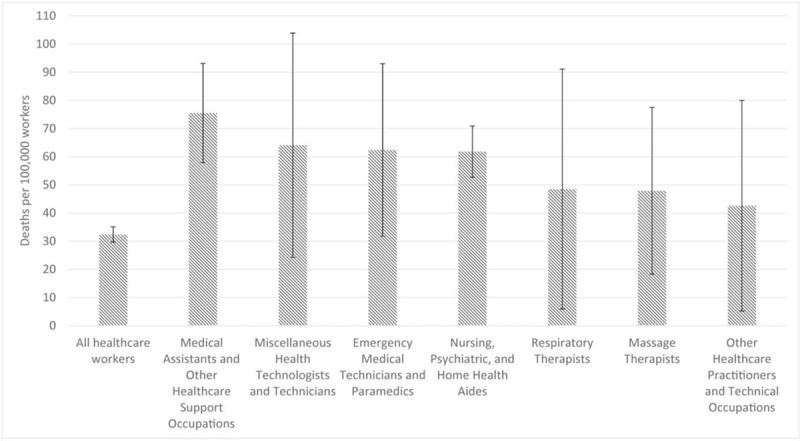
Mortality rates for deaths of despair by occupation among healthcare workers with rates higher than the rate for all healthcare workers, Massachusetts, 2011 to 2015.
TABLE 1.
Mortality Rate Ratios for Deaths of Despair Among Healthcare Workers, Massachusetts, 2011 to 2015
| Job Title | All Deaths of Despair | Poisoning | Suicide | Alcoholic Liver Disease | Opioid-Related Death |
| Rate ratio (95% CI) | |||||
| Medical assistants and other healthcare support occupations | 2.53 (1.97, 3.25) | 2.73 (1.96, 3.82) | 2.16 (1.30, 3.57) | 2.55 (1.45, 4.47) | 2.77 (1.95, 3.92) |
| Nursing, psychiatric, and home health aides | 2.35 (1.97, 2.82) | 3.12 (2.46, 3.96) | 1.48 (1.01, 2.16) | 1.90 (1.25, 2.91) | 3.25 (2.54, 4.16) |
| Miscellaneous health technologists and technicians | 2.00 (1.07, 3.74) | 1.51 (0.56, 4.05) | 2.18 (0.69, 6.83) | 3.09 (0.98, 9.73) | 0.41 (0.06, 2.90) |
| Emergency medical technicians and paramedics | 1.96 (1.19, 3.22) | 2.57 (1.41, 4.70) | 1.32 (0.42, 4.13) | 1.23 (0.30, 4.99) | 2.82 (1.54, 5.16) |
| Respiratory therapists | 1.50 (0.62, 3.63) | 0.57 (0.08, 4.03) | 2.19 (0.54, 8.83) | 3.09 (0.76, 12.53) | 0.62 (0.09, 4.41) |
| Massage therapists | 1.49 (0.80, 2.78) | 1.41 (0.58, 3.41) | 2.74 (1.12, 6.68) | [1] | 1.86 (0.83, 4.17) |
| Other healthcare practitioners and technical occupations | 1.32 (0.55, 3.18) | 1.50 (0.48, 4.68) | [1] | 2.71 (0.67, 11.00) | 1.09 (0.27, 4.38) |
| Health diagnosing and treating practitioner support technicians | 1.00 (0.66, 1.52) | 1.16 (0.68, 1.98) | 0.46 (0.15, 1.45) | 1.35 (0.59, 3.07) | 1.37 (0.81, 2.30) |
| Occupational therapists | 0.98 (0.44, 2.20) | 0.31 (0.04, 2.20) | 3.04 (1.25, 7.42) | [1] | [1] |
| Medical records and health information technicians | 0.89 (0.40, 1.99) | 0.84 (0.27, 2.63) | 1.08 (0.27, 4.35) | 0.75 (0.11, 5.40) | 0.92 (0.30, 2.87) |
| Dental assistants | 0.76 (0.38, 1.53) | 0.36 (0.09, 1.44) | 0.69 (0.17, 2.78) | 1.99 (0.73, 5.39) | 0.39 (0.10, 1.57) |
| Registered nurses | 0.72 (0.59, 0.88) | 0.59 (0.44, 0.79) | 0.85 (0.59, 1.24) | 0.93 (0.60, 1.43) | 0.58 (0.42, 0.79) |
| Clinical laboratory technologists and technicians | 0.66 (0.38, 1.15) | 0.68 (0.32, 1.43) | 0.55 (0.18, 1.73) | 0.78 (0.25, 2.47) | 0.52 (0.22, 1.27) |
| Diagnostic related technologists and technicians | 0.66 (0.34, 1.28) | 0.28 (0.07, 1.11) | 1.64 (0.73, 3.72) | 0.37 (0.05, 2.67) | 0.30 (0.08, 1.22) |
| Licensed practical and licensed vocational nurses | 0.62 (0.38, 1.01) | 0.63 (0.32, 1.21) | 0.67 (0.27, 1.62) | 0.56 (0.18, 1.76) | 0.61 (0.30, 1.23) |
| Pharmacists | 0.49 (0.22, 1.09) | 0.31 (0.08, 1.24) | 0.89 (0.29, 2.81) | 0.41 (0.06, 2.97) | 0.34 (0.08, 1.35) |
| Physicians and surgeons | 0.23 (0.13, 0.40) | 0.13 (0.05, 0.36) | 0.46 (0.22, 0.99) | 0.18 (0.04, 0.73) | 0.11 (0.04, 0.34) |
[1] is used to denote categories that had 0 deaths.
Bold indicates statistically significant rate ratios.
With respect to poisonings, there were 17.1 deaths per 100,000 workers (95% CI: 15.1, 19.1). Nursing, psychiatric, and home health aides account for 39.2% of all poisoning deaths (Supplementary Table 1, http://links.lww.com/JOM/A872). Nursing, psychiatric, and home health aides; medical assistants; emergency medical technicians, and paramedics had mortality rates due to poisonings significantly higher than that for all other workers. Similar patterns were observed with respect to opioid-related overdose deaths (Supplementary Table 1, http://links.lww.com/JOM/A872).
With respect to suicide, there were 8.9 deaths per 100,000 workers (95% CI: 7.5, 10.4) (Supplementary Table 1, http://links.lww.com/JOM/A872). Medical assistants and other healthcare support occupations; nursing, psychiatric, and home health aides; massage therapists; and occupational therapists had mortality rates due to suicide significantly higher than that for all other workers (Supplementary Table 1, http://links.lww.com/JOM/A872).
With respect to alcoholic liver disease and cirrhosis deaths, there were 6.4 deaths per 100,000 workers (95% CI: 5.1, 7.6) (Supplementary Table 1, http://links.lww.com/JOM/A872). Chiropractors; respiratory therapists; and miscellaneous health technologists and technicians had mortality rates due to alcoholic liver disease and cirrhosis higher than the average for all workers (Supplementary Table 1, http://links.lww.com/JOM/A872).
Table 2 shows the number, rate and percent of deaths of despair among healthcare workers according to age group, sex, race/ethnicity, and education. Mortality rates for all deaths of despair and suicides and alcoholic liver disease and cirrhosis deaths tended to be higher among the older age groups (45 to 54 and 55 to 64 years old), while poisoning and opioid-related mortality rates were highest in the 35- to 44-year-old age group. There were many more deaths among women compared with men and rates among women tended to be higher than rates among men. Mortality rates for all deaths of despair among white workers were higher than any other race/ethnicity group. This pattern was true for suicides. Hispanics had the highest rates for alcoholic liver disease and cirrhosis deaths and the other or unknown race/ethnicity group had higher rates for poisonings and opioid-related deaths. Mortality rates were much higher among those with a high school education or less compared to those with at least some college.
TABLE 2.
Deaths of Despair Among Healthcare Workers According to Age, Sex, Race/Ethnicity, and Education, Massachusetts, 2011 to 2015
| All Deaths of Despair | Poisoning | Suicide | Alcoholic Liver Disease and Cirrhosis | Opioid-Related Deaths | ||||||
| Deaths (n [%]) | Deaths Per 100,000 (95% CI) | Deaths (n [%]) | Deaths per 100,000 (95% CI) | Deaths (n [%]) | Deaths Per 100,000 (95% CI) | Deaths (n [%]) | Deaths Per 100,000 (95% CI) | Deaths (n [%]) | Deaths per 100,000 (95% CI) | |
| Age group | ||||||||||
| 16–24 | 17 (3.6) | 12.2 (6.4, 18.0) | 11 (4.4) | 7.9 (3.2, 12.6) | 6 (4.8) | 4.3 (0.9, 7.8) | 0 (0.0) | 0.0 (0.0, 0.0) | 12 (5.2) | 8.6 (3.7, 13.5) |
| 25–34 | 80 (16.9) | 20.8 (16.3, 25.4) | 55 (22.0) | 14.3 (10.5, 18.1) | 21 (16.7) | 5.5 (3.1, 7.8) | [1] | [1] | 54 (23.3) | 14.1 (10.3, 17.8) |
| 35–44 | 107 (22.6) | 31.3 (25.4, 37.2) | 70 (28.0) | 20.5 (15.7, 25.3) | 28 (22.2) | 8.2 (5.2, 11.2) | 9 (9.2) | 2.6 (0.9, 4.4) | 62 (26.7) | 18.1 (13.6, 22.7) |
| 45–54 | 143 (30.2) | 38.3 (32.1, 44.6) | 69 (27.6) | 18.5 (14.1, 22.9) | 39 (31.0) | 10.5 (7.2, 13.7) | 35 (35.7) | 9.4 (6.3, 12.5) | 65 (28.0) | 17.4 (13.2, 21.7) |
| 55–64 | 127 (26.8) | 39.7 (32.8, 46.6) | 45 (18.0) | 14.1 (9.9, 18.2) | 32 (25.4) | 10.0 (6.5, 13.5) | 50 (51.0) | 15.6 (11.3, 19.9) | 39 (16.8) | 12.2 (8.4, 16.0) |
| Sex | ||||||||||
| Female | 390 (82.3) | 31.1 (28.0, 34.2) | 212 (84.8) | 16.9 (14.6, 19.2) | 95 (75.4) | 7.6 (6.0, 9.1) | 83 (84.7) | 6.6 (5.2, 8.0) | 196 (84.5) | 15.6 (13.4, 17.8) |
| Male | 84 (17.7) | 27.7 (21.8, 33.6) | 38 (15.2) | 12.5 (8.5, 16.5) | 31 (24.6) | 10.2 (6.6, 13.8) | 15 (15.3) | 4.9 (2.4, 7.5) | 36 (15.5) | 11.9 (8.0, 15.8) |
| Race/ethnicity | ||||||||||
| Asian, non-Hispanic | [1] | [1] | 0 (0.0) | 0.0 (0.0, 0.0) | [1] | [1] | 0 (0.0) | 0.0 (0.0, 0.0) | [1] | [1] |
| Black, non-Hispanic | 23 (4.9) | 12.7 (7.5, 17.9) | 19 (7.6) | 10.5 (5.8, 15.2) | [1] | [1] | [1] | [1] | 16 (6.9) | 8.8 (4.5, 13.1) |
| Hispanic, all races | 22 (4.6) | 19.3 (11.2, 27.3) | 9 (3.6) | 7.9 (2.7, 13.0) | [1] | [1] | 9 (9.2) | 7.9 (2.7, 13.0) | 7 (3.0) | 6.1 (1.6, 10.7) |
| Other or unknown | 8 (1.7) | 25.9 (8.0, 43.9) | 6 (2.4) | 19.4 (3.9, 35.0) | [1] | [1] | 0 (0.0) | 0.0 (0.0, 0.0) | 6 (2.6) | 19.4 (3.9, 35.0) |
| White, non-Hispanic | 418 (88.2) | 36.6 (33.1, 40.1) | 216 (86.4) | 18.9 (16.4, 21.4) | 116 (92.1) | 10.2 (8.3, 12.0) | 86 (87.8) | 7.5 (5.9, 9.1) | 202 (87.1) | 17.7 (15.2, 20.1) |
| Education | ||||||||||
| High school or less | 179 (37.8) | 73.2 (62.5, 84.0) | 107 (42.8) | 43.8 (35.5, 52.1) | 35 (27.8) | 14.3 (9.6, 19.1) | 37 (37.8) | 15.1 (10.3, 20.0) | 101 (43.5) | 41.3 (33.3, 49.4) |
| Some college or more | 295 (62.2) | 22.5 (19.9, 25.0) | 143 (57.2) | 10.9 (9.1, 12.7) | 91 (72.2) | 6.9 (5.5, 8.4) | 61 (62.2) | 4.6 (3.5, 5.8) | 131 (56.5) | 10.0 (8.3, 11.7) |
| All workers | 474 (100.0) | 30.4 (27.7, 33.2) | 250 (100.0) | 16.0 (14.1, 18.0) | 126 (100.0) | 8.1 (6.7, 9.5) | 98 (100.0) | 6.3 (5.0, 7.5) | 232 (100.0) | 14.9 (13.0, 16.8) |
[1] indicates a cell has one to four deaths in a specific category.
Table 3 shows mortality RRs while controlling for demographic factors. RRs in model 1 for occupation differ from Table 2 because demographic data were not available for all workers and those workers were excluded from this analysis. RRs for this subset of the dataset were generally similar to those observed for the overall dataset. Fewer occupations were found to be significantly elevated likely due to less precision from the smaller sample size. Controlling for demographics factors did not have a substantial impact on rate ratios, which generally stayed the same in the different models.
TABLE 3.
Mortality Rate Ratio for Deaths of Despair Among Healthcare Workers Controlling for Covariates With All Other Workers as Reference Group, Massachusetts, 2011 to 2015
| Occupation | Rate Ratio—Model 1 | Rate Ratio—Model 2 | Rate Ratio—Model 3 | Rate Ratio—Model 4 | Rate ratio—Model 5 |
| Nursing, psychiatric, and home health aides | 2.55 (2.12, 3.08) | 2.72 (2.25, 3.28) | 2.71 (2.25, 3.28) | 3.64 (3.00, 4.43) | 2.25 (1.80, 2.82) |
| Medical assistants and other healthcare support occupations | 2.30 (1.76, 3.01) | 2.64 (2.01, 3.46) | 2.63 (2.00, 3.45) | 2.73 (2.08, 3.59) | 2.05 (1.56, 2.70) |
| Emergency medical technicians and paramedics | 1.58 (0.89, 2.80) | 2.00 (1.13, 3.57) | 2.14 (1.19, 3.85) | 1.91 (1.06, 3.45) | 1.42 (0.78, 2.57) |
| Miscellaneous health technologists and technicians | 1.57 (0.74, 3.31) | 1.66 (0.79, 3.50) | 1.67 (0.79, 3.53) | 1.94 (0.92, 4.09) | 1.65 (0.78, 3.48) |
| Respiratory therapists | 1.03 (0.33, 3.21) | 0.93 (0.30, 2.90) | 0.94 (0.30, 2.94) | 0.90 (0.29, 2.80) | 1.20 (0.39, 3.76) |
| Health diagnosing and treating practitioner support technicians | 0.96 (0.61, 1.49) | 1.16 (0.74, 1.82) | 1.16 (0.74, 1.82) | 1.12 (0.72, 1.77) | 0.89 (0.57, 1.41) |
| Other healthcare practitioners and technical occupations | 0.90 (0.29, 2.81) | 0.90 (0.29, 2.81) | 0.94 (0.30, 2.92) | 0.87 (0.28, 2.72) | 0.95 (0.30, 2.96) |
| Registered nurses | 0.89 (0.72, 1.10) | 0.80 (0.64, 0.98) | 0.78 (0.63, 0.96) | 0.71 (0.58, 0.88) | 1.11 (0.88, 1.40) |
| Occupational therapists | 0.71 (0.27, 1.90) | 0.70 (0.26, 1.86) | 0.69 (0.26, 1.84) | 0.60 (0.23, 1.62) | 0.83 (0.31, 2.22) |
| Diagnostic related technologists and technicians | 0.67 (0.33, 1.35) | 0.63 (0.31, 1.27) | 0.63 (0.32, 1.28) | 0.57 (0.28, 1.15) | 0.74 (0.37, 1.49) |
| Licensed practical and licensed vocational nurses | 0.67 (0.40, 1.13) | 0.64 (0.38, 1.07) | 0.63 (0.38, 1.06) | 0.67 (0.40, 1.13) | 0.58 (0.35, 0.97) |
| Massage therapists | 0.63 (0.23, 1.68) | 0.66 (0.25, 1.76) | 0.66 (0.25, 1.76) | 0.62 (0.23, 1.67) | 0.57 (0.21, 1.52) |
| Dental assistants | 0.61 (0.27, 1.35) | 0.68 (0.30, 1.52) | 0.67 (0.30, 1.50) | 0.68 (0.31, 1.53) | 0.52 (0.23, 1.18) |
| Medical records and health information records | 0.55 (0.18, 1.70) | 0.56 (0.18, 1.73) | 0.55 (0.18, 1.72) | 0.54 (0.17, 1.69) | 0.38 (0.12, 1.18) |
| Clinical laboratory technologists and technicians | 0.45 (0.23, 0.91) | 0.49 (0.24, 0.99) | 0.49 (0.25, 0.99) | 0.51 (0.25, 1.03) | 0.53 (0.26, 1.06) |
| Pharmacists | 0.37 (0.14, 1.00) | 0.39 (0.15, 1.04) | 0.40 (0.15, 1.06) | 0.42 (0.16, 1.12) | 0.56 (0.21, 1.51) |
| Physicians and surgeons | 0.24 (0.13, 0.44) | 0.23 (0.12, 0.41) | 0.22 (0.12, 0.40) | 0.23 (0.12, 0.42) | 0.31 (0.17, 0.56) |
Model 1—Occupation only.
Model 2—Adjusting for age.
Model 3—Adjusting for age and sex.
Model 4—Adjusting for age, sex, and race/ethnicity.
Model 5—Adjusting age, sex, race/ethnicity, and education.
Bold indicates statistically significant rate ratios.
Table 4 shows mortality rate for deaths of despair with occupations coded according to their occupational injury and illness rates. When treating occupational injury and illness rates as a continuous variable, there was a positive association between the occupation's injury and illness rate and deaths of despair. This pattern was true for the individual categories of deaths of despair as well, with the strongest association observed for poisonings and opioid-related deaths. A similar pattern of higher mortality rates with higher injury and illness rate was also observed when occupations were categorized into four categories according to their occupational injury and illness rates. The only exception to this pattern was the 40 to 69 injuries per 10,000 full-time equivalents group, which had a lower rate of poisoning and opioid-related deaths than the less than 40 injuries per 10,000 full-time equivalents and the 100 or more injuries per 10,000 full-time equivalents having a lower rate of suicides than the 70 to 99 injuries per 10,000 full-time equivalents group.
TABLE 4.
Mortality Rate Ratios for Deaths of Despair Among Healthcare Workers According to Occupational Injury Rate, Massachusetts, 2011 to 2015
| All | Poisoning | Suicide | Alcoholic Liver Disease and Cirrhosis | Opioid-Related Deaths | |
| Occupational injury and illness rate (continuous) | 1.049 (1.041, 1.058) | 1.068 (1.056, 1.080) | 1.023 (1.007, 1.039) | 1.040 (1.022, 1.060) | 1.073 (1.060, 1.086) |
| Occupational injury and illness rate category1 | |||||
| Less than 40 injuries per 10,000 full-time equivalents | 1 | 1 | 1 | 1 | 1 |
| 40–69 injuries per 10,000 full-time equivalents | 1.35 (0.76, 2.38) | 0.73 (0.24, 2.21) | 1.82 (0.81, 4.09) | 1.70 (0.81, 4.09) | 0.73 (0.24, 2.21) |
| 70–99 injuries per 10,000 full-time equivalents | 2.47 (1.59, 3.85) | 2.61 (1.32, 5.17) | 2.35 (1.17, 4.72) | 2.44 (1.17, 4.72) | 2.61 (1.32, 5.17) |
| 100 or more injuries per 10,000 full-time equivalents | 3.40 (2.39, 4.84) | 4.63 (2.69, 7.97) | 2.02 (1.15, 3.56) | 3.75 (1.15, 3.56) | 4.63 (2.69, 7.97) |
1—Occupations categorized according to the occupational injury and illness rate for that occupation as published by the Bureau of Labor Statistics Survey of Occupational Injury and Illnesses, 2011 to 2015.
DISCUSSION
Among healthcare workers in MA the overall mortality rate for deaths of despair was 32.4 deaths per 100,000 workers, which is only slightly lower than that found for all workers in MA during the same time period.9 There was substantial variability in mortality rates from deaths of despair among MA healthcare workers. In particular, medical assistants; nursing, psychiatric, and home health aides; miscellaneous; health technologists and technicians; and emergency medical technicians and paramedics had mortality rates for all deaths of despair significantly higher than that for all workers. Mortality rates also varied according to cause of deaths. Consistent with previous findings,9 deaths were highest for poisoning deaths, most of which were opioid-related, followed by suicides, and alcoholic liver disease and cirrhosis deaths. Occupations with significantly different rates differed with respect to cause of death as well. For example, massage therapists and occupational therapists had significantly elevated rates for suicides, but not other deaths of despair.
In general, occupations with elevated mortality rates for all deaths of despair also had elevated mortality rates of specific causes of death as well. Medical assistants and nursing, psychiatric, and home health aides stood out in particular as having very elevated rates across the categories. Both of these occupations are healthcare support occupations. They both have occupational injury and illness rates two to three times higher than that of all workers.28 Emergency medical technicians and paramedics also had elevated mortality rates. Previous work has suggested that these workers may be at an increased risk of suicidal thought and behaviors, which may be related to the often traumatic nature of the work performed.29 Although the elevated rate among emergency medical technicians and paramedics was not significant in this study, this lack of significance may have been due to the study being unpowered for these occupations. Massage and occupational therapists stood out for having elevated rates for suicides, but not other deaths of despair. To the best of our knowledge previous work has not explored factors that may explain this findings.
Other factors may also be associated with these occupation specific differences. Most of the occupations with low mortality rates were health practioners and technical occupations. Weekly earnings among these workers are nearly double earnings among healthcare support workers.30 The occupations with the two lowest mortality rates physician and surgeons and pharmacists have the second and third highest earnings among detailed health practioners and technical occupations, exceeded only by dentists.30 A previous ecological study suggested that higher income may be protective against deaths of despair.31 Healthcare support workers are also substantially more likely to be unemployed compared with workers in health practioners and technical occupations,32 which may mean that these workers are less able to get treatment for factors that may contribute to the risk of deaths of despair such as substance abuse treatment or psychiatric care.
Patterns with respect to race, ethnicity, and age were similar to those for all workers in MA.9 Notably, women comprised the vast majority of deaths. While this is likely due to women comprising a larger share of the healthcare workforce, rates were slightly elevated among women compared with men, while most previous research has found that men have higher rates of deaths of despair.6 A majority of deaths occurred among those with some college or more education; this finding is likely due to many healthcare professions requiring some education above the high school level. However rates among those with a high school education or less was significantly higher than those with more education, which is consistent with previous work.6
Controlling for demographic factors did not substantially attenuate rate ratios. This finding is surprising because previous evidence has suggested that deaths of despair are strongly associated with the demographic factors explored (age, sex, race/ethnicity, and education)5,6 and that controlling for these factors attenuate mortality rate ratios comparing deaths of despair between occupations.9 Additionally, we found that demographic factors were associated with the deaths of despair in this study. It may be the case that while healthcare workers are very diverse overall with respect to these demographic factors within specific healthcare occupation there is not as much diversity. Therefore, controlling for these factors would not be expected to have as much of an impact.
This study also demonstrated that among healthcare workers, occupations with higher injury rates had higher rates of deaths of despair. This finding is consistent with other studies which have found that different categories of deaths of despair are associated with occupational injuries.23,24,26,27 While longitudinal studies suggest that occupational injuries may precede deaths from drug overdoses and suicides, alternative explanations cannot be ruled out. For example, it might be that occupations where workers have a higher likelihood to use opioids may also be occupations where workers have a higher likelihood of getting injured, perhaps due to impairment caused by the use of these substances.22
There are a number of factors that many contribute to deaths of despair among healthcare workers. For instance, access to medications likely differs between occupations. A previous study showed that up to 43% of suicides among veterinarians are caused by suicide, which may partially be due to easy access to lethal drugs.33,34 Healthcare workers are more likely to use medications to commit suicide compared with other workers.17 Furthermore, socioeconomic factors may play a role. Most occupations found in our study to have higher rates of deaths of despair are healthcare support occupations which generally have lower levels of educational attainment than other healthcare occupations. Healthcare workers also face a number of exposures that may contribute to occupational stress, such as rotating shifts or long work hours, which may further lead to a greater risk of deaths of despair.34,35
This study had some limitations. There may be some misclassification with respect to occupation. Death certificates only have information about usual occupation of the decedent and therefore, it is not possible to be certain whether workers were employed in these occupations at their time of death. Indeed, it is not possible to be certain whether the worker was in fact employed at all at the time of death. This can result in misclassification and over/underestimation of rates. Additionally, because of the limited sample size with usable demographic data, we were not able to fully investigate the role of potential confounders in this analysis. Finally, there may be some misclassification of cause of death. For example, some suicides may have been misclassified due to a societal stigma against suicide. Generally, more evidence is required to classify a death as a suicide therefore some deaths that were in reality suicides may be classified as being of unintentional or undetermined intent.
Deaths of despair among healthcare workers deserves further attention. Workers in these occupations face a number of physical and psychosocial factors that may put them at a higher risk for deaths of despair compared with other workers. Methods to protect workers from these exposures should be implemented. Prevention of these injuries can take place at a number of levels. For example, primary prevention injuries may prevent exposure to opioids in the first place. For example, patient handling injuries are common source of injuries among healthcare workers.36 Methods that can be used to prevent these patient handling and other musculoskeletal injuries including patient lifting devices and integrated ergonomic programs have been shown to be effective to prevent these injuries.37 After workers have become injured, guidelines for prescribing opioids to working populations should be followed.38 Methods to organize work that may protect workers from mental health comorbidites should be implemented. For example, there is some evidence that organization interventions can reduce stress among healthcare workers.39 Among workers who have substance use or mental health issues, workplaces should provide support for these workers. This support can include dedicated mental health counseling, such as those provided through Employee Assistance Programs or benefits that allow for paid time off for treatment, such as paid sick leave. With respect to harm reduction, placing naloxone at the workplace can prevent opioid overdoses that occur at work.40 Further research should examine the role of psychosocial and work organizations exposures in explaining differences in risks for deaths of despair and risk factors for these deaths.
Acknowledgments
The authors would like to thank the Massachusetts Registry of Vital Records and Statistics for providing the data used in this study.
Footnotes
Conflicts of interest (financial, consultant, institutional, and other relationships that might lead to bias or a conflict of interest): None declared.
Kaki and Hawkins have no relationships/conditions/circumstances that present potential conflict of interest.
The JOEM editorial board and planners have no financial interest related to this research.
Clinical significance: This paper helps to identify healthcare occupations that may be at particularly high risk for the deaths of despair (drug overdoses, suicides, and alcoholic liver disease). Additionally, these findings may be useful for identifying occupational risk factors for these causes of death. Findings suggest that occupational injury may be one important factor contributing to increased risk.
Supplemental digital contents are available for this article. Direct URL citation appears in the printed text and is provided in the HTML and PDF versions of this article on the journal's Web site (www.joem.org).
REFERENCES
- 1.Xu JQ, Murphy SL, Kochanek KD, Arias E. Mortality in the United States, 2015. NCHS Data Brief, No 267. Hyattsville, MD: National Center for Health Statistics; 2016. [PubMed] [Google Scholar]
- 2.Kochanek KD, Murphy SL, Xu JQ, Arias E. Mortality in the United States, 2016. NCHS Data Brief, No 293. Hyattsville, MD: National Center for Health Statistics; 2017. [PubMed] [Google Scholar]
- 3. Murphy SL, Xu J, Kochanek KD, Arias E. Mortality in the United States, 2017; 2018. [PubMed] [Google Scholar]
- 4.Xu JQ, Murphy SL, Kochanek KD, Arias E. Mortality in the United States, 2018. NCHS Data Brief, No 355. Hyattsville, MD: National Center for Health Statistics; 2020. [Google Scholar]
- 5.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A 2015; 112:15078–15083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Case A, Deaton A. Mortality and morbidity in the 21st century. Brookings Papers on Economic Activity 2017; 23–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Woolf SH, Chapman DA, Buchanich JM, Bobby KJ, Zimmerman EB, Blackburn SM. Changes in midlife death rates across racial and ethnic groups in the United States: systematic analysis of vital statistics. BMJ 2018; 362:k3096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gutin I, Hummer RA. Occupation, employment status, and “despair”-associated mortality risk among working-aged U.S. adults, 1997-2015. Prev Med 2020; 137:106129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hawkins D, Davis L, Punnett L, Kriebel D. Disparities in the deaths of despair by occupation, Massachusetts, 2000 to 2015. J Occup Environ Med 2020; 62:484–492. [DOI] [PubMed] [Google Scholar]
- 10.Walter AW, Morocho C, King L, et al. Preventing opioid use disorders among fishing industry workers. Int J Environ Res Public Health 2018; 15:648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dong XS, Brooks RD, Cain CT. Prescription opioid use and associated factors among US construction workers. Am J Ind Med 2020; 63:868–877. [DOI] [PubMed] [Google Scholar]
- 12. Educational attainment for workers 25 years and older by detailed occupation; 2020. Available at: https://www.bls.gov/emp/tables/educational-attainment.htm#1. Accessed December 30, 2020. [Google Scholar]
- 13. Employed persons by detailed occupation, sex, race, and Hispanic or Latino ethnicity; 2020. Available at: https://www.bls.gov/cps/cpsaat11.htm. Accessed December 30, 2020. [Google Scholar]
- 14. Industries with the fastest growing and most rapidly declining wage and salary employment; 2020. Available at: https://www.bls.gov/emp/tables/industries-fast-grow-decline-employment.htm. Accessed December 30, 2020. [Google Scholar]
- 15.Stallones L, Doenges T, Dik BJ, Valley MA. Occupation and suicide: Colorado, 2004-2006. Am J Ind Med 2013; 56:1290–1295. [DOI] [PubMed] [Google Scholar]
- 16.Bartram DJ, Baldwin DS. Veterinary surgeons and suicide: a structured review of possible influences on increased risk. Vet Rec 2010; 166:388–397. [DOI] [PubMed] [Google Scholar]
- 17.Hawton K, Clements A, Simkin S, Malmberg A. Doctors who kill themselves: a study of the methods used for suicide. QJM 2000; 93:351–357. [DOI] [PubMed] [Google Scholar]
- 18. Bureau of Labor Statistics. 2018 Survey of Occupational Injury and Illnesses; 2019. Available at: https://www.bls.gov/iif/soii-charts-2018.pdf. Accessed December 30, 2020. [Google Scholar]
- 19. Number of nonfatal occupational injuries and illnesses involving days away from work by event or exposure leading to injury or illness and industry sector, private industry, 2019; 2020. Available at: https://www.bls.gov/iif/oshwc/osh/case/cd_r64_2019.htm. Accessed December 30, 2020. [Google Scholar]
- 20. Hawkins D. Violence in healthcare: trends and disparities. In APHA's 2019 Annual Meeting and Expo (Nov. 2-Nov. 6). Washington, DC: American Public Health Association; 2019. [Google Scholar]
- 21.d’Errico A, Punnett L, Cifuentes M, et al. Promoting Healthy and Safe Employment In Healthcare Research Team. Hospital injury rates in relation to socioeconomic status and working conditions. Occup Environ Med 2007; 64:325–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kowalski-McGraw M, Green-McKenzie J, Pandalai SP, Schulte PA. Characterizing the interrelationships of prescription opioid and benzodiazepine drugs with worker health and workplace hazards. J Occup Environ Med 2017; 59:1114–1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Applebaum KM, Asfaw A, O’Leary PK, Busey A, Tripodis Y, Boden LI. Suicide and drug-related mortality following occupational injury. Am J Ind Med 2019; 62:733–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Martin CJ, Jin C, Bertke SJ, Yiin JH, Pinkerton LE. Increased overall and cause-specific mortality associated with disability among workers’ compensation claimants with low back injuries. Am J Ind Med 2020; 63:209–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Greenspan LS, Alley L, Rice S, Olson R. Exploring biopsychosocial correlates of pain, pain management strategies, and risk for opioid misuse among home care workers in Washington State. Home Health Care Serv Q 2020. 1–21. [DOI] [PubMed] [Google Scholar]
- 26.Hawkins D, Roelofs C, Laing J, Davis L. Opioid-related overdose deaths by industry and occupation—Massachusetts, 2011-2015. Am J Ind Med 2019; 62:815–825. [DOI] [PubMed] [Google Scholar]
- 27. Hawkins DM. The Contribution of Work to the Deaths of Despair (Doctoral dissertation). Lowell, MA: University of Massachusetts; 2020. [Google Scholar]
- 28. Bureau of Labor Statistics. Injuries, Illnesses, and Fatalities; 2019. Available at: https://www.bls.gov/iif/. Accessed December 30, 2020. [Google Scholar]
- 29.Stanley IH, Hom MA, Joiner TE. A systematic review of suicidal thoughts and behaviors among police officers, firefighters, EMTs, and paramedics. Clin Psychol Rev 2016; 44:25–44. [DOI] [PubMed] [Google Scholar]
- 30. Bureau of Labor Statistics. Median weekly earnings of full-time wage and salary workers by detailed occupation and sex; 2020. Available at: https://www.bls.gov/cps/cpsaat39.htm. Accessed December 30, 2020. [Google Scholar]
- 31.Zeglin RJ, Niemela D, Baynard CW. Deaths of despair in Florida: assessing the role of social determinants of health. Health Educ Behav 2019; 46:329–339. [DOI] [PubMed] [Google Scholar]
- 32.Boal WL, Li J, Sussell A. Health insurance coverage by occupation among adults aged 18-64 years—17 States, 2013-2014. Morb Mortal Wkly Rep 2018; 67:593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Platt B, Hawton K, Simkin S, Mellanby RJ. Systematic review of the prevalence of suicide in veterinary surgeons. Occup Med (Lond) 2010; 60:436–446. [DOI] [PubMed] [Google Scholar]
- 34.Tomasi SE, Fechter-Leggett ED, Edwards NT, Reddish AD, Crosby AE, Nett RJ. Suicide among veterinarians in the United States from 1979 through, 2015. J Am Vet Med Assoc 2019; 254:104–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dutheil F, Aubert C, Pereira B, et al. Suicide among physicians and health-care workers: a systematic review and meta-analysis. PLoS ONE 2019; 14:e0226361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pompeii LA, Lipscomb HJ, Schoenfisch AL, Dement JM. Musculoskeletal injuries resulting from patient handling tasks among hospital workers. Am J Ind Med 2009; 52:571–578. [DOI] [PubMed] [Google Scholar]
- 37.Garg A, Kapellusch JM. Long-term efficacy of an ergonomics program that includes patient-handling devices on reducing musculoskeletal injuries to nursing personnel. Hum Factors 2012; 54:608–625. [DOI] [PubMed] [Google Scholar]
- 38. MA Department of Industrial Accidents (MA DIA). Opioid/Controlled Substances Protocol; 2016. Available at: https://www.mass.gov/files/documents/2017/09/27/opioid-controlled-substance protocol.pdf. Accessed December 30, 2020. [Google Scholar]
- 39.Ruotsalainen J, Serra C, Marine A, Verbeek J. Systematic review of interventions for reducing occupational stress in health care workers. Scand J Work Environ Health 2008; 38:169–178. [DOI] [PubMed] [Google Scholar]
- 40. National Institute of Occupational Safety and Health (NIOSH). Using Naloxone to Reverse Opioid Overdose in the Workplace: Information for Employers and Workers; 2018. Available at: https://www.cdc.gov/niosh/docs/2019-101/pdfs/2019-101.pdf. Accessed December 30, 2020. [Google Scholar]


