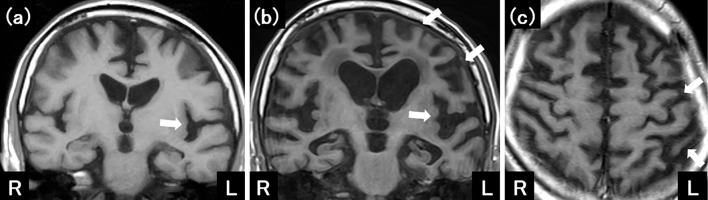
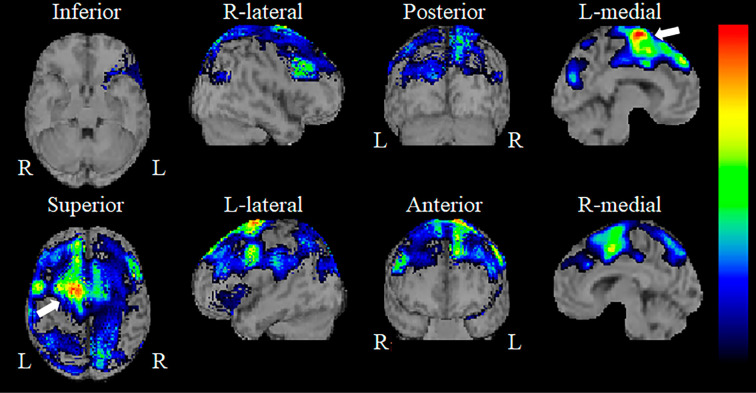
A 65-year-old man experienced a gradual decline in speech. His speech was sparse and required great effort, but he had a preserved reading ability, comprehension, and repetition. Naming was also almost normal, but his word enumeration decreased considerably. Magnetic resonance imaging of the brain showed left-dominant, asymmetric cortical atrophy (Picture 1a; white arrows). Brain single-photon emission computed tomography with 99mTc-ECD established asymmetric hypoperfusion mainly in the left frontoparietal lobe, especially in the supplementary motor area (SMA) (Picture 2; white arrows). Cerebrospinal fluid β-amyloid 1-42 levels were normal. After three years, levodopa-resistant akinetic-rigid syndrome and asymmetric limb dystonia with cortical sensory deficit became apparent, and bilateral, but left-dominant cerebral atrophy became more prominent (Picture 1b, c; white arrows). Corticobasal syndrome (CBS) with SMA aphasia was confirmed based on the modified Cambridge criteria. The main etiology of SMA aphasia is stroke, tumors, and head injury (1). However, speech requiring great effort is sometimes observed in patients with corticobasal degeneration (2). Thus, SMA aphasia may be an initial symptom of CBS.
Picture 1.
Picture 2.
The authors state that they have no Conflict of Interest (COI).
Acknowledgement
We thank Dr. K. Kasuga and Dr. T. Ikeuchi, Department of Molecular Genetics, Brain Research Institute, Niigata University, Niigata, Japan, for their assistance with the CSF analysis.
References
- 1. Ardila A. Other aphasic syndromes. In: Aphasia Handbook. Florida International University, Florida, 2014: 85-91. [Google Scholar]
- 2. Oliveira LM, Barcellos I, Teive HAG, Munhoz RP. Cognitive dysfunction in corticobassal degeneration. Arq Neuropsiquiatr 75: 570-579, 2017. [DOI] [PubMed] [Google Scholar]