Abstract
Background:
African American women have lower levels of leisure-time physical activity compared to White American women. Interventions to improve physical activity have mixed benefits for African American women, even when guided by theory. Understanding how theoretical constructs used in physical activity interventions relate to changing behavior may provide direction for more successful interventions.
Objective:
The study aimed to examine the relationships among social cognitive constructs (self-efficacy, social support from group behavioral meetings, outcome expectations/realizations), and change in physical activity from baseline to 48 weeks in African American women participating in a lifestyle physical activity program.
Methods:
A secondary data analysis of longitudinal data using a correlational design was conducted using data from a 48-week physical activity randomized controlled trial (RCT). The RCT included a group behavioral meeting component with one of three telephone intervention conditions (no calls, personal motivation calls, or automated motivational calls) randomly assigned across six community health care sites. The participants were 260 sedentary, midlife African American women with no major signs or symptoms of cardiovascular disease who completed baseline and 48-week assessments of the RTC. Measures included self-efficacy for change in overcoming barriers to physical activity at 24 weeks, physical and psychological-outcome realizations at 24 weeks, social support from group behavioral meetings at 24 weeks, and physical activity (self-report and device-measured) change from baseline to 48 weeks.
Results:
In a hierarchical regression model predicting change in self-reported time spent in weekly moderate-vigorous physical activity (MVPA) at 48 weeks, psychological-outcome realizations at 24 weeks were significant positive predictors. In a hierarchical regression model for change in device-measured daily steps at 48 weeks, a self-efficacy change at 24 weeks was a significant positive predictor.
Discussion:
Attention should be given to increasing self-efficacy to overcome physical activity barriers and achieve self-identified physical and psychological outcomes in PA programs.
Keywords: African American, behavior, physical activity
Sixty-five percent of African American women versus 49% of White women do not meet accepted physical activity recommendations (150 min per week of moderate-intensity physical activity; Benjamin et al., 2019). This contributes to the disproportionate risk that African American women have for obesity, cardiovascular disease, hypertension, and strokes (Benjamin et al., 2019). Theory-guided interventions using a variety of frameworks that incorporate self-management and ongoing group behavioral meeting support have increased physical activity for ethnic minority individuals residing in socioeconomically disadvantaged neighborhoods (Cleland et al., 2012). However, a recent review found mixed benefits of theory-guided physical activity interventions for African American women (Jenkins, 2017). Understanding how theoretical constructs used in physical activity interventions relate to performance may provide direction for more successful interventions in this population.
Social Cognitive Theory
Bandura’s (2004) social cognitive theory (SCT) has been widely used to guide physical activity interventions (Rhodes & Niggs, 2011). Four key SCT constructs that have served as behavior targets for improving physical activity performance include self-efficacy, social support, perceived outcome expectations, and perceived outcome realizations (Bandura, 2004). Self-efficacy—confidence in one’s ability to carry out physical activity in the face of barriers—is the most common target of physical activity interventions (Rhodes & Nigg, 2011). A systematic review of physical activity intervention studies based on SCT found that higher self-efficacy was consistently associated with improved physical activity (Young et al., 2014). Moreover, early work by Eyler et al. (1999) found that high social support from both friends and family was associated with higher physical activity levels in women. Mama et al.’s (2015) review of theory in physical activity interventions with minorities found that interventions that targeted either self-efficacy or social support reported the greatest changes in physical activity behavior.
Perceived outcome expectations refer to one’s belief about the physical benefits (e.g., improved shape, fitness) or psychological benefits (e.g., improved depression, anxiety) physical activity will bring. Perceived outcome realizations are the subjective beliefs of the extent to which those benefits were achieved. These two constructs have received less attention than self-efficacy and social support but may provide an additional target for behavioral interventions (Wilcox et al., 2006). Young et al.’s (2014) systematic review reported several studies in which outcome expectations were positively associated with physical activity, although this relationship was not consistent across studies. On the other hand, there is evidence from a study of predominately middle-aged White adults (Brassington et al., 2002) and a study of predominately White older women (Wilcox et al., 2006) that although outcome expectations were not associated with physical activity participation, satisfaction with outcome realizations had an influence on subsequent physical activity.
To understand the interactions between outcome expectations at baseline, outcome realizations at 6 months, and subsequent physical activity, Neff and King (1995) categorized these concepts into four outcome expectation/realization groups: “Disappointed optimists” had higher than average outcome expectations for physical/psychological benefits but had lower than average outcome realizations; “pessimistic realists” had lower than average outcome expectations and lower than average outcome realizations; “surprised pessimists” had lower than average outcome expectations and higher than average outcome realizations; and “optimistic realists” had both higher than average outcome expectations and outcome realizations. Using these categorizations, in a sample of predominately White middle-aged adults, Neff and King (1995) found that surprised pessimists had the highest subsequent physical activity, and Wilcox et al. (2006) found that disappointed optimists had the lowest subsequent physical activity. These studies suggest the importance of evaluating perceived outcome expectations in consort with perceived outcome realizations rather than examining them independently.
We identified 11 intervention studies, published since 2005, of healthy African American women guided by SCT or other constructs designed to increase physical activity behavior (Anderson & Pullen, 2013; Banks-Wallace, 2007; Fitzgibbon et al., 2010; Hornbuckle et al., 2012; Newton & Perri, 2004; Parra-Medina et al., 2011; Peterson & Cheng, 2011; Speck et al., 2007; Wilbur et al., 2016; Yancey et al., 2006; Yanek et al., 2001; Young & Stewart, 2006). Only two studies linked physical activity results to SCT constructs (Peterson & Cheng, 2011; Young & Stewart, 2006). Young and Stewart (2006) found small effects for self-efficacy and social support from family and friends on self-reported physical activity change. Peterson and Cheng (2011) found a large effect of total social support on self-reported physical activity change. The heterogeneity of these associations makes it difficult to predict the effect of theoretical constructs on physical activity among African American women. None of the studies examined outcome expectations or realizations. There is a need for a comprehensive approach to examining self-efficacy, social support, and outcome expectations/realizations in the context of physical activity change among African American women.
The Women’s Lifestyle Physical Activity Program
Wilbur et al. (2016) conducted a randomized controlled trial (RCT) of a 48-week lifestyle physical activity intervention (The Women’s Lifestyle Physical Activity Program) for African American women. Based on prior work showing the success of group behavioral meetings on physical activity in African American women (Wilbur et al., 2008), the three treatment conditions included five group behavioral meetings focused on increasing physical activity held during the 24-week adoption phase and one booster group meeting held midway during the 24-week maintenance phase. Each condition differed by telephone support between group meetings: One condition received personal calls with motivational interviewing, one condition received automated calls with motivational tips, and one condition received no telephone calls.
The intervention, guided by SCT, targeted self-efficacy for overcoming physical activity barriers, used group behavioral meetings to facilitate social support for physical activity and helped participants identify realistic expectations for physical and psychological outcomes. Participants in all three treatment conditions increased physical activity from baseline to the end of the adoption phase (24 weeks). Increased physical activity was sustained through the end of the maintenance phase (48 weeks; Wilbur et al., 2016). Data were collected on self-efficacy, group social support, and perceived outcome expectations and realizations. These data provide a unique opportunity to examine the associations of selected social cognitive constructs with successful physical activity outcomes.
The purpose of this study was to examine associations among SCT constructs (self-efficacy, social support from behavioral meetings, outcome expectations, outcome realizations) and improvement in physical activity from baseline to the end of the intervention maintenance phase in African American women participating in the Women’s Lifestyle Physical Activity Program. We hypothesized that (a) combined effects of improved self-efficacy at 24 weeks (end of adoption phase), greater social support from group behavioral meeting at 24 weeks, and higher outcome realizations at 24 weeks would be associated with improved physical activity from baseline to 48 weeks. We also hypothesized that based on outcome expectation/realization categories, optimistic realists and surprised pessimists would have the greatest improvement at 48 weeks and disappointed optimists and pessimistic realists would have the least progress in physical activity from baseline to 48 weeks.
Methods
Design
We conducted a secondary analysis of longitudinal data using a correlational design from women who participated in the full primary RCT of the Women’s Lifestyle Physical Activity Program (Wilbur et al., 2016). As noted, although all three treatment conditions showed improvement in physical activity, no treatment condition differences were based on adding or excluding a telephone component. Thus, data from all three conditions were pooled for these secondary analyses, and a nonexperimental design was used.
Participants
The sample comprised 260 (90.3% of 288) African American women who completed the primary RCT (Wilbur et al., 2016). As reported earlier, the 28 women who participated in the primary study but did not complete the 48-week assessment were younger and more active at baseline based on self-report of minutes per week of moderate-vigorous leisure physical activity (MVPA; Wilbur et al., 2016). The mean age of the 260 women was 53.1 years (SD = 6.5). Just over one third were married or living with a partner (38.8%), and just over one third had at least one child under age 18 living in the household (36.5%). Just under half of the participants had a college education (49.2%). Forty-seven percent had an income under $30,000. Device step data were available for 180 (69%) at baseline and 48 weeks. The strongest effect size for correlations between SCT constructs and physical activity was r = .26 for change in self-reported MVPA and 24-week outcome realizations. Given this effect size and a sample size of 260, this analysis’s power is .97 (Cohen, 1988).
Treatment
All women participated in in-person group behavioral meetings with 14 to 18 participants (Wilbur et al., 2016). There was individual time to discuss goal setting and review physical activity progress. The goal was to increase participants’ physical activity by at least 3,000 steps per day (approximately 30 min of moderate-paced walking daily) over their daily baseline steps. Average baseline daily steps were obtained from a blocked (no data displayed) physical activity device (accelerometer) worn for 1 week before the first group behavioral meeting. Devices were unblocked for the remainder of the study, and all participants entered their steps weekly into an automated phone system.
Consistent with SCT, group discussion began with a short DVD to illustrate self-efficacy. It featured African American women demonstrating skills and sharing experiences and challenges while becoming more active (Bandura, 2004). African American nurse interventionists facilitated the discussions centered on role modeling, encouraging problem-solving, and encouraging social support among the women. All discussions addressed physical activity barriers and dispelled misinformation identified in earlier focus groups (Wilbur et al., 2002). The discussion in the booster group behavioral meeting focused on anticipating barriers and handling challenges. Interventionists followed a detailed manual that included content and learning activities to guide meeting discussions.
Measures
Physical Activity
Physical activity was measured by a self-report physical activity questionnaire and accelerometer at baseline and 48 weeks. Self-reported moderate- to vigorous-lifestyle physical activity was measured with the Community Healthy Activities Model Program for Seniors (CHAMPS) questionnaire (Stewart et al., 2001). Respondents were asked the types of physical activities, frequency, and time spent in each activity in a typical week over the last 4 weeks. Six categories ranged from less than 1 hr/week to 9 or more hr/week, with the midpoint of each category range used to estimate time for each activity. Each activity had an assigned metabolic equivalent (MET) value based on the 2011 Compendium of Physical Activities (moderate physical activity MET values > 3.0 to < 6.0 and vigorous physical activity MET values > 6.0. Average minutes per week were calculated for overall MVPA. Change scores were obtained by subtracting average minutes per week of MVPA at baseline from average minutes per week of MVPA at 48 weeks. Prior 6-month reliabilities for self-reported MVPA were .76 (Stewart et al., 2001). Validity for African Americans was supported by correlations (0.16–0.32) with estimated VO2max (Resnicow et al., 2003).
Women were given a Lifecorder EX (NL2200) accelerometer (Suzuken Co., Ltd., Nagoya, Japan) to wear daily during waking hours. The device stores 200 days of steps and registers date, time, and total steps for each hour (Crouter et al., 2005). Data were screened for device wearing time, excluding days in the analyses that included fewer than 1,200 steps (Wilbur et al., 2016). Weeks with fewer than 3 days of valid data were excluded. Mean baseline steps per day were obtained by summing the days with valid step data in the week before the first behavioral meeting and dividing by the total number of days with valid data. To obtain the mean steps per day at 48 weeks, steps accrued during weeks with valid data in the 4 weeks before the 48-week assessment were summed and divided by the total number of weeks with valid data. Change scores were obtained by subtracting average steps per day at baseline from average steps per day at 48 weeks. Validity was demonstrated by no differences between Lifecorder EX and ActiGraph accelerometer outputs of steps and time in various intensity derivations in adults (McClain et al., 2007).
Self-Efficacy
Self-efficacy was measured with a modified McAuley’s Self-Efficacy for Overcoming Barriers to Exercise (McAuley, 1992) at 6 weeks postbaseline to allow an opportunity to experience the intervention and at 24 weeks. The measure consists of 14 items regarding confidence to overcome personal, social, work, and environmental barriers. Six items were modified to reflect barriers to lifestyle physical activity rather than structured exercise. Three additional items, specifically identified from the literature regarding barriers to women’s physical activity, were added: “family relationships and responsibilities,” “lack of encouragement from family,” and “personal safety” (Wilbur et al., 2003). The respondent rated her ability to continue to be physically active in the face of barriers on an 11-point scale from 0% (not at all confident) to 100% (highly confident). Change scores were obtained by subtracting average baseline self-efficacy from average 24-week self-efficacy. McAuley (1992) reported high Cronbach alphas (> .70) and construct validity with principal components analyses. The Cronbach alpha for this study was .94.
Social Support From Behavioral Group Meetings
Social support from the behavioral group meetings was measured with the 24-item Social Provision Scale for Physical Activity (Cutrona & Russell, 1987) at 24 weeks. There are four items for each of six social provisions, including attachment, social integration, reassurance of worth, reliable alliance, guidance, and opportunity for nurturance. The items are rated on a 4-point scale from 1 = strongly disagree to 4 = strongly agree. Following reverse coding of 11 negatively worded items, the items were summed for an overall score of 24 to 96. Higher scores indicate greater perceived social support from behavioral meetings. Cutrona and Russell (1987) reported Cronbach alphas ranging from .65 to .76 and concurrent validity with scores on the six social provisions predictive of loneliness. The Cronbach alpha for this study was .89.
Outcome Expectations/Realizations
Outcome expectations for physical activity were measured at baseline with a 14-item measure of expected changes scale (King et al., 1989). Items are physical (shape, appetite, fitness, etc.) and psychological attributes (depression, anxiety, sleep quality, etc.). Respondents were asked to select the number that most closely corresponds to how they would expect the item to change (if at all) during the next 6 months due to their becoming more physically active. Items were rated on an 11-point scale, including “get worse” (0), “no change” (1–3), “moderate improvement” (4–7), or “extreme improvement” (8–10). The respondents were also asked to select the one item most important to them (Wilcox et al., 2006). The score ranges for physical attributes, psychological attributes, and the overall measures are 0 to 10 each (Wilcox et al., 2006), with higher scores indicating greater outcome expectations. Cronbach alphas for this study were .87 for physical attributes and .92 for psychological attributes.
Outcome realizations (perceived change due to physical activity) were measured at 24 weeks (King et al., 1989). Respondents selected how they felt the physical and psychological attributes had changed over the past 6 months of the intervention (King et al., 1989). The items were scaled “got worse” (0), “no change” (1–3), “moderate improvement” (4–7), or “extreme improvement” (8–10). The realized expectations were scored in the same manner as outcome expectations. King et al. (1989) reported high test–retest reliability and concurrent validity. Cronbach alphas for this study were .89 for physical and .95 for psychological attributes.
According to guidelines by Neff and King (1995), participants were separated into four categories (Figure 1) to understand the interaction between baseline outcome expectations (physical, psychological, and overall benefits) and subsequently perceived outcome realizations after participating in the intervention: (a) disappointed optimists scored above the sample median on outcome expectations and below the sample median on outcome realizations; (b) optimistic realists scored above the sample median on both outcome expectations and outcome realizations; (c) surprised pessimists scored below the sample median on outcome expectations but above the median on outcome realizations; and (d) pessimistic realists scored below the sample median on both outcome expectations and outcome realizations.
Figure 1.
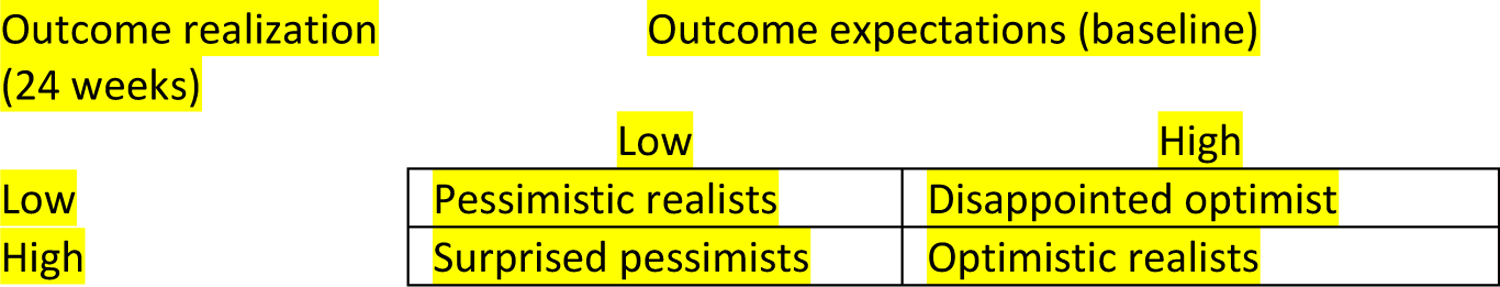
Categorization of Outcome Expectations and Outcome Realizations
Procedures
Institutional review board from Rush University approved the study protocol. Complete information related to the primary study RCT design and procedures are available elsewhere (Wilbur et al., 2016). Briefly, inclusion criteria were the following: (a) African American female; (b) ages 40 to 65 years; (c) self-reported MVPA less than three times a week; (d) systolic blood pressure < 160 mm Hg and diastolic blood pressure < 100 mm Hg; and (e) if diagnosed as a diabetic, A1C < 9. Exclusion criteria were: (a) major signs or symptoms suggestive of pulmonary or cardiovascular disease or disabilities that would prevent regular participation in physical activity, as determined by the Physical Activity Readiness Questionnaire (King et al., 2007); and (b) self-reported history of myocardial infarction or stroke. Further, women had to have a telephone and the ability to attend group behavioral meetings. Recruitment to the RCT targeted communities within a 2-mile radius of six community health care sites—each in a predominantly African American (≥ 90%) community, in or nearby low-income census tracts of Chicago (U.S. Census Bureau, n.d.). To ensure treatment fidelity, interventionists received training with a standardized manual and followed a second manual for intervention delivery (Wilbur et al., 2016). Table 1 provides a timeline of the intervention and associated data collection pertinent to these analyses.
Table 1.
Timeline for Data Collection Related to Secondary Data Analyses and Intervention
| Time | Data collection and Intervention |
|---|---|
| Prior to intervention | Measures (baseline) Self-efficacy (administered week 6) Outcome expectations Physical activity (self-report, device) |
| Weeks 1–24 | Intervention: adoption phase Group behavioral meetings total 5 meetings (held every 4–5 weeks over 24 weeks) Telephone condition (each group for behavioral meetings received a different condition) Personal motivational telephone calls (between behavioral meetings total 6) Automated telephone calls with motivational tips (between behavioral meetings total 6) No telephone calls Measures (24 weeks) Outcome realizations Social support from behavioral meetings |
| Weeks 25–48 | Intervention: maintenance phase Behavioral meetings (one delivered at approximately week 36) Telephone condition Personal motivational calls (1 call before and 1 call after the behavioral meeting) Automated motivational tips (total 1 before and 1 after behavioral meeting) No calls |
| End intervention | Measures Physical activity (self-report, device) |
Statistical Analysis
A paired comparison t-test was done to determine change in self-efficacy at 6 weeks to the end of the adoption phase (24 weeks). Pearson correlations were completed among social cognitive variables (self-efficacy change at 24 weeks, outcome realizations at 24 weeks, social support at 24 weeks), and change in self-reported weekly minutes of MVPA and change in device daily steps from baseline to 48 weeks. Hypothesis 1 was tested using a two stepwise theoretical hierarchical multiple regression analyses (Pedhazur, 1982) with change in physical activity (self-report and device) from baseline to 48 weeks as the dependent variables and change in self-efficacy from 6 weeks to 24 weeks, physical- and psychological-outcome realizations at 24 weeks, and social support from behavioral meetings at 24 weeks as independent variables in each model. Frequencies were used to describe the four-outcome expectation/realization categories. Hypothesis 2 was tested using analysis of variance (ANOVA) and Tukey comparisons.
Results
Independent Relationships Between Social Cognitive Variables and Change in Physical Activity From Baseline to 48 Weeks
At 6 weeks postbaseline, women had an average of 72.84% confidence in their ability to overcome barriers (self-efficacy) to physical activity, and the average declined to 68.17% at 24 weeks (F(2,223) = 6.15 p = .014). Bivariate Pearson product-moment correlations revealed that self-efficacy improvement at 24 weeks was associated with higher physical- and psychological-outcome realizations at 24 weeks and higher social support from behavioral meetings at 24 weeks (see Table 2). Higher social support from group meetings at 24 weeks was associated with higher physical and psychological outcome realizations at 24 weeks.
Table 2.
Correlations Among Social Cognitive Variables and Physical Activity
| 1 | 2 | 3 | 4 | 5 | ||
|---|---|---|---|---|---|---|
|
1 |
Social cognitive variables Self-efficacy (change 6-weeks to 24-weeks) |
|||||
| 2 | Physical-outcome realizations (at 24-weeks) | .194** | ||||
| 3 | Psychological-outcome realizations (at 24-weeks) | .212** | .779** | |||
| 4 | Group social support at 24-weeks | .203** | .282** | .259** | ||
|
5 |
Physical activity Physical activity: self-report minutes per week MVPA (change baseline to 48 weeks) |
.031 |
.255** |
.260** |
.099 |
|
| 6 | Physical activity: device steps per day (change from baseline to 48 weeks) | .288** | .083 | .031 | −.056 | .114 |
Note. 1 = self-efficacy, 2 = physical-outcome realizations, 3 = psychological-outcome realizations, 4= group social support. 5 = physical activity. Self-report: MVPA = moderate/vigorous physical activity.
p = .01 level (2-tailed).
Correlations of the social cognitive variables with physical activity revealed that greater self-efficacy improvement at 24 weeks was associated with greater improvement in device daily steps from baseline to 48 weeks (see Table 2). However, there was no significant association between self-efficacy change at 24 weeks and change in self-reported minutes per week of MVPA from baseline to 48 weeks. There was no association between social support from group meetings at 24 weeks and either change in minutes per week of MVPA or device daily steps from baseline to 48 weeks. Higher physical and psychological outcome realizations at 24 weeks were associated with greater improvement in self-reported minutes per week of MVPA from baseline to 48 weeks. However, there was no association between outcome realizations and change in device daily steps.
Hypothesis 1. Combined Effects of Social Cognitive Variable on Change in Physical Activity From Baseline to 48 Weeks
In the final hierarchical multiple regression analyses model for change in self-reported minutes per week of MVPA, only psychological-outcome realizations at 24 weeks were independently and positively associated with change in self-reported MVPA from baseline to 48 weeks (see Table 3). Higher psychological-outcome realizations were associated with greater improvement in self-reported MVPA from baseline to 48 weeks. In the final model for change in device daily steps, only change in self-efficacy for overcoming barriers from 6 weeks to 24 weeks was independently and positively associated with change in device daily steps from baseline to 48 weeks (see Table 3). Greater positive change in self-efficacy was associated with greater improvement in device daily steps.
Table 3.
Final Regressions of Change in Physical Activity (Self-Report, Device) from Baseline to 48 weeks on Social-Cognitive Constructs
| Variable | Model physical activity self-report MVPAa | Model physical activity device stepsb | ||||
|---|---|---|---|---|---|---|
| Standardized coefficient | t | p | Standardized coefficient | t | p | |
| Constant | −.452 | .000 | 4.05 | <.001 | ||
| Psychological outcome realizations 24-weeksc | .26 | 4.300 | .000 | - | ||
| Self-efficacy change (6-weeks to 24-weeksc | - | .28 | 3.674 | <.001 | ||
Note. MVPA = moderate/vigorous physical activity
R2= .06, F(1,256) 18.49, p=<.001
F(1,149) 13.49, p=<.001
This is the independent variable retained in the final regression model using a hierarchical /theoretical regression analysis.
Hypothesis 2: Outcome Expectation/Realization Groups and Change in Physical Activity at 48 Weeks
ANOVA showed significant differences between overall- and physical-outcome realization groups (pessimistic realist, surprised pessimist, disappointed optimist, optimistic realist) on change in self-reported minutes per week of MVPA from baseline to 48 weeks (see Table 4). Tukey post-hoc testing revealed for both overall- and physical-outcome realization groups, pessimistic realists had (p < .01) less improvement in minutes per week of MVPA than optimistic realists. For overall-outcome realizations, disappointed optimists had less improvement in minutes per week of MVPA than pessimistic realists. For physical-outcome realizations, disappointed optimists had greater improvement in minutes per week of MVPA than pessimistic realists. No differences were found between psychological-outcome realization groups on change in self-reported minutes per week of MVPA. Further, there were no differences between overall-, physical-, or psychological-outcome realization groups for change in device daily steps from baseline to 48 weeks.
Table 4.
Change in Physical Activity from Baseline to 48 Weeks by Outcome Expectation/Realization Category
| Change in physical activity self-report MVPA(minutes/week) a | Change in physical activity device (steps/day)b | |||||
|---|---|---|---|---|---|---|
| Outcome expectation/ realization category | n (%) | M(SD) | ANOVA | n (%) | M(SD) | ANOVA |
| Overall benefits | F (3,256) 4.56, p < .01 | F (3,174) .14 p = .932 | ||||
| Pessimistic realist | 80(30.76) | 114.37(346.89) | 53(29.77) | 815.49(2605.82) | ||
| Surprised pessimist | 53(20.38) | 236.60(397.74) | 37(20.78) | 910.23(2479.80) | ||
| Disappointed optimist | 47(18.07) | 77.55(284.02) | 31 (17.41) | 538.81(1949.59) | ||
| Optimistic realist | 80(30.76) | 277.50(382.29) | 57(32.02) | 666.18(2919.18) | ||
| Physical benefits | F (3,256) 4.97, p < .01 | |||||
| Pessimistic realist | 79(30.38) | 306.12(412.56) | 48(26.96) | 592.71(2741.05) | F (3,174) .30 p = .825 | |
| Surprised pessimist | 57(21.92) | 203.68(355.25) | 40(22.47) | 1075.29(2201.43) | ||
| Disappointed optimist | 53(20.38) | 134.15(347.80) | 37 (20.78) | 677.38(1821.07) | ||
| Optimistic realist | 71(27.30) | 306.12(412.56) | 53 (29.77) | 626.17(3085.72) | ||
| Psychological benefits | F(3,259) 2.32 p = .75 |
F (3,174) .36 p = .776 |
||||
| Pessimistic realist | 66(25.38) | 127.50(346.22) | 46(25.84) | 878.61(2617.50) | ||
| Surprised pessimist | 65(25.00) | 227.30(397.94) | 46(25.84) | 937.88(2631.93) | ||
| Disappointed optimist | 37(14.23) | 127.50(346.22) | 26(14.60) | 321.96(1833.78) | ||
| Optimistic realist | 92(35.38) | 231.52(377.12) | 65(36.51) | 677.49(2771.01) | ||
Note. MVPA = moderate/vigorous physical activity, ANOVA = analysis of variance
N=260
N=178
Discussion
This study examined self-efficacy, group social support, and outcome expectations/realizations in relationship to subsequent physical activity in midlife African American women. When SCT constructs were considered together, contrary to our hypothesis, only improvement in self-efficacy for overcoming physical activity barriers over the adoption phase of the intervention was associated with improvement in physical activity from baseline to 48 weeks measured by a daily-steps device. However, this is consistent with earlier systematic reviews that found self-efficacy to be consistently associated with improvement in physical activity (Mama et al., 2015; Young et al., 2014). Earlier studies tended to examine self-reported physical activity, but in our study, there was no association between improvement in self-efficacy and improvement in self-reported MVPA. We speculate that the device gave the women feedback on their steps in real-time; thus, there was better concordance between perceived self-efficacy and daily device steps than self-reported physical activity.
It is interesting that, at the 24-week end of the intervention’s adoption phase, women had a decrease in self-efficacy for overcoming barriers to physical activity. This decrease is consistent with an earlier study of urban midlife African American and Caucasian women that found women reported higher self-efficacy at the start of an intervention than at the end of a 24-week adoption phase (Wilbur et al., 2003). The authors speculated that high baseline self-efficacy reflects the optimism of women who joined a physical activity program specifically to become more active. When faced with the real challenges to becoming more active over a 24-week period, participants readjusted their confidence in overcoming barriers downward (McAuley & Blissmer, 2000). To address these earlier findings, the barriers questionnaire in the primary RCT was administered approximately 6 weeks following the start of the intervention (Wilbur et al., 2016). The intent was to assure that women had time to experience some initial challenges. Also, the intervention content in the behavioral meetings focused on setting realistic physical activity goals in anticipation of setbacks in their ability to become more active. However, mean self-efficacy for overcoming physical activity barriers at 6 weeks after the start of the intervention was even somewhat higher than self-efficacy at baseline in the earlier study (Wilbur et al., 2003). At 24 weeks, or the end of the intervention adoption phase, self-efficacy was the same for both studies. Clearly, close attention needs to be paid to identifying women who begin to lose confidence in overcoming barriers after 6 weeks of being in a physical-activity program.
Contrary to our first hypothesis, perceived social support from women who participated with them in the behavioral meetings did not contribute to improved physical activity by self-reported or device-measured physical activity at 48 weeks. Likewise, an earlier study (Brassington et al., 2002) included a measure of support from exercise classmates and found no association with subsequent physical activity improvement. Most studies that have included social support have identified the effect of support from just family and friends (Peterson & Cheng; 2011; Young & Stewart, 2006). It may be that social support from lasting familial and friend relationships contributes to improvement at 48 weeks or end of maintenance more than time-limited social support from the behavioral meetings.
Considered independently, both perceived higher physical and psychological outcome realizations at 24 weeks were associated with self-reported change in physical activity at 48 weeks. These findings are consistent with a previous study involving older adults in which higher fitness- and psychological-outcome realizations were associated with subsequent physical activity (Brassington et al., 2002). In the presence of one another, however, as well as with self-efficacy, it appears that psychological-outcome realizations had a stronger association with self-reported change in physical activity at 48 weeks.
To consider outcome expectations at the start of the intervention in relation to outcome realizations (Hypothesis 2), we examined outcome expectation/realization groups regarding change in physical activity at 48 weeks. As hypothesized, optimistic realists—women who had high initial outcome expectations for overall benefits and physical outcomes with high perceived realizations—showed the most improvement in self-report minutes per week of MVPA. Also, disappointed optimists—women who had high outcome expectations for overall benefits and physical outcomes but low perceived outcome realizations—had among the lowest improvement in self-reported minutes per week of MVPA. These findings mirror those of an earlier study of older women (Wilcox et al., 2006). Attention should likely be paid to more frequent assessment of women’s outcome realizations so interventions can be made early when perceived expected benefits are low.
A limitation of the primary study was that participants had higher education levels than the median norm for Chicago (Yonek & Hasnain-Wynia, 2011). Thus, findings may not represent all African American women in Chicago.
Conclusion
Our findings show that increased self-efficacy to overcome physical activity barriers and perceived outcome realizations following the intervention may be important intervention targets. A suggested next step in testing targets for physical activity interventions in African American women is conducting an intervention focused on realistic expectations for physical and psychological outcomes and more frequent self-efficacy assessments and perceived outcome realizations. Additional assessments could be followed by spending focused intervention time supporting self-efficacy for overcoming physical activity barriers and aligning physical- and psychological-outcome expectations with outcome realizations.
Acknowledgement:
Research reported in this publication was supported by the National Institute of Nursing Research of the National Institutes of Health under Award Number R01 NCT01700894. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors thank Dr. Pamela Semanik, Rush University College of Nursing, for her assistance editing the manuscript.
Footnotes
The authors have no conflicts of interest to report.
Ethical Conduct of Research: The research conducted for this manuscript were ethically conducted under the approval and supervision of the Rush University Institutional Review Board
Clinical Trial Registration: Trial registry: National Institute of Health, trial number NCT01700894, date of registration: October 4, 2012, first enrollment March 15, 2012, link https://clinicaltrials.gov/ct2/show/NCT01700894
References
- Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR, Tudor-Locke C, Greer JL, Vezina J, Whitt-Glover MC, & Leon AS (2011). Compendium of physical activities: A second update of codes and MET values. Medicine & Science in Sports & Exercise, 43, 1575–1581. [DOI] [PubMed] [Google Scholar]
- Anderson KJ, & Pullen CH (2013). Physical activity with spiritual strategies intervention: A cluster randomized trial with older African American women. Research in Gerontological Nursing, 6, 11–21. 10.3928/19404921-20121203-01 [DOI] [PubMed] [Google Scholar]
- Bandura A (2004). Health promotion by social cognitive means. Health Education & Behavior, 31, 143–164. 10.1177/1090198104263660 [DOI] [PubMed] [Google Scholar]
- Banks-Wallace J (2007). Outcomes from Walk the Talk: A nursing intervention for Black women. ABNF Journal, 18, 19–24. [PubMed] [Google Scholar]
- Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Jordan LC, Khan SS, Kissela BM, Knutson KL, … Virani SS (2019). Heart disease and stroke statistics–2019 update: A report from the American heart association. Circulation, 139, e56–e528. 10.1161/CIR.0000000000000659 [DOI] [PubMed] [Google Scholar]
- Brassington GS, Atienza AA, Perczek RE, DiLorenzo TM, & King AC (2002). Intervention-related cognitive versus social mediators of exercise adherence in the elderly. American Journal of Preventive Medicine, 23, 80–86. 10.1016/s0749-3797(02)00477-4 [DOI] [PubMed] [Google Scholar]
- Cleland CL, Tully MA, Kee F, & Cupples ME (2012). The effectiveness of physical activity interventions in socio-economically disadvantaged communities: A systematic review. Preventive Medicine, 54, 371–380. 10.1016/j.ypmed.2012.04.004 [DOI] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Lawrence Erlbaum Associates. [Google Scholar]
- Crouter SE, Schneider PL, & Bassett JD Jr. (2005). Spring-levered versus piezo-electric pedometer accuracy in overweight and obese adults. Medicine and Science in Sports and Exercise, 37, 1673–1679. 10.1249/01.mss.0000181677.36658.a8 [DOI] [PubMed] [Google Scholar]
- Cutrona CE, & Russell DW (1987). The provisions of social relationships and adaptation to stress. Advances in Personal Relationships, 1, 37–67. [Google Scholar]
- Eyler AA, Brownson RC, Donatelle RJ, King AC, Brown D, & Sallis JF (1999). Physical activity social support and middle- and older-aged minority women: Results from a US survey. Social Science & Medicine, 49, 781–789. 10.1016/S0277-9536(99)00137-9 [DOI] [PubMed] [Google Scholar]
- Fitzgibbon ML, Stolley MR, Schiffer L, Sharp LK, Singh V, & Dyer A (2010). Obesity reduction black intervention trial (ORBIT): 18-month results. Obesity, 18, 2317–2325. 10.1038/oby.2010.47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hornbuckle LM, Liu PY, Ilich JZ, Kim JS, Arjmandi BH, & Panton LB (2012). Effects of resistance training and walking on cardiovascular disease risk in African-American women. Medicine and Science in Sports and Exercise, 44, 525–533. 10.1249/mss.0b013e31822e5a12 [DOI] [PubMed] [Google Scholar]
- Jenkins F, Jenkins C, Gregoski MJ, & Magwood GS (2017). Interventions promoting physical activity in African American women: An integrative review. Journal of Cardiovascular Nursing, 32, 22–29. 10.1097/jcn.0000000000000298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King AC, Taylor CB, Haskell WL, & DeBusk RF (1989). Influence of regular aerobic exercise on psychological health: A randomized, controlled trial of healthy middle-aged adults. Health Psychology, 8, 305–324. 10.1037/0278-6133.8.3.305 [DOI] [PubMed] [Google Scholar]
- King AC, Friedman R, Marcus B, Castro C, Napolitano M, Ahn D, &; Baker L (2007). Ongoing physical activity advice by humans versus computers: The Community Health Advice by Telephone (CHAT) trial. Health Psychology, 26, 718–727. 10.1037/0278-6133.26.6.718 [DOI] [PubMed] [Google Scholar]
- Mama SK, McNeill LH, McCurdy SA, Evans AE, Diamond PM, Adamus-Leach HJ, & Lee RE (2015). Psychosocial factors and theory in physical activity studies in minorities. American Journal of Health Behavior, 39, 68–76. 10.5993/AJHB.39.1.8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAuley E, & Blissmer B (2000). Self-efficacy determinants and consequences of physical activity. Exercise and Sport Sciences Reviews, 28, 85–88. [PubMed] [Google Scholar]
- McAuley E (1992). The role of efficacy cognitions in the prediction of exercise behavior in middle-aged adults. Journal of Behavioral Medicine, 15, 65–88. 10.1007/bf00848378 [DOI] [PubMed] [Google Scholar]
- McClain JJ, Craig CL, Sisson SB, & Tudor-Locke C (2007). Comparison of Lifecorder EX and ActiGraph accelerometers under free-living conditions. Applied Physiology, Nutrition, and Metabolism, 32, 753–761. 10.1139/h07-060 [DOI] [PubMed] [Google Scholar]
- Neff KL, & King AC (1995). Exercise program adherence in older adults: The importance of achieving one’s expected benefits. Medicine, Exercise, Nutrition and Health, 4, 355–362. [Google Scholar]
- Newton RL Jr., & Perri MG (2004). A randomized pilot trial of exercise promotion in sedentary African American adults. Ethnicity & Disease, 14, 548–557. [PubMed] [Google Scholar]
- Parra-Medina D, Wilcox S, Salinas J, Addy C, Fore E, Poston M, & Wilson DK (2011). Results of the heart healthy and ethnically relevant lifestyle trial: A cardiovascular risk reduction intervention for African American women attending community health centers. American Journal of Public Health, 101, 1914–1921. 10.2105/AJPH.2011.300151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedhazur EJ, & Kerlinger FN (1982). Multiple regression in behavioral research: Explanation and prediction. Holt, Rinehart, and Winston. [Google Scholar]
- Peterson JA, & Cheng A-L (2011). Heart and soul physical activity program for African American women. Western Journal of Nursing Research, 33, 652–670. 10.1177/0193945910383706 [DOI] [PubMed] [Google Scholar]
- Resnicow K, McCarty F, Blissett D, Wang T, Heitzler C, & Lee RE (2003). Validity of a modified CHAMPS physical activity questionnaire among African-Americans. Medicine & Science in Sports & Exercise, 35, 1537–1545. 10.1249/01.mss.0000084419.64044.2b [DOI] [PubMed] [Google Scholar]
- Rhodes RE, & Nigg CR (2011). Advancing physical activity theory: A review and future directions. Exercise and Sport Sciences Reviews, 39, 113–119. 10.1097/JES.0b013e31821b94c8 [DOI] [PubMed] [Google Scholar]
- Speck BJ, Hines-Martin V, Stetson BA, & Looney SW (2007). An environmental intervention aimed at increasing physical activity levels in low-income women. Journal of Cardiovascular Nursing, 22, 263–271. 10.1097/01.JCN.0000278957.98124.8a [DOI] [PubMed] [Google Scholar]
- Stewart AL, Mills KM, King AC, Haskell WL, Gillis D, & Ritter PL (2001). CHAMPS physical activity questionnaire for older adults: Outcomes for interventions. Medicine & Science in Sports & Exercise, 33, 1126–1141. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. (n.d.). State and county quick facts. Retrieved April 6, 2021, from https://www.census.gov/quickfacts/fact/table/US/PST045219
- Wilbur J, Chandler P, Dancy B, Choi J, & Plonczynski D (2002). Environmental, policy, and cultural factors related to physical activity in urban, African American women. Women & Health, 36, 17–28. 10.1300/J013v36n02_02 [DOI] [PubMed] [Google Scholar]
- Wilbur J, McDevitt JH, Wang E, Dancy BL, Miller AM, Briller J, Ingram DLM, Nicola TL, Ju S, & Lee H (2008). Outcomes of a home-based walking program for African-American women. American Journal of Health Promotion, 22, 307–317. 10.4278/ajhp.22.5.307 [DOI] [PubMed] [Google Scholar]
- Wilbur J, Michaels Miller A, Chandler P, & McDevitt J (2003). Determinants of physical activity and adherence to a 24-week home-based walking program in African American and Caucasian women. Research in Nursing & Health, 26, 213–224. 10.1002/nur.10083 [DOI] [PubMed] [Google Scholar]
- Wilbur J, Miller AM, Fogg L, McDevitt J, Castro CM, Schoeny ME, Buchholz SW, Braun LT, Ingram DM, Volgman AS, & Dancy BL (2016). Randomized clinical trial of the women’s lifestyle physical activity program for African-American women: 24- and 48-week outcomes. American Journal of Health Promotion, 30, 335–345. 10.1177/0890117116646342 [DOI] [PubMed] [Google Scholar]
- Wilcox S, Castro CM, & King AC (2006). Outcome expectations and physical activity participation in two samples of older women. Journal of Health Psychology, 11, 65–77. 10.1177/1359105306058850 [DOI] [PubMed] [Google Scholar]
- Yancey AK, Lewis LB, Guinyard JJ, Sloane DC, Nascimento LM, Galloway-Gilliam L, Diamant AL, & McCarthy WJ (2006). Putting promotion into practice: The African Americans building a legacy of health organizational wellness program. Health Promotion Practice, 7, 233S–246S. 10.1177/1524839906288696 [DOI] [PubMed] [Google Scholar]
- Yanek LR, Becker DM, Moy TF, Gittelsohn J, & Koffman DM (2001). Project Joy: Faith based cardiovascular health promotion for African American women. Public Health Reports, 116, 68–81. 10.1093/phr/116.s1.68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yonek J, & Hasnain-Wynia R (2011). A profile of health and health resources within Chicago’s 77 communities. Northwestern University: Institute for Healthcare Studies, 14. [Google Scholar]
- Young DR, & Stewart KJ (2006). A church-based physical activity intervention for African American women. Family & Community Health, 29, 103–117. [DOI] [PubMed] [Google Scholar]
- Young MD, Plotnikoff RC, Collins CE, Callister R, & Morgan PJ (2014). Social cognitive theory and physical activity: A systematic review and meta-analysis. Obesity Reviews, 15, 983–995. 10.1111/obr.12225 [DOI] [PubMed] [Google Scholar]


