On 11 March 2020, the novel coronavirus disease COVID‐19 was declared a pandemic. As a response, most countries in the world enforced strict lockdown policies including the closure of preschools and schools. Sweden imposed less rigorous restrictions, and preschools and primary schools remained open. 1 Recommendations from the Public Health Agency of Sweden included physical distancing of 2 metres, encouragement to work from home to the greatest possible extent, minimising contacts outside the family, frequent hand‐washing and home quarantine from work/school and preschool in case of infectious symptoms with two additional days after recovery, which was also incited with economic compensation for the absence. 1 However, there was no recommendation of general usage of face masks in the community and preschools and primary schools remained open, while upper secondary schools switched to distance learning for three months during 2020. 1 While hand hygiene has been known to prevent the spread of bacterial infections since the beginning of the 19th century, there are more contradicting results regarding the impact of school closures and the use of face masks to prevent the spread of communicable diseases. 2
We aimed to assess the number of emergency visits during 2020 as compared to the two previous years at the two paediatric hospitals in Stockholm. These two hospitals cover approximately 514.000 (24%) of all Swedish children 0‐18 years with about 70 000 paediatric visits per year 2018‐2019. In Sweden, you do not need a referral from a primary care physician to seek medical care at a paediatric emergency unit. The data on ICD‐10 billing codes were retrieved from the paediatric emergency records. We assessed the total number of paediatric emergency visits as well as visits for lower respiratory tract infections (LRTI) (ICD‐10 A37, J09‐J22), gastroenteritis (A00‐G09, A11) and urinary tract infections (UTI) (N10.0, N30.9) comparing cumulative incidences for the years 2018‐2019 with 2020 using chi‐squared tests. The study was approved by the Swedish Ethical Review Authority (Dnr: 2020‐02061 and 2020‐04717).
Results show a clear reduction in the number of paediatric emergency visits for the year 2020 (predominantly for the period March‐June) as compared to the two previous years. The change is temporally associated with the announcement of community transmission of SARS‐Cov‐2 in Sweden, along with the hygiene recommendations from the Public Health Agency of Sweden (p<0.001) (Figure 1). The same trend was observed when specifically assessing the visits for LRTI (cumulative incidence 0.24% in 2020 versus 0.57% p<0.001) and gastroenteritis (cumulative incidence 0.26% in 2020 versus 0.87%, p<0.001) whereas the number of UTI visits was slightly increased in 2020 as compared to the previous two years (0.22% versus 0.20%, p=0.01). In Stockholm, the SARS‐CoV‐2 transmission followed a two‐wave spreading pattern in 2020 with a first wave in March‐July and a second wave starting in late October continuing into February 2021. Testing for SARS‐CoV‐2 was performed on most admitted patients but not routinely performed on all children presenting with respiratory symptoms.
FIGURE 1.
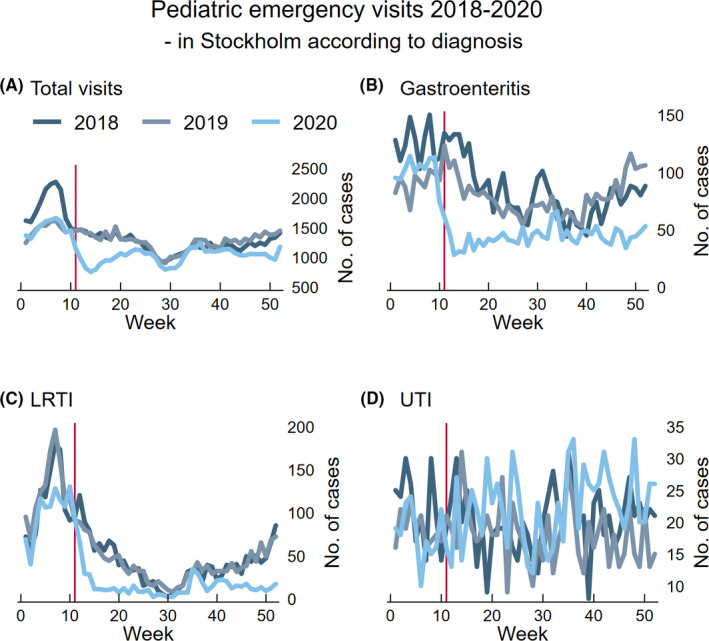
Number of paediatric emergency visits per week at two paediatric hospitals in Stockholm during 2018–2020 expressed as A) total number of emergency visits and according to the discharge diagnosis of B) gastroenteritis (ICD‐10 code: A00‐A09, R11), C) lower respiratory tract infections (ICD‐10 code: A37, J09‐ J22) and D) urinary tract infections (ICD‐10 codes: N10.0, N30.9). Red vertical line indicating week 11 when COVID‐19 was declared a pandemic. Abbreviations: LRTI, lower respiratory tract infection; UTI, urinary tract infection.
School closures have been a central part of most countries disease preventive strategies, and hence, it has been associated with mitigation of the COVID‐19 disease and the reduction in the spread of communicable diseases in children. 3 , 4 As the Swedish strategy deviated from most other countries with less strict lockdown restrictions and open preschools and primary schools, it offers a unique opportunity to assess the effect of other behavioural changes as explained in the introduction, including basal hygiene routines, on the transmission of paediatric communicable diseases. We report a dramatic reduction in paediatric emergency visits for two communicable diseases mainly with mainly contact/droplet transmission, which was temporally associated with the recommendations from the Public Health Agency of Sweden on behavioural changes including physical distancing, improved basal hygiene and home quarantine when experiencing symptoms of infection. It is possible that some of the effect could be explained by a change in health‐seeking behaviour and a raised threshold for seeking medical care at the emergency department due to fear of acquiring COVID‐19. However, as a control diagnosis, we assessed the number of visits for UTI, a communicable disease without contact/droplet transmission. Visits for UTI did not decrease between the studied periods, suggesting that the observed decline in emergency visits was not fully explained by a change in health‐seeking behaviour. We did not have data on primary care visits and would hence have missed an increase in visits for LRTI and gastroenteritis in the primary care during the study period. There is also a risk of misclassification bias due to changes in coding routines over the years as our analysis was based on billing codes. Further, it is possible that the introduction of SARS‐Cov‐2 interfered with the normally circulating viruses by triggering immunological changes. Such viral interference has been described for the pandemic influenza A(H1N1) pdm09‐virus. 5 Finally, the respiratory syncytial virus (RSV) season in Sweden 2019/2020 was mild and the levels of circulating RSV were low already at the beginning of 2020. This likely partly explained the low number of LRTI visits during the first month of 2020. Yet, our results suggest that the recommendation of behavioural changes including physical distancing and improved basal hygiene routines, but without preschool or school closures or general usage of face masks in the community, likely contributed to the observed decrease in disease transmission of LRTIs and gastroenteritis in children. This raises the question to what extent some of these recommendations can and should be extended in the postpandemic era.
CONFLICT OF INTEREST
None declared.
ACKNOWLEDGEMENT
We would like to acknowledge the EPISODES network (study registry ID: https://doi.org/10.1186/ISRCTN91495258) for facilitating the data extraction.
Rhedin SA, Ryd Rinder M, Hildenwall H, et al. Reduction in paediatric emergency visits during the COVID‐19 pandemic in a region with open preschools and schools. Acta Paediatr. 2021;110:2802–2804. 10.1111/apa.15978
FUNDING INFORMATION
SAR was supported by Region Stockholm (clinical postdoctorial appointment), HH was supported by the Swedish Society of Medicine (COVID‐19 project grant SLS‐938140), EH was supported by Region Stockholm (20190400) and the Swedish Research Council (2019‐31 01157), and EM was supported by grants from the Swedish Research Council (2020‐02171 and 2016‐03086). RN was supported by NIHR Award ACL‐2018‐021‐007. TA was supported by Region Stockholm (ALF‐20180292 grant) and the Swedish Research Council (2018‐02770).
[Correction added on 2 July 2022, after first online publication: The term "G00‐G09, R11" has been changed as "A00‐A09, R11" in this version.]
REFERENCES
- 1. Ludvigsson JF. The first eight months of Sweden's COVID‐19 strategy and the key actions and actors that were involved. Acta Paediatr. 2020;109(12):2459‐2471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Aiello AE, Murray GF, Perez V, et al. Mask use, hand hygiene, and seasonal influenza‐like illness among young adults: a randomized intervention trial. J Infect Dis. 2010;201:491‐498. [DOI] [PubMed] [Google Scholar]
- 3. Gavish R, Levinsky Y, Dizitzer Y, et al. The COVID‐19 pandemic dramatically reduced admissions of children with and without chronic conditions to general paediatric wards. Acta Paediatr. 2021. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Polcwiartek LB, Polcwiartek C, Andersen MP, et al. Consequences of coronavirus disease‐2019 (COVID‐19) lockdown on infection‐related hospitalizations among the pediatric population in Denmark. Eur J Pediatr. 2021;180(6):1955‐1963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chan KF, Carolan LA, Korenkov D, et al. Investigating viral interference between influenza A virus and human respiratory syncytial virus in a ferret model of infection. J Infect Dis. 2018;218:406‐417. [DOI] [PMC free article] [PubMed] [Google Scholar]


