Abstract
Aim
Our study aimed to understand the acceptance level of the COVID-19 vaccine and its determinants among the adult Bangladeshi population.
Methodology
This cross-sectional study was conducted in all eight divisions of Bangladesh. Data from 7,357 adult respondents were collected between January 17 and February 2, 2021, using a self-administered semi-structured questionnaire. Statistical software STATA (Version 16.1) was used for all analyses.
Results
The majority of study participants were from the Dhaka division (34.24%). The most common age group was ≤30 years (46.18%). Almost two-thirds of respondents were male (65.50%) and married (67.76%). A large portion (79.85%) of people who had positive vaccine intentions believed that vaccination should be made mandatory for everyone. The majority of the respondents thought that the vaccine would work against COVID-19 infection (67%). In the binary logistic regression analysis, participants who had the education level of graduation or above (AOR = 1.80), age ≥50 years (AOR = 1.97), students (AOR = 2.98), monthly income ≥41,000 BDT (AOR = 2.22), being resident of rural area (AOR = 2.24), respondents from Khulna division (AOR = 6.43) were more likely to receive a COVID-19 vaccine. Those who had family members diagnosed with COVID-19 (AOR = 1.24), presence of chronic disease (AOR = 0.72), and those who were vaccinated in the last few years (AOR = 1.32) were also more likely to accept the COVID-19 vaccine.
Conclusion
Most of the respondents were willing to be vaccinated based on the belief that the vaccine will work against COVID-19. As rumors are generating daily, there is a need for policy-level initiative and evidence-based mass media promotion to keep inspired the general Bangladeshi people to accept the COVID-19 vaccine whenever it will be available at the individual level.
Keywords: COVID-19, Vaccine, Acceptance, Hesitancy, Bangladesh
COVID-19; Vaccine; Acceptance; Hesitancy; Bangladesh.
1. Introduction
The deadliest pandemic since World War II, the COVID-19 pandemic, caused a staggering impact not only on health but also on socioeconomic conditions [1]. With the loss of 2.63 million lives globally due to COVID-19 [2], 10 million people are at the risk of severe economic hardship [3]. Simultaneously, the count of malnourished people may rise to 132 million [3]. In Bangladesh, the Government confirmed the earliest COVID-19 case on March 8, 2020, followed by a Government imposed total lockdown [4]. Until January 31, 2021, 535 thousand cases were detected, among them 89.6% recovered, and 8,730 died due to COVID-19 infection as of March 26, 2021. Most of the COVID-19 victims were from Dhaka city, with 57.7% of total cases and more than 50% of the country's total deaths [5]. The Bangladesh Government took necessary steps to build awareness throughout the country by ensuring diagnosis, quarantine of suspected cases, isolation of infected patients, enforcement of social distancing, mask-wearing, and personal hygiene maintenance. The Government also announced stimulant financial packages of approximately USD 11.90 billion [6]. To organize, DGHS developed the 'National Preparedness and Response Plan' [7]. The plan's implementation is that there are now 10,331 general beds and 595 ICU beds dedicated to the COVID-19 affected patients [5]. Lockdown was relaxed after eight weeks to revive the failing economy [8]. Though all these steps mildly slowed down the spread of the pandemic, only vaccination of the mass population has a chance of entirely eradicating the Coronavirus.
Though a vaccine might never be fully effective, full coverage of vaccination throughout a community can significantly improve disease control [9]. Vaccine hesitancy is a continuum between vaccine approval and denial, which has become the most distinct public health issue in the current situation. It "refers to delays in acceptance or refusal of vaccines despite the availability of vaccination services [10]. Even though vaccine hesitancy is a worldwide social phenomenon, it remains a crisis among the population. Karafillakis et al. found vaccine hesitancy mostly related to safety concerns related to worry of adverse effects from vaccination in Europe [11]. On the other hand, a US study found vaccine hesitancy prevailing in the minority groups (Black Americans) [12]. In India, limited knowledge of vaccination and fear of side effects are reasons for vaccine hesitancy [13].
A few studies have been conducted to investigate the reasons behind vaccine hesitancy in the South Asian region, including Bangladesh [14, 15]. But none of those studies was effective enough to portray the actual picture of the current scenario due to lack of generalizability. However, vaccine acceptance among the general population nationwide is necessary to be explored to ensure herd immunity. Consequently, we performed this study to determine the underlying factors behind vaccine acceptance and people's notion behind the general population's hesitancy.
2. Methodology
2.1. Design
We conducted this cross-sectional survey, including all Bangladeshi administrative divisions, between January 17 to February 2, 2021. Data were collected from participants by face-to-face interviews and self-administered method where appropriate.
2.2. Study procedures
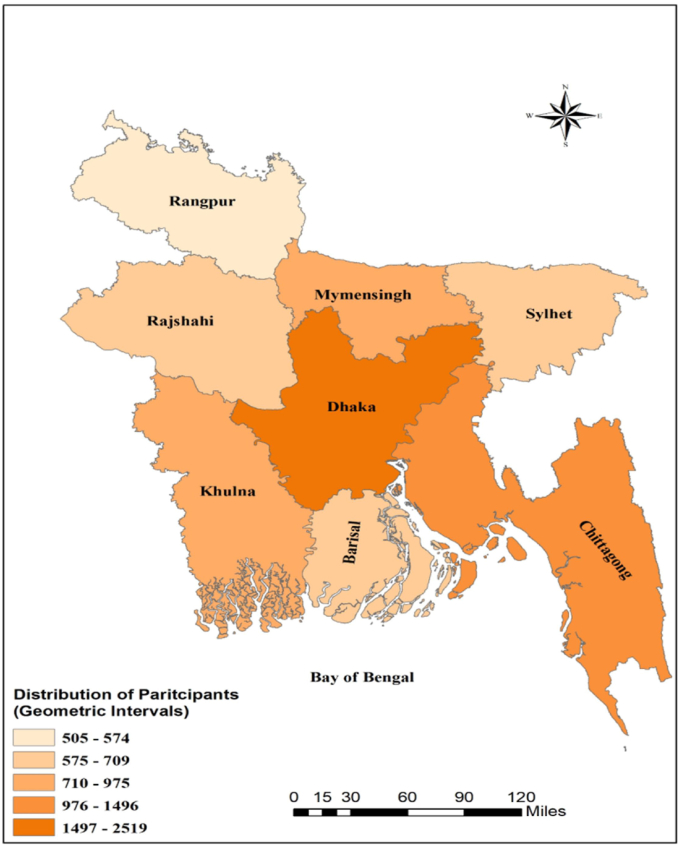
We approached adults aged 18 years or above with no mental illness from eight Bangladeshi divisions, i.e., Dhaka, Mymensingh, Chattogram, Khulna, Rajshahi, Sylhet, Rangpur, and Barishal. A team of 23 experienced researchers conducted and monitored the whole data collection procedure. As a convenience sampling technique was used, the interviewers were instructed to approach as many people as possible irrespective of their varying class, caste, and socioeconomic background to redeem our data's representation. We took explicit informed consent from all approached individuals. Our researchers gave the voluntary participants detailed information about the survey and a thorough explanation when they failed to understand specific questions during the interview. The participants were then given the questionnaire to complete the answers on their own. A face-to-face interview was conducted using the questionnaire if the participant was unable to read. A total of 7,357 people completed the study from our approached population; among them, 2,519 were from Dhaka, 900 were from Chattogram, 721 were from Khulna, 718 were from Mymensingh, 690 were from Barisal, 631 were from Sylhet, 583 were from Rajshahi, and 505 were from Rangpur (Figure 1). We excluded people who did not like to participate or were not interested in giving consent.
Figure 1.
Division wise distribution of the study participants (Created with ArcGIS version 10.5).
2.3. Measures
This study used a semi-structured questionnaire consisting of questions to assess the impact of COVID-19 and attitude and beliefs towards COVID-19 and the vaccine. The term COVID-19 was used instead of Coronavirus Disease SARS-CoV-2 infection for better comprehension of the general population. We divided the questionnaire into the following sections: socio-demographic information, the impact of COVID-19, previous vaccinations, attitude and belief on COVID-19 and the vaccine, and intention behind taking the vaccine. We developed a draft questionnaire based on the tool used by Sherman et al. 2020 [16]. The original questionnaire was modified and designed in English, then translated to Bengali. The two questionnaires were then compared, and the authors settled their dissimilarities in discussion with the research assistants. In the general information section, the participants were asked to write the interview date, name, and current address (district, division).
For information on the intention to receive a vaccine, a couple of queries were used ("When a coronavirus vaccination becomes available to you, are you going to take one?" and "Please specify why you are not willing or not sure to take the vaccine?"). The first question responses were 'yes' and 'no,' where the "yes" represented acceptance, and the "no" was considered hesitancy/resistance. The first version of the questionnaire was authenticated step by step. At first, the supervisor and the co-authors provided carefully observed feedback regarding the intelligibility, relativeness, and implication of the questionnaire. Next, the co-authors ran a trial study with 200 participants. Then we received the comments from the participants on making the questionnaire short and straightforward. We selected participants from different socioeconomic backgrounds for the pilot study where the public was involved in developing survey materials. Participants' adjustments were accepted and incorporated into the study to ensure the study's consistency with current research. All the authors settled for the final version of the questionnaire after a focused group discussion and rolled out the questionnaire for starting the survey procedure. The complete questionnaire has been shared as supplementary material.
2.4. Statistical analysis
We performed descriptive analysis to present the socio-demographic characteristics of 7,357 respondents from all eight administrative divisions of Bangladesh. We visualized the nominal variables as frequencies and proportions. The associations of beliefs & attitudes towards COVID-19 and its vaccine & vaccine acceptance intention were assessed using the Chi-square. The multivariable binary logistic regression analysis was performed to determine the association of socio-demographic and health indicators with COVID-19 vaccine acceptance. Adjusted odds ratio (AOR) with corresponding 95% confidence interval were presented to compare associations of socio-demographic and health indicators with vaccine acceptance. Statistical software STATA (Version 16.1) was used for the fundamental analyses. All tests were two-tailed, and we accepted p-values less than 0.05 as statistically significant.
2.5. Ethical consideration
Many of the methods were applied consistently following the Ethical Review Committee (ERC) ethical guidelines of North South University, Bangladesh (2021/OR-NSU/IRB-No.0304). Wherever possible, the moral norms outlined in the 1964 Declaration of Helsinki and its subsequent revisions, as well as equivalent moral principles, were followed. We obtained written informed consent from each one of the study's participants during the face-to-face interviews.
3. Results
The demographic table (Table 1) showcases the socio-demographic attributes of the study participants. This study included 7,357 participants from all over Bangladesh. Geographically, although the majority of the study participants were from the Dhaka division (n = 2519, 34.24%), a minimum involvement of 500 participants was ensured from each division during this study. The most common age group was ≤30 years (n = 3394, 46.18%). Almost two thirds of respondents were male (n = 4819, 65.50%) and married (n = 4985, 67.76%). Majority of our respondents were graduates (≤17 years of schooling) (n = 1895, 25.76%) followed by passed secondary or equivalent education (≤10 years of schooling) (n = 1762, 23.95%). Service holders (n = 2877, 39.16%) participated were more than any other occupation. 977 (13.28%) of the participants were Healthcare Workers. The largest income group (n = 4,167, 56.76%) of our study was people who earned ≤20,000 BDT. The majority of participants were urban dwellers (n = 4,212, 57.27%) in this study. Almost equal portion of participants belonged to small (≤4 people) (n = 3,466, 47.43%) and Large (≥5 people) (n = 3,841, 52.57%) families. A plethora of people with varying levels of education and involvement of the 3rd gender group are noteworthy features.
Table 1.
(Demographic table): Sociodemographic features of population of the survey.
| Characteristics | Level | n (%) |
|---|---|---|
| Age (Years) | ≤30 | 3,394 (46.18) |
| 31–50 | 3,069 (41.76) | |
| >50 | 887 (12.07) | |
| Total | 7,350 (100.00) | |
| Gender | Male | 4,819 (65.59) |
| Female | 2,528 (34.41) | |
| Total | 7,347 (100.00) | |
| Marital Status | Married | 4,985 (67.76) |
| Unmarried | 2,214 (30.09) | |
| Divorced/widowed/separated | 158 (2.15) | |
| Total | 7,357 (100.00) | |
| Education (Years of schooling) | No or primary education (≤5) | 1,296 (17.62) |
| Secondary or equivalent (≤10) | 1,762 (23.95) | |
| Higher secondary or diploma (≤12) | 1,612 (21.91) | |
| Graduate (≤17) | 1,895 (25.76) | |
| Postgraduate (≥18) | 792 (10.77) | |
| Total | 7,357 (100.00) | |
| Occupation | Service Holder† | 2,877 (39.16) |
| Businessperson | 1,324 (18.02) | |
| Student | 1,262 (17.18) | |
| Others‡ | 1,884 (25.64) | |
| Total | 7,347 (100.00) | |
| Health Care Worker | No | 6,380 (86.72) |
| Yes | 977 (13.28) | |
| Total | 7,357 (100.00) | |
| Monthly income (BDT) | ≤20000 | 4,162 (56.76) |
| 20001–40000 | 2,080 (28.36) | |
| ≥40001 | 1,091 (14.88) | |
| Total | 7,333 (100.00) | |
| Residence | Rural | 1,979 (26.91) |
| Semi-urban | 1,164 (15.83) | |
| Urban | 4,212 (57.27) | |
| Total | 7,355 (100.00) | |
| Family size | Small (≤4) | 3,466 (47.43) |
| Large (≥5) | 3,841 (52.57) | |
| Total | 7,307 (100.00) | |
| Division | Barisal | 690 (9.38) |
| Chattogram | 990 (13.46) | |
| Dhaka | 2,519 (34.24) | |
| Khulna | 721 (9.80) | |
| Mymensingh | 718 (9.76) | |
| Rajshahi | 583 (7.92) | |
| Rangpur | 505 (6.86) | |
| Sylhet | 631 (8.58) | |
| Total | 7,357 (100.00) |
Government and private jobholders.
Others including farmers, day laborers, rickshaw pullers, van drivers, auto drivers, independent workers, homemakers, retired, and unemployed.
Chi-square table (Table 2) described the association between people's attitudes, beliefs, and intentions to accept COVID-19 vaccines. We observed more people were willing to accept the vaccine regardless of worrying about COVID-19 infection. In the hesitant group, about two-thirds of people did not feel worried about the COVID-19 infection (65.90%). An almost equal proportion of participants believed in the mild severity of the Coronavirus in the hesitant group. In contrast, about 61.65% of people in the accepting group thought of it as more than a mild disease. About three-quarters of people thought that the fuss being made about COVID-19 is adequate, and all of them were ready to receive the vaccine (78.62%). Most of the respondents believed that they all were responsible for reducing COVID-19 infection (90.67%, 87.92%). 61% in the hesitant group believed that they were immune to COVID-19, whereas, in the accepting group, 58.24% didn't. However, both groups believed that COVID-19 had a big impact on their life (67.26%, 60.52%). A large portion (79.85%) of the acceptance group believed that vaccination should be made mandatory for everyone. The respondents in the hesitant group were in the dilemma of believing (51.83:48.17). In the accepting group, almost two-thirds (68.63%) voted 'no' to believe that only people at serious risk should get the vaccination, where more than half of the participants from the hesitant group marked 'yes.' Almost three-quarters of the total study participants (76%) showed their belief in the Government. They were willing to take the vaccine if the Government recommended it. 77.60% of people in the hesitant group expressed worry regarding the adverse effects of immunizations. In the hesitant group, 75.23 % of people were not interested in receiving a vaccine when it was not provided free of value. However, more than half in the acceptance group (55.74%) were willing to get vaccinated, irrespective of the cost. The majority of the respondents believed that the vaccine would work against COVID-19 infection. (n = 4,954, 67%). Out of them, 3,745 were accepting, and 1,479 were hesitant.
Table 2.
(Chi-square table): Results of the logistic regression model showing associations of factors related to vaccination acceptance (n = 7357).
| Factors | Hesitant/resistant n (%) | Accepting n (%) | p-value |
|---|---|---|---|
|
Worry about COVID-19 infection | |||
| No | 1,695 (65.90) | 2,848 (59.52) | <0.001 |
| Yes |
877 (34.10) |
1,937 (40.48) |
|
|
Belief COVID-19 would cause mild illness | |||
| No | 1,275 (49.57) | 2,950 (61.65) | <0.001 |
| Yes |
1,297 (50.43) |
1,835 (38.35) |
|
|
Thinking too much fuss is made about COVID-19 | |||
| No | 1.791 (69.63) | 3,762 (78.62) | <0.001 |
| Yes |
781 (30.37) |
1,023 (21.38) |
|
|
Thinking we all are responsible for reducing COVID-19 | |||
| No | 240 (9.33) | 578 (12.08) | <0.001 |
| Yes |
2,332 (90.67) |
4,207 (87.92) |
|
|
The belief that one is immune to COVID-19 | |||
| No | 1,003 (39.00) | 2,787 (58.24) | <0.001 |
| Yes |
1,569 (61.00) |
1,998 (41.76) |
|
|
The belief that COVID-19 has a big compact on life | |||
| No | 842 (32.74) | 1,889 (39.48) | <0.001 |
| Yes |
1,730 (67.26) |
2,896 (60.52) |
|
|
The belief that vaccination should be made mandatory for everyone | |||
| No | 1,333 (51.83) | 964 (20.15) | <0.001 |
| Yes |
1,239 (48.17) |
3,821 (79.85) |
|
|
The belief that only people who are at serious risk from COVID-19 should receive the vaccine | |||
| No | 1,087 (42.26) | 3,284 (68.63) | |
| Yes |
1,485 (57.74) |
1,501 (31.37) |
|
|
Will take the vaccine if recommended by the Government | |||
| No | 1,153 (44.83) | 609 (12.73) | <0.001 |
| Yes |
1,419 (55.17) |
4,176 (87.27) |
|
|
Worried about side- effects of COVID-19 | |||
| No | 576 (22.40) | 2,305 (48.17) | <0.001 |
| Yes |
1,996 (77.60) |
2,480 (51.83) |
|
|
Will take COVID- 19 vaccine even if it is not free | |||
| No | 1,935 (75.23) | 2,118 (44.26) | <0.001 |
| Yes |
637 (24.77) |
2,667 (55.74) |
|
|
The belief that vaccines will work against COVID-19 | |||
| No | 1,093 (42.50) | 1,040 (21.73) | <0.001 |
| Yes | 1,479 (57.50) | 3,745 (78.27) | |
The logistic regression table (Table 3) shows the binary logistic regression analysis results determining associations between demographic and health indicators and acceptability of the COVID-19 vaccine in Bangladesh. Participants with graduate or above education levels (≥18 years of schooling) were 1.80 times more likely to get vaccinated against COVID-19 than people with up to higher secondary level education (≤12 years of schooling). Intent to get vaccinated was higher among those ages 31 and older than among comparatively younger adults (ages 30 and below). Moreover, being residents of the countryside (AOR = 2.24) and higher-income groups were associated with an increased odds of taking the vaccine. The likelihood of accepting vaccines was significantly higher among service holders (30%), students (198%), and other professionals (55%) compared to businesspersons. Participants from other divisions showed comparatively higher intention to take the vaccine than Barisal, especially Khulna (AOR = 6.43). The presence of chronic diseases (AOR = 0.72) was associated with a decreased trend of getting vaccinated. On the other hand, participants with family members previously diagnosed COVID-19 and a history of getting vaccinated in the last few years showed a greater likelihood to accept vaccines (1.24 and 1.32 times, respectively) compared to their counterparts.
Table 3.
(Logistic regression table): The association between beliefs and attitude towards COVID-19 and COVID-19 vaccine, and vaccine acceptance intention.
| Variable | Crude ORa | 95% CI | Adjusted ORb | 95% CI |
|---|---|---|---|---|
|
Education | ||||
| <Graduate | 1 | 1 | 1 | 1 |
| ≥Graduate |
1.85 |
1.67–2.05 |
1.80∗ |
1.58–2.06 |
|
Age (years old) | ||||
| ≤30 | 1 | 1 | 1 | 1 |
| 31 to 50 | 1.07 | 0.96–1.18 | 1.45∗ | 1.29–1.65 |
| ≥50 |
1.41 |
1.20–1.66 |
1.97∗ |
1.63–2.38 |
|
Gender | ||||
| Male | 1 | 1 | 1 | 1 |
| Female |
1.10 |
0.99–1.22 |
1.05 |
0.93–1.19 |
|
Occupation | ||||
| Businessperson | 1 | 1 | 1 | 1 |
| Service holder | 1.39 | 1.22–1.59 | 1.30∗ | 1.11–1.52 |
| Student | 2.29 | 1.93–2.70 | 2.98∗ | 2.44–3.64 |
| Others |
1.39 |
1.20–1.61 |
1.55∗ |
1.30–1.85 |
|
Health Care Worker | ||||
| Yes | 1 | 1 | 1 | 1 |
| No |
1.15 |
1.00–1.32 |
1.04 |
0.88–1.25 |
|
Income | ||||
| ≤20000 BDT | 1 | 1 | 1 | 1 |
| 21000 to 40000 | 1.21 | 1.08–1.35 | 1.35∗ | 1.18–1.54 |
| ≥41000 |
2.46 |
2.10–2.89 |
2.22∗ |
1.83–2.68 |
|
Residence | ||||
| Urban | 1 | 1 | 1 | 1 |
| Rural |
1.77 |
1.58–1.98 |
2.24∗ |
1.95–2.57 |
|
Family size | ||||
| Large | 1 | 1 | 1 | 1 |
| Small |
1.08 |
0.98–1.19 |
0.99 |
0.89–1.10 |
|
Division | ||||
| Barishal | 1 | 1 | 1 | 1 |
| Chattogram | 3.11 | 2.54–3.81 | 2.76∗ | 2.21–3.45 |
| Dhaka | 2.25 | 1.89–2.67 | 2.20∗ | 1.81–2.69 |
| Khulna | 6.92 | 5.39–8.89 | 6.43∗ | 4.92–8.41 |
| Mymensingh | 2.96 | 2.38–3.69 | 3.17∗ | 2.50–4.02 |
| Rajshahi | 3.21 | 2.54–4.06 | 3.20∗ | 2.48–4.13 |
| Rangpur | 1.89 | 1.50–2.38 | 2.00∗ | 1.55–2.58 |
| Sylhet |
1.86 |
1.49–2.31 |
1.96∗ |
1.54–2.49 |
|
Diagnosed with COVID-19 | ||||
| No | 1 | 1 | 1 | 1 |
| Yes |
1.07 |
0.89–1.28 |
1.12 |
0.90–1.40 |
|
Family members Diagnosed with COVID-19 | ||||
| No | 1 | 1 | 1 | 1 |
| Yes |
1.21 |
1.02–1.45 |
1.24∗ |
1.01–1.52 |
|
Chronic Disease | ||||
| No | 1 | 1 | 1 | 1 |
| Yes |
0.72 |
0.64–0.81 |
0.72∗ |
0.63–0.82 |
|
Family members aged above 60 years old | ||||
| No | 1 | 1 | 1 | 1 |
| Yes |
0.96 |
0.87–1.05 |
1.02 |
0.91–1.13 |
|
History of taking vaccine in the last few years | ||||
| No | 1 | 1 | 1 | 1 |
| Yes | 1.44 | 1.28–1.63 | 1.32∗ | 1.16–1.50 |
Notes: Variables with significant OR at p < 0.05 level were indicated using asterisk sign (∗).
Multivariate logistic regression analysis was done using the enter method.
Adjusted for age, gender, education, occupation, health care worker, income, residence, family size, division, health indicators (previously diagnosed with COVID-19, chronic diseases, having 60 + ages family members, previous vaccination history).
4. Discussion
It took time for the COVID-19 vaccine to arrive in Bangladesh compared to the rest of the world. Incidents regarding vaccination worldwide affected decision-making regarding accepting a vaccine when available on some level in this region. The most critical barriers in vaccine acceptance worldwide seem to be the vaccine's efficacy and worry related to the vaccine's side effects [17, 18, 19]. However, several other location-specific factors to vaccine hesitancy came up in countries like Italy, where trust issues with authority and belief about the virus's origin were the most significant determinants for receiving a COVID-19 vaccine [20]. Given the different findings in contemporary studies, it is necessary to evaluate the attitude and belief towards the COVID-19 vaccine among Bangladesh's general population. We conducted nationwide research collecting samples from every administrative division to have a general understanding of this.
Vaccine hesitancy or resistance was higher in people who believed people at serious risk from COVID-19 should receive the vaccine. We also found that most of our study populations were not worried about COVID-19 infection. People thinking too much fuss about the disease being made were significantly less likely to receive a vaccine. The notion that much confusion was being created surrounding the disease's severity is disbelieving the seriousness & sensibility of the pandemic [21]. Though this population is comparatively small, specific research is needed to determine what factors might behind this belief. Public health workers worldwide should concentrate on enlightening and building faith among the unsure and reluctant population regarding security, effectiveness, and adverse effects of the COVID-19 vaccine [16, 22, 23]. Our study also found that people with chronic disease in Bangladesh have shown less interest in vaccination, which is again most likely because of their concern of probable side effects, which are still under investigation. However, studies conducted in Ireland [24] and the UK [24, 25] showed similar results, and similar reasons were proposed.
Vaccines recommended by the Government create a much less reluctance to take the vaccine. Likely so, an incredibly motivated authority is a robust measure to expand immunization handling [26]. It is expected that for this reason, in this study, the highest percentage of respondents (76.05%) showed a willingness to receive the COVID-19 vaccine when the Government recommends it. A noteworthy finding in our research is that people are more interested in receiving the vaccine if they freely receive it [18]. When the vaccine is not accessible free of cost, around two-thirds of our study participants hesitated to receive the vaccine. Chen et al. has found similar results and assessed that a trustworthy government is a solid factor to upscale vaccine acceptance [26].
We performed binary logistic regression analysis to determine the association of several factors related to socio-demography and health with vaccine acceptance among the Bangladeshi people. Higher education was associated with higher vaccine acceptance in our study. Specifically, graduates (≥18 years of schooling) were 80% more likely to receive a vaccine when it is available compared to less educated people. Guidry et al. have argued that this finding supports the Health Belief Model and the Theory of Planned Behavior. They predict people with a positive attitude and solid subjective norms and people who believe they are more vulnerable to be ill should be more willing to accept a vaccine [28].
We found the vaccine acceptance rate significantly higher among adults (age 30 and above) and older groups (53.83%) than the younger population (Table 2). The reason for comparatively more vaccine acceptance among the more aging population is most likely because COVID-19 affected the adult and more senior people. This group faced the highest death toll [5]. A similar result was found in a study conducted in the United States [12]. Moreover, people from higher income groups have shown more vaccine acceptance rate than lower-income groups in Bangladesh. As most of the Bangladeshi participants were experiencing a financial crisis and lost their jobs during COVID-19, people in the low-income range may lack interest in the COVID-19 vaccine. It was also found as a common finding across many countries of the world [26–28]. This is particularly problematic, as this result indicates that the people with lower income are most likely out of proportion for COVID-19 infection and, therefore, more vulnerable to ongoing outbreaks even when a vaccine is available [12].
Additionally, in Bangladesh, students and Government and non-government employees were more likely to receive vaccines than the business populace. People working or studying in enclosed areas might be concerned about their peers' safety [19]. Additionally, businesspersons are lower educated in most cases, whereas service holders are more educated, careful, and conscious. Though it has not been visualized, we observed a low education level among businesspersons during our study. So most probably, education might have an impact on this result. Similar findings were also found in Western Uganda [29].
Furthermore, participants with previously COVID-19 affected family members and a history of being vaccinated within the last few years were associated with an increasing vaccination trend. Social responsibility and positive experience with vaccination and vaccination services might have worked as an influencer here [30].
Our study's strength is that it has been exercised on a large sample, a better representation of participants from eight divisions of Bangladesh. Another strong point is that we have included almost all variables related to vaccine intentions in our questionnaire after an extensive literature review. It makes us ahead of others. However, as we collected data through convenience sampling, it is impossible to guarantee that our findings represent the whole population. There is no way to deny social media's influence on vaccine intake decisions, especially during the pandemic. But, we didn't collect data on social media's role in the participants' decision to take/not to take the vaccine. However, having based on a large sample, we believe that a population-based study might show similar patterns in the findings as we found in the current study. The logistic regression results present noteworthy discussion points on vaccine intention's socio-demographic characteristics but cannot display relationships and should be interpreted with caution. As we have a large sample, the causality of few determinants is most probably small and likely not to be clinically meaningful.
5. Conclusion
To achieve the COVID-19 tackling plan, increased vaccination would be paramount for Bangladesh Government. Given that almost 65 percent of our respondents were likely to be vaccinated against COVID-19, we are still way behind the standard minimum coverage (75 percent) to fight back with the virus [31]. Although it is an original systematically meticulous study observing the belief, attitude, and intention towards a COVID-19 vaccine in an enormous sample of Bangladeshi people, fast-spreading rumors regarding the vaccine may affect the vaccine intake decision. That's why a proactive strategy emphasizing the usefulness of herd immunity should be taken from the policy level. Besides, our suggestion is to use the mass media to minimize the hesitancy by addressing the vaccine's effectiveness and rightful public health information.
Declarations
Author contribution statement
Miah Md. Akiful Haque: Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
Mohammad Lutfor Rahman: Conceived and designed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools, or data; Wrote the paper.
Mosharop Hossian, Shuvajit Saha: Analyzed and interpreted the data; Contributed reagents, materials, analysis tools, or data; Wrote the paper.
Mohammad Hayatun Nabi: Conceived and designed the experiments; Contributed reagents, materials, analysis tools, or data; Wrote the paper.
Mehedi Hasan, Ridwana Maher Manna, S. M. Rezwanul Hasan, Saleka Raihana Siddiquea, Mahfil Ara Rahman, Kazi Farhana Matin: Contributed reagents, materials, analysis tools, or data; Wrote the paper.
Sabrina Yesmin Barsha: Performed the experiments; Contributed reagents, materials, analysis tools, or data; Wrote the paper.
Md Abdullah Saeed Khan, Md Utba Rashid, Mohammad Ali Hossain: Performed the experiments; Contributed reagents, materials, analysis tools, or data.
Mohammad Delwer Hossain Hawlader: Conceived and designed the experiments; Performed the experiments; Contributed reagents, materials, analysis tools, or data.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
Data will be made available on request.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
We would like to convey our heartfelt appreciation for the participants' assistance.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.UNDP Coronavirus Disease COVID-19 Pandemic | UNDP, UNDP. https://www.undp.org/content/undp/en/home/coronavirus.html (n.d.)
- 2.WHO Coronavirus disease (COVID-19) https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (n.d.)
- 3.ILO, FAO, IFAD, WHO . WHO; 2020. Impact of COVID-19 on People’s Livelihoods, Their Health and Our Food Systems.https://www.who.int/news/item/13-10-2020-impact-of-covid-19-on-people%27s-livelihoods-their-health-and-our-food-systems [Google Scholar]
- 4.Kamruzzaman M., Sakib S.N. AA; 2020. Bangladesh Imposes Total Lockdown over COVID-19.https://www.aa.com.tr/en/asia-pacific/bangladesh-imposes-total-lockdown-over-covid-19/1778272 [Google Scholar]
- 5.WHO . WHO; 2021. WHO Bangladesh COVID-19 Morbidity and Mortality Weekly Update.https://cdn.who.int/media/docs/default-source/searo/bangladesh/covid-19-who-bangladesh-situation-reports/who_covid-19-update_49_20210201.pdf?sfvrsn=a365c489_9 [Google Scholar]
- 6.Islam M.T., Talukder A.K., Siddiqui M.N., Islam T. Tackling the COVID-19 pandemic: the Bangladesh perspective. J. Public Health Res. 2020;9:389–397. doi: 10.4081/jphr.2020.1794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bangladesh Governement . 2020. National Preparedness and Response Plan for COVID-19, Bangladesh - Bangladesh | ReliefWeb, Reliefweb.https://reliefweb.int/report/bangladesh/national-preparedness-and-response-plan-covid-19-bangladesh [Google Scholar]
- 8.Biswas R.K., Huq S., Afiaz A. Relaxed lockdown in Bangladesh during COVID-19: should economy outweigh health? Kerman Univ. Med. Sci. 2020;9:488–490. doi: 10.34172/ijhpm.2020.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eskola J., Liang X. WHO | SAGE working group dealing with vaccine hesitancy (March 2012 to November 2014) https://www.who.int/immunization/sage/sage_wg_vaccine_hesitancy_apr12/en/ (n.d.)
- 10.Butler R. Vaccine Hesitancy: what it means and what we need to know in order to tackle it. J. Vaccine. 2016;34:1643–1649. https://www.who.int/immunization/research/forums_and_initiatives/1_RButler_VH_Threat_Child_Health_gvirf16.pdf?ua=1 [Google Scholar]
- 11.Karafillakis E., Larson H.J. The benefit of the doubt or doubts over benefits? A systematic literature review of perceived risks of vaccines in European populations. Vaccine. 2017;35:4840–4850. doi: 10.1016/j.vaccine.2017.07.061. [DOI] [PubMed] [Google Scholar]
- 12.Malik A.A., McFadden S.A.M., Elharake J., Omer S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMed. 2020;26:100495. doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gurnani V., Haldar P., Aggarwal M.K., Das M.K., Chauhan A., Murray J., Arora N.K., Jhalani M., Sudan P. Improving vaccination coverage in India: lessons from Intensified Mission Indradhanush, a cross-sectoral systems strengthening strategy. BMJ. 2018;363:1–7. doi: 10.1136/bmj.k4782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ali M., Hossain A. Medrxiv.Org.; 2021. What Is the Extent of COVID-19 Vaccine Hesitancy in Bangladesh? : A Cross-Sectional Rapid National Survey. (n.d.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Islam S., Siddique A.B., Akter R., Tasnim R., Sujan M.S.H., Ward P.R., Sikder M.T. 2021. Knowledge, Attitudes and Perceptions towards COVID-19 Vaccinations: a Cross-Sectional Community Survey in Bangladesh. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sherman S.M., Smith L.E., Sim J., Amlôt R., Cutts M., Dasch H., Rubin G.J., Sevdalis N. COVID-19 vaccination intention in the UK: results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. Hum. Vaccines Immunother. 2020:1–10. doi: 10.1080/21645515.2020.1846397. 00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bhartiya S., Kumar N., Singh T., Murugan S., Rajavel S., Wadhwani M. Knowledge, attitude and practice towards COVID-19 vaccination acceptance in West India. Int. J. Commun. Med. Public Heal. 2021;8:1–7. [Google Scholar]
- 18.Harapan H., Wagner A.L., Yufika A., Winardi W., Anwar S., Gan A.K., Setiawan A.M., Rajamoorthy Y., Sofyan H., Mudatsir M. Acceptance of a COVID-19 vaccine in southeast Asia: a cross-sectional study in Indonesia. Front. Public Heal. 2020;8:1–8. doi: 10.3389/fpubh.2020.00381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lin Y., Hu Z., Zhao Q., Alias H., Danaee M., Wong L.P. Understanding COVID-19 vaccine demand and hesitancy: a nationwide online survey in China. PLoS Neglected Trop. Dis. 2020;14 doi: 10.1371/journal.pntd.0008961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Prati G. Intention to receive a vaccine against SARS-CoV-2 in Italy and its association with trust, worry and beliefs about the origin of the virus. Health Educ. Res. 2020;35:505–511. doi: 10.1093/her/cyaa043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rubin G.J., Finn Y., Potts H.W.W., Michie S. Who is sceptical about emerging public health threats? Results from 39 national surveys in the United Kingdom. Publ. Health. 2015;129:1553–1562. doi: 10.1016/j.puhe.2015.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thunstrom L., Ashworth M., Finnoff D., Newbold S. Hesitancy towards a COVID-19 vaccine and prospects for herd immunity. SSRN Electron. J. 2020 doi: 10.1007/s10393-021-01524-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Butter S., McGlinchey E., Berry E., Armour C. Vol. 4520. 2020. Psychological, social, and situational factors associated with COVID-19 vaccination intentions: a study of UK key workers and non-key workers; pp. 1–26. (n.d.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Murphy J., Vallières F., Bentall R., Shevlin M., McBride O., Hartman T., McKay R., bennett kate, Mason L., Gibson Miller J., Levita L., Martinez A., Stocks T.V.A., Karatzias T., Hyland P. 2020. Preparing for a COVID-19 Vaccine: Identifying and Psychologically Profiling Those Who Are Vaccine Hesitant or Resistant in Two General Population Samples. [Google Scholar]
- 25.Paul E., Steptoe A., Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID-19: implications for public health communications. Lancet Reg. Heal. - Eur. 2021;1:100012. doi: 10.1016/j.lanepe.2020.100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen M., Li Y., Chen J., Wen Z., Feng F., Zou H., Fu C., Chen L., Shu Y., Sun C. An online survey of the attitude and willingness of Chinese adults to receive COVID-19 vaccination. Hum. Vaccines Immunother. 2021:1–10. doi: 10.1080/21645515.2020.1853449. 00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bartsch S.M., O'Shea K.J., Ferguson M.C., Bottazzi M.E., Wedlock P.T., Strych U. Vaccine efficacy needed for a COVID-19 coronavirus vaccine to prevent or stop an epidemic as the sole intervention. Am. J. Prev. Med. 2020;59:493–503. doi: 10.1016/j.amepre.2020.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.