Dear Editor,
As the Coronavirus Disease 2019 (COVID-19) pandemic spreads, there is a concern regarding its clinical and epidemiological implications of bacterial, fungal and viral coinfections in patients with COVID-19 [1]. Particularly, the coinfection of the Severe Acute Respiratory Syndrome coronavirus 2 (SARS-CoV-2) and Mycobacterium tuberculosis (MTB) in patients with the Human Immunodeficiency Virus (HIV) infection remains a matter of concern, and the results and clinical course have not been thoroughly studied. Here, we present one case of triple coinfection (HIV/MTB/SARS-CoV-2) in a patient from Northeastern Colombia.
A 34-year-old woman from Bucaramanga, Colombia, arrived at the emergency department in January 2021 with a known diagnosis of HIV/AIDS for six years in irregular treatment with zidovudine/lamivudine plus lopinavir/ritonavir and a 7-day history of unquantified fever, dyspnea and headache. In addition, she had poor adherence to antiretroviral therapy and a history of illicit drug abuse (marijuana and cocaine) and generalized anxiety disorder. Furthermore, the patient had lost clinical and laboratory follow-up in the last two years. In 2019, the HIV viral load was 317 copies/mm3, and the T-CD4 cell count was 105/mm3.
On physical examination, she was cachectic (weight 42 kg) with signs of moderate/severe dehydration and mild respiratory distress, with respiratory rates ranging from 28 to 30 breaths/minute, oxygen saturation ranging from 85 to 90% on ambient air, and a heart rate of 108 bpm. A chest examination revealed bilateral crepitations of apical predominance and wheezes. These findings supported hospital admission as a suspected COVID-19 case. A nasopharyngeal swab test (rRT-PCR) confirmed the presence of SARS‐CoV‐2. The patient was transferred to a respiratory isolation room with oxygen at 4 L/min via nasal cannula.
Baseline blood test analysis revealed severe anemia (hemoglobin 6.8 g/dL), leukocytosis (WBC 13.8 × 103/μL), neutrophilia (13.0 × 103/μL), lymphopenia (0.2 × 103/μL), normal platelet count, elevated inflammation-related biomarkers (LDH 467 U/L, Ferritin 2778 ng/ml, CRP 121 mg/dL), severe elevation in D-dimer (4430 mg/dL) and severe hypoalbuminemia (1.95 g/dL) among relevant serum findings. There were no alterations in the patient's kidney function or liver function tests.
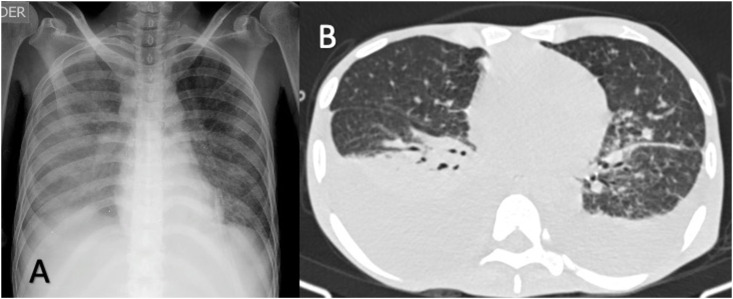
A chest radiograph showed bilateral diffuse micronodular and reticular interstitial opacities (Fig. 1 ). Chest computed tomography revealed bilateral pleural effusion, diffuse miliary opacities associated with glass-ground opacities (Fig. 1). Acid-fast bacilli smears were positive, and GeneXpert MTB/RIF assay resulted positive for infection with Mycobacterium tuberculosis without resistance to rifampicin. Additionally, we confirmed coinfection with HIV with a T-CD4 cell count of 25/mm3 and a viral load of 911,241 copies/mL.
Fig. 1.
Thorax radiography (A) demonstrates bilateral diffuse micronodular and reticular interstitial opacities. Chest computed tomography (B) axial thin-section unenhanced CT image showing randomly distributed (miliary) nodules in both lungs associated with glass-ground opacities in the left lower lobe and bilateral pleural effusion.
She was initially managed with ampicillin/sulbactam, doxycycline, dexamethasone and oxygen supplementation. During hospitalization, the patient deteriorated clinically with increasing dyspnea and worsening of respiratory parameters, requiring mechanical ventilation. Despite all measures, the patient rapidly deteriorated and succumbed to the illness on the second day of hospital management.
This is the first fatal, reported case of triple coinfection (HIV/MTB/SARS-CoV-2) worldwide to the best of our knowledge. Two cases of COVID-19 in patients with HIV/MTB coinfection were reported from Panama in August 2020; both patients showed clinical progress and recovery from COVID-19 within two weeks [2]; and two more cases of COVID-19 in patients with a known diagnosis of pulmonary tuberculosis and HIV were reported from Brazil in August 2020, with complete recovery and discharge to home with outpatient follow-up [3].
HIV/SARS-COV-2 and MTB/SARS-COV-2 coinfections are poorly known. On one side, patients co-infected with HIV and COVID-19 share many of the same disease risk and progression characteristics as HIV-uninfected patients [4]. However, a recent report found poorer COVID-related outcomes (higher rates of severe disease requiring hospitalization) in HIV patients than those without an HIV diagnosis, especially in those with multimorbidity and older age [5]. On the other hand, a systematic review reported a higher risk of mortality in MTB/SARS-CoV-2 patients [6]. Nevertheless, a previous meta-analysis found that tuberculosis was not associated with the increased risk of mortality in patients with COVID‐19, which was also found in a systematic study of cases of SARS-CoV-2 coinfection with drug-resistant TB. In both cases, the evidence is currently inconsistent, and more high-quality studies are required to understand better the association between HIV, tuberculosis and COVID‐19 prognosis.
Multiple factors could contribute to the death of our patient, including non-adherence to antiretroviral treatment, low CD4 count, high viral load, hypoalbuminemia, lymphopenia, increased acute phase reactants and a late diagnosis of tuberculosis, and these could be factors associated with the worsening of HIV/MTB/SARS-CoV-2 coinfection. According to our findings, triple infection can occur, even though it is uncommon. As a result, the existence of other infectious diseases should be carefully evaluated and ruled out in patients with COVID-19, especially in HIV and immunocompromised patients. More extensive studies are needed to fully comprehend the physiopathology of M. tuberculosis, HIV, and SARS-CoV-2 coinfection.
Ethical statement
Written consent of the relatives of the patient was obtained.
Author contribution
YOM conceived the idea of the letter and drafted the first version. The rest of the authors contributed to subsequent versions. Finally, all authors read and approved the final submitted version.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
Declaration of competing interest
None.
Acknowledgements
None.
References
- 1.Lansbury L., Lim B., Baskaran V., Lim W.S. Coinfections in people with COVID-19: a systematic review and meta-analysis. J Infect. 2020;81(2):266–275. doi: 10.1016/j.jinf.2020.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rivas N., Espinoza M., Loban A., Luque O., Jurado J., Henry-Hurtado N., Goodridge A. Case report: COVID-19 recovery from triple infection with Mycobacterium tuberculosis, HIV, and SARS-CoV-2. Am J Trop Med Hyg. 2020;103(4):1597–1599. doi: 10.4269/ajtmh.20-0756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gadelha Farias L.A.B., Gomes Moreira A.L., Austregésilo Corrêa E., Landim de Oliveira Lima C.A., Lopes I.M.P., de Holanda P.E.L., et al. Case report: coronavirus disease and pulmonary tuberculosis in patients with human immunodeficiency virus: report of two cases. Am J Trop Med Hyg. 2020;103(4):1593–1596. doi: 10.4269/ajtmh.20-0737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mirzaei H., McFarland W., Karamouzian M., Sharifi H. COVID-19 among people living with HIV: a systematic review. AIDS Behav. 2021;25(1):85–92. doi: 10.1007/s10461-020-02983-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tesoriero J.M., Swain C.E., Pierce J.L., Zamboni L., Wu M., Holtgrave D.R., Gonzalez C.J., et al. COVID-19 outcomes among persons living with or without diagnosed HIV infection in New York state. JAMA Netw Open. 2021;4(2) doi: 10.1001/jamanetworkopen.2020.37069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sarkar S., Khanna P., Singh A.K. Impact of COVID-19 in patients with concurrent coinfections: a systematic review and meta-analyses. J Med Virol. 2021;93(4):2385–2395. doi: 10.1002/jmv.26740. [DOI] [PubMed] [Google Scholar]