Abstract
Purpose
The aim of this paper is to describe our experience with a virtual fracture management pathway in the setting of a paediatric trauma service.
Methods
All patients referred to the virtual fracture clinic service from the Paediatric Emergency Department (PED) were prospectively collected. Outcome data of interest (patients discharged, referred for urgent operative treatment, referred back to emergency department for further evaluation, referred for face-to-face clinical assessment and all patients who re-presented on an unplanned basis for further management of the index injury) were compiled and collated. Cost analysis was performed using established costing for a virtual fracture clinic within the Irish Healthcare System.
Results
There were a total of 3961 patients referred to the virtual fracture clinic from the PED. Of these, 70% (n = 2776) were discharged. In all, 26% (n = 1033) were referred to a face-to-face appointment. Of discharged patients, 7.5% (n = 207) required an unplanned face-to-face evaluation. A total of 0.1% (n = 3) subsequently required operative treatment relating to their index injury. Implementation of the virtual fracture clinic model generated calculated savings of €254 120.
Conclusion
This prospective evaluation has demonstrated that a virtual fracture clinic pathway for minor paediatric trauma is safe, effective and brings significant cost savings.
Level of Evidence
II
Keywords: Virtual, fracture, pathway
Introduction
Clinical pathways and healthcare funding have largely been utilized to support and reinforce the face-to-face model of care.1 Providing a specialist orthopaedic trauma service to children with minor trauma in a timely manner can be challenging.2 Failing to meet the patient need can lead to adverse clinical outcomes with numerous negative consequences for the patient, doctor and health service. More recently the impact of the novel coronavirus (COVID-19) has pushed telehealth to deliver timely home-based care where the opportunity arises.3
International evidence has revealed that a virtual fracture clinic pathway offers safe, timely, effective care that delivers both resource and cost-efficient care to patients with minor paediatric trauma.2,4-8 Multiple reports have demonstrated that many simple paediatric injuries require minimal intervention,9-16 however, there is a paucity of evidence of the effectiveness of virtual fracture clinics in the setting of children’s trauma.
The authors hypothesized that most paediatric minor trauma care could be managed definitively on initial contact within the Paediatric Emergency Department (PED) with subsequent confirmation of treatment and re-triage at an orthopaedic specialist delivered virtual fracture clinic. The aim of this paper is to describe the experience of a virtual fracture management pathway in the setting of a dedicated paediatric trauma service.
Materials and methods
We performed a prospective observational study of paediatric virtual fracture clinic attendances from the 01 August 2017 to 01 March 2020. Ethical approval for prospective evaluation of this process was granted by the local research and ethics committee.
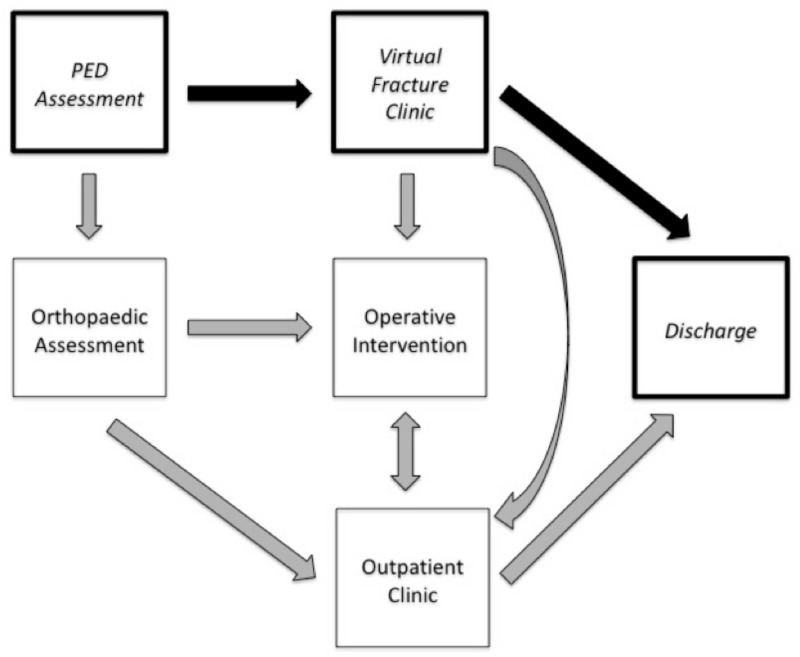
This study was conducted by the Departments of Orthopaedic Surgery and Emergency Medicine at the tertiary university affiliated paediatric hospital, Children’s Health Ireland, Crumlin, Dublin. Suitable children with fractures as determined by PED staff were referred to this pathway which was created through a collaboration of fellowship-trained paediatric emergency medicine (PEM) and orthopaedic specialists (Fig. 1). A weekly multidisciplinary quality improvement process was instigated to discuss all patients who were not discharged directly from the virtual fracture clinic so as to patient safety and refine pathway efficiency.
Fig 1.
Trauma management pathway incorporating virtual fracture clinic (PED, Paediatric Emergency Department).
All children with appropriate fractures who were not referred to the on-call orthopaedic team were referred to the next day virtual fracture clinic. Standardized referral guidance, radiographs, a detailed pro-forma clinical assessment (see supplementary material) and immobilization protocols were completed by the emergency department staff for every case referred. Patients were managed with removable immobilization and were provided with an injury specific information sheet detailing expected recovery course and precautions (see supplementary material).
As expected, the routine assessment of injury in the PED included consideration of the possibility of non-accidental injury under the supervision of the PEM specialist and no suspected cases of non-accidental injury were referred to this pathway. National and institutional child protection guidelines were adhered to. All radiological investigations were reported by specialist paediatric radiologists, and PEM staff were formally advised if their diagnosis was at variance with the radiology opinion. On the following working day, radiographs and pro-forma clinical assessments were evaluated by a fellowship trained paediatric orthopaedic surgeon who was responsible for the final deposition of all referred patients. The patient management plan was validated. At this point patients were discharged via a phone call with confirmation of the appropriate protocol, returned to the PED for further evaluation, or diverted to further surgical/non-surgical management. All discharged patients were given a contact number to re-engage with the fracture service if they were not entirely satisfied with the outcome after the duration described in the treatment protocol.
The patient’s virtual clinical disposition was prospectively captured as one of the following: discharged, referred for urgent operative treatment, referred back to PED for further evaluation, referred for face-to-face fracture clinic assessment. All unscheduled patient attendances relating to the index injury were prospectively identified. Patients who represented with an identical fracture to their index injury within three months were considered to have sustained a refracture. Emergency department, radiology and theatre information systems were cross referenced.
Cost analysis of the implementation of a virtual fracture clinic model for children’s injuries within the Irish healthcare setting was performed using the methodology described by Reilly.17
All data were analyzed using Excel (Microsoft, Redmond, Washington) Descriptive statistics were calculated using proportions, means or medians and ranges as appropriate. Simple linear regression analysis was used to describe relationships between continuous variables.
Results
A total of 3961 consecutive patients were prospectively identified who were referred to the virtual fracture clinic service from the PED. The mean age of patients referred was 8.9 years (0.5 to 17). There were 1693 (43%) girls and 2268 (57%) boys. The mean follow-up was 20.9 months (5 to 36). Patient demographics are displayed in Table 1.
Table 1.
Patient number, characteristics and virtual clinic disposition (n = 3961)
| Patient characteristics | n (%) |
|---|---|
| Mean age, yrs (range) | 8.9 (0.5 to 17) |
| Sex | |
| Female | 1693 (43) |
| Male | 2268 (57) |
| Area injured | |
| Hand | 1056 (23) |
| Upper extremity (excluding hand) | 1822 (46) |
| Lower extremity | 832 (21) |
| Virtual clinic disposition | |
| Discharged | 2776 (70) |
| Face-to-face clinic | 1033 (26) |
| Emergency department | 125 (3) |
| Direct operative care | 27 (1) |
Definitive management at the first interaction was delivered for 70% of patients (n = 2776), this group was discharged from the virtual clinic pathway. Of these patients 23% (n = 1056) had hand injuries, 46% (n = 1822) had other upper extremity injuries and 21% (n = 832) had lower extremity injuries (Table 1). Breakdown of the injuries treated definitively via the virtual fracture clinic protocol is given in Table 2.
Table 2.
Diagnosis and virtual clinic disposition
| Diagnosis as referred by PED | Total number of patients (n = 3961) | Percentage of total (n = 3961) | Number discharged (n = 2767) | Percentage of each injury discharged (n = 2767) |
|---|---|---|---|---|
| Buckle fracture distal radius | 1019 | 22 | 812 | 80 |
| Stable hand fracture (with no rotation)* | 858 | 22 | 615 | 72 |
| Stable foot fracture (with no rotation)* | 544 | 14 | 399 | 73 |
| Gartland 1 supracondylar fracture | 530 | 13 | 295 | 56 |
| Stable fracture of the lateral malleolus* | 407 | 10 | 248 | 61 |
| Clavicle fracture | 261 | 7 | 214 | 82 |
| Proximal humerus fracture* | 148 | 4 | 115 | 78 |
| Toddlers fracture (tibia) | 123 | 3 | 49 | 40 |
| Volar plate injury of the finger | 37 | 1 | 14 | 38 |
| Miscellaneous | 35 | 1 | 6 | 0.2 |
stable fractures as confirmed by treating paediatric orthopaedic specialist
Of those referred to the virtual fracture clinic, 26% (n = 1033) required a subsequent face-to-face appointment at orthopaedic facture clinic. Only 1% of the patients (n = 27) assessed at the virtual fracture clinic were admitted directly to the day surgical unit for operative care. The decision for surgical treatment in these cases was made within 24 hours and treatment was provided within a clinically appropriate timeframe. A further seven patients were assessed acutely in the day surgical unit and were subsequently followed up in orthopaedic outpatients without surgical intervention. A small number, 3% (n = 125) were referred back to the PED on the day of the virtual fracture clinic for immediate assessment. Reasons for re-attendance are given in Table 3.
Table 3.
Post-virtual fracture clinic booked emergency department attendances
| Reason | Number of re-attendances | Percentage |
|---|---|---|
| PED scheduled returns | ||
| Incomplete documentation | 54 | 43 |
| Inadequate radiological assessment | 31 | 25 |
| Non-trauma referral | 21 | 17 |
| Required further examination | 5 | 4 |
| Miscellaneous | 14 | 11 |
| Total referrals to PED | 125 | 100 |
PED, Paediatric Emergency Department
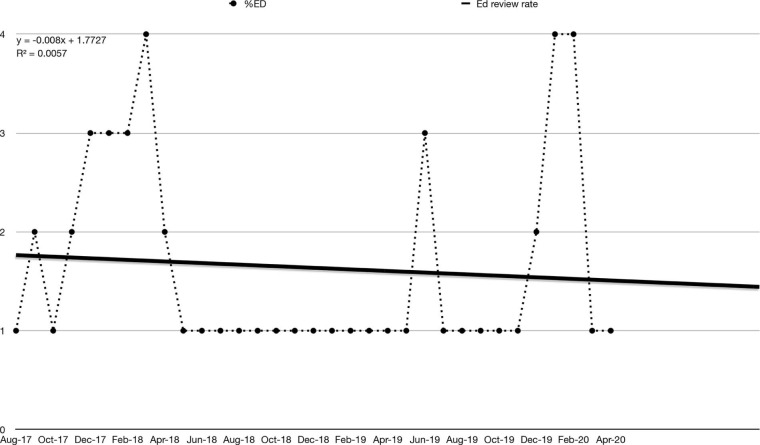
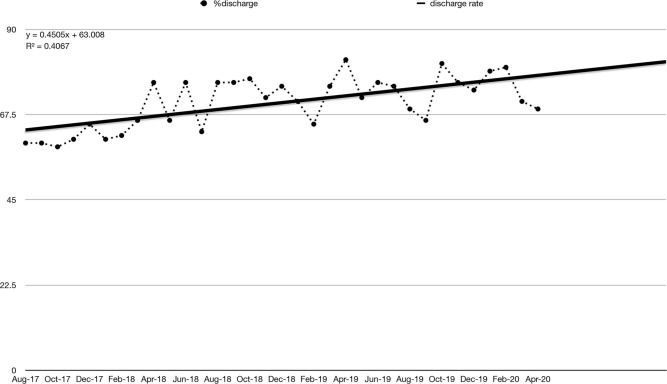
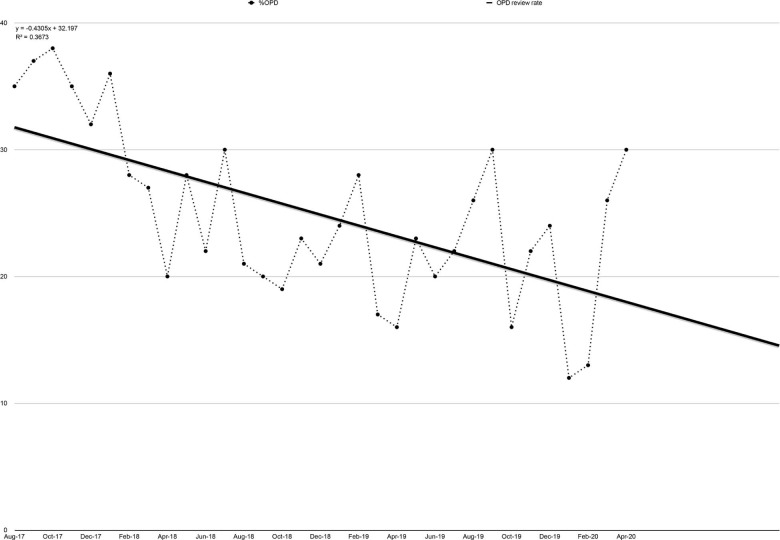
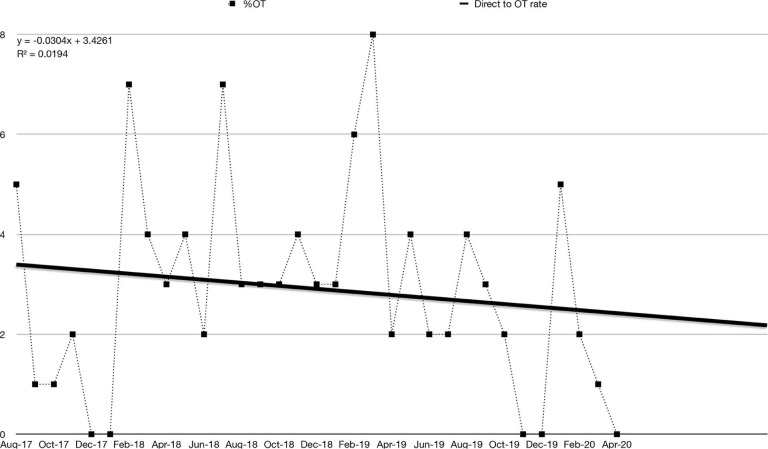
Variation in disposition over time is shown in Figures 1 to 4. Linear regression analysis highlights a trend towards increasing discharge rates (R2 = 0.41) (Fig. 2) and reducing orthopaedic fracture clinic referral rates (R2 = 0.37) (Fig. 3) over time. No strong correlation with time was appreciated for rate of re-referral to PED (R2 = 0.006) (Fig. 4) and direct operating theatre admission rates (R2 = 0.02) (Fig. 5).
Fig 4.
Variation in Paediatric Emergency Department reassessment rate (ED, Emergency Department).
Fig 2.
Variation in discharge rate.
Fig 3.
Variation in fracture clinic review rate.
Fig 5.
Variation in rate operative treatment after assessment at virtual fracture clinic (OT, operating theatre).
At a minimum three-month follow-up a total of 7.5% (n = 207 of 2776) who were discharged from the virtual fracture clinic re-attended the hospital. A description of all returns is given in Table 4.
Table 4.
Post-trauma assessment clinic unplanned emergency department and orthopaedic attendances
| Reason | Number of re-attendances | Percentage |
|---|---|---|
| PED unscheduled returns | ||
| Patient/carer immobilization issue or concern | 92 | 54 |
| Pain | 64 | 37 |
| Primary care referral | 4 | 2 |
| Unknown/other reasons | 4 | 2 |
| Other parental concern | 3 | 2 |
| Medical admission investigating limp | 2 | 1 |
| Paraesthesia | 1 | 0.5 |
| Wound issue | 1 | 0.5 |
| Subtotal of Emergency Department unscheduled returns | 171 | |
| Orthopaedic clinic returns | ||
| Scheduled return for previous injury | 20 | 55.5 |
| Scheduled return for subsequent injury | 4 | 11.1 |
| Unplanned return re-fracture index injury | 6 | 16.7 |
| Unplanned return index injury | 6 | 16.7 |
| Subtotal of orthopaedic clinic returns | 36 | |
| Surgery for subsequent injury | 5 | |
| Unanticipated surgery for index injury | 3 | |
| Subtotal orthopaedic surgery | 8 | |
Cross-referencing with the national radiology database (National Integrated Medical Imaging System (NIMIS)) and theatre logs demonstrated that eight patients (0.2%) who were discharged via the virtual fracture clinic pathway had orthopaedic operative treatment within the follow-up period. All eight of these patients were treated at our institution. Of the patients who underwent operative treatment for an orthopaedic injury post-discharge from the virtual fracture clinic pathway, five were treated for a second injury unrelated to their index presentation. In all, 0.1% (n = 3) of patients who were discharged from the virtual fracture clinic pathway subsequently underwent operative treatment directly relating to their index injury. The first, a 12-year-old female, underwent an ankle injection to relieve pain after persistent ankle inversion injuries, and she remains under the care of our institution. A second patient, an 11-year-old female underwent arthroscopic removal of a loose body from her elbow five months post-index injury. The extent of her injury was not appreciated on initial review of radiographs. She has gone on to make a complete recovery. A final patient, a 15-year-old male, unsatisfied with the appearance of his hand three weeks after non-operative management of a boxer’s fracture re-presented to the PED. An attempted manipulation under anaesthesia was performed and while no rotational misalignment was detected the flexion deformity could not be corrected. No further management is planned.
Economic analysis was performed based on the work of Reilly.17 Total potential cost for face-to-face review for 3961 patients (€129 per patient) within the Irish healthcare setting is €510 969. Costs incurred in treating all these patients via a virtual fracture clinic model (€28 per patient) was calculated to be €110 908. A total of 2770 patients (2776, minus six unplanned representations to the fracture clinic for index injury) who were discharged generated a saving (€101 per patient) to the orthopaedic department of €279 770. A conservative estimation of potential savings assumes that none of the 171 patients who had an unscheduled return to the PED would have returned if they had been seen in a face-to-face orthopaedic clinic. Based on the average cost to the hospital of an assessment of a child in PED (€150 per patient),18 we calculate a net saving delivered from implementation of the virtual fracture clinic pathway as €254 120.
Discussion
A recent systematic review confirmed the safety, efficacy and cost-effectiveness of the virtual fracture clinic model within the broader provision of trauma services.19 However, it was notable that this review of 21 articles contained a single series of 253 children managed by a dedicated paediatric virtual fracture clinic pathway.6 Other reports describe results from isolated protocols to manage individual childhood injuries20 or describe an iterative processes to implement a virtual fracture clinic within the setting of district general hospital.21 Our cohort of 3961 paediatric trauma patients managed via a virtual fracture clinic is the largest published implementation of a virtual fracture clinic model that exclusively treats children. To our knowledge, this is the first study to examine the large-scale safety, utility and cost-effectiveness of a virtual fracture clinic pathway in the management of a broad range of childhood fractures exclusively within the setting of a specialist paediatric hospital.
Examination of our results demonstrates the importance of training and familiarity in the implementation of a new trauma system. Simple linear regression analysis highlights a positive correlation between discharge rates (R2 = 0.41) and time from instigation of the virtual fracture clinic pathway. Similarly, a negative correlation between orthopaedic OPD referrals rates and time (R2 = 0.37) was observed. These correlations are suggestive of an improving familiarity and confidence of both orthopaedic and PEM staff with the virtual fracture clinic protocols. While no strong correlation with time was appreciated for rate of re-referral to PED (R2 = 0.006) or direct admission rates for surgical intervention (R2 = 0.02), it should be appreciated that absolute numbers of cases in these series were likely too small to detect a relationship despite the size of the prospective database. A pattern of increased diversion back to the PED and OPD review rate was noted for periods when the PEM and orthopaedic trainee’s changeover (annually in January and July) and we hypothesize that this may be due to an initial lack of familiarity with the conditions and processes for referral.
A significant barrier to continued success of this model of care is the lack of recognition of the financial gains of implementing such a service.2,22 The magnitude of any potential savings is predicated on local economic factors. Based on known costing within the Irish healthcare system, implementation of a paediatric virtual fracture clinic generated savings of €254 120 for our hospital. We expect that savings realized in other jurisdictions would vary from our local experience. It is important to state that our calculated savings are a significant underestimation of the wider societal savings accruing from reduced absence from school and reduced costs incurred to parents in time of work, travel and child-care expenses.23,24 Around 15 years ago, Morris and Bell23 estimated that each face-to-face fracture clinic appointment costs 0.25 work days, 0.18 days wages and 0.54 days schooling. As a current local model of the socio-economic impact of attendances to a children’s fracture clinic is not available, a more complete estimation of the broader economic impact of a virtual fracture clinic in minor children’s trauma is beyond the scope of this study and represents an avenue for further research.
A limitation of this study is that we did not prospectively capture patient satisfaction with a patient-related outcome measure. This constraint is currently unavoidable to the lack of adequate child-specific patient-related outcome measures for children’s trauma. Furthermore, since all fractures are unpleasant, without a control group we feel the patients would lack context for their experience. Finally, the validity of visual analogue scales and other instruments has been challenged of late, with some arguing against their usefulness.25 That said, a prospective case control study would be useful in assessing patient satisfaction, and would represent an avenue for further academic investigation.
It is important to note that the guardians of all children who were discharged were given an easy avenue to re-engage with the orthopaedic department if they were unhappy with their outcomes after fulfilling the proscribed treatment algorithm. Review of both local theatre logs and the national radiological archiving system reports that only 0.1% (n = 3) of those who were discharged via the virtual fracture clinic subsequently underwent operative treatment relating to their index injury. All of these children sought treatment in the index institution. This rate of unplanned operative intervention is lower than we would have normally anticipated and lower than has been reported in face-to-face orthopaedic and trauma interactions.26,27 We attribute this largely to the fact that the injuries referred to the virtual fracture clinic pathway were at the lower end of complexity. Other contributing factors may be the regular collaborative quality improvement meetings and the ability to rapidly refer indeterminate diagnosis directly to either the PED or orthopaedic outpatient clinics. Expert reporting of radiological investigations by a specialist paediatric radiologist is also a significant factor. The low observed incidence of unplanned returns indicates that the pathway provides safe care. This study was performed in Ireland where all operative children’s fracture management is prospectively captured by the national radiology archive (NIMIS). This has given us confidence to measure the outcomes of the virtual fracture clinic with the understanding that we could potentially loose only the very small number of children who would seek operative fracture management internationally. Localities with multiple institutions providing operative children’s trauma would need to act cooperatively in order to safely implement a similar pathway.
This prospective study has illustrated that creating a paediatric virtual fracture clinic pathway allows the majority of paediatric minor trauma to be safely discharged without requiring further face-to-face interaction. Similar processes would be valuable to all institutions that face challenges in providing an adequate service within the constraints of available resources. In the setting of the COVID-19 pandemic a virtual fracture clinic pathway confers further benefit to patients and families by maintaining social distancing and reducing physical exposure to hospital settings.
Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical statement
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed patient/guardian consent was waived as not required.
ICMJE Conflict of interest statement
None declared.
Acknowledgements
We would like to acknowledge the assistance of Dr. Mark Camp, (Dept. of Orthopaedics, The Hospital for Sick Children, Toronto, Canada) for his assistance in developing injury management protocols. The authors would like to thank Mr. Jacques Noel, Ms. Ciara Egan, Ms. Paula Kelly and Mr. Patrick Kiely for contributing data from their virtual fracture clinics. We would also like to thank Ms. Lauren Kelly (Dept. of Orthopaedics, Children’s Health Ireland at Crumlin, Dublin, Ireland) for her assistance in prospectively maintaining the database of patient outcomes on which this study is based. We would finally like to thank Mr. John Corcoran (Advanced Nurse Practitioner) for his invaluable assistance in running the virtual fracture clinics.
Author Contributions
JK: Study design, Draft, Data Analysis.
CB: Study design, Draft.
MB: Study design, Draft.
PO’T: Draft.
DM: Study design, Draft.
Supplemental Material
Supplemental material is available for this paper at https://online.boneandjoint.org.uk/doi/suppl/10.1302/1863-2548.15.200235
References
- 1. Keesara S, Jonas A, Schulman K. Covid-19 and health care’s digital revolution. N Engl J Med 2020;382:e82. [DOI] [PubMed] [Google Scholar]
- 2. Anderson GH, Jenkins PJ, McDonald DA, et al. Cost comparison of orthopaedic fracture pathways using discrete event simulation in a Glasgow hospital. BMJ Open 2017;7:e014509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Keshet D, Bernstein M, Dahan-Oliel N, et al. Management of common elective paediatric orthopaedic conditions during the COVID-19 pandemic: the Montreal experience. J Child Orthop 2020;14:161-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Holgate J, Kirmani S, Anand B. Virtual fracture clinic delivers British Orthopaedic Association compliance. Ann R Coll Surg Engl 2017;99:51-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Seewoonarain S, Babu S, Sangoi D, Avasthi A, Ricketts D. Introducing a virtual fracture clinic increases efficiency and reduces costs in torus fracture management. Pediatr Qual Saf 2019;4:e202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Robinson PM, Sim F, Latimer M, Mitchell PD. Paediatric fracture clinic re-design: incorporating a virtual fracture clinic. Injury 2017;48:2101-2105. [DOI] [PubMed] [Google Scholar]
- 7. Vardy J, Jenkins PJ, Clark K, et al. Effect of a redesigned fracture management pathway and ‘virtual’ fracture clinic on ED performance. BMJ Open 2014;4:e005282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Koenig KM, Bozic KJ. Orthopaedic healthcare worldwide: the role of standardization in improving outcomes. Clin Orthop Relat Res 2015;473:3360-3363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Boutis K. Common pediatric fractures treated with minimal intervention. Pediatr Emerg Care 2010;26:152-157. [DOI] [PubMed] [Google Scholar]
- 10. Boutis K. The emergency evaluation and management of pediatric extremity fractures. Emerg Med Clin North Am 2020;38:31-59. [DOI] [PubMed] [Google Scholar]
- 11. Boutis K, Plint A, Stimec J, et al. Radiograph-negative lateral ankle injuries in children: occult growth plate fracture or sprain? JAMA Pediatr 2016;170:e154114. [DOI] [PubMed] [Google Scholar]
- 12. Boutis K, Willan A, Babyn P, Goeree R, Howard A. Cast versus splint in children with minimally angulated fractures of the distal radius: a randomized controlled trial. CMAJ 2010;182:1507-1512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cuomo AV, Howard A, Hsueh S, Boutis K. Gartland type I supracondylar humerus fractures in children: is splint immobilization enough? Pediatr Emerg Care 2012;28:1150-1153. [DOI] [PubMed] [Google Scholar]
- 14. Farias M, Jenkins K, Lock J, et al. Standardized Clinical Assessment And Management Plans (SCAMPs) provide a better alternative to clinical practice guidelines. Health Aff (Millwood) 2013;32:911-920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ferguson KB, McGlynn J, Jenkins P, et al. Fifth metatarsal fractures - Is routine follow-up necessary? Injury 2015;46:1664-1668. [DOI] [PubMed] [Google Scholar]
- 16. von Keyserlingk C, Boutis K, Willan AR, Hopkins RB, Goeree R. Cost-effectiveness analysis of cast versus splint in children with acceptably angulated wrist fractures. Int J Technol Assess Health Care 2011;27:101-107. [DOI] [PubMed] [Google Scholar]
- 17. Reilly MO. A national virtual fracture clinic service: a more tactful approach. Int J Orthop Trauma & Surg Sci 2020;6:35-38. [Google Scholar]
- 18. Ireland CsH . Children’s Health Ireland Annual Report 2019. https://childrenshealthireland.ie/connolly/childrens-health-ireland-annual-report-2019/ (date last accessed 30 March 2021).
- 19. Khan SA, Asokan A, Handford C, Logan P, Moores T. How useful are virtual fracture clinics?: a systematic review. Bone Joint Open 2020;1:683-690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Calder JD, Solan M, Gidwani S, Allen S, Ricketts DM. Management of paediatric clavicle fractures—is follow-up necessary? An audit of 346 cases. Ann R Coll Surg Engl 2002;84:331-333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Logishetty K. Adopting and sustaining a Virtual Fracture Clinic model in the District Hospital setting - a quality improvement approach. BMJ Qual Improv Rep 2017;6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kaplan R, Porter M. The big idea: how to solve the cost crisis in health care. Harvard Business Review. http://hbr.org/2011/09/how-to-solve-the-cost-crisis-in-health-care/ar/1 (date last accessed 30 March 2021). [PubMed]
- 23. Morris MW, Bell MJ. The socio-economical impact of paediatric fracture clinic appointments. Injury 2006;37:395-397. [DOI] [PubMed] [Google Scholar]
- 24. Holm AGV, Lurås H, Randsborg P-H. The economic burden of outpatient appointments following paediatric fractures. Injury 2016;47:1410-1413. [DOI] [PubMed] [Google Scholar]
- 25. Ring D, Leopold SS. Editorial-measuring satisfaction: can it be done? Clin Orthop Relat Res 2015;473:3071-3073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bernatz JT, Tueting JL, Hetzel S, Anderson PA. What are the 30-day readmission rates across orthopaedic subspecialties? Clin Orthop Relat Res 2016;474:838-847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wheeler KK, Shi J, Xiang H, Thakkar RK, Groner JI. US pediatric trauma patient unplanned 30-day readmissions. J Pediatr Surg 2018;53:765-770. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.