Abstract
Purpose
Controversy exists regarding fibular status related to tibial alignment after congenital pseudarthrosis of the tibia (CPT) achieves union. We aimed to determine whether fibular status affected frontal plane tibial alignment post-CPT union.
Methods
Between January 2010 and December 2013, we followed 36 patients treated using a combined surgical technique (mean 6.6 years (2.2 to 9.4)). Outcome measures comprised medial proximal tibial angle, tibial diaphyseal angulation, lateral distal tibial angle (LDTA), relative intramedullary rod length and relative fibula length discrepancy.
Results
The frequency of proximal tibial valgus deformity and ankle valgus deformity were significantly lower in the fibular integrity group than in the fibular un-integrity group (proximal tibial valgus deformity: 2/17 versus 11/19; p = 0.006; ankle valgus deformity: 10/17 versus 18/19; p = 0.016). The mean LDTA was notably higher in the fibular integrity group than in the fibular un-integrity group (81.2° (sd 6.7°) versus 71.3° (sd 6.6°); p < 0.001). A statistically significant difference was observed in relative fibula length discrepancy between patients with fibular integrity (0.06 (0 to 0.11); Malhotra grade 0, n = 6; Malhotra grade I, n = 11) and those without (0.24 (0.01 to 0.36); Malhotra grade 2, n = 2; Malhotra grade 3, n = 17; p < 0.001). Ankle valgus deformity had a significant positive correlation with proximal tibial valgus deformity (r = 0.402; p = 0.015). Patients with an intact and normal length fibula had a lower frequency of ankle valgus deformity than those with an intact but shortening fibula (1/6 versus 9/11; p = 0.035).
Conclusion
Shortening or pseudarthrosis of the fibula was associated with ankle valgus and proximal tibial valgus deformities post-CPT union.
Level of evidence
III
Keywords: fibular status, congenital pseudarthrosis of the tibia, tibial alignment
Introduction
Congenital pseudarthrosis of the tibia (CPT) presents as a spontaneous pathological tibial fracture and scarcely achieves bony union; it remains a challenging condition to treat successfully in children. As surgical techniques for CPT have improved, primary bony union has exceeded 80%.1 We have acquired a high frequency of primary healing (89% to 95%) using the combined surgical technique to treat CPT.2,3
Nevertheless, some complications are still unavoidable after the union of CPT.3,4 Tibial malalignment in the frontal plane existed in > 50% of patients after the union was achieved.5 Tibial malalignment often needs to be corrected by surgery to prevent imbalanced stress distribution in the lower extremity, decrease the risk of refracture and maintain patients’ normal walking ability.
To date, the critical target in treating CPT is the achievement of a straight, functional extremity after bony union.6 Some researchers stated that the intramedullary rod (IMR) could restore tibial alignment in CPT.7 However, tibial malalignment in the frontal plane cannot be avoided in patients treated with IMR.8 Some authors proposed that an intact fibula can maintain tibial alignment,9 but Vigouroux et al10 disclosed that tibial malalignment was independent of fibular pseudarthrosis.
It is still unclear whether fibular pseudarthrosis can affect the tibial alignment or whether fibular shortening correlates with tibial malalignment in the frontal plane. Besides, researchers seldom place much importance on this problem. This study aimed to identify whether fibular status can affect tibial alignment in the frontal plane after healing of pseudarthrosis.
Materials and methods
The medical records of 63 patients with CPT, who were diagnosed and treated at the authors’ institution between January 1 2010 and December 31 2013, were analyzed retrospectively. Inclusion criteria were: 1) no record of preliminary history of operations in patients with CPT; 2) the patients were treated by the combined surgical operation; 3) each surgery was performed or supervised by a single surgeon (HBM) and a postoperative follow-up was conducted for more than two years; 4) patients were preoperatively diagnosed with or without fibular pseudarthrosis; 5) patients achieved primary bone union that presented as cortex-bridging fragments with sufficient thickness and radiodensity at the site of tibial pseudarthrosis after the index surgery on anteroposterior and lateral radiographs.11 Exclusion criteria were patients who underwent tibial lengthening procedures in the initial surgery or those with incomplete clinical data and radiographic images. We excluded 27 patients and included 36 patients (24 boys and 12 girls) with unilateral CPT in this study.
Surgical technique
The surgical technique, based on our previous reports,2,3 consisted of complete resection of the pseudarthrosis and surrounding hamartomatous tissue, a trans-calcaneal IMR, namely, a Williams IMR, consisting of an indwelling rod and an insertion rod, was inserted into the medullary canal of the involved tibia in a proximal to distal direction via the talus and the calcaneus and out through the heel pad. Using wrapped cancellous bone grafting, a rectangular cortex (size 4 cm x 4 cm) was obtained from the outer wall of the ilium, along with as much curetted cancellous bone as possible that could be taken from the supra-acetabular region. A 1.5-mm Kirschner-wire was used to make several holes in the rectangular cortex and absorbable sutures were weaved through the rectangular cortex to mould a cylindrical shape. An Ilizarov external fixator was then fitted.
If fibular pseudarthrosis existed in patients, it was stabilized by a 1.6-mm to 1.8 mm Kirschner-wire after the surrounding hamartomatous tissue was resected. The Kirschner-wire size was chosen according to the fibular diameter and the patient’s age at surgery.
If patients had an intact fibula, proximal fibular osteotomy was performed to increase compression forces on the ends of the tibial pseudarthrosis when the Ilizarov external fixator was used to keep both segments of the pseudarthrosis secure. The treatment regimen in all patients was not performed distal tibiofibular synostosis during the primary surgery.
Pharmacological protocol
Intravenous pamidronate disodium was administered one week following the primary surgery and following removal of the external fixation device and at three to four-month intervals thereafter over a two-year duration.
Postoperative management
The location through which the Kirschner-wire penetrated the skin was routinely disinfected with 75% alcohol once daily after the operation. On the first, sixth and 12th weeks postoperatively, the radiograph films were obtained to observe healing conditions. When the tibial pseudarthrosis was consolidated, the Ilizarov external fixator was removed. Then, the tibia was immobilized in a short-leg cast for an average of two months. When the cast was removed, all the patients wore a knee-ankle-foot orthosis until skeletal maturity to prevent refracture. The anteroposterior radiograph film was obtained to monitor the status and development of the lower leg.
For the intention of preventing ankle joint stiffness, with the aid of C-arm fluoroscopes, the distal end of the IMR in the calcaneus was pushed into the epiphysis of the distal tibia by a 2.5-mm Kirschner-wire at 18 to 24 months after tibial pseudarthrosis healed.
Medial proximal tibial angle (MPTA)
The MPTA was quantified using the medial angle between a line parallel to the proximal physis and another line along the anatomical axis of the proximal third of the tibial diaphyseal on an anteroposterior radiograph (Fig. 1). Using the contralateral limb for comparison, the proximal tibial valgus deformity was defined as an MPTA > 93° and a proximal tibial varus deformity was defined as an angle < 85º.3,12
Fig. 1.

Schematic illustration of the measurements obtained from an anteroposterior radiograph. a: Medial proximal tibial angle (MPTA), the angle between a line parallel to the proximal physis and another line along the anatomic axis of the proximal third of the tibial diaphyseal; b: tibial diaphyseal angulation, the angle between the proximal tibial anatomic axis and the distal tibial anatomic axis; c: Lateral distal tibial angle (LDTA), the angle between the tibial mid-diaphyseal line and a line created across the superior facet of the talus. The distal fibular epiphysis was at the level between the distal tibial epiphyseal line and the talar platform.
Tibial diaphyseal angulation
An acute angle of the proximal tibial anatomical axis with the distal tibial anatomical axis was utilized to indicate the severity of tibial diaphyseal angulation (Fig. 1). Using the contralateral limb for comparison, the normal value for tibial diaphyseal angulation was 0°. The tibial diaphyseal angulation orientation was classified as either tibial diaphyseal valgus deformity when the distal tibial anatomic axis oriented only laterally or tibial diaphyseal varus deformity when found only medially.
Lateral distal tibial angle (LDTA)
The LDTA was measured by the lateral angle between the distal tibial anatomic axis and a line created across the superior articular facet of the talus (Fig. 1). Using the contralateral limb for comparison, an ankle valgus or varus deformity was confirmed when the LDTA was < 85º or > 90º, respectively.3,13
Relative IMR length
The relative length of the IMR was calculated as the ratio of the IMR length over the tibial length at the final follow-up (Fig. 2).
Fig. 2.
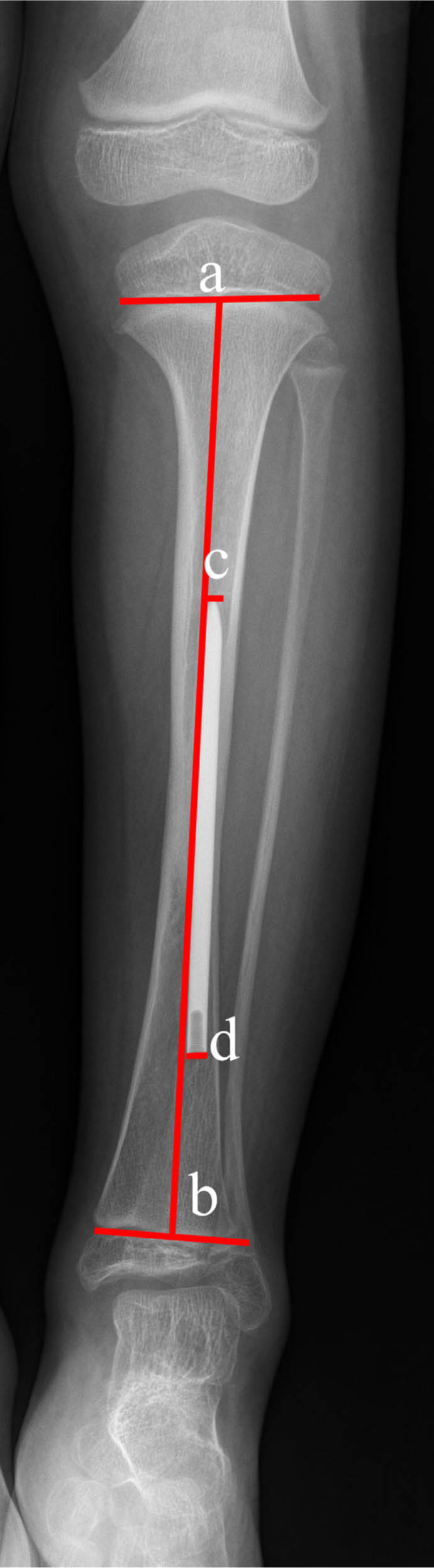
Schematic illustration of the relative intramedullary rod (IMR) length .The value of cd/ab defines the relative IMR length. The distal fibular epiphysis was located at the same level as the distal tibial physis.
Relative fibula length discrepancy
Relative fibula length discrepancy included the difference in the ratio between the affected fibula length and the unaffected fibula length divided by the unaffected fibula length and the difference between the ipsilateral tibia and fibula of the involved limb. If pseudarthrosis of the fibula was present, the proximal and distal longitudinal lines from the pseudarthrosis site were measured to calculate the affected fibula length. The relative fibula length discrepancy between the ipsilateral tibia and fibula of the involved limb was assessed using the Malhotra classification,14 which involves four levels: i) grade 0, reasonable fibula length, indicating that the distal fibula physis is located at the level of the talar dome; ii) grade 1, slightly shortening, implying that the distal fibula physis is located at a level between the distal tibial epiphyseal line and the talar dome; iii) grade 2, moderate shortening, indicating that both the fibula and tibial physis are located at the same level; and iv) grade 3, severe shortening, implying that the distal fibula physis is located above the distal tibial physis and that the distal tibial epiphysis is wedge-shaped.
Fibular status
Based on continuity of the fibula when the tibial pseudarthrosis had healed postoperatively, we classified the status of the fibula as having: i) fibular integrity, that is, an unmanaged intact fibula preoperatively or pseudarthrosis of the fibula that had healed postoperatively; or ii) fibular un-integrity, in which the pseudarthrosis of the fibula had failed to achieve synostosis.
All outcome measurements were collected at the end of follow-up. If a refracture occurred, the data recorded prior to refracture was used.
Statistical analysis
Statistical significance was analyzed using SPSS 21.0 software (IBM Corp, Armonk, New York). Fisher’s exact test was used to compare the frequencies in sex, neurofibromatosis type 1(NF1), proximal tibial valgus deformity, proximal tibial varus deformity, tibial diaphyseal valgus deformity, tibial diaphyseal varus deformity, ankle valgus deformity and ankle varus deformity between the fibular integrity group and fibular un-integrity group. The measurement data had a normal distribution according to the Shapiro-Wilk test. The quantitative data are presented as the mean (sd) (normal distribution) or as the median and range (non-normal distribution). The independent samples t-test or rank-sum test (Mann-Whitney U test) was used to compare the LDTA, age at the time of surgery, relative length of the IMR, MPTA, relative fibula length discrepancy and follow-up duration between the groups. The Spearman rank correlation test was used to assess correlations that were considered significant if r ≥ 0.25. A p-value < 0.05 was considered statistically significant.
Interobserver agreements between three sets of measurements taken by three observers and intra-observer agreement between two sets of measurements taken by one observer were analyzed using an intraclass correlation coefficient (ICC) and Weighted Cohen’s kappa test. Concordance was determined as follows: < 0.2 (poor); 0.2 to 0.4 (low); 0.4 to 0.6 (moderate); 0.6 to 0.8 (good); and > 0.8 (excellent).
Results
Among the 36 study patients, the right leg was affected in 16 and the left leg in 20. NF-1 was noted in 26 patients. In all, 22 cases were preoperatively concomitant with fibular pseudarthrosis and 14 patients had an intact fibula. The tibial pseudarthrosis location was in the lower-third in 35 cases and the middle-third in one case. According to the Crawford classification15, three patients were classified as type II and 33 patients as type IV. The mean age at the operation was 2.4 years (0.8 to 7.8). The mean follow-up time was 6.6 years (2.2 to 9.4). Refracture occurred in seven patients more than two years after the primary surgery. No significant differences existed in sex, age at the time of surgery, NF1, the MPTA and LDTA between the fibular integrity group and fibular un-integrity group preoperatively, as shown in Table 1. For MPTA, tibial diaphyseal angulation, LDTA and Malhotra classification, the ICCs and Weighted Cohen’s kappa were > 0.7, indicating excellent agreement (Table 2).
Table 1.
Comparisons of preoperative general information between the fibular integrity group and the fibular un-integrity group
| Sex | NF1 | Age, yrs | MPTA, ° | LDTA, ° | |||
|---|---|---|---|---|---|---|---|
| Female | Male | Yes | No | Median (range) | Median (range) | Median (range) | |
| A | 5 | 12 | 11 | 6 | 2.0 (0.8 to 7.8) | 90 (88 to 91) | 90 (88 to 91) |
| B | 7 | 12 | 15 | 4 | 2.0 (0.9 to 8.9) | 90 (89 to 92) | 90 (89 to 92) |
| p-value* | 0.732* | - | 0.463* | 0.452† | 0.196† | 1.000† | |
Fisher’s exact test
Mann-Whitney U test
A, fibular integrity group; B, fibular un-integrity group; NF1, neurofibromatosis type 1; MPTA, medial proximal tibial angle; LDTA, lateral distal tibial angle
Table 2.
Evaluation of intra- and interobserver agreements for medial proximal tibial angle (MPTA) and tibial diaphyseal angulation, lateral distal tibial angle (LDTA) and Malhotra classification
| Observers | MPTA, ° | Tibial diaphyseal angulation, ° | LDTA, ° | Malhotra classification | p-value* |
|---|---|---|---|---|---|
| ICC (95% CI) | ICC (95% CI) | ICC (95% CI) | Cohen’s kappa (95% CI) | ||
| HJD-HJD | 0.982 (0.965 to 0.991) | 0.966 (0.934 to 0.983) | 0.938 (0.879 to 0.968) | 0.889 (0.797 to 0.982) | < 0.001 |
| HJD-HBM | 0.908 (0.819 to 0.953) | 0.857 (0.720 to 0.927) | 0.849 (0.705 to 0.923) | 0.778 (0.650 to 0.905) | < 0.001 |
| HJD-LYL | 0.820 (0.647 to 0.908) | 0.807 (0.622 to 0.902) | 0.755 (0.520 to 0.875) | 0.742 (0.603 to 0.880) | < 0.001 |
| HBM-LYL | 0.721 (0.453 to 0.858) | 0.892 (0.788 to 0.945) | 0.729 (0.468 to 0.862) | 0.799 (0.678 to 0.920) | < 0.001 |
ICC, intraclass correlation coefficient; CI, confidence interval
MPTA,Tibial diaphyseal angulation and LDTA were used the ICC test; Malhotra classification was evaluated by Weighted Cohen’s kappa test.
There were 17 patients with fibular integrity at the final follow-up, including three cases with fibular pseudarthrosis and 14 cases with an intact fibula preoperatively; 19 patients still had a non-integrity fibular pseudarthrosis due to failure of union (Table 3).
Table 3.
Data concerning 36 patients with congenital pseudarthrosis of the tibia in the frontal plane at final follow-up
| Case No. | Fibular status | MPTA, ° | Tibial diaphyseal angulation, °* | LDTA, ° | Relative fibular length discrepancy | |||
|---|---|---|---|---|---|---|---|---|
| Contra | AT | Contra | AT | Contra | AT | |||
| 1 | Integrity | 91 | 90 | 0 | 0 | 90 | 89 | 0.01 |
| 2 | Integrity | 89 | 87 | 0 | 6 | 89 | 85 | 0 |
| 3 | Un-integrity | 88 | 95 | 0 | 15 | 89 | 70 | 0.33 |
| 4 | Un-integrity | 90 | 90 | 0 | 0 | 90 | 81 | 0.13 |
| 5 | Un-integrity | 91 | 102 | 0 | 5 | 89 | 75 | 0.01 |
| 6 | Un-integrity | 90 | 97 | 0 | 10 | 90 | 70 | 0.29 |
| 7 | Integrity | 90 | 90 | 0 | 0 | 89 | 88 | 0.10 |
| 8 | Un-integrity | 90 | 85 | 0 | 15 | 90 | 65 | 0.23 |
| 9 | Un-integrity | 88 | 95 | 0 | 14 | 89 | 77 | 0.13 |
| 10 | Integrity | 91 | 91 | 0 | 0 | 91 | 89 | 0 |
| 11 | Un-integrity | 90 | 95 | 0 | 8 | 90 | 76 | 0.24 |
| 12 | Integrity | 90 | 87 | 0 | 9 | 89 | 75 | 0.06 |
| 13 | Integrity | 90 | 92 | 0 | 15 | 90 | 82 | 0.05 |
| 14 | Un-integrity | 92 | 90 | 0 | 13 | 90 | 62 | 0.33 |
| 15 | Integrity | 91 | 96 | 0 | 7 | 90 | 80 | 0.11 |
| 16 | Integrity | 90 | 88 | 0 | 7 | 91 | 74 | 0.08 |
| 17 | Un-integrity | 90 | 88 | 0 | 4 | 91 | 88 | 0.22 |
| 18 | Un-integrity | 93 | 94 | 0 | 13 | 89 | 63 | 0.06 |
| 19 | Integrity | 91 | 87 | 0 | 10 | 90 | 85 | 0 |
| 20 | Un-integrity | 89 | 86 | 0 | 7 | 90 | 66 | 0.27 |
| 21 | Un-integrity | 90 | 94 | 0 | 8 | 89 | 65 | 0.36 |
| 22 | Un-integrity | 88 | 85 | 0 | 12 | 90 | 72 | 0.25 |
| 23 | Un-integrity | 90 | 99 | 0 | 0 | 89 | 68 | 0.28 |
| 24 | Integrity | 90 | 93 | 0 | 12 | 90 | 90 | 0.10 |
| 25 | Integrity | 90 | 90 | 0 | 0 | 90 | 90 | 0 |
| 26 | Integrity | 90 | 92 | 0 | 0 | 88 | 76 | 0.09 |
| 27 | Un-integrity | 92 | 93 | 0 | 16 | 90 | 70 | 0.24 |
| 28 | Integrity | 90 | 85 | 0 | 0 | 90 | 80 | 0.06 |
| 29 | Un-integrity | 90 | 94 | 0 | 13 | 90 | 65 | 0.22 |
| 30 | Un-integrity | 90 | 95 | 0 | 0 | 88 | 75 | 0.35 |
| 31 | Integrity | 92 | 87 | 0 | 10 | 89 | 79 | 0.09 |
| 32 | Integrity | 92 | 90 | 0 | 17 | 90 | 70 | 0.03 |
| 33 | Un-integrity | 92 | 110 | 0 | 0 | 90 | 75 | 0.22 |
| 34 | Un-integrity | 90 | 87 | 0 | 9 | 89 | 72 | 0.20 |
| 35 | Integrity | 92 | 97 | 0 | 0 | 88 | 71 | 0.02 |
| 36 | Integrity | 91 | 93 | 0 | 0 | 89 | 78 | 0.09 |
tibial diaphyseal valgus deformity
MPTA, medial proximal tibial angle; LDTA, lateral distal tibial angle; Contra, contralateral; AT, affected tibia
At the final follow-up, 35 patients could bear weight and walk normally, and one patient with refracture was immobilized in a long-leg cast. No patients had restrictions in terms of knee joint range of movement, however, ankle joint stiffness was identified in five patients, comprising four patients with pseudarthrosis of the fibula and one patient with fibular integrity.
MPTA
At the final follow-up, the mean MPTA was lower in the fibular integrity group than in the fibular un-integrity group (90.3° (sd 3.3°) versus 93.4° (sd 6.2°)), but there were no statistical differences in MPTA between the groups (p = 0.077). However, proximal tibial valgus deformity developed in 2/17 patients (11.8%) in the fibular integrity group and 11/19 (57.9%) in the fibular un-integrity group, and this was statistically significantly different between the groups (p = 0.006). None of the patients had proximal tibial varus deformity in this study (Figs 3 and 4).
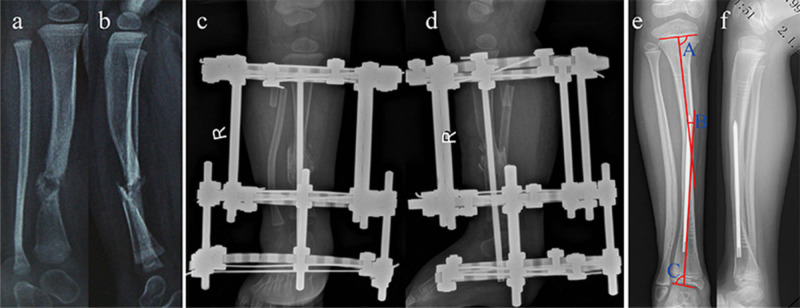
Fig. 3.
Preoperative frontal (a) and lateral (b) radiographs of an 11-month-old girl with Crawford type IV congenital pseudarthrosis of the right tibia with an intact fibula and associated neurofibromatosis type 1. Anteroposterior (c) and lateral (d) radiographs of the same patient presented at 1 week after combined surgery. Anteroposterior (e) and lateral (f) radiographs show the healed tibial pseudarthrosis with a normal fibula length and a normal medial proximal tibial angle (A, 87º), tibial diaphyseal valgus deformity (B, 10º), and lateral distal tibial angle (C, 85º) at 7 years after the combined surgery; the distal fibular physis was located at the level of the talar dome.
Fig. 4.
Preoperative frontal (a) and lateral (b) radiographs of a 4-year-old boy with Crawford type IV congenital pseudarthrosis of the right tibia with fibular pseudarthrosis and was not concomitant neurofibromatosis type 1. Anteroposterior (c) and lateral (d) radiograph of the same patient taken at 1 week after the combined surgery. Anteroposterior(e)and lateral (f) radiographs suggest bone union of tibial pseudarthrosis with Malhotra grade 3 fibular shortening displaying proximal tibial valgus deformity (A, 95°) and ankle valgus deformity(B, 75°) at 4 years postoperatively; a persistent non-union of the fibula and the distal fibular physis was located above the distal tibial physis.
Tibial diaphyseal angulation
In this study, no patients presented with tibial diaphyseal varus deformity. In the fibular integrity group, 9/17 patients (52.9%) developed tibial diaphyseal valgus deformity with a median deformity of 10° (6° to 17°). In the fibular un-integrity group, 15/19 patients (78.9%) had tibial diaphyseal valgus deformity with a median deformity of 12° (4° to 16°). No between-group statistical differences were found in terms of tibial diaphyseal valgus deformity (p = 0.158).
LDTA
In the fibular integrity group, the mean LDTA was 81.2° (sd 6.7°), and in the fibular un-integrity group, the mean LDTA was 71.3° (sd 6.6°). The LDTA was statistically significantly different between the groups (p < 0.001).
In the fibular integrity group, 10/17 patients (58.8%) with ankle valgus deformity had a mean deformity of 76.5° (70° to 82°). In the fibular un-integrity group, 18/19 patients (94.7%) with ankle valgus deformity had a mean deformity of 70.4° (62° to 81°). There was a statistically significant difference in ankle valgus deformity between the groups (p = 0.016). None of the cases exhibited ankle varus deformity in this study.
Relative IMR length
No statistical differences were observed in relative IMR length and follow-up duration between the fibular integrity group and fibular un-integrity group (relative IMR length 0.64 (sd 0.14) versus 0.70 (sd 0.12); p = 0.198; follow-up time 6.4 years (sd 2.0) versus 6.8 years (sd 1.7); p = 0.484).
Relative fibula length discrepancy
In the fibular integrity group, the median value was 0.06 (0 to 0.11); six patients displayed overgrowing, five patients had a normal fibula length and six patients had a shortened fibula (Malhotra grade 0, n = 6; Malhotra grade 1, n = 11). In the fibular un-integrity group, the median value was 0.24 (0.01 to 0.36) and all patients had fibular shortening (Malhotra grade 2, n = 2; Malhotra grade 3, n = 17). There was a statistically significant difference in relative fibula length discrepancy and severity of fibular shortening between patients with fibular integrity and those without (p < 0.001).
The severity of fibular shortening negatively correlated with LDTA (correlation coefficient (r) -0.694; p < 0.001).
Based on fibular integrity, patients were divided into two groups according to the extent of fibular shortening: the normal fibular length group (six cases) and the fibular shortening group (11 cases). No significant differences in tibial diaphyseal angulation and proximal tibial valgus deformity were observed between the groups, however, the normal fibular length group demonstrated a statistically significant lower incidence of ankle valgus deformity than the fibular shortening group (Table 4).
Table 4.
Postoperative tibial malalignment in patients with an intact fibula
| Proximal tibial valgus deformity | Tibial diaphyseal angulation | Ankle valgus deformity | ||||
|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | |
| Normal fibular length group | 0 | 6 | 4 | 2 | 1 | 5 |
| Fibular shortening group | 2 | 9 | 5 | 6 | 9 | 2 |
| p-value* | - | 0.515 | - | 0.620 | - | 0.035 |
Fisher’s exact test
The relationship between proximal tibial valgus deformity and ankle valgus deformity
Considering that there was a significantly higher incidence of proximal tibial valgus deformity and ankle valgus deformity in the fibular un-integrity group than in the fibular integrity group, we found that ankle valgus deformity had a significant positive correlation with proximal tibial valgus deformity (r = 0.402; p = 0.015).
Discussion
Regarding the fibular status when tibial pseudarthrosis heals, many researchers only focused on whether fibular pseudarthrosis was united. In this study, we considered the condition of fibular pseudarthrosis healing and relative fibula length discrepancy. We found that fibular pseudarthrosis could result in ankle valgus deformity and proximal tibial valgus deformity after the CPT union, and there was a significant positive correlation between ankle valgus deformity and proximal tibial valgus deformity. Even in patients with an intact fibula, fibular shortening can also cause ankle valgus deformity.
Some researchers believe that the involved tibia in patients should be amputated early to preserve extremity function with an adequate prosthesis because the residual deformities impair the affected lower-extremity walking function.16 One of the typical residual deformities was tibial malalignment in the frontal plane, which includes proximal tibial valgus and ankle valgus deformities and tibial diaphyseal angulation. To address this rather intractable problem, Charnley17 first reported that using an IMR to transfix the talus and calcaneus successfully treated two cases of CPT in 1956, demonstrating that an IMR can maintain the involved tibial alignment and turn abnormal angulation strains into longitudinal compression forces to reduce the possibility of refracture occurrence. Afterwards, there was a shared opinion that an IMR adds stability in the medullary canal to control tibial alignment.18 However, by applying an IMR for tibial pseudarthrosis in the combined surgical technique, we found that tibial malalignment cannot be eliminated in the frontal plane after the union is achieved.3 Other researchers have also reported that various surgical methods were used to treat CPT, such as the vascularized fibula or induced membrane technique and induced membrane combined IMR technique, and that tibial malalignment remained unresolved.10,19 This may imply that other factors affect tibial alignment after the union of CPT.
In total, > 60% of CPT cases were associated with fibular abnormalities or pseudarthrosis.20 Many researchers have previously overemphasized how to achieve a union of the tibia, and little attention was paid to treating fibular pseudarthrosis.
In this study, all patients were treated with an IMR, and the relative IMR length was not significantly different between the fibular integrity group and fibular un-integrity group. Our results indicated that fibular pseudarthrosis could cause proximal tibial valgus deformity but not affect tibial diaphyseal angulation. However, our study showed that fibular pseudarthrosis could progress to ankle valgus deformity, which agrees with other researchers’ views.20,21 Nevertheless, few researchers have reported that fibular pseudarthrosis has a relationship with proximal tibial malalignment. Wiltse20 also reported that if distal fibular pseudarthrosis develops in children before 11 or 12 years of age, a bone-grafting procedure should be performed to restore the distal length to prevent further ankle valgus.
In this study, we confirmed again that fibular shortening could result in ankle valgus deformity after the union of CPT. Moreover, our results suggest that the shorter fibular length was, the more apparent ankle valgus presented. The new finding of this study was proof that fibular pseudarthrosis can lead to proximal tibial valgus deformity. In addition, fibular pseudarthrosis can result in ankle valgus deformity, and ankle valgus deformity had a positive correlation with proximal tibial valgus deformity.
Possible biomechanical mechanisms for the occurrence of proximal tibial valgus deformity have been proposed. The fibula supports between 7% and 17% of one’s body weight in the lower extremity during walking.22 Recently, Burssens et al23 found that the hindfoot’s valgus mechanical axis could make the lower limb mechanical axis move laterally. Horn et al24 also reported using an Ilizarov external fixator or intramedullary nail to treat 20 cases of CPT and 13 of 16 patients who had ankle valgus deformity at the final follow-up presented with a laterally displaced mechanical axis of the involved lower extremity. If the lower limb mechanical axis is displaced laterally, it could increase compressive loads of the lateral compartment of the knee joint. According to the Hueter-Volkmann law,25 increasing pressure of the lateral compartment of the knee joint could inhibit lateral proximal tibial physis growth. Similarly, in our study, we found that ankle valgus deformity had a significant positive correlation with proximal tibial valgus deformity. Therefore, it seems that fibular pseudarthrosis contributed to the formation of ankle valgus deformity that could cause lateral displacement of the lower limb mechanical axis, resulting in proximal tibial valgus deformity.
There are several limitations to this study. The clinical and radiographic outcomes in patients were not followed up to skeletal maturity. Because of the nature of the retrospective study design, selective bias was inevitable in the enrolled cases, such as patients who achieved good union and maintained tibial alignment might have had a longer follow-up time and vice versa. We could not obtain long-standing radiographs to measure the whole lower extremities’ mechanical axis when patients developed proximal tibial valgus or ankle valgus deformity. However, we had crucial evidence that proximal tibial valgus deformity was more likely to occur when CPT healed but with fibular pseudarthrosis. Since this is an uncommon disease, this study included only a limited number of cases; especially, there were only six patients with a normal fibular length in the fibular integrity group.
In summary, the status of the fibula was found to be associated with tibial alignment in the frontal plane post-CPT union. Shortening or pseudarthrosis of the fibula was associated with ankle valgus and proximal tibial valgus deformities. For patients with an intact fibula preoperatively, a proximal fibular osteotomy is necessary to effectively promote tibial pseudarthrosis healing. However, close attention should be paid to managing union in patients with pseudarthrosis of the fibula and maintaining a normal fibula length to reduce the occurrence of tibial malalignment in the frontal plane post-CPT union. More clinical trials are required to verify our results and to determine the mechanisms involved in proximal tibial valgus deformity.
Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical statement
Ethical approval: This research involved human participants. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: The hospital research ethics committee approved this study (approval number: 2020PS767K), and informed consent was obtained from the participants’ parents or guardians before the survey was conducted.
ICMJE Conflict of interest statement
None of the authors received any funding for the study, and none has any potential conflict of interest.
Acknowledgements
The authors would like to thank Editage (www.editage.cn) for English language editing.
Author Contributions
HJD: Data collection and analysis, Manuscript preparation.
HBM: Data collection and analysis, Manuscript revision.
EBW: Data analysis, Manuscript revision.
QWL: Data analysis, Manuscript revision.
LJZ: Data analysis, Manuscript revision.
FC: Data analysis, Manuscript revision.
LYL: Project administration, Manuscript revision and analysis, Data collection.
References
- 1. Shah H, Rousset M, Canavese F. Congenital pseudarthrosis of the tibia: management and complications. Indian J Orthop 2012;46:616-626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Yan A, Mei H-B, Liu K, et al. Wrapping grafting for congenital pseudarthrosis of the tibia: A preliminary report. Medicine (Baltimore) 2017;96:e8835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zhu GH, Mei HB, He RG, et al. Combination of intramedullary rod, wrapping bone grafting and Ilizarov’s fixator for the treatment of Crawford type IV congenital pseudarthrosis of the tibia: mid-term follow up of 56 cases. BMC Musculoskelet Disord 2016;17:443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. El-Rosasy MA-M. Congenital pseudarthrosis of the tibia: the outcome of a pathology-oriented classification system and treatment protocol. J Pediatr Orthop B 2020;29:337-347. [DOI] [PubMed] [Google Scholar]
- 5. Inan M, El Rassi G, Riddle EC, Kumar SJ. Residual deformities following successful initial bone union in congenital pseudoarthrosis of the tibia. J Pediatr Orthop 2006;26:393-399. [DOI] [PubMed] [Google Scholar]
- 6. Eisenberg KA, Vuillermin CB. Management of congenital pseudoarthrosis of the tibia and fibula. Curr Rev Musculoskelet Med 2019;12:356-368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dobbs MB, Rich MM, Gordon JE, Szymanski DA, Schoenecker PL. Use of an intramedullary rod for the treatment of congenital pseudarthrosis of the tibia. Surgical technique. J Bone Joint Surg [Am] 2005;87-A(suppl 1):33-40. [DOI] [PubMed] [Google Scholar]
- 8. Shah H, Doddabasappa SN, Joseph B. Congenital pseudarthrosis of the tibia treated with intramedullary rodding and cortical bone grafting: a follow-up study at skeletal maturity. J Pediatr Orthop 2011;31:79-88. [DOI] [PubMed] [Google Scholar]
- 9. Ohnishi I, Sato W, Matsuyama J, et al. Treatment of congenital pseudarthrosis of the tibia: a multicenter study in Japan. J Pediatr Orthop 2005;25:219-224. [DOI] [PubMed] [Google Scholar]
- 10. Vigouroux F, Mezzadri G, Parot R, et al. Vascularised fibula or induced membrane to treat congenital pseudarthrosis of the tibia: A multicentre study of 18 patients with a mean 9.5-year follow-up. Orthop Traumatol Surg Res 2017;103:747-753. [DOI] [PubMed] [Google Scholar]
- 11. Ohnishi I, Sato W, Matsuyama J, et al. Treatment of congenital pseudarthrosis of the tibia: a multicenter study in Japan. J Pediatr Orthop 2005;25:219-224. [DOI] [PubMed] [Google Scholar]
- 12. Paley D, Herzenberg J. Principles of deformity correction. Berlin, Heidelberg, New York: Springer-Verlag, 2002. [Google Scholar]
- 13. Rupprecht M, Spiro AS, Schlickewei C, et al. Rebound of ankle valgus deformity in patients with hereditary multiple exostosis. J Pediatr Orthop 2015;35:94-99. [DOI] [PubMed] [Google Scholar]
- 14. Malhotra D, Puri R, Owen R. Valgus deformity of the ankle in children with spina bifida aperta. J Bone Joint Surg [Br] 1984;66-B:381-385. [DOI] [PubMed] [Google Scholar]
- 15. Crawford AH, Schorry EK. Neurofibromatosis in children: the role of the orthopaedist. J Am Acad Orthop Surg. 1999;7(4):217-230. [DOI] [PubMed] [Google Scholar]
- 16. Westberry DE, Carpenter AM, Tisch J, Wack LI. Amputation outcomes in congenital pseudarthrosis of the tibia. J Pediatr Orthop 2018;38:e475-e481. [DOI] [PubMed] [Google Scholar]
- 17. Charnley J. Congenital pseudarthrosis of the tibia treated by intramedullary nail. J Bone Joint Surg [Am] 1956;38-A:283-290. [PubMed] [Google Scholar]
- 18. Kesireddy N, Kheireldin RK, Lu A, et al. Current treatment of congenital pseudarthrosis of the tibia: a systematic review and meta-analysis. J Pediatr Orthop B 2018;27:541-550. [DOI] [PubMed] [Google Scholar]
- 19. Pollon T, Sales de Gauzy J, Pham T, Thévenin Lemoine C, Accadbled F. Salvage of congenital pseudarthrosis of the tibia by the induced membrane technique followed by a motorised lengthening nail. Orthop Traumatol Surg Res 2018;104:147-153 [DOI] [PubMed] [Google Scholar]
- 20. Wiltse LL. Valgus deformity of the ankle: a sequel to acquired or congenital abnormalities of the fibula. J Bone Joint Surg [Am] 1972;54-A:595-606. [PubMed] [Google Scholar]
- 21. Cho T-J, Choi IH, Chung CY, et al. Isolated congenital pseudarthrosis of the fibula: clinical course and optimal treatment. J Pediatr Orthop 2006;26:449-454. [DOI] [PubMed] [Google Scholar]
- 22. Goh JC, Mech AM, Lee EH, et al. Biomechanical study on the load-bearing characteristics of the fibula and the effects of fibular resection. Clin Orthop Relat Res 1992;279:223-228. [PubMed] [Google Scholar]
- 23. Burssens ABM, Buedts K, Barg A, et al. Is lower-limb alignment associated with hindfoot deformity in the coronal plane? A weightbearing CT analysis. Clin Orthop Relat Res 2020;478:154-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Horn J, Steen H, Terjesen T. Epidemiology and treatment outcome of congenital pseudarthrosis of the tibia. J Child Orthop 2013;7:157-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mehlman CT, Araghi A, Roy DR. Hyphenated history: the Hueter-Volkmann law. Am J Orthop 1997;26:798-800. [PubMed] [Google Scholar]