Abstract
Objectives
To evaluate the reliability of high‐resolution CT scans (HRCT scans) in the diagnosis of tympanosclerosis and to determine its benefit to predict the post‐surgical hearing outcome based on comparing radiological and surgical findings.
Methods
A retrospective study at a tertiary institute included 940 ears that underwent tyampanoplasty for chronic suppurative otitis media (CSOM) between January 2013 and March 2017. Preoperative temporal bone HRCT scans were analyzed to check for the prediction of tympanosclerosis and ossicular fixation. Intraoperatively, ossicular chain integrity was checked. Preoperative and postoperative audiometric evaluations using air‐bone gap (ABG) were compared. A postoperative pure‐tone ABG of 20 dB or less was considered as a successful hearing result. Results are compared with historical control groups, the study has been reviewed and approved by the IRB at the medical research center in Hamad Medical Corporation; however, it is a retrospective study so no informed consent was obtained from the patients.
Results
The study included 940 ears that underwent tympanoplasties due to CSOM, where 238 out of 940 (25.3%) of ears showed tympanosclerosis during tympanoplasty, intraoperatively, tympanosclerosis was localized to the eardrum in 174 of the 238 involved ears (73.1%), A 64 out of 238 (26.9%) of the ears with tympanosclerosis showed ossicular fixation, divided as 45 ears with Incudo‐malleal fixation, 14 ears with stapes fixation, and 5 ears with triple ossicular fixation. HRCT scan of the temporal bone was suggestive of ossicular chain fixation in 79 cases distributed as 55 incudo‐malleal fixations, 19 stapes fixation, and 5 complete ossicular fixations, with a sensitivity of 96.8%, and specificity of 98%. The audiological results were analyzed, with a patient follow‐up after 6 months.
Conclusions
Our study showed that CT scans when combined with the clinical findings can be an informative guide to otolaryngologists for preoperative evaluation and counseling of tympanosclerosis surgeries.
Keywords: chronic suppurative otitis media, CT scan, myringosclerosis, ossicular chain reconstruction, tympanoplasty, tympanosclerosis
1. INTRODUCTION
Chronic suppurative otitis media (CSOM) is a prevalent middle ear pathology that constitutes chronically inflamed middle ear mucosa in the presence of tympanic membrane perforation. CSOM is the leading cause of conductive hearing loss in adults, which is secondary to damage of the eardrum and middle ear ossicles induced by chronic inflammation present in the tympanic cavity.
Tympanosclerosis reflects deposits of hyalinized collagen in the tympanic cavity. It appears as unifocal or multifocal punctate or web‐like calcifications in the middle ear cavity or on the tympanic membrane (myringosclerosis). In the tympanic cavity (intratympanic), it may be present in any location, visible as focal calcified densities in the middle ear cavity, along with tendons, also in direct opposition to the ossicular chain. It is present in 7%‐38% of ears with CSOM. 1 , 2 , 3 , 4
Tympanosclerosis affects most frequently the tympanic membrane alone (50%). In 30%, middle ear structures are affected, as ossicular ligaments, interosseous joints, muscle tendons, and submucosal areas, causing varying degrees of fixity of the ossicular chain. 5 In 20%, tympanosclerosis affects both, tympanic membrane, and middle ear structures.
Intratympanic TS usually involves silent areas in the middle ear, Ossicular involvement is usually seen in about 30%‐40% of cases of intratympanic tympanosclerosis resulting in substantial conductive hearing loss. 1 , 2 , 3
Hearing restoration surgery in CSOM, aimed at disease eradication and hearing revival, comprises eardrum repair and ossicular chain reconstruction in‐ears housing defective ossicles. The latter scenario is associated with a higher rate of long‐term acoustic failure that may reach 50%. 6 , 7 Myringoplasty is the absence of ossicular damage is bracketed with a much higher long‐term success rate—more than 90% even in wet ears. 8 Ossicular fixation can only be confirmed intraoperatively. Therefore, the preoperative information given to the patient must be comprehensive and should include details of the probabilities of having ossicular dysfunction and the associated risk of acoustic failure with the possible need for revision surgery. Lacking prior information, patient prognosis, and surgical management techniques can only be determined during the surgery.
High‐resolution multidetector computed tomography (MDCT) is an excellent modality for the evaluation of a variety of conditions affecting the temporal bones. With the recently improved software in MDCT machines, it is now possible to obtain multiplanar reconstructions in all planes with nearly isotropic resolution. This helps immensely to delineate those structures which lie in different anatomical planes. A High‐Resolution CT scan of the temporal bone is a valuable method to detect the localization of tympanosclerosis in patients with chronic otitis media and conductive hearing loss. When combined with clinical findings, CT scans can be an informative guide to otolaryngologists for preoperative evaluation of tympanosclerosis. Tympanosclerosis is identified in CT scans as ossified or calcified high‐density regions in the soft tissue in the middle ear cavity, leading to ovoid, linear or web‐like forms.
This should help to predict ossicular chain status and therefore determine the conduct and the prognosis of ear surgery. This study was conducted to assess the potential value of HRCT in predicting OCF in CSOM. The findings of this study could be exploited to predict preoperatively the probability of having OCF in CSOM ears, and thus patients could be suitably informed, and an appropriate consent taken regarding these possible issues before surgery.
Clinico‐radiologic correlations have been established over a period of several years of follow‐up, aided by a series of typical tympanosclerotic aspects on CT imaging yet rarely reported in the literature, up to our knowledge there were no published studies in the literature that discussed the CT scan findings and their reliability for diagnosis of tympanosclerosis.
The main goal of this study was to specify the reliability of high‐resolution CT scans (HRCT scans) in the diagnosis of tympanosclerosis based on comparing radiological and surgical findings.
2. MATERIALS AND METHODS
2.1. Patients
We retrospectively searched our database for all patients who operated for tympanoplasty for non‐cholesteatoma CSOM within a period from January 2013 to March 2017. The diagnosis of CSOM was based on the clinical presentation of the chronically perforated tympanic membrane with a history of recurrent ear discharge. The charts of the patients were reviewed and all patients with cholesteatoma, ossicular chain discontinuity, or a history of previous otologic surgery were excluded from this study. We included 640 patients (940 ears) with CSOM in at least one ear.
At our institution, all patients with a clinical diagnosis of CSOM and planned for surgery undergo a CT scan preoperatively to confirm the diagnosis, exclude associated pathologies, evaluate the status of the middle ear and ossicles, and evaluate the anatomical conditions of the middle ear before surgery (eg, high jugular bulb, dehiscence or protrusion of facial nerve, sclerotic mastoid). We retrospectively reviewed the temporal bone CT scans and the medical chart of all 640 patients (940 ears).
No consent was obtained from the patients as it was a retrospective analysis, the study has been approved from HMC IRB with a license number of 16100/16.
2.2. Radiological evaluation
All the patients underwent a high‐resolution temporal bone CT scan using A 64 slice multi‐detector CT scan machine (Somatom Sensation, Siemens, Germany). 0.6 mm axial sections were acquired in all cases (120 kV, 60/100 mAs, collimation 0.75). Appropriate thinner slices up to 0.1 mm multiplanar reconstructions were carried out in all cases in all orthogonal planes. A Specialized team of neuro‐radiologists reported their findings in every case.
Tympanosclerosis usually appears as high‐density foci within the tympanic membrane or middle ear cavity. When the middle ear is involved, findings include high‐density foci or calcifications on the surface of the ossicles, thickening of the stapes crura and footplate, thickening and increased density of suspensory ligaments and muscle tendons. New bone formation is often considered to fall within the spectrum of tympanosclerosis.
Intratympanic tympanosclerosis can manifest by diffuse calcifications throughout the tympanic cavity and its recesses or even calcified block formations with narrowing of the lumen of the cavity.
Analysis of the ossicular chain for possible tympanoscleosis involvement was performed on several consecutive axial cuts in the caudo‐cranial direction. Coronal reconstruction allows analysis primarily of the attic fixation.
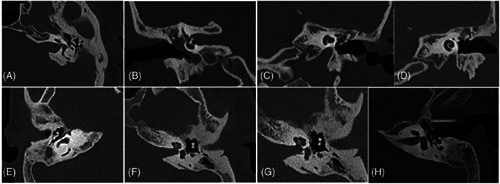
Tympanosclerosis of incudo‐malleal complex be variable condensation encases the incudo‐malleal complex and fixing it to the tegmen, lateral, medial, and/or anterior attic wall (Figure 1A‐E).
FIGURE 1.
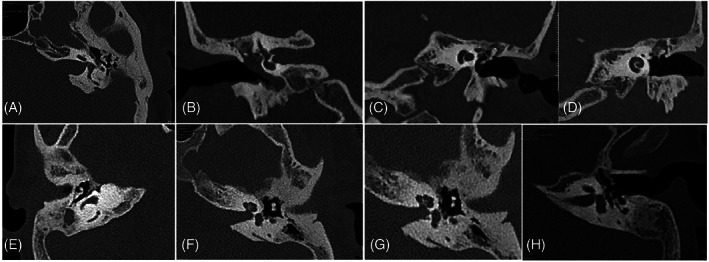
A, Axial CT‐image of a left ear, showing tympanosclerosis encases the incudo‐malleal complex and fixing it to the anterior attic wall. B, Coronal CT‐image of a left ear, showing tympanosclerosis extending around the head of malleus laterally, medially, and superiorly. C, Axial CT‐image of a left ear, showing tympanosclerosis with thickened footplate. D, Axial CT‐image of a left ear, showing tympanosclerosis with thickened stapedial crura. E, Axial CT‐image of a left ear, showing tympanosclerosis with calcified stapedial muscle tendon. F, Axial CT‐image of a right ear, showing tympanosclerosis extending between body of incus and lateral wall of attic. G, Axial CT‐image of a left ear, showing tympanosclerosis with thickened stapedial crura. H, Axial CT‐image of a left ear, showing tympanosclerosis with calcified stapedial muscle tendon
Tympanosclerosis of the stapedial complex can be seen as a global thickening of the crura and the footplate (Figure 1F,G), or with apposition of calcified material on the footplate or by a diffuse obliteration of the oval niche with sclerotic material, or by calcified stapedial tendon (Figure 1H), all are highly suggestive of tympanosclerosis.
2.3. Audiological evaluation
An audiological evaluation was carried out in a double‐walled sound room within at least 2 months before surgery, and 6 months after surgery in operated patients. Air and bone conduction four‐frequency pure‐tone average (PTA) and the air‐bone gap (ABG) were calculated according to the guidelines of the committee on hearing and equilibrium of the American Academy of Otolaryngology‐Head and Neck Surgery, using 0.5, 1, 2, and 3 kHz. 9 The sensorineural hearing level (SNHL) was estimated by averaging the bone‐conduction levels for frequencies 1, 2, and 3 kHz. The preoperative to postoperative change in SNHL was the measure of surgically induced sensorineural hearing loss.
2.4. Surgical technique
During middle ear surgery and after the elevation of the tympano‐meatal flap, exploration of the middle ear and evaluation of ossicular mobility, if there is an ossicular chain fixation, then incudo‐stapedial dislocation was carried out, thereafter stapes and incudo‐malleal complex mobility was checked separately. In cases where stapes was fixed, myringoplasty was carried out and a staged stapedectomy was planned after 6 months. In cases where incudo‐malleal complex fixation was found, the incus and head of the malleus were removed, and a partial ossicular replacement prosthesis (PORP) was placed inserted between the head of the stapes and handle of the malleus. In case of all ossicles were fixed, then only myringoplasty was done.
2.5. Statistical analysis
Statistical analyses were performed using SPSS statistics software (17th edition). Following testing for homogeneity of variance, parametric statistics were used, including one‐way analysis of variance (ANOVA) for comparison of all groups on all interval level measures, with pair‐wise comparisons by posthoc analysis using the Least Significant Difference (LSD) test. Paired‐comparison t‐tests were used to evaluate any change in BC from pre‐ to postoperatively for each group. The criterion for statistical significance was set at P ≤ .05.
3. RESULTS
We included 640 patients (940 ears) with CSOM who underwent tympanoplasties in at least one ear. The mean age was 32.8 + 11.3 years, the age range was from 5 to 58 years with a male‐female ratio of 1.7.
Figure 2 shows the clinical and surgical findings of the patients. Of the 940 of ears with CSOM, (238/940) 25.3% ears showed tympanosclerosis during middle ear exploration during tympanoplasty.
FIGURE 2.
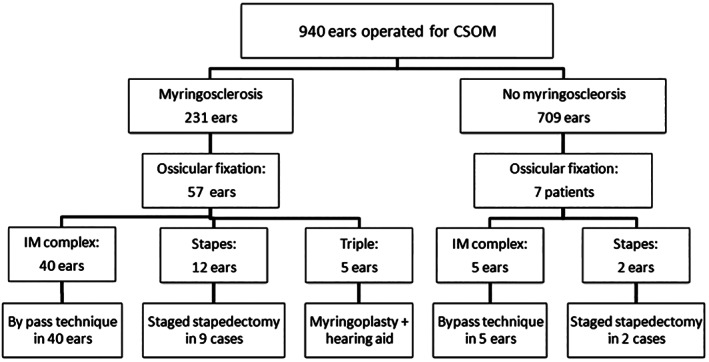
Summary of the clinical and surgical findings of the patients
Tympanosclerosis was localized to the eardrum (myringosclerosis) in (174/238) 73.1% of involved ears.
(64/238) 26.9% of ears with tympanosclerosis showed ossicular fixation, 7 of these ears did not show myringosclerosis.
Ossicular tympanosclerotic fixations were distributed as 45 (70.3%) ears with Incudo‐malleal fixation, 14 (21.9%) ears with stapes fixation and, 5 (7.8%) with triple ossicular fixation).
3.1. Radiological data and clinico‐radiological correlation
Of the 940 ears, preoperative HRCT was suggestive ossicular chain fixations in 79 cases (8.4%) distributed as 55 incudo‐malleal fixation, 19 stapes fixation, and 5 complete ossicular fixations. Intraoperative diagnosis of tympanosclerosis with ossicular fixation was found in 64 ears distributed as 43 out of the 55 ears with preoperative radiological suspicion of Incudo‐malleal fixation, 14 out of 19 ears with radiologically suspicious stapes fixation, and 5 out of 5 in suspicious triple fixation. Two ears out of the 861 ears with no radiological signs of ossicular tympanosclerosis showed ossicular fixation localized to the incudo‐malleal complex. A comparison of the radiological findings and the confirmed intraoperative TS data was summarized in Figure 3.
FIGURE 3.
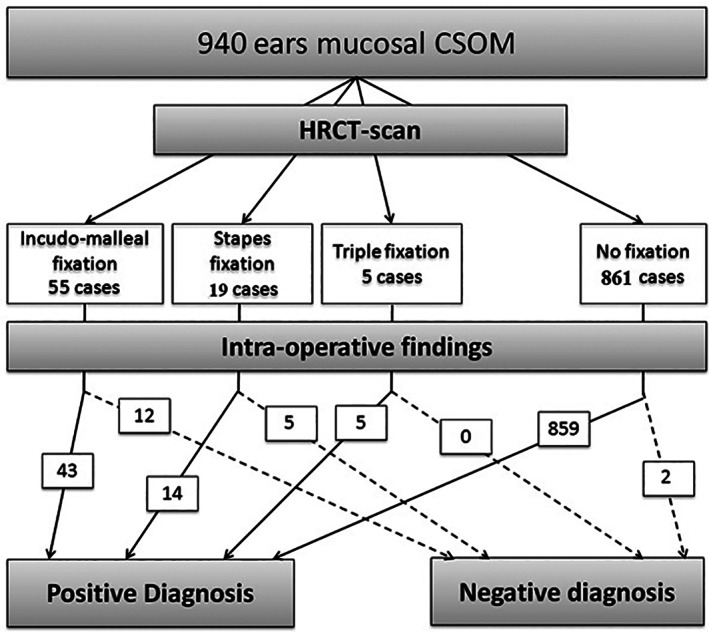
Summarize the radiological data and clinico‐radiological correlation
The comparison between radiological and intraoperative diagnosis of ossicular fixation tympanosclerosis is summarized in Table 1. It showed that the preoperative positive predictive value (PPV) of HRCT scan in the diagnosis of ossicular chain TS was 78.5% and its NPV is 99.7%.
TABLE 1.
Show the comparison between radiological and intraoperative diagnosis of ossicular fixation tympanosclerosis
| Positive surgical fixation | Negative surgical fixation | Total | ||
|---|---|---|---|---|
| Scans suggestive of fixation | 62 | 17 | 79 | PPV = 62/79, 78.6% |
| Scans not suggestive of fixation | 2 | 859 | 861 | NPV = 859/861, 99.7% |
| Total | 64 | 876 | 940 | |
| Sensitivity = 62/64, 96.8% | Specificity = 859/876, 98% |
Note: Positive predictive value (PPV) = 78.5%; negative predictive value = 99.7%; sensitivity = 96.8%; specificity = 98%.
3.2. Hearing outcome
A postoperative air‐bone gap (ABG) ≤ 20 dB was obtained in (908/940) 96.6% of the patients. We have divided the audiological results into three groups to ease the comparison between them and to emphasize the effect of the presence and the type of tympanosclerosis on hearing outcome as summarized in Table 2.
TABLE 2.
Outcome of hearing in different groups of CSOM post operatively
| Group 1—(CSOM without tympanoscelrosis) | Group 2—(CSOM with tympanoscelrosis) | Group 3—(CSOM ears with ossicular fixation tympanosclerosis) | Total | |
|---|---|---|---|---|
| Postoperative air‐bone gap (ABG) ≤ 20 dB | 691 | 168 | 49 | 908 |
| Postoperative air‐bone gap (ABG) > 20 dB | 11 | 6 | 7 | 24 |
| Total | 702 | 174 | 56 | 932 |
| 98.4% | 96.5% | 87.8% |
In the first group, which includes CSOM ears without tympanosclerosis, a postoperative air‐bone gap (ABG) ≤ 20 dB was obtained in (691/702) 98.4% of cases, the mean preoperative air‐bone gap (ABG) was 21.8 ± 6.9, mean, which becomes post‐operatively 5.4 ± 4.6 dB with P‐value .001. The mean preoperative bone conduction (BC) was 7.6 ± 5.1 dB when comparing it to the postoperative results with mean postoperative BC was 8.2 ± 4.8 dB with P‐value = .001.
In the second group, which includes CSOM ears with tympanosclerosis that limited to the tympanic membrane (myringosclerosis), a postoperative air‐bone gap (ABG) ≤ of 20 dB was obtained in (168/174) 96.5% of cases, the mean preoperative air‐bone gap (ABG) was 22 ± 7.3, mean, which becomes postoperatively 6.2 ± 5.3 dB with P‐value .001. The mean preoperative bone conduction (BC) was 7.8 ± 5.2 dB when compared to the postoperative results with mean postoperative BC was 8.8 ± 4.6 dB with P‐value = .001.
In the third group, which includes CSOM ears with ossicular fixation tympanosclerosis, a postoperative air‐bone gap (ABG) ≤ 20 dB was obtained in (49/56) 87.8% for all patients who underwent ossicular reconstruction, divided as (40/45) 88.8% for ossiculoplasty with Incudo‐malleal fixation tympanosclerosis, and (9/11) 81.8% for staged stapedectomy cases with operable stapes fixation tympanosclerosis.
The third group hearing outcome was divided into three subgroups depending on the site of the ossicular fixation and the surgical intervention required. The first subgroup was ears with Incudo‐malleal fixation, the mean preoperative air‐bone gap (ABG) was 32 ± 6.4 dB, mean, which becomes post‐operatively 13.9 ± 12 dB with P‐value .0001. The mean preoperative bone conduction (BC) was 6.9 ± 5.4 dB when comparing it to the postoperative results with mean postoperative BC was 9.5 ± 4.5 dB with P‐value = .001. The second subgroup was ears with stapes fixation, only 11 of 14 cases were operable for stapedectomy, the mean preoperative air‐bone gap (ABG) was 36.8 ± 2.5 dB, mean, which becomes postoperatively 17.7 ± 4.7 dB with P‐value .0001. The mean preoperative bone conduction (BC) in was 6.2 ± 6.2 dB, when compare it to the postoperative results with mean postoperative BC was 14 ± 6.6 dB with P‐value = .001. The third subgroup was ears with triple ossicular fixation, in this group, only tympanoplasty was done with no ossicular reconstruction surgery and they have been provided with a hearing aid for hearing rehabilitation.
When we compared the postoperative ABG results for group I, group II, and group III we can see that a successful postoperative ABG closure was found in 98.4%, 96.5%, and 87.8%, respectively. A comparison in the post‐operative ABG in group I to group II shows a high ABG closure rate with comparable post‐operative ABG values in both groups indicates that myringosclerosis effect on hearing outcome is limited with an insignificant P‐value of .3 while comparing group I and group III postoperative ABG closure were group I has a higher success rate with better values indicating that the presences of ossicular fixation tympanosclerosis have a poorer outcome with a statistically significant P value of .0001. A similar significant statistically P value (.0001) was found when comparing group II and group III postoperative ABG closure indicating that the limited myringosclerosis has a favorable outcome than ossicular fixation tympanosclerosis group. Table 3 demonstrates the hearing outcome of middle ear surgery in the three groups.
TABLE 3.
Pre and post‐operative audiological parameters according to the type of tympanosclerosis
| Group III: Tympanosclerosis with ossicular fixation underwent ossicular intervention (56) | ||||
|---|---|---|---|---|
| Variable (group) | Group I: No Tympanosclerosis (702) | Group II: Myringosclerosis (174) | Incudo‐malleal fixation (45) | Stapes fixation‐Stapedectomy (11) |
| ABG | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD |
| Pre‐operation | 21.8 ± 7 | 22.1 ± 7 | 32 ± 6.4 dB | 36.8 ± 2.5 dB |
| Post‐operation | 5.4 ± 4.6 | 6.2 ± 5.3 | 13.9 ± 12 dB | 17.7 ± 4.7 dB |
| Closure | 16.4 ± 2.4 | 15.9 ± 1.7 | 18 ± 12.5 | 19 ± 5.4 |
| P value | .0001 | .001 | .0001 | .0001 |
| BC | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD |
| Pre‐operation | 7.6 ± 5.1 | 7.8 ± 5.2 | 6.9 ± 5.4 dB | 6.2 ± 6.2 dB |
| Post‐operation | 8.2 ± 4.8 | 8.8 ± 4.6 | 9.5 ± 4.5 dB | 14 ± 6.6 dB |
| P value | .001 | .001 | .001 | .001 |
Abbreviations: ABG, air‐bone gap; AC, air conduction threshold; BC, bone conduction threshold.
4. DISCUSSION
4.1. Definition and pathology
Tympanosclerosis reflects a hyalinization with subsequent dystrophic calcification of the subepithelial connective tissue (lamina propria) of the tympanic membrane and the mucosa of the middle ear, typically appears as chalky white plaques involve the tympanic membrane and/or middle ear cleft. 10 The etiopathology of tympanosclerosis still not fully understood, tympanosclerosis is considered as an irreversible, result of a degenerative inflammatory process that gives rise to abnormal scarring with hyalinization, calcification, and bone deposition. Several underlying causes and factors are assumed in the pathogenesis of tympanosclerosis, including immunological reactions, genetic redisposition, long‐standing chronic middle ear infection, surgery, trauma, and free oxygen radicals. 4 , 11
4.2. Prevalence and sites of involvement
The incidence of tympanosclerosis in chronic suppurative otitis media (CSOM) varies between 7% and 33%. 1 , 4 In our study, tympanosclerosis was diagnosed in 25.3% of patients with CSOM who underwent tympanoplasty. Clinically, it presents in a single or multiple white plaques or web‐like calcifications either in the tympanic membrane (myringosclerosis), or the tympanic cavity (intratympanic), or both locations. It mainly affects ears with tympanic membrane perforation (80%), but it can appear in intact membranes in 20% of cases. 4 In our study, all our included patients were CSOM cases with perforated TM. Tympanosclerosis affects most commonly the tympanic membrane alone in 50% of cases, it affects the intratympanic structures in 30%, where it can involve any part of the tympanic cleft, such as submucosal areas and the ossicles including the ligaments, joints, and muscle tendons leading to varying degrees of fixity of the ossicular chain. 5 In 20%, tympanosclerosis affects both locations. We found in our study that tympanosclerosis was localized to the eardrum (myringosclerosis) in 73.1% of the cases, isolated intratympanic involvement was seen in 3% which is less than the expectations and the rates in literature, and in 24% was present in both locations of involved ears. Tympanosclerosis is bilateral in around 50% of cases, and it is more frequent in females. 12 But our study showed a higher rate in males.
4.3. Diagnosis and the role of imaging in the diagnosis
Diagnosis of TS can be achieved in most cases by otoscopic examination aided by high resolution computed tomography (HRCT). 4 However, surgical exploration of the middle ear remains the most accurate diagnostic measure especially in determining the actual status of the functional structures. High resolution computed tomography (HRCT) is an excellent tool for the evaluation of a variety of conditions affecting the temporal bone. It has been described that a temporal bone CT scan is a valuable method to diagnose tympanosclerosis and to detect the localization of tympanosclerosis. 13 The main imaging signs of tympanosclerosis on CT include new bone formation and the presence of diffuse or web‐like calcified hyperdense plaques on the tympanic membrane or inside the tympanic cavity involving the ligaments, folds, tendons, and joints. 14 , 15 It has been reported that TS can be associated with reduced pneumatization and soft tissue density inside the middle ear which makes it sometimes hard to differentiate from other soft tissue or chronic inflammatory pathologies. 16
When combined with clinical findings of otoscopy and audiometry, we believe that high resolution computed tomography (HRCT) in tympanosclerosis is of great value in confirming the diagnosis and predicting ossicular involvement and fixation. The surgical approach for a patient with CT showing limited myringosclerosis differs from a patient with intratympanic ossicular involvement which is further differs depending on the degrees, extent, and the ossicles or the complexes are affected. Kikkawa et al comment about the role of the middle ear and mastoid pneumatization in temporal CT in predicting the hearing outcome after stapes surgery for tympanosclerosis with stapes fixation; where they suggested that well‐aerated ears have good hearing results with single‐stage surgery, but for poor pneumatized ears a staged surgery is recommended to get a good hearing improvement. 17 For these reasons, temporal HRCT has a significant role in determining and planning the surgical intervention along with proper pre‐operative counseling for the patient.
In our institution, preoperative temporal bone high‐resolution CT imaging is considered an essential step for preparing patients for ear surgeries. All our patients in this study underwent HRCT of temporal bone preoperatively. The sensitivity and specificity of HRCT to diagnose ossicular tympanosclerotic fixation was sensitivity 96.8% and 98% respectively. Incudo‐malleal fixation diagnosis was the most common type of ossicular fixation in 55 patients (70%), while intraoperatively it was confirmed in 43 ears, while 2 ears out of the 45 confirmed incudo‐malleal fixation no radiological signs of ossicular tympanosclerosis were showed. HRCT stapedial fixation was diagnosed in 19 patients (24%), while intraoperatively it was confirmed in 14 ears. And 5 patients (6%) showed HRCT finding of complete ossicular fixation, all of them were confirmed Intraoperatively. The preoperative positive predictive value (PPV) of HRCT scan in the diagnosis of ossicular chain TS was 78.5% and its preoperative negative predictive value NPV is 99.7%.
4.4. Impact on hearing
The clinical importance of TS arises from the association with significant progressive hearing loss due to interference with sound conduction, transmission, and rarely transduction. Around 6% of tympanosclerosis patients complained of hearing loss. 12 On other hand, the most common presenting complaint is conductive hearing loss. 2 The conductive hearing loss (CHL) presents mainly as a result of fixing the ossicles and to less extent by reducing the tympanic membrane mobility when the TS plaques involve large areas of the TM or fixing it to the annulus, ossicles, or the promontory. 4 An additional factor that can lead to CHL is the association in 80% of cases with TM perforation. A sensorineural component could be present with TS due to previous attacks of middle ear inflammation or due to the involvement of the inner ear by tympanosclerosis toxins as suggested by Gibb et al. 12
The severity of tympanosclerosis impact on hearing is determined mainly by the site and extent of tympanosclerosis plaques. 4 Myringosclerosis in most cases is asymptomatic or has a slight effect on hearing. In contrast, the intratympanic type is expected to cause more significant hearing loss. The principal site of occurrence in the tympanic cavity is the epitympanum area, with the involvement of the incudomalleal joint and the oval window area, with the involvement of the stapes, stapedial tendon, and incudostapedial joint. 12 In the literature, intratympanic tympanosclerosis ossicular involvement is usually seen in about 30%‐40% of cases. 2 Incudomalleal complex fixation in the attic occurs most frequently in around 70% of all tympanosclerotic ossicular fixations, followed by the stapes fixation in around 30% of cases. 18 Our results compare favorably to those as mentioned in the literature where 26.9% of ears with tympanosclerosis showed ossicular fixation, distributed as 70.3% ears with Incudomalleal fixation with ABG of 32 ± 6.4 dB, 21.9% ears with stapes fixation with ABG of 36.8 ± 2.5 dB and 7.8% with triple ossicular fixation with ABG 48 ± 6 dB.
4.5. Treatment and impact of surgical intervention on the hearing
Treatment of tympanosclerosis aims to improve hearing either by hearing aid or surgery. Although the surgical option for tympanosclerosis treatment is challenging; it is widely used and reported. The choice of surgery is believed to be reliable, efficient with long‐lasting hearing results and it is associated with a low incidence of complications. 16 , 19 , 20 Ears with less ossicular chain involvement and limited localization of sclerotic plaques have better hearing gain. 21 The first aim of surgery is to repair the perforated drum, knowing that the graft uptake in tympanosclerosis is excellent and similar to tympanoplasty without tympanosclerosis with a success rate of around 90%; irrespective of whether plaques are excised or not. 21 , 22 The removal of the tympanosclerotic plaques from the residual tympanic membrane is not indicated unless it is large and/or joining the tympanic annulus to the manubrium which impairs the TM mobility. In our series, we had a high success rate of tympanoplasty in the myringosclerosis ears with a postoperative ABG ≤ 20 dB in 96.5% of cases, these results conform with those found in the literature.
The second aim is to restore the transmission function of the fixed ossicles by remobilization or bypass technique via ossiculoplasty or stapes surgery. The surgical strategy depends on the extent and severity of tympanosclerosis which can be predicted using the HRCT and confirmed intraoperatively. An isolated fixed incudo‐malleal complex with mobile stapes can be dealt with in two techniques. The most common method involves bypass technique with PORP ossiculoplasty after disarticulation of the incudostapedial joint followed by removal of the incus and the malleus head just above the insertion of the tensor tympani. 14 The other technique involves mobilization by performing canaloplasty using a diamond burr to clean the sclerotic plaques without damaging the ossicles. In our study, the surgery of the isolated fixed incudomalleal complex tympanosclerosis was achieved using the bypass technique, as we believe it offers a shorter operating time and lower risk of postoperative sensorineural hearing loss. Teufert et al suggest that ossicular reconstruction with PORP can give better results than the mobilization of the major ossicles in patients with tympanosclerosis. 23 Bayazit et al reported that patients with fixed malleus and mobile stapes had significantly better hearing results than those with stapes fixation. 22 The success rate of the surgical treatment was reported with a rate between 65% and 80%. 16 , 21 , 23 , 24 The success rate with a postoperative ABG ≤ 20 dB in our patients using the bypass technique was 88.8%.
Stapes fixation from tympanosclerosis represents a more complicated problem. It is suggested to be more expected with dry ears. 25 The surgical treatment includes surgical mobilization and stapedectomy. The choice of mobilization or stapedectomy relies on the surgical skill and the extent of the disease. Stapedectomy can be performed as one or two‐staged surgery. In the literature, several authors preferred stapedectomy/stapedotomy rather than mobilization as it is more effective and associated with better long‐standing stable results. 22 , 26 , 27 While some authors conclude that both techniques provide similar hearing improvement results. 20 , 23 It is found that stapes remains mobile and does not refix after tympanosclerosis plaque removal. 20 All our cases with fixed stapes underwent stapedectomy by staged surgery. The success rate of the surgical treatment was reported with a rate between 25% and 72%. The success rate. 20 , 21 , 23 , 26 , 27 In our patients using a staged stapedectomy procedure was 81.8%. In the literature, the risk of developing a significant postoperative sensorineural hearing loss is between 1 and 3%. 19 , 23 No significant sensorineural hearing loss or dead ear was seen in our series. In triple ossicular fixation, amplification should always be considered as an alternative to ossicular reconstruction in these instances.
5. CONCLUSION
This study shows that a temporal bone CT scan is a valuable method to diagnose the etiology of hearing loss and to detect the localization of tympanosclerosis, in patients with chronic otitis media and conductive hearing loss. When combined with clinical findings, CT scans can be an informative guide to otolaryngologists for preoperative evaluation of tympanosclerosis. Although surgery of tympanosclerosis is demanding and includes complex counseling, it can lead to a safe and successful surgical treatment of tympanosclerosis.
CONFLICT OF INTEREST
The authors do not have any conflict of interest to disclose.
ACKNOWLEDGMENT
We thank Open Access funding provided by the Qatar National Library.
Larem A, Abu Rajab Altamimi Z, Aljariri AA, et al. Reliability of high‐resolution CT scan in diagnosis of ossicular tympanosclerosis. Laryngoscope Investigative Otolaryngology. 2021;6(3):540–548. 10.1002/lio2.594
Funding information Hamad Medical Corporation, Grant/Award Number: 16100/16; Qatar National Library
BIBLIOGRAPHY
- 1. Kinney SE. Postinflammatory ossicular fixation in tympanoplasty. Laryngoscope. 1978;88:821‐838. [DOI] [PubMed] [Google Scholar]
- 2. Ho KY, Tsai SM, Chai CY, Wang HM. Clinical analysis of intratympanic tympanosclerosis: etiology, ossicular chain findings, and hearing results of surgery. Acta Otolaryngol. 2010;130(3):370‐374. [DOI] [PubMed] [Google Scholar]
- 3. Austin DF. Reconstructive techniques for tympanosclerosis. Ann Otol Rhinol Laryngol. 1988;97:670‐674. [DOI] [PubMed] [Google Scholar]
- 4. Asiri S, Hasham A, Anazy FA, Zakzouk S, Banjar A. Tympanosclerosis: review of literature and incidence among patients with middle ear infection. JLO. 1999;113:1076‐1080. [DOI] [PubMed] [Google Scholar]
- 5. Pal I, Sengupta A. Clinicopathological and audiological study of tympanosclerrosis. Indian J Otolaryngol Head Neck Surg. 2005;57:235‐239. [Google Scholar]
- 6. Yung M, Vowler SL. Long‐term results in ossiculoplasty: an analysis of prognostic factors. Otol Neurotol. 2006;27(6):874‐881. [DOI] [PubMed] [Google Scholar]
- 7. Iñiguez‐Cuadra R, Alobid I, Borés‐Domenech A, Menéndez‐Colino LM, Caballero‐Borrego M, Bernal‐Sprekelsen M. Type III tympanoplasty with titanium total ossicular replacement prosthesis: anatomic and functional results. Otol Neurotol. 2010;31(3):409‐414. [DOI] [PubMed] [Google Scholar]
- 8. Hosny S, El‐Anwar M, Abd‐Elhady M, Khazbak A, El Feky A. Outcomes of myringoplasty in wet and dry ears. Int Adv Otol. 2014;10:256‐259. [Google Scholar]
- 9. Committee on Hearing and Equilibrium guidelines for the evaluation of results of treatment of conductive hearing loss. Otolaryngol Head Neck Surg. 1995;113:186‐187. [DOI] [PubMed] [Google Scholar]
- 10. Miller P. Tympanosclerosis of the eardrum in secretory otitis media. Ada Otolaryngologica (Suppl) (Stockholm). 1984;414:171‐177. [Google Scholar]
- 11. Forseni M, Hansson GK, Bagger‐Sjöback D, Hultcrantz M. An immunohistochemical study of inducible nitric oxide synthase in the rat middle ear, with reference to tympanosclerosis. Acta Otolaryngol. 1999;119:577‐582. [DOI] [PubMed] [Google Scholar]
- 12. Gibb AG, Pang YT. Current considerations in the etiology and diagnosis of tympanosclerosis. Arch Otorhinolaryngol. 1994;251:439‐451. [DOI] [PubMed] [Google Scholar]
- 13. Boyraz E, Erdoğan N, Boyraz I, Kazikdaş C, Etit D, Uluç E. Timpanosklerozun saptanmasinda temporal kemik bilgisayarli tomografi incelemenin yeri ve önemi [The importance of computed tomography examination of temporal bone in detecting tympanosclerosis]. Kulak Burun Bogaz Ihtis Derg. 2009;19(6):294‐298. [PubMed] [Google Scholar]
- 14. Mansour S, Magnan J, Nicolas K, Haidar H. Tympanosclerosis. Middle Ear Diseases. Cham: Springer; 2018. [Google Scholar]
- 15. Swartz JD, Goodman RS, Russell KB, Marlowe FI, Wolfson RJ. High‐resolution computed tomography of the middle ear and mastoid. Part II: Tubotympanic disease. Radiology. 1983;148(2):455‐459. [DOI] [PubMed] [Google Scholar]
- 16. Stankovic MD. Hearing results of surgery for tympanosclerosis. Eur Arch Otorhinolaryngol. 2009;266(5):635‐640. 10.1007/s00405-008-0789-3. [DOI] [PubMed] [Google Scholar]
- 17. Kikkawa S, Kubo K, Kawano H, Komune S. Efficacy of pre‐operative computed tomography evaluation of the tympanic cavity for hearing improvement after stapes surgery for tympanosclerosis with stapes fixation. J Laryngol Otol. 2015;129(suppl 2):S27‐S32. [DOI] [PubMed] [Google Scholar]
- 18. Hussl B, Lim DJ. Histopathology of tympanosclerosis. In: Lim DJ, Bluestone CD, Klein JO, eds. Recent Advances in Otitis Media with Effusion. Philadelphia: Mosby; 1984. [Google Scholar]
- 19. Celik H, Aslan Felek S, Islam A, Safak MA, Arslan N, Gocmen H. Analysis of long‐term hearing after tympanosclerosis with total/partial stapedectomy and prosthesis used. Acta Otolaryngol. 2008;128(12):1308‐1313. [DOI] [PubMed] [Google Scholar]
- 20. Giddings NA, House JW. Tympanosclerosis of the stapes: hearing results for various surgical treatments. Otolaryngol Head Neck Surg. 1992;107:644‐650. [DOI] [PubMed] [Google Scholar]
- 21. Mutlu F, Iseri M, Erdogan S, Ozturk M, Sari F. An analysis of surgical treatment results of patients with tympanosclerosis. J Craniofac Surg. 2015;26(8):2393‐2395. [DOI] [PubMed] [Google Scholar]
- 22. Bayazit YA, Ozer E, Kara C, Gökpinar S, Kanlikama M, Mumbuç S. An analysis of the single‐stage tympanoplasty with over‐underlay grafting in tympanosclerosis. Otol Neurotol. 2004;25(3):211‐214. [DOI] [PubMed] [Google Scholar]
- 23. Teufert KB, De La Cruz A. Tympanosclerosis: long‐term hearing results after ossicular reconstruction. Otolaryngol Head Neck Surg. 2002;126:264‐272. [DOI] [PubMed] [Google Scholar]
- 24. Sakalli E, Celikyurt C, Guler B, Biskin S, Tansuker HD, Erdurak SC. Surgery of isolated malleus fixation due to tympanosclerosis. Eur Arch Otorhinolaryngol. 2015;272(12):3663‐3667. [DOI] [PubMed] [Google Scholar]
- 25. Dinç AE, Kumbul YÇ. Clinical landmarks in chronic otitis media with tympanosclerosis: clinical history may have predictive value in the diagnosis of ossicular chain mobility. J Laryngol Otol. 2019;133(11):1‐3. [DOI] [PubMed] [Google Scholar]
- 26. Vincent R, Oates J, Sperling NM. Stapedotomy for tympanosclerotic stapes fixation: is it safe and efficient? A review of 68 cases. Otol Neurotol. 2002;23(6):866‐872. [DOI] [PubMed] [Google Scholar]
- 27. Kizilkaya Z, Emir H, Ceylan K, Gocmen H, Samim E. The effect of stapes mobility on hearing outcome and which procedure to choose in fixed stapes in children tympanosclerosis. Int J Pediatr Otorhinolaryngol. 2008;72(6):849‐856. [DOI] [PubMed] [Google Scholar]


