Abstract
Background
Head and neck cancer occurs predominantly in the Developing World, with significant challenges relating to a high burden of disease, late presentation, and poor access to curative and palliative care.
Aims
This article describes challenges relating to head and neck cancer care in Sub‐Saharan Africa.
Material & Methods
Educational and training innovations that have been undertaken to improve access to cancer care are presented under the following headings: Open Access Educational Resources African Head and Neck Society (AfHNS); African head and neck surgery fellowship training; AfHNS Virtual Tumor Board; The AfHNS Clinical Practice Guidelines for Head & Neck Cancers in Developing Countries and Limited Resource Settings. Concerns are also raised about universally applicable cancer staging systems.
Results
The challenges facing African patients apply to equally to many other parts of the developing world.
Discussion
The challenges facing African patients apply to equally to many other parts of the developing world.
Conclusions
For outcomes of head and neck cancers to be improved globally, a far greater investment needs to be made in education and training to improve access to care in developing countries. To make a meaningful global impact on morbidity and mortality related to HNC, clinicians, academic institutions and professional societies in developed countries need to be sensitive to these developing world challenges and should directly engage in improving access to care through promoting open access educational resources, offering specialist and fellowship training, collaborating with appropriate research, and establishing and strengthening centers of excellence in developing countries.
Level of Evidence
2c “Outcomes research”.
Keywords: Africa, cancer, guidelines, head, interventions, neck
To make a meaningful global impact on morbidity and mortality related to HNC, clinicians, academic institutions and professional societies in developed countries need to be sensitive to these developing world challenges and should directly engage in improving access to care through promoting open access educational resources, offering specialist and fellowship training, collaborating with appropriate research, and establishing and strengthening centers of excellence in developing countries.
1. INTRODUCTION
Head and neck cancer (HNC) is primarily a Developing World disease. Developing countries account for 67% of global HNC and 82% of HNC‐related deaths. 1 Despite this large cancer burden, developing countries account for only 5% of global cancer spending. 2 Both the incidence and mortality from cancer in Africa are predicted to increase almost 2‐fold between 2010 and 2030. 3
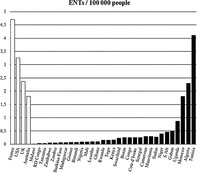
Patients in developing countries tend to present late with HNC; two‐thirds of patients in India present with advanced tumors 4 ; and in Cape Town ~50% of laryngectomees require emergency tracheostomy. 5 Access to investigations and treatment in developing countries is limited. Only about 5% of patients in Africa and 3% in South Asia have timely access to safe, affordable surgery (Figure 1). 6 Sub‐Saharan Africa has only 18 fellowship‐trained head and neck surgeons for its >1 billion people. 7
FIGURE 1.
No access to timely safe affordable surgery 6
Access to cytology, histopathology, specialized radiology, operating time, safe anaesthesia and ICU beds are also limited, 7 and many poor patients cannot afford to pay out of pocket for cancer investigations and treatment. Only 24/52 African countries have radiotherapy services, and in some countries with radiation therapy facilities, patients may wait up to 46 weeks to commence treatment. 8 Even where radiation is available, old technology is often employed. Palliation for cancer in developing countries also presents a challenge with <4% of people in India who are suffering with chronic pain from cancer having access to morphine, 9 and many African countries do not dispense opioids.
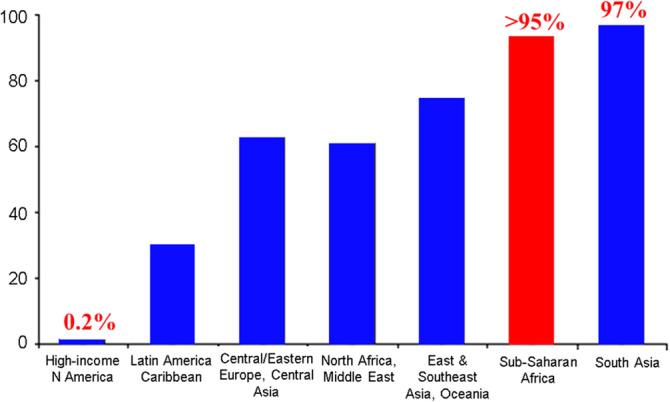
Because of the lack of head and neck surgeons in Africa, reliance mostly falls on medical officers, otolaryngologists, and general surgeons to diagnose and manage HNC. However, Africa has a severe shortage of doctors and otolaryngologists (Figure 2). 10 Part of the reason for the shortage of doctors is medical migration. About 25% of doctors who train in Sub‐Saharan Africa migrate to higher income countries. 11 The UK actively recruits international medical graduates to make up for the shortfall of doctors in their National Health Service. 12 In addition to the impact on healthcare delivery, this migration of doctors from lower‐ to higher‐income settings has substantial economic consequences that are not simply due to movement of human capital, but also due to excess mortality associated with loss of physicians. 13
FIGURE 2.
Otolaryngologists/100 000 people in Africa, compared to France, USA, UK, and Australia
In summary, HNC is primarily a Developing World problem with significant challenges relating to a high (and increasing) burden of disease, late presentation, and poor access to both curative and palliative care, and how HNCs are investigated and treated in developed vs developing countries is increasingly divergent because of technological, financial, and infrastructural disparities.
For outcomes of HNC to be significantly impacted globally, and because HNC is primarily a Developing World disease, an international effort is required to improve access to HNC care in developing countries. Some initiatives that have been introduced to improve access to HNC care in Sub‐Saharan Africa are presented. Because challenges facing African HNC patients and clinicians reflect those in other developing countries, these interventions have global relevance.
2. OPEN ACCESS EDUCATIONAL RESOURCES
Accessing appropriate educational and scientific material is central to improving HNC care in developing countries. Yet many trainees, practitioners, and researchers in Sub‐Saharan Africa simply cannot afford to purchase textbooks and pay‐to‐view journals or to publish their research in pay‐to‐publish journals. The content of journals and textbooks is also often inappropriate for resource constrained settings that do not have modern investigations and treatment modalities such as robotic, laser or microvascular free tissue transfer reconstructive surgery. These were the reasons for establishing The Open Access Atlas of Otolaryngology, Head and Neck Operative Surgery (http://www.entdev.uct.ac.za/guides/open-access-atlas-of-otolaryngology-head-neck-operative-surgery/). It is a free, open access surgical atlas edited and self‐published by the author (JJF) in Cape Town, South Africa. More than 100 authors from >20 countries have contributed, with senior authors generally being international leaders in their fields. Volunteers have translated chapters into Spanish, French and Portuguese. Chapters provide detailed step‐by‐step descriptions of a range of head and neck surgical procedures, that includes operations no longer performed in developed countries such as laryngofissure for early laryngeal cancer which would not be included in modern textbooks. Being in electronic format, chapters are very detailed with photographs and videoclips used to illustrate the text. Being a “living” document it can be regularly edited and updated. It has not cost a cent to produce or to publish. The atlas has been popular both in developing and developed countries, with the United States its biggest user, followed by India and the United Kingdom. With >2 m chapters downloaded at a rate of a chapter download every 43 seconds, it raises questions about the future of conventional textbooks. Authors and societies should be encouraged to embrace open access publishing to freely share knowledge as widely as possible.
3. AFRICAN HEAD AND NECK SOCIETY (AfHNS)
Because of resource constraints, the way that patients are managed in Africa often differs from that in Developed World centers of excellence. The African Head and Neck Society (https://afhns.org) was founded in 2016 by the 1st 14 African fellowship‐trained head and neck surgeons. Its mission is to improve outcomes of patients with diseases of the head and neck in Africa through prevention, clinical excellence, teaching, training, and research. It has held annual conferences and surgical cadaver dissection courses and ultrasound workshops, has published research, and has advocated about issues that affect HNC in developing countries such as cancer staging (see below). It fulfills a key role in advancing HNC care and training in Sub‐Saharan Africa and nurturing an African (and Developing World) culture of HNC care through its monthly AfHNS Virtual Tumor Board meetings, and its African Head and Neck Society Clinical Practice Guidelines for Head & Neck Cancers in Developing Countries and Limited Resource Settings.
4. AFRICAN HEAD AND NECK SURGERY FELLOWSHIP TRAINING
For access to HNC care to improve, Africa needs more head and neck surgeons who can teach head and neck oncologic surgery through establishing centers of excellence across the continent. Two African head and neck fellowship programs have trained 17 head and neck surgeons from 13 African countries, with an 18th currently in training. The University of Cape Town has a 1‐year hands‐on fellowship that is modelled on American head and neck fellowship programs and is funded by Karl Storz; it is currently training its 15th fellow. The surgical exposure of Cape Town fellows is equivalent to fellowships in the United States. 8 The Pan‐African Association of Christian Surgeons (PAACS)/Johns Hopkins fellowship is based at Mbingo Baptist Hospital in Cameroon. It is a novel hybrid training model with American teaching faculty rotating at the hospital. This fellowship has unfortunately temporarily been suspended due to civil unrest. An analysis of whether African fellowships make a sustainable impact on HNC care in Sub‐Saharan Africa reported that all fellows had returned to their countries; all were doing work in public hospitals and transferring surgical skills to trainees; those with radiation therapy services had established multidisciplinary clinics at their centers; and there had been a 335% overall increase in major head and neck surgeries. The authors concluded that high volume, specialized head and neck surgical training was possible in Africa; and that training was appropriate in terms of pathology and types of surgery. They also concluded that the fellowships had made a sustainable contribution to head and neck practice in Sub‐Saharan Africa by populating it with surgeons and teachers of head and neck surgery, by them establishing centers of excellence, by building clinical capacity, and by instituting resource appropriate management. 7 The African Head and Neck Society (AfHNS) is currently formulating an AfHNS‐endorsed fellowship programme to increase training opportunities at more training centers in Africa. Unlike other fellowships, training would not be restricted to 1 or 2 years, but may be extended to ensure adequate clinical exposure and training. Clinical experience could be acquired at more than one institution and through international surgical outreach programs. The AfHNS Fellowship would include a formal workplace‐based assessment of clinical competence for a range of surgical procedures that includes those relevant to resource constrained settings, as well as a virtual theoretical examination to assess knowledge, clinical reasoning and complex decision making related to HNC. However, to accelerate the growth of head and neck services in Africa, developed countries should be encouraged to ringfence a number of funded fellowship training opportunities for African trainees.
5. AfHNS VIRTUAL TUMOR BOARD
The AfHNS introduced a monthly virtual tumor board meeting using ZOOM in 2020. It is a free, open access, multidisciplinary meeting at which interesting HNC cases are presented and discussed from around Sub‐Saharan Africa. It attracts up to150 attendees also from outside Africa, including North America, Europe, Middle East and South and Southeast Asia. These tumor board case presentations are fostering a HNC treatment culture tailored to resource constrained settings, which may sometimes differ from that in Developed World centers. The AfHNS virtual tumor board illustrates how virtual conferencing platforms have empowered developing countries to advance education and to disseminate knowledge, and to promote international collaboration.
6. THE AFRICAN HEAD AND NECK SOCIETY CLINICAL PRACTICE GUIDELINES FOR HEAD & NECK CANCERS IN DEVELOPING COUNTRIES AND LIMITED RESOURCE SETTINGS
International HNC guidelines (eg, NCCN) are often unhelpful, inappropriate or even harmful when applied in resource constrained settings when special investigations, radiotherapy, and complex surgery are unavailable or unaffordable, or when management of sequelae of treatment such as hypothyroidism, renal failure, and dysphagia are inadequate, or cancer surveillance is not possible. The African Head and Neck Society Clinical Practice Guidelines (https://afhns.org or https://developingworldheadandneckcancerguidelines.com/) seek to optimize HNC care by precisely tailoring investigations and treatment according to resources available (or affordable) to a patient, or whether a patient can cope with consequences of treatment, or is likely to return for follow‐up. Figure 3 illustrates management algorithms for parotid tumors. The first is a management algorithm for when there are no resource limitations; the second is a management algorithm for when FNAC and imaging are not available; and the third applies to a situation when FNAC, imaging and total parotidectomy expertise are unavailable. Management algorithms have also been published for cancers of the thyroid, submandibular glands, oral cavity, oropharynx, hypopharynx, and larynx, with guidelines currently being written for nasopharynx cancer and the unknown primary.
FIGURE 3.
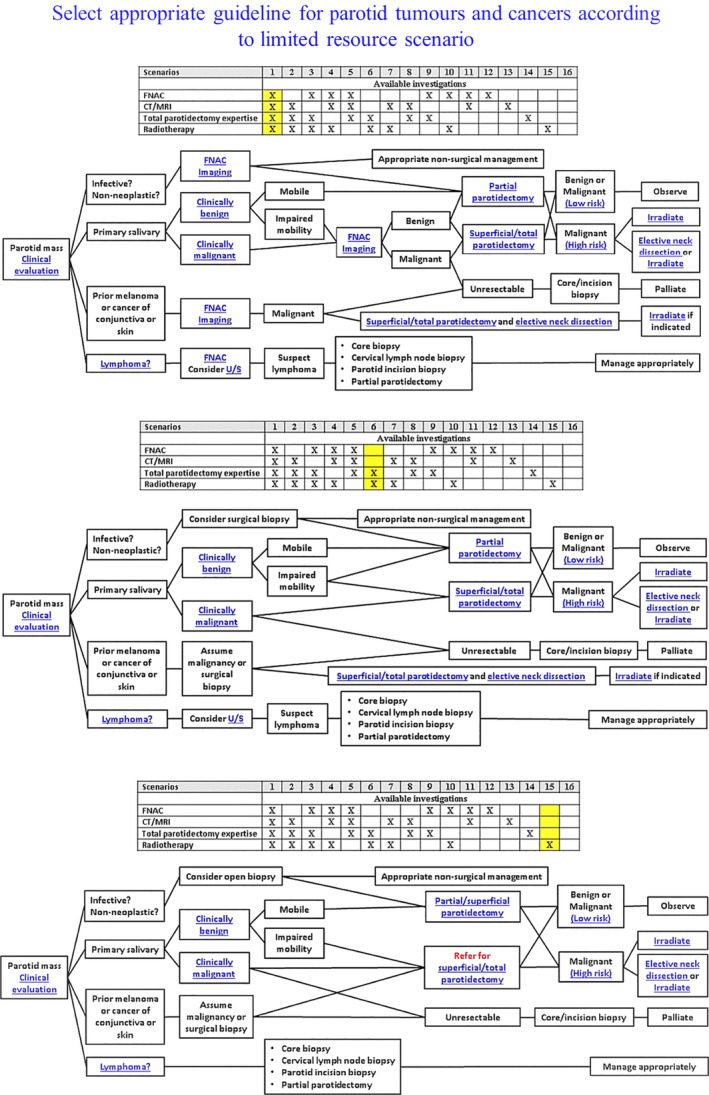
AfHNS Clinical Practice Guidelines for parotid tumours: three resource scenarios
The AfHNS guidelines reflect expert opinion of senior members of the AfHNS and selected international surgeons and oncologists and are directed not only at local surgeons and oncologists, but also at those engaged in surgical outreach to developing countries. Clinicians in Africa and the “Global South” are best qualified to write such guidelines as they best understand the challenges, constraints, and possibilities of HNC care in limited resource settings. These guidelines also reflect the “Global South” assuming ownership, leadership, and responsibility for HNC practice in developing countries. The guidelines are well used and have been accessed by >9000 visitors with >46 000 page views in the initial 2 years.
7. DEVELOPING WORLD HNC STAGING DILEMMAS
The AfHNS has expressed concerns about the applicability of AJCC/UICC staging in developing countries. 14 Although anatomical site and tumor extent remain central to defining cancer prognosis and staging, the AJCC and UICC have increasingly incorporated non‐anatomic prognostic factors into stage groupings. In the eighth edition of the AJCC cancer staging manual, p16 status was included in staging of oropharyngeal carcinoma. However, 16/17 fellowship‐trained head and neck surgeons in 13 Sub‐Saharan African countries cannot test oropharynx cancers for p16 as the test is either unavailable in their country or is unaffordable for the patient. 14 Another issue for staging bodies to consider is the diversity of the type and quality of therapeutic interventions in developed vs developing countries that might affect cancer outcomes and prognosis. As previously stated, many African and developing countries have no radiotherapy facilities, or access is very limited. Some chemotherapy drugs and most targeted agents are also not available to patients in such countries. Such treatment limitations would for instance invalidate the favorable prognosis associated with advanced p16+ oropharyngeal cancer in such settings, as is reflected in the current staging.
Due to widening disparities in healthcare resources across the world, having a universal staging system is therefore becoming ever more difficult to achieve. Therefore, while the AJCC/UICC should be encouraged to refine staging systems that best reflect prognosis by incorporating non‐anatomical factors, anatomically based staging needs to be retained for resource‐constrained settings. Not having resource‐appropriate staging would reduce the AJCC/UICC's global relevance and disadvantage most of the world's HNC patients. A staging system that considers available diagnostic and therapeutic resources, as has been done with the African Head and Neck Society Clinical Treatment Guidelines for Head and Neck Cancer should be considered. Should the AJCC/UICC elect not to address this issue, then it may present an opportunity for the “Global South” to promulgate its own resource‐appropriate staging guidelines.
8. CONCLUSIONS
HNC is predominantly a Developing World disease. Challenges facing African HNC patients apply equally in much of the Developing World such as overwhelming burden of disease, late presentation, and poor access to special investigations and curative and palliative care. To make a meaningful global impact on morbidity and mortality related to HNC, clinicians, academic institutions and professional societies in developed countries need to be sensitive to these developing world challenges and should directly engage in improving access to care through promoting open access educational resources, offering specialist and fellowship training, collaborating with appropriate research, and establishing and strengthening centers of excellence in developing countries.
Fagan JJ. Africa: A window on challenges and opportunities for head and neck cancer. Laryngoscope Investigative Otolaryngology. 2021;6:414–419. 10.1002/lio2.554
Meeting information: Grand Rounds at Massachusetts Eye & Ear, Harvard, USA: January 14, 2021: Africa: A Window on Challenges and Opportunities for Head and Neck Cancer.
Funding information Invited article so no charge
REFERENCES
- 1. Patterson RH, Fischman VG, Wasserman I, et al. Global burden of head and neck cancer: economic consequences, health, and the role of surgery. Otolaryngol Head Neck Surg. 2020;162(3):296‐303. [DOI] [PubMed] [Google Scholar]
- 2. Farmer P, Frenk J, Knaul FM, et al. Expansion of cancer care and control in countries of low and middle income: a call to action. Lancet. 2010;376(9747):1186‐1193. [DOI] [PubMed] [Google Scholar]
- 3. Sylla BS, Wild CP. A million Africans a year dying from cancer by 2030: what can cancer research and control offer to the continent? Int J Cancer. 2012;130(2):245‐250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Joshi P, Datta S, Chaturvedi P, Nair S. Head and neck cancers in developing countries. Rambam Maimonides Med J. 2014;5(2):e0009. 10.5041/RMMJ.10143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fagan JJ. Semon lecture, Royal Society of Medicine: 'laryngectomy practice based on personal research'. J Laryngol Otol. 2020; (In press). [DOI] [PubMed] [Google Scholar]
- 6. Alkire BC, Raykar NP, Shrime MG, et al. Global access to surgical care. A modelling study. Lancet Global Health. 2015;3:e316‐e323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fagan JJ, Otiti J, Aswani J, et al. African head and neck fellowships: a model for a sustainable impact on head and neck cancer care in developing countries. Head Neck. 2019;41(6):1824‐1829. [DOI] [PubMed] [Google Scholar]
- 8. Fagan JJ, Zafereo M, Aswani J, Netterville JL, Koch W. Head and neck surgical subspecialty training in Africa: sustainable models to improve cancer care in developing countries. Head Neck. 2017;39(3):605‐611. [DOI] [PubMed] [Google Scholar]
- 9. Human Rights Watch . Unbearable Pain: India's Obligation to Ensure Palliative Care. October 28, 2009. https://www.hrw.org/report/2009/10/28/unbearable-pain/indias-obligation-ensure-palliative-care (accessed February 2, 2021).
- 10. Mulwafu W, Ensink R, Kuper H, Fagan JJ. Survey of ENT services in sub‐Saharan Africa: little progress between 2009 and 2015. Global Health Action. 2017;10(1). 10.1080/16549716.2017.1289736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. World Health Organization . World Health Report: Working Together For Health; 2006. http://www.who.int/whr/2006/whr06_en.pdf (accessed February 2, 2021).
- 12. Fagan JJ, Bhutta MF. General medical council report exposes unethical recruitment of doctors in the UKfrom low‐resource countries. S Afr Med J. 2021;111(3):189. http://www.samj.org.za/index.php/samj/article/view/13161. [DOI] [PubMed] [Google Scholar]
- 13. Saluja S, Rudolfson N, Massenburg BB, Meara JG, Shrime MG. The impact of physician migration on mortality in low and middle‐income countries: an economic modelling study. BMJ Glob Health. 2020;5(1):e001535. 10.1136/2Fbmjgh-2019-001535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fagan JJ, Wetter J, Otiti J, et al. Is AJCC/UICC staging still appropriate for head and neck cancers in developing countries? OTO Open. 2020;4(3):2473974X20938313. 10.1177/2473974X20938313. [DOI] [PMC free article] [PubMed] [Google Scholar]


